Moderate-Intensity Constant and High-Intensity Interval Training Confer Differential Metabolic Benefits in Skeletal Muscle, White Adipose Tissue, and Liver of Candidates to Undergo Bariatric Surgery
Abstract
1. Introduction
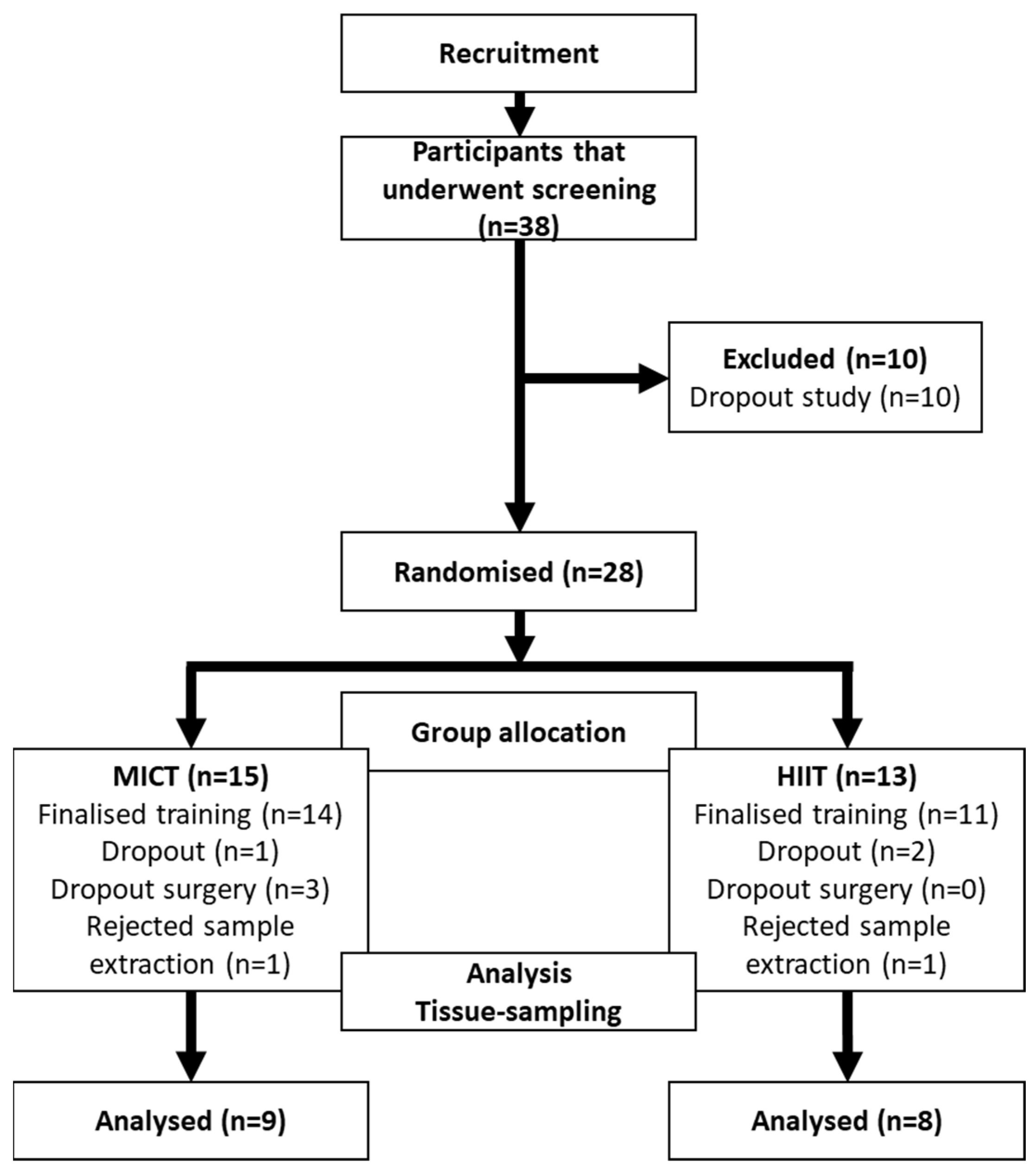
2. Materials and Methods
2.1. Ethics Statement
2.2. Study Design
2.3. Participants
2.4. Exercise Intervention and Sample Extraction
2.5. Phenotypical Measurements
2.6. Laboratory Exams
2.7. Protein Analysis by Western Immunoblotting and Histology
2.8. Statistical Analysis
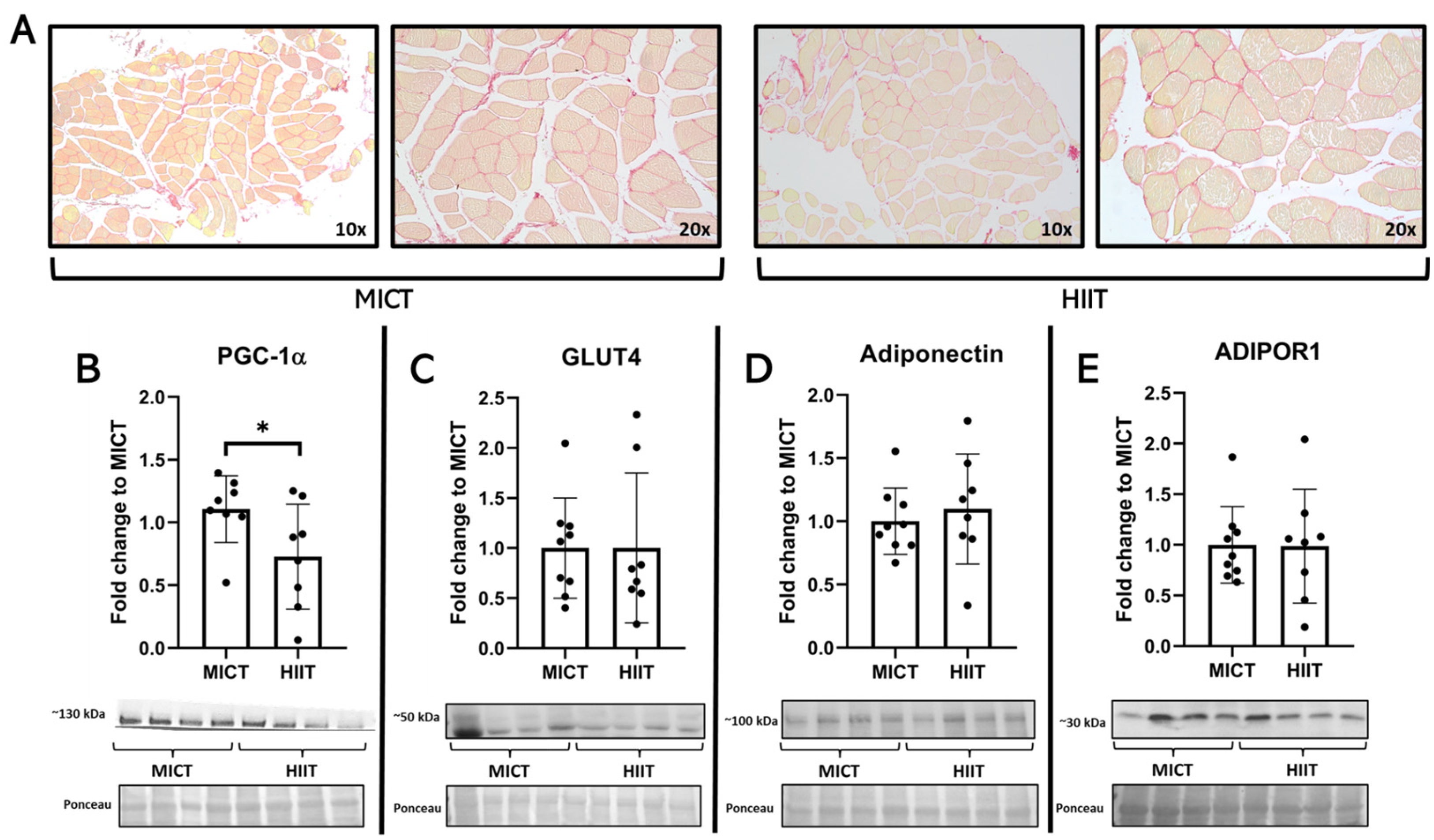
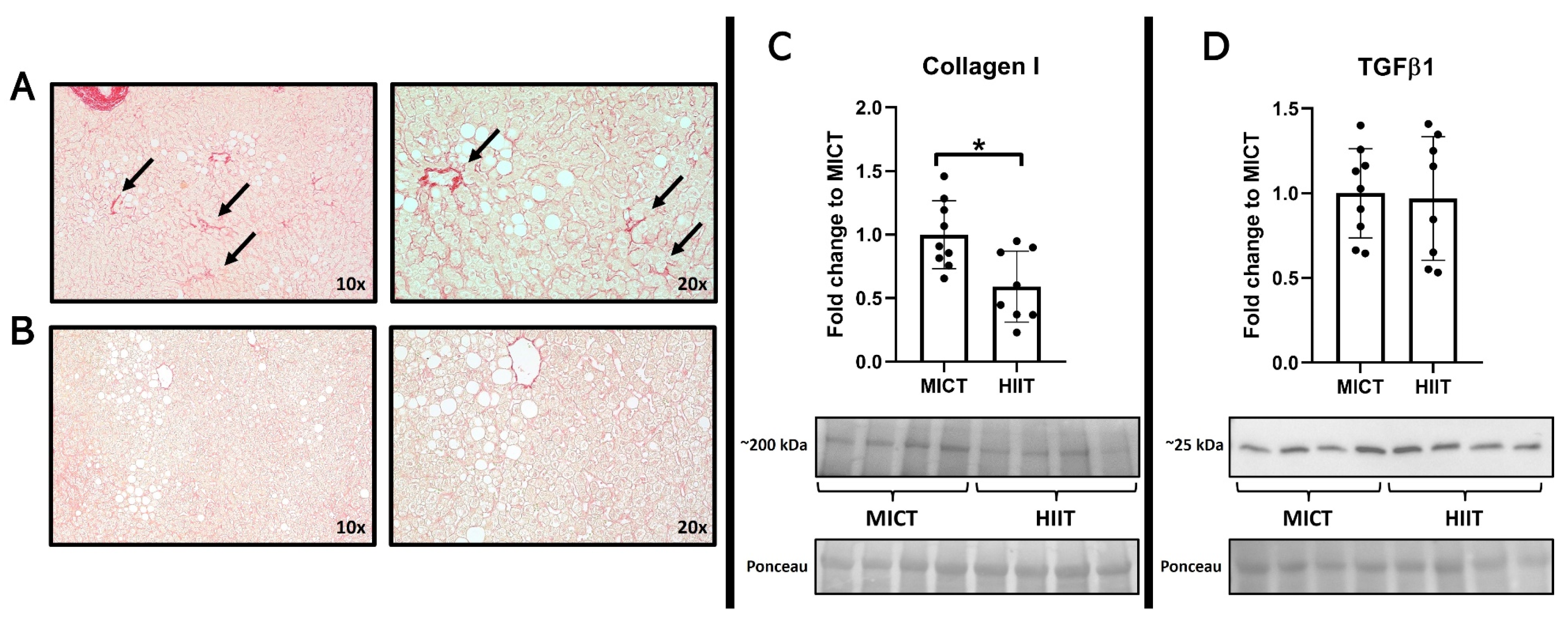
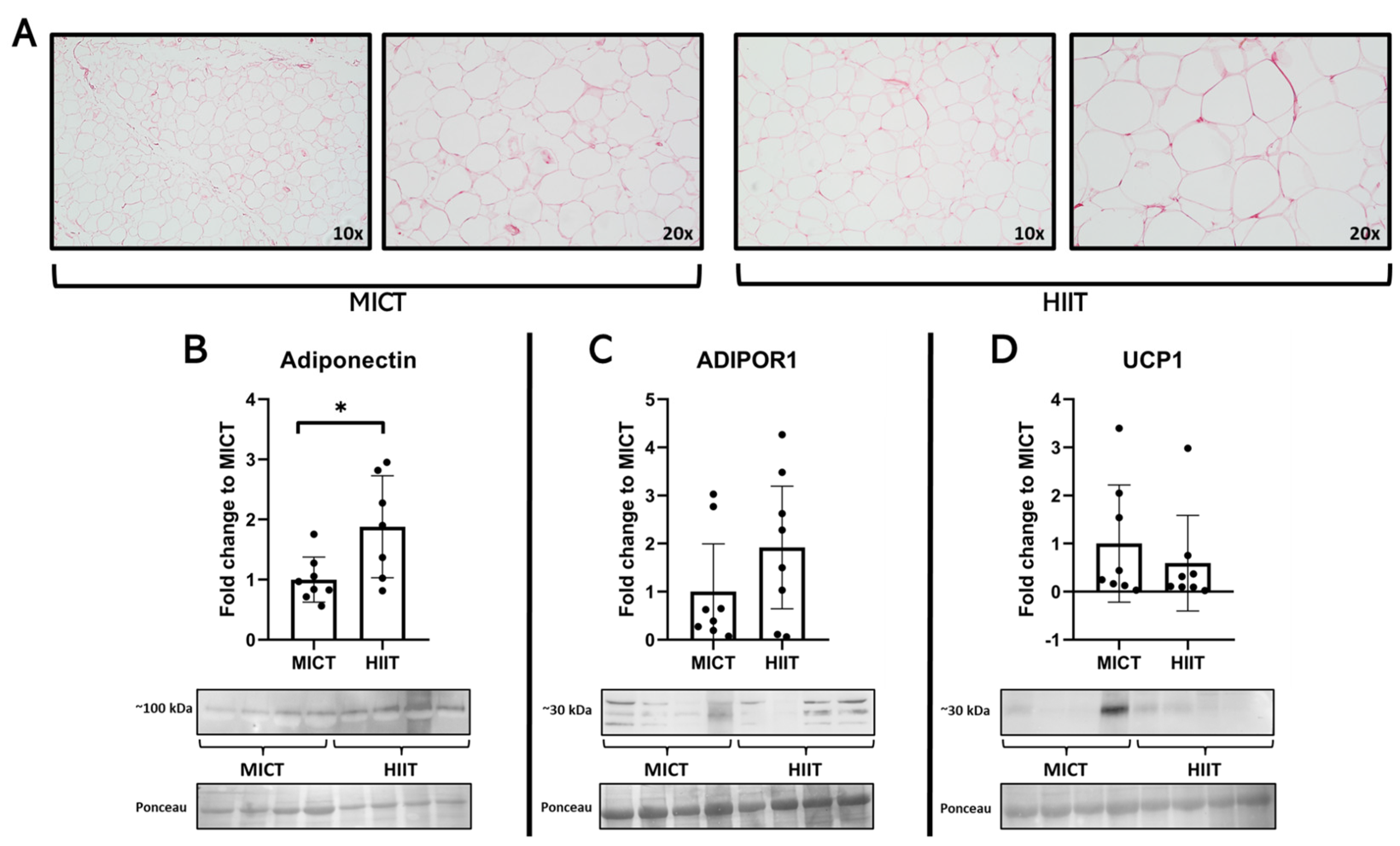
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Drozdz, D.; Alvarez-Pitti, J.; Wójcik, M.; Borghi, C.; Gabbianelli, R.; Mazur, A.; Herceg-Čavrak, V.; Lopez-Valcarcel, B.G.; Brzeziński, M.; Lurbe, E.; et al. Obesity and Cardiometabolic Risk Factors: From Childhood to Adulthood. Nutrients 2021, 13, 4176. [Google Scholar] [CrossRef] [PubMed]
- Cosentino, C.; Marchetti, C.; Monami, M.; Mannucci, E.; Cresci, B. Efficacy and effects of bariatric surgery in the treatment of obesity: Network meta-analysis of randomized controlled trials. Nutr. Metab. Cardiovasc. Dis. 2021, 31, 2815–2824. [Google Scholar] [CrossRef]
- Kassir, R.; Debs, T.; Blanc, P.; Gugenheim, J.; Ben Amor, I.; Boutet, C.; Tiffet, O. Complications of bariatric surgery: Presentation and emergency management. Int. J. Surg. 2016, 27, 77–81. [Google Scholar] [CrossRef] [PubMed]
- Varbanova, M.; Maggard, B.; Lenhardt, R. Preoperative preparation and premedication of bariatric surgical patient. Saudi J. Anaesth. 2022, 16, 287–298. [Google Scholar] [CrossRef] [PubMed]
- Hardy, K.; Kwok, K.; Bouchard, D.R.; Bharti, N.; Gamey, D.; Vergis, A. Impact of a Preoperative Exercise Program on General Fitness in Patients Awaiting Bariatric Surgery: A Pilot Randomized Trial. Cureus 2022, 14, e22566. [Google Scholar] [CrossRef]
- Mao, R.-M.D.; Franco-Mesa, C.; Samreen, S. Prehabilitation in metabolic and bariatric surgery: A narrative review. Ann. Laparosc. Endosc. Surg. 2023, 8, 3. [Google Scholar] [CrossRef]
- Martinez-Huenchullan, S.F.; Kalazich Rosales, M.; Mautner Molina, C.; Fuentes Leal, F.; Cárcamo Ibaceta, C.; Tam, C.S.; Ehrenfeld, P. Physiological relevance of aerobic exercise training for the preparation of bariatric surgery candidates. Physiol. Mini Rev. 2021, 14, 20–33. [Google Scholar]
- Bond, D.S.; Jakicic, J.M.; Unick, J.L.; Vithiananthan, S.; Pohl, D.; Roye, G.D.; Ryder, B.A.; Sax, H.C.; Wing, R.R. Pre- to postoperative physical activity changes in bariatric surgery patients: Self report vs. objective measures. Obesity 2010, 18, 2395–2397. [Google Scholar] [CrossRef] [PubMed]
- Mika, A.; Macaluso, F.; Barone, R.; Di Felice, V.; Sledzinski, T. Effect of Exercise on Fatty Acid Metabolism and Adipokine Secretion in Adipose Tissue. Front. Physiol. 2019, 10, 26. [Google Scholar] [CrossRef]
- Gerosa-Neto, J.; Panissa, V.L.G.; Monteiro, P.A.; Inoue, D.S.; Ribeiro, J.P.J.; Figueiredo, C.; Zagatto, A.M.; Little, J.P.; Lira, F.S. High- or moderate-intensity training promotes change in cardiorespiratory fitness, but not visceral fat, in obese men: A randomised trial of equal energy expenditure exercise. Respir. Physiol. Neurobiol. 2019, 266, 150–155. [Google Scholar] [CrossRef]
- Jung, M.E.; Bourne, J.E.; Beauchamp, M.R.; Robinson, E.; Little, J.P. High-intensity interval training as an efficacious alternative to moderate-intensity continuous training for adults with prediabetes. J. Diabetes Res. 2015, 2015, 191595. [Google Scholar] [CrossRef]
- Martínez-Huenchullán, S.F.; Fox, S.L.; Tam, C.S.; Maharjan, B.R.; Olaya-Agudo, L.F.; Ehrenfeld, P.; Williams, P.F.; Mclennan, S.V.; Twigg, S.M. Constant-moderate versus high-intensity interval training on heart adiponectin levels in high-fat fed mice: A preventive and treatment approach. Arch. Physiol. Biochem. 2023, 129, 41–45. [Google Scholar] [CrossRef] [PubMed]
- Martinez-Huenchullan, S.F.; Ban, L.A.; Olaya-Agudo, L.F.; Maharjan, B.R.; Williams, P.F.; Tam, C.S.; Mclennan, S.V.; Twigg, S.M. Constant-Moderate and High-Intensity Interval Training Have Differential Benefits on Insulin Sensitive Tissues in High-Fat Fed Mice. Front. Physiol. 2019, 10, 459. [Google Scholar] [CrossRef] [PubMed]
- Chavanelle, V.; Boisseau, N.; Otero, Y.F.; Combaret, L.; Dardevet, D.; Montaurier, C.; Delcros, G.; Peltier, S.L.; Sirvent, P. Effects of high-intensity interval training and moderate-intensity continuous training on glycaemic control and skeletal muscle mitochondrial function in db/db mice. Sci. Rep. 2017, 7, 204. [Google Scholar] [CrossRef] [PubMed]
- Cho, J.; Kim, S.; Lee, S.; Kang, H. Effect of Training Intensity on Nonalcoholic Fatty Liver Disease. Med. Sci. Sports Exerc. 2015, 47, 1624–1634. [Google Scholar] [CrossRef] [PubMed]
- Cancino-Ramirez, J.; Troncoso-Ortiz, E.J.; Pino, J.; Olivares, M.; Escaffi, M.J.; Riffo, A.; Podestá, D.I.; Vásquez, M.M.; Gonzalez-Rojas, L. Exercise and physical activity in adults who underwent bariatric surgery. Consensus document. Rev. Med. Chil. 2019, 147, 1468–1486. [Google Scholar] [CrossRef] [PubMed]
- Czartoryski, P.; Garcia, J.; Manimaleth, R.; Napolitano, P.; Watters, H.; Weber, C.; Alvarez-Beaton, A.; Nieto, A.C.; Patel, A.; Peacock, C.; et al. Body Composition Assessment: A Comparison of the DXA, InBody 270, and Omron. J. Exerc. Nutr. 2020, 3, 1–6. [Google Scholar]
- Lira, V.A.; Benton, C.R.; Yan, Z.; Bonen, A. PGC-1alpha regulation by exercise training and its influences on muscle function and insulin sensitivity. Am. J. Physiol. Endocrinol. Metab. 2010, 299, E145–E161. [Google Scholar] [CrossRef]
- Halling, J.F.; Pilegaard, H. PGC-1alpha-mediated regulation of mitochondrial function and physiological implications. Appl. Physiol. Nutr. Metab. 2020, 45, 927–936. [Google Scholar] [CrossRef]
- Egan, B.; Carson, B.P.; Garcia-Roves, P.M.; Chibalin, A.V.; Sarsfield, F.M.; Barron, N.; McCaffrey, N.; Moyna, N.M.; Zierath, J.R.; O’gorman, D.J. Exercise intensity-dependent regulation of peroxisome proliferator-activated receptor coactivator-1 mRNA abundance is associated with differential activation of upstream signalling kinases in human skeletal muscle. J. Physiol. 2010, 588, 1779–1790. [Google Scholar] [CrossRef]
- Zheng, L.; Rao, Z.; Guo, Y.; Chen, P.; Xiao, W. High-Intensity Interval Training Restores Glycolipid Metabolism and Mitochondrial Function in Skeletal Muscle of Mice with Type 2 Diabetes. Front. Endocrinol. (Lausanne) 2020, 11, 561. [Google Scholar] [CrossRef] [PubMed]
- Gastaldi, G.; Russell, A.; Golay, A.; Giacobino, J.-P.; Habicht, F.; Barthassat, V.; Muzzin, P.; Bobbioni-Harsch, E. Upregulation of peroxisome proliferator-activated receptor gamma coactivator gene (PGC1A) during weight loss is related to insulin sensitivity but not to energy expenditure. Diabetologia 2007, 50, 2348–2355. [Google Scholar] [CrossRef]
- Ryan, B.J.; Schleh, M.W.; Ahn, C.; Ludzki, A.C.; Gillen, J.B.; Varshney, P.; Van Pelt, D.W.; Pitchford, L.M.; Chenevert, T.L.; A Gioscia-Ryan, R.; et al. Moderate-Intensity Exercise and High-Intensity Interval Training Affect Insulin Sensitivity Similarly in Obese Adults. J. Clin. Endocrinol. Metab. 2020, 105, e2941-59. [Google Scholar] [CrossRef] [PubMed]
- Khalafi, M.; Ravasi, A.A.; Malandish, A.; Rosenkranz, S.K. The impact of high-intensity interval training on postprandial glucose and insulin: A systematic review and meta-analysis. Diabetes Res. Clin. Pract. 2022, 186, 109815. [Google Scholar] [CrossRef] [PubMed]
- Richter, E.A. Is GLUT4 translocation the answer to exercise-stimulated muscle glucose uptake? Am. J. Physiol. Endocrinol. Metab. 2021, 320, E240–E243. [Google Scholar] [CrossRef]
- Roy, D.; Marette, A. Exercise induces the translocation of GLUT4 to transverse tubules from an intracellular pool in rat skeletal muscle. Biochem. Biophys. Res. Commun. 1996, 223, 147–152. [Google Scholar] [CrossRef] [PubMed]
- Host, H.H.; Hansen, P.A.; Nolte, L.A.; Chen, M.M.; Holloszy, J.O. Rapid reversal of adaptive increases in muscle GLUT-4 and glucose transport capacity after training cessation. J. Appl. Physiol. (1985) 1998, 84, 798–802. [Google Scholar] [CrossRef]
- Martinez-Huenchullan, S.F.; Maharjan, B.R.; Williams, P.F.; Tam, C.S.; McLennan, S.V.; Twigg, S.M. Differential metabolic effects of constant moderate versus high intensity interval training in high-fat fed mice: Possible role of muscle adiponectin. Physiol. Rep. 2018, 6, e13599. [Google Scholar] [CrossRef] [PubMed]
- Dai, Y.; Pang, J.; Gong, H.; Fan, W.; Zhang, T.M. Roles and tissue source of adiponectin involved in lifestyle modifications. J. Gerontol. A Biol. Sci. Med. Sci. 2013, 68, 117–128. [Google Scholar] [CrossRef]
- Garekani, E.T.; Mohebbi, H.; Kraemer, R.R.; Fathi, R. Exercise training intensity/volume affects plasma and tissue adiponectin concentrations in the male rat. Peptides 2011, 32, 1008–1012. [Google Scholar] [CrossRef]
- Goto, A.; Ohno, Y.; Ikuta, A.; Suzuki, M.; Ohira, T.; Egawa, T.; Sugiura, T.; Yoshioka, T.; Ohira, Y.; Goto, K. Up-regulation of adiponectin expression in antigravitational soleus muscle in response to unloading followed by reloading, and functional overloading in mice. PLoS ONE 2013, 8, e81929. [Google Scholar] [CrossRef]
- Francque, S.M.A.; Dirinck, E. NAFLD prevalence and severity in overweight and obese populations. Lancet Gastroenterol. Hepatol. 2023, 8, 2–3. [Google Scholar] [CrossRef] [PubMed]
- Baker, C.J.; Martinez-Huenchullan, S.F.; D’Souza, M.; Xu, Y.; Li, M.; Bi, Y.; Johnson, N.A.; Twigg, S.M. Effect of exercise on hepatic steatosis: Are benefits seen without dietary intervention? A systematic review and meta-analysis. J. Diabetes 2021, 13, 63–77. [Google Scholar] [CrossRef] [PubMed]
- Houttu, V.; Bouts, J.; Vali, Y.; Daams, J.; Grefhorst, A.; Nieuwdorp, M.; Holleboom, A.G. Does aerobic exercise reduce NASH and liver fibrosis in patients with non-alcoholic fatty liver disease? A systematic literature review and meta-analysis. Front. Endocrinol. (Lausanne) 2022, 13, 1032164. [Google Scholar] [CrossRef] [PubMed]
- Oh, S.; So, R.; Shida, T.; Matsuo, T.; Kim, B.; Akiyama, K.; Isobe, T.; Okamoto, Y.; Tanaka, K.; Shoda, J. High-Intensity Aerobic Exercise Improves Both Hepatic Fat Content and Stiffness in Sedentary Obese Men with Nonalcoholic Fatty Liver Disease. Sci. Rep. 2017, 7, 43029. [Google Scholar] [CrossRef]
- O’Gorman, P.; Naimimohasses, S.; Monaghan, A.; Kennedy, M.; Melo, A.M.; Ni Fhloinn, D.; Doherty, D.G.; Beddy, P.; Finn, S.P.; Moore, J.B.; et al. Improvement in histological endpoints of MAFLD following a 12-week aerobic exercise intervention. Aliment. Pharmacol. Ther. 2020, 52, 1387–1398. [Google Scholar] [CrossRef] [PubMed]
- Fabregat, I.; Moreno-Càceres, J.; Sánchez, A.; Dooley, S.; Dewidar, B.; Giannelli, G.; ten Dijke, P.; IT-LIVER Consortium. TGF-beta signalling and liver disease. FEBS J. 2016, 283, 2219–2232. [Google Scholar] [CrossRef] [PubMed]
- Lo, L.; McLennan, S.V.; Williams, P.F.; Bonner, J.; Chowdhury, S.; McCaughan, G.W.; Gorrell, M.D.; Yue, D.K.; Twigg, S.M. Diabetes is a progression factor for hepatic fibrosis in a high fat fed mouse obesity model of non-alcoholic steatohepatitis. J. Hepatol. 2011, 55, 435–444. [Google Scholar] [CrossRef] [PubMed]
- Koliaki, C.; Szendroedi, J.; Kaul, K.; Jelenik, T.; Nowotny, P.; Jankowiak, F.; Herder, C.; Carstensen, M.; Krausch, M.; Knoefel, W.T.; et al. Adaptation of hepatic mitochondrial function in humans with non-alcoholic fatty liver is lost in steatohepatitis. Cell Metab. 2015, 21, 739–746. [Google Scholar] [CrossRef]
- Sun, K.; Tordjman, J.; Clement, K.; Scherer, P.E. Fibrosis and adipose tissue dysfunction. Cell Metab. 2013, 18, 470–477. [Google Scholar] [CrossRef]
- Marcelin, G.; Gautier, E.L.; Clement, K. Adipose Tissue Fibrosis in Obesity: Etiology and Challenges. Annu. Rev. Physiol. 2022, 84, 135–155. [Google Scholar] [CrossRef] [PubMed]
- Sun, K.; Li, X.; Scherer, P.E. Extracellular Matrix (ECM) and Fibrosis in Adipose Tissue: Overview and Perspectives. Compr. Physiol. 2023, 13, 4387–4407. [Google Scholar] [CrossRef] [PubMed]
- Becic, T.; Studenik, C.; Hoffmann, G. Exercise Increases Adiponectin and Reduces Leptin Levels in Prediabetic and Diabetic Individuals: Systematic Review and Meta-Analysis of Randomized Controlled Trials. Med. Sci. 2018, 6, 97. [Google Scholar] [CrossRef]
- Golbidi, S.; Laher, I. Exercise induced adipokine changes and the metabolic syndrome. J. Diabetes Res. 2014, 2014, 726861. [Google Scholar] [CrossRef] [PubMed]
- Malin, S.K.; Rynders, C.A.; Weltman, J.Y.; Barrett, E.J.; Weltman, A. Exercise Intensity Modulates Glucose-Stimulated Insulin Secretion when Adjusted for Adipose, Liver and Skeletal Muscle Insulin Resistance. PLoS ONE 2016, 11, e0154063. [Google Scholar] [CrossRef]
- Blumer, R.M.; van Roomen, C.P.; Meijer, A.J.; Houben-Weerts, J.H.; Sauerwein, H.P.; Dubbelhuis, P.F. Regulation of adiponectin secretion by insulin and amino acids in 3T3-L1 adipocytes. Metabolism 2008, 57, 1655–1662. [Google Scholar] [CrossRef]
- Tsiloulis, T.; Carey, A.L.; Bayliss, J.; Canny, B.; Meex, R.C.R.; Watt, M.J. No evidence of white adipocyte browning after endurance exercise training in obese men. Int. J. Obes. 2018, 42, 721–727. [Google Scholar] [CrossRef]
- Martinez-Tellez, B.; Sanchez-Delgado, G.; Acosta, F.M.; Alcantara, J.M.A.; Amaro-Gahete, F.J.; Martinez-Avila, W.D.; Merchan-Ramirez, E.; Muñoz-Hernandez, V.; Osuna-Prieto, F.J.; Jurado-Fasoli, L.; et al. No evidence of brown adipose tissue activation after 24 weeks of supervised exercise training in young sedentary adults in the ACTIBATE randomized controlled trial. Nat. Commun. 2022, 13, 5259. [Google Scholar] [CrossRef]

| Parameter | MICT (n = 9) | HIIT (n = 8) | ||
|---|---|---|---|---|
| Pre | Post | Pre | Post | |
| Sex (F/M) | 8/1 | 7/1 | ||
| Age (years) | 36.1 ± 6.7 | 33.3 ± 8.3 | ||
| Height (m) | 1.62 ± 0.08 | 1.65 ± 0.08 | ||
| Weight (kg) | 104 ± 14 | 101 ± 14 * | 109 ± 18 | 107 ± 19 |
| BMI (kg/m2) | 41 ± 4.8 | 38 ± 2.9 * | 40 ± 6.6 | 39 ± 6.8 |
| Fat mass (%) | 48 ± 3.1 | 46 ± 3.2 * | 46 ± 6.5 | 48 ± 4.6 |
| Muscle mass (%) | 29 ± 1.8 | 30 ± 1.9 * | 29 ± 3.1 | 29 ± 2.7 |
| Waist circumference (cm) | 114 ± 13 | 110 ± 14 * | 124 ± 16 | 117 ± 17 * |
| Hip circumference (cm) | 124 ± 7 | 121 ± 4 | 129 ± 8 | 126 ± 9 * |
| Waist-to-hip ratio | 0.92 ± 0.09 | 0.90 ± 0.10 | 0.96 ± 0.08 | 0.93 ± 0.08 * |
| Waist-to-height ratio | 0.71 ± 0.08 | 0.68 ± 0.08 * | 0.75 ± 0.11 | 0.71 ± 0.11 * |
| Spontaneous physical activity (MET × min × week) | 1189 ± 754 | 1984 ± 883 | 934 ± 791 | 2039 ± 1221 |
| Sitting hours per day (n) | 5.5 ± 2.8 | 4.9 ± 2.4 | 5.8 ± 3.3 | 4.8 ± 1.7 |
| Grip strength (kg) | 33.7 ± 7.1 | 34.1 ± 7.3 | 30.5 ± 6.4 | 30.6 ± 5.4 |
Comorbidities (n)
| ||||
| 2 | 3 | |||
| 2 | 2 | |||
| 3 | 2 | |||
| 0 | 0 | |||
| 1 | 1 | |||
| 0 | 1 | |||
| 4 | 4 | |||
| MICT (n = 9) | HIIT (n = 8) | |||
|---|---|---|---|---|
| Parameter | Pre | Post | Pre | Post |
| Cholesterol (mg/dL) | 177 ± 22 | 170 ± 22 | 183 ± 51 | 185 ± 55 |
| Triglycerides (mg/dL) | 126 ± 52 | 144 ± 68 | 148 ± 123 | 118 ± 63 |
| HDL (mg/dL) | 40 ± 12 | 38 ± 12 | 47 ± 10 | 47 ± 10 |
| LDL (mg/dL) | 112 ± 24 | 103 ± 23 | 112 ± 40 | 114 ± 41 |
| VLDL (mg/dL) | 25 ± 10 | 29 ± 14 | 30 ± 24 | 23 ± 13 |
| No-HDL (mg/dL) | 138 ± 23 | 132 ± 14 | 136 ± 49 | 138 ± 51 |
| Albumin (g/dL) | 4.3 ± 0.19 | 4.3 ± 0.17 | 4.3 ± 0.20 | 4.4 ± 0.22 |
| Uric acid (mg/dL) | 5.2 ± 1.5 | 5.2 ± 1.5 | 4.6 ± 1.4 | 4.5 ± 1.0 |
| Creatinine (mg/dL) | 0.74 ± 0.11 | 0.82 ± 0.12 * | 0.77 ± 0.11 | 0.77 ± 0.14 |
| Urea (mg/dL) | 27 ± 7 | 36 ± 12 * | 27 ± 8 | 26 ± 7 |
| Blood uric nitrogen (mg/dL) | 12 ± 3.3 | 17 ± 5.6 * | 13 ± 3.8 | 12 ± 3.0 |
| GOT (UI/L) | 22 ± 6.3 | 31 ± 36 | 21 ± 6.8 | 23 ± 10 |
| GPT (UI/L) | 29 ± 11 | 46 ± 51 | 29 ± 14 | 33 ± 20 |
| Fasting blood glucose (mg/dL) | 98 ± 11 | 98 ± 10 | 93 ± 14 | 94 ± 11 |
| Fasting insulin (µUI/mL) | 19 ± 8 | 21 ± 16 | 20 ± 10 | 18 ± 7 |
| HOMA-IR | 4.6 ± 1.8 | 5.3 ± 4.5 | 4.7 ± 2.4 | 4.1 ± 1.6 |
| HbA1c (%) | 5.6 ± 0.6 | 5.5 ± 0.5 | 5.5 ± 0.4 | 5.4 ± 0.4 * |
| TSH (µUI/mL) | 2.3 ± 1.7 | 2.7 ± 1.5 | 2.4 ± 1.6 | 2.2 ± 1.2 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ruíz-Uribe, M.; Enríquez-Schmidt, J.; Monrroy-Uarac, M.; Mautner-Molina, C.; Kalazich-Rosales, M.; Muñoz, M.; Fuentes-Leal, F.; Cárcamo-Ibaceta, C.; Fazakerley, D.J.; Larance, M.; et al. Moderate-Intensity Constant and High-Intensity Interval Training Confer Differential Metabolic Benefits in Skeletal Muscle, White Adipose Tissue, and Liver of Candidates to Undergo Bariatric Surgery. J. Clin. Med. 2024, 13, 3273. https://doi.org/10.3390/jcm13113273
Ruíz-Uribe M, Enríquez-Schmidt J, Monrroy-Uarac M, Mautner-Molina C, Kalazich-Rosales M, Muñoz M, Fuentes-Leal F, Cárcamo-Ibaceta C, Fazakerley DJ, Larance M, et al. Moderate-Intensity Constant and High-Intensity Interval Training Confer Differential Metabolic Benefits in Skeletal Muscle, White Adipose Tissue, and Liver of Candidates to Undergo Bariatric Surgery. Journal of Clinical Medicine. 2024; 13(11):3273. https://doi.org/10.3390/jcm13113273
Chicago/Turabian StyleRuíz-Uribe, Matías, Javier Enríquez-Schmidt, Manuel Monrroy-Uarac, Camila Mautner-Molina, Mariana Kalazich-Rosales, Maximiliano Muñoz, Francisca Fuentes-Leal, Carlos Cárcamo-Ibaceta, Daniel J. Fazakerley, Mark Larance, and et al. 2024. "Moderate-Intensity Constant and High-Intensity Interval Training Confer Differential Metabolic Benefits in Skeletal Muscle, White Adipose Tissue, and Liver of Candidates to Undergo Bariatric Surgery" Journal of Clinical Medicine 13, no. 11: 3273. https://doi.org/10.3390/jcm13113273
APA StyleRuíz-Uribe, M., Enríquez-Schmidt, J., Monrroy-Uarac, M., Mautner-Molina, C., Kalazich-Rosales, M., Muñoz, M., Fuentes-Leal, F., Cárcamo-Ibaceta, C., Fazakerley, D. J., Larance, M., Ehrenfeld, P., & Martínez-Huenchullán, S. (2024). Moderate-Intensity Constant and High-Intensity Interval Training Confer Differential Metabolic Benefits in Skeletal Muscle, White Adipose Tissue, and Liver of Candidates to Undergo Bariatric Surgery. Journal of Clinical Medicine, 13(11), 3273. https://doi.org/10.3390/jcm13113273







