A Systematic Review to Evaluate the Barriers to Breast Cancer Screening in Women with Disability
Abstract
1. Introduction
2. Material and Methodology
2.1. Data Source and Search Strategy
2.2. Study Selection Criteria
2.3. Data Extraction and Quality Assessment
3. Results
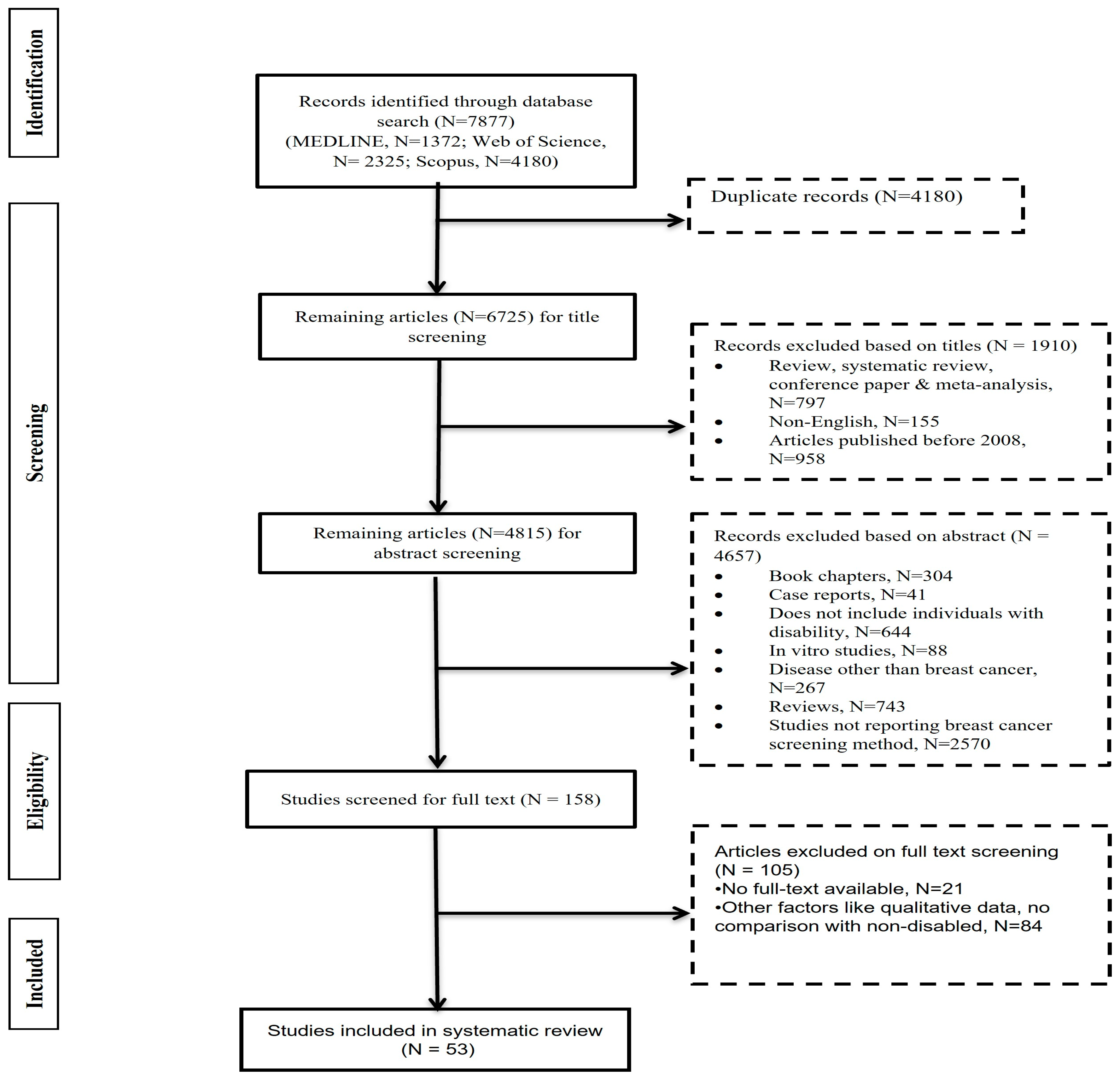
3.1. Search and Study Selection
3.2. Study Characteristics
3.3. Methodological Quality
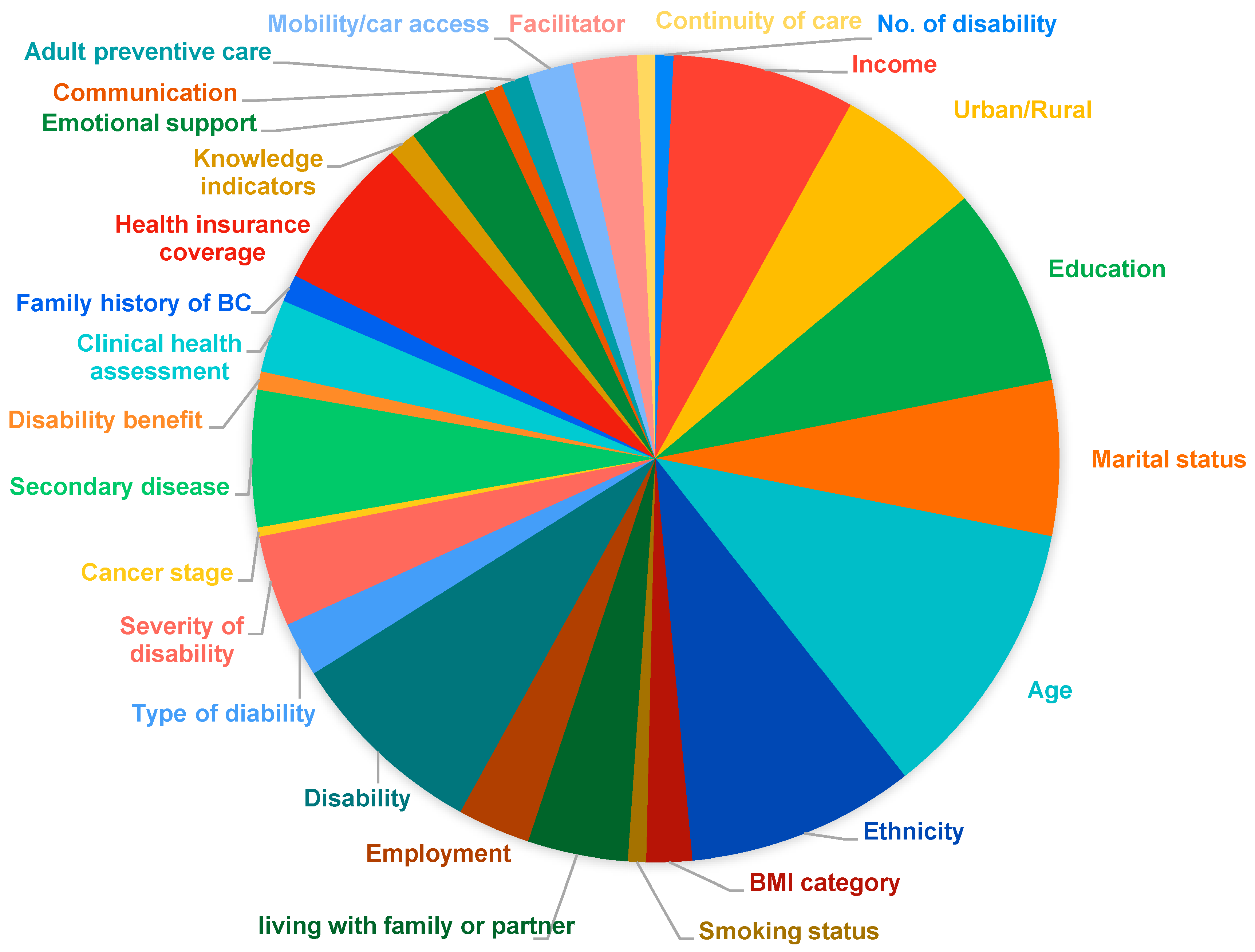
3.4. Risk Factors Associated with Breast Cancer Screening in Patients with Disability
4. Discussion
Supplementary Materials
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Torre, L.A.; Bray, F.; Siegel, R.L.; Ferlay, J.; Lortet-Tieulent, J.; Jemal, A. Global cancer statistics, 2012. CA Cancer J. Clin. 2015, 65, 87–108. [Google Scholar] [CrossRef] [PubMed]
- Mandelblatt, J.S.; Stout, N.K.; Schechter, C.B.; Van Den Broek, J.J.; Miglioretti, D.L.; Krapcho, M.; Trentham-Dietz, A.; Munoz, D.; Lee, S.J.; Berry, D.A.; et al. Collaborative modeling of the benefits and harms associated with different US breast cancer screening strategies. Ann. Intern. Med. 2016, 164, 215–225. [Google Scholar] [CrossRef] [PubMed]
- Gangnon, R.E.; Sprague, B.L.; Stout, N.K.; Alagoz, O.; Weedon-Fekjær, H.; Holford, T.R.; Trentham-Dietz, A. The contribution of mammography screening to breast cancer incidence trends in the United States: An updated age–period–cohort model. Cancer Epidemiol. Biomarkers Prev. 2015, 24, 905–912. [Google Scholar] [CrossRef] [PubMed]
- Nelson, H.D.; Fu, R.; Cantor, A.; Pappas, M.; Daeges, M.; Humphrey, L. Effectiveness of breast cancer screening: Systematic review and meta-analysis to update the 2009 US Preventive Services Task Force recommendation. Ann. Intern. Med. 2016, 164, 244–255. [Google Scholar] [CrossRef]
- Damiani, G.; Federico, B.; Basso, D.; Ronconi, A.; Bianchi, C.B.N.A.; Anzellotti, G.M.; Nasi, G.; Sassi, F.; Ricciardi, W. Socioeconomic disparities in the uptake of breast and cervical cancer screening in Italy: A cross-sectional study. BMC Public Health 2012, 12, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Casebolt, M.T. Barriers to reproductive health services for women with disability in low-and middle-income countries: A review of the literature. Sex. Reprod. Healthc. 2020, 24, 100485. [Google Scholar] [CrossRef] [PubMed]
- Chan, D.N.; Law, B.M.; Au, D.W.; So, W.K.; Fan, N. A systematic review of the barriers and facilitators influencing the cancer screening behaviour among people with intellectual disabilities. Cancer Epidemiol. 2022, 76, 102084. [Google Scholar] [CrossRef] [PubMed]
- Inchai, P.; Tsai, W.C.; Chiu, L.T.; Kung, P.T. Inequality in the utilization of breast cancer screening between women with and without disabilities in Taiwan: A propensity-score-matched nationwide cohort study. Int. J. Environ. Res. Public Health 2022, 19, 5280. [Google Scholar] [CrossRef] [PubMed]
- Ross, E.; Maguire, A.; Donnelly, M.; Mairs, A.; Hall, C.; O’Reilly, D. Disability as a predictor of breast cancer screening uptake: A population-based study of 57,328 women. J. Med. Screen. 2020, 27, 194–200. [Google Scholar] [CrossRef]
- Floud, S.; Barnes, I.; Verfürden, M.; Kuper, H.; Gathani, T.; Blanks, R.G.; Alison, R.; Patnick, J.; Beral, V.; Green, J.; et al. Disability and participation in breast and bowel cancer screening in England: A large prospective study. Br. J. Cancer 2017, 117, 1711–1714. [Google Scholar] [CrossRef]
- Steele, C.B.; Townsend, J.S.; Courtney-Long, E.A.; Young, M. Peer reviewed: Prevalence of cancer screening among adults with disabilities, United States, 2013. Prev. Chronic Dis. 2017, 14, E09. [Google Scholar] [CrossRef] [PubMed]
- Pichetti, S.; Penneau, A.; Lengagne, P.; Sermet, C. Access to care and prevention for people with disabilities in France: Analysis based on data from the 2008 French health and disabilities households surveys (Handicap-Sante-Menages). Rev. Epidemiol. Sante. Publique. 2016, 64, 79–94. [Google Scholar] [CrossRef]
- Zha, N.; Alabousi, M.; Patel, B.K.; Patlas, M.N. Beyond universal health care: Barriers to breast cancer screening participation in Canada. J. Am. Coll. Radiol. 2019, 16, 570–579. [Google Scholar] [CrossRef] [PubMed]
- Centers of Disease Control and Prevention. Available online: https://www.cdc.gov/ncbddd/disabilityandhealth/righttoknow/overview.html#:~:text=What%20Is%20The%20Right%20To,have%20ever%20received%20a%20mammogram (accessed on 9 April 2024).
- Peters, K.; Cotton, A. Barriers to breast cancer screening in Australia: Experiences of women with physical disabilities. J. Clin. Nurs. 2015, 24, 563–572. [Google Scholar] [CrossRef]
- Net, J.M.; Feliciano, Y.Z.; Podsiadlo, V.; Dialani, V.; Grimm, L.J. Optimizing the Patient Experience for Women With Disabilities in the Breast Imaging Clinic. J. Breast Imaging 2024, 6, 183–191. [Google Scholar] [CrossRef]
- Welch Saleeby, P.; Hunter-Jones, J. Identifying barriers and facilitators to breast health services among women with disabilities. Soc. Work Public Health 2016, 31, 255–263. [Google Scholar] [CrossRef] [PubMed]
- Moher, D.; Shamseer, L.; Clarke, M.; Ghersi, D.; Liberati, A.; Petticrew, M.; Paul, S.; Stewart, L.A.; PRISMA-P Group. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst. Rev. 2015, 4, 1–9. [Google Scholar] [CrossRef]
- Brooke, B.S.; Schwartz, T.A.; Pawlik, T.M. MOOSE reporting guidelines for meta-analyses of observational studies. JAMA Surg. 2021, 156, 787–788. [Google Scholar] [CrossRef]
- Harms, M. Medline. Physiotherapy 2009, 95, 149–150. [Google Scholar] [CrossRef]
- Wells, G.A.; Shea, B.; O’Connell, D.; Peterson, J.; Welch, V.; Losos, M.; Tugwell, P. The Newcastle-Ottawa Scale (NOS) For Assessing the Quality of Nonrandomised Studies in Meta-Analyses. 2000. Available online: https://www.ohri.ca/programs/clinical_epidemiology/oxford.asp (accessed on 5 July 2000).
- Parish, S.L.; Swaine, J.G.; Luken, K.; Rose, R.A.; Dababnah, S. Cervical and breast cancer–screening knowledge of women with developmental disabilities. Intellect. Dev. Disabil. 2012, 50, 79–91. [Google Scholar] [CrossRef]
- Zhang, D.; Abraham, L.; Demb, J.; Miglioretti, D.L.; Advani, S.; Sprague, B.L.; Henderson, L.M.; Onega, T.; Wernli, K.J.; Walter, L.C.; et al. Function-related indicators and outcomes of screening mammography in older women: Evidence from the Breast Cancer Surveillance Consortium Cohort. Cancer Epidemiol. Biomarkers Prev. 2021, 30, 1582–1590. [Google Scholar] [CrossRef]
- Trétarre, B.; Bourgarel, S.; Stoebner-Delbarre, A.; Jacot, W.; Bessaoud, F.; Satge, D. Breast cancer and screening in persons with an intellectual disability living in institutions in France. J. Intellect. Disabil. Res. 2017, 61, 266–278. [Google Scholar] [CrossRef] [PubMed]
- Alagoz, O.; Hajjar, A.; Chootipongchaivat, S.; van Ravesteyn, N.T.; Yeh, J.M.; Ergun, M.A.; de Koning, H.J.; Chicoine, B.; Martin, B. Benefits and harms of mammography screening for women with Down syndrome: A collaborative modeling study. J. Gen. Intern. Med. 2019, 34, 2374–2381. [Google Scholar] [CrossRef]
- Xu, X.; Mann, J.R.; Hardin, J.W.; Gustafson, E.; McDermott, S.W.; Deroche, C.B. Adherence to US Preventive Services Task Force recommendations for breast and cervical cancer screening for women who have a spinal cord injury. J. Spinal Cord Med. 2017, 40, 76–84. [Google Scholar] [CrossRef]
- Parish, S.L.; Rose, R.A.; Luken, K.; Swaine, J.G.; O’Hare, L. Cancer screening knowledge changes: Results from a randomized control trial of women with developmental disabilities. Res. Soc. Work. Pract. 2012, 22, 43–53. [Google Scholar] [CrossRef]
- Caban, M.; Kuo, Y.F.; Raji, M.; Tan, A.; Freeman, J. Predictors of mammography use in older women with disability: The patients’ perspectives. Med. Oncol. 2011, 28, 8–14. [Google Scholar] [CrossRef] [PubMed]
- Horsbøl, T.A.; Michelsen, S.I.; Lassen, T.H.; Juel, K.; Bigaard, J.; Hoei-Hansen, C.E.; Vejborg, I.; Thygesen, L.C. Breast cancer screening among women with intellectual disability in Denmark. JAMA Netw. Open 2023, 6, e2248980. [Google Scholar] [CrossRef]
- Andiwijaya, F.R.; Davey, C.; Bessame, K.; Ndong, A.; Kuper, H. Disability and participation in breast and cervical cancer screening: A systematic review and meta-analysis. Int. J. Environ. Res. Public Health 2022, 19, 9465. [Google Scholar] [CrossRef]
- Glover, G.; Christie, A.; Hatton, C. Access to cancer screening by people with learning disabilities in England 2012/13: Information from the Joint Health and Social Care Assessment Framework. Tizard Learn. Disabil. Rev. 2014, 19, 194–198. [Google Scholar] [CrossRef]
- Son, E.; Parish, S.L.; Swaine, J.G.; Luken, K. Accuracy of self-reported cervical and breast cancer screening by women with intellectual disability. Am. J. Intellect. Dev. Disabil. 2013, 118, 327–336. [Google Scholar] [CrossRef]
- Paraska, K. Relationship between expanded health belief model variables and mammography screening adherence in women with multiple sclerosis: A pilot study. Int. J. MS Care 2012, 14, 142–147. [Google Scholar] [CrossRef] [PubMed]
- Iezzoni, L.I.; Rao, S.R.; Agaronnik, N.D.; El-Jawahri, A. Associations between disability and breast or cervical cancers, accounting for screening disparities. Med. Care 2021, 59, 139–147. [Google Scholar] [CrossRef] [PubMed]
- Arana, E.; Carroll-Scott, A.; Massey, P.M.; Lee, N.L.; Klassen, A.C.; Yudell, M. Racial/ethnic disparities in mammogram frequency among women with intellectual disability. Intellect. Dev. Disabil. 2019, 57, 177–187. [Google Scholar] [CrossRef] [PubMed]
- Horner-Johnson, W.; Dobbertin, K.; Andresen, E.M.; Iezzoni, L.I. Breast and cervical cancer screening disparities associated with disability severity. Women's Health Issues 2014, 24, e147–e153. [Google Scholar] [CrossRef]
- Merten, J.W.; Pomeranz, J.L.; King, J.L.; Moorhouse, M.; Wynn, R.D. Barriers to cancer screening for people with disabilities: A literature review. Disabil. Health J. 2015, 8, 9–16. [Google Scholar] [CrossRef] [PubMed]
- Keegan, G.; Rizzo, J.R.; Joseph, K.A. Disparities in breast cancer among patients with disabilities: Care gaps, accessibility, and best practices. J. Natl. Cancer Inst. 2023, 115, 1139–1144. [Google Scholar] [CrossRef] [PubMed]
- Sarkeala, T.; Heinävaara, S.; Anttila, A. Breast cancer mortality with varying invitational policies in organised mammography. Br. J. Cancer 2008, 98, 641–645. [Google Scholar] [CrossRef]
- Government of the Republic of Korea. Act on the Prohibition of Discrimination Against Disabled Persons, Remedy Against Infringement of their Rights (Korean Law). Available online: https://www.un.org/development/desa/disabilities/wp-content/uploads/sites/15/2019/11/Korea-Republic-of_Act-on-the-Prohibition-of-Discrimination-of-Disabled-Persons-Remedy-Against-Infringement-of-their-Rights-etc.pdf (accessed on 9 April 2024).
- Iezzoni, L.I.; Kurtz, S.G.; Rao, S.R. Trends in mammography over time for women with and without chronic disability. J. Women's Health 2015, 24, 593–601. [Google Scholar] [CrossRef]
- Todd, A.; Stuifbergen, A. Breast cancer screening barriers and disability. Rehabil. Nurs. J. 2012, 37, 74–79. [Google Scholar] [CrossRef]
- Nuche-Berenguer, B.; Sakellariou, D. Socioeconomic Determinants of Participation in Cancer Screening in Argentina: A Cross-Sectional Study. Front. Public Health 2021, 9, 699108. [Google Scholar] [CrossRef]
- Shin, D.W.; Yu, J.; Cho, J.; Lee, S.K.; Jung, J.H.; Han, K.; Kim, S.Y.; Yoo, J.E.; Yeob, K.E.; Kim, Y.Y.; et al. Breast cancer screening disparities between women with and without disabilities: A national database study in South Korea. Cancer 2020, 126, 1522–1529. [Google Scholar] [CrossRef] [PubMed]
- Groß, S.E.; Pfaff, H.; Swora, M.; Ansmann, L.; Albert, U.S.; Groß-Kunkel, A. Health disparities among breast cancer patients with/without disabilities in Germany. Disabil. Health J. 2020, 13, 100873. [Google Scholar] [CrossRef] [PubMed]
- Nandam, N.; Gaebler-Spira, D.; Byrne, R.; Wolfman, J.; Reis, J.P.; Hung, C.W.; Todd, A.; Durkin, J.; Marciniak, C. Breast cancer screening in women with cerebral palsy: Could care delivery be improved? Disabil. Health J. 2018, 11, 435–441. [Google Scholar] [CrossRef] [PubMed]
- Fujiwara, M.; Inagaki, M.; Nakaya, N.; Fujimori, M.; Higuchi, Y.; Hayashibara, C.; So, R.; Kakeda, K.; Kodama, M.; Uchitomi, Y.; et al. Cancer screening participation in schizophrenic outpatients and the influence of their functional disability on the screening rate: A cross-sectional study in Japan. Psychiatry Clin. Neurosci. 2017, 71, 813–825. [Google Scholar] [CrossRef]
- Xu, X.; McDermott, S.W.; Mann, J.R.; Hardin, J.W.; Deroche, C.B.; Carroll, D.D.; Courtney-Long, E.A. A longitudinal assessment of adherence to breast and cervical cancer screening recommendations among women with and without intellectual disability. Prev. Med. 2017, 100, 167–172. [Google Scholar] [CrossRef] [PubMed]
- Yen, S.M.; Kung, P.T.; Tsai, W.C. Mammography usage with relevant factors among women with mental disabilities in Taiwan: A nationwide population-based study. Res. Dev. Disabil. 2015, 37, 182–188. [Google Scholar] [CrossRef]
- Bussière, C.; Sicsic, J.; Pelletier-Fleury, N. The effects of obesity and mobility disability in access to breast and cervical cancer screening in france: Results from the national health and disability survey. PLoS ONE 2014, 9, e104901. [Google Scholar] [CrossRef]
- Guilcher, S.J.; Lofters, A.; Glazier, R.H.; Jaglal, S.B.; Voth, J.; Bayoumi, A.M. Level of disability, multi-morbidity and breast cancer screening: Does severity matter? Prev. Med. 2014, 67, 193–198. [Google Scholar] [CrossRef]
- Swaine, J.G.; Parish, S.L.; Luken, K.; Son, E.; Dickens, P. Test of an intervention to improve knowledge of women with intellectual disabilities about cervical and breast cancer screening. J. Intellect. Disabil. Res. 2014, 58, 651–663. [Google Scholar] [CrossRef]
- Cobigo, V.; Ouellette-Kuntz, H.; Balogh, R.; Leung, F.; Lin, E.; Lunsky, Y. Are cervical and breast cancer screening programmes equitable? The case of women with intellectual and developmental disabilities. J. Intellect. Disabil. Res. 2013, 57, 478–488. [Google Scholar] [CrossRef]
- Parish, S.L.; Swaine, J.G.; Son, E.; Luken, K. Receipt of mammography among women with intellectual disabilities: Medical record data indicate substantial disparities for African American women. Disabil. Health J. 2013, 6, 36–42. [Google Scholar] [CrossRef] [PubMed]
- Osborn, D.P.; Horsfall, L.; Hassiotis, A.; Petersen, I.; Walters, K.; Nazareth, I. Access to cancer screening in people with learning disabilities in the UK: Cohort study in the health improvement network, a primary care research database. PLoS ONE 2012, 7, e43841. [Google Scholar] [CrossRef] [PubMed]
- Buckley, D.I.; Davis, M.M.; Andresen, E.M. Does a standard measure of self-reported physical disability correlate with clinician perception of impairment related to cancer screening? Cancer 2012, 118, 1345–1352. [Google Scholar] [CrossRef] [PubMed]
- Weir, S.; Posner, H.E.; Zhang, J.; Jones, W.C.; Willis, G.; Baxter, J.D.; Clark, R.E. Disparities in routine breast cancer screening for Medicaid managed care members with a work-limiting disability. Medicare Medicaid Res. Rev. 2011, 1, 001.04.a02. [Google Scholar] [CrossRef] [PubMed]
- Kung, P.T.; Tsai, W.C.; Chiou, S.J. The assessment of the likelihood of mammography usage with relevant factors among women with disabilities. Res. Dev. Disabil. 2012, 33, 136–143. [Google Scholar] [CrossRef] [PubMed]
- Wilkinson, J.E.; Lauer, E.; Freund, K.M.; Rosen, A.K. Determinants of mammography in women with intellectual disabilities. J. Am. Board. Fam. Med. 2011, 24, 693–703. [Google Scholar] [CrossRef] [PubMed]
- Courtney-Long, E.; Armour, B.; Frammartino, B.; Miller, J. Factors associated with self-reported mammography use for women with and women without a disability. J. Women’s Health 2011, 20, 1279–1286. [Google Scholar] [CrossRef]
- Todd, A.; Stuifbergen, A. Barriers and Facilitators to Breast Cancer Screening: A Qualitative Study of Women with Multiple Sclerosis. Int. J. MS Care 2011, 13, 49–56. [Google Scholar] [CrossRef]
- Clark, M.A.; Rogers, M.L.; Wen, X.; Wilcox, V.; McCarthy-Barnett, K.; Panarace, J.; Manning, C.; Allen, S.; Rakowski, W. Repeat mammography screening among unmarried women with and without a disability. Womens Health Issues 2009, 19, 415–424. [Google Scholar] [CrossRef]
- Darcey, E.; Ambati, R.; Lund, H.; Redfern, A.; Saunders, C.; Thompson, S.; Wylie, E.; Stone, J. Measuring height and weight as part of routine mammographic screening for breast cancer. J. Med. Screen. 2019, 26, 204–211. [Google Scholar] [CrossRef]
- Sakellariou, D.; Rotarou, E.S. Utilisation of mammography by women with mobility impairment in the UK: Secondary analysis of cross-sectional data. BMJ Open 2019, 9, e024571. [Google Scholar] [CrossRef]
- Plourde, N.; Brown, H.K.; Vigod, S.; Cobigo, V. The Association Between Continuity of Primary Care and Preventive Cancer Screening in Women With Intellectual Disability. Am. J. Intellect. Dev. Disabil. 2018, 123, 499–513. [Google Scholar] [CrossRef] [PubMed]
- Sakellariou, D.; Rotarou, E.S. Utilisation of cancer screening services by disabled women in Chile. PLoS ONE 2017, 12, e0176270. [Google Scholar] [CrossRef]
- Yankaskas, B.C.; Dickens, P.; Bowling, J.M.; Jarman, M.P.; Luken, K.; Salisbury, K.; Halladay, J.; Lorenz, C.E. Barriers to adherence to screening mammography among women with disabilities. Am. J. Public Health 2010, 100, 947–953. [Google Scholar] [CrossRef] [PubMed]
- Reidy, M.; Denieffe, S.; Foran, S. Exploring breast cancer and screening awareness among Irish women with intellectual disabilities. Br. J. Learn. Disabil. 2018, 46, 193–201. [Google Scholar] [CrossRef]
- Kerrison, R.S.; Jones, A.; Peng, J.; Price, G.; Verne, J.; Barley, E.A.; Lugton, C. Inequalities in cancer screening participation between adults with and without severe mental illness: Results from a cross-sectional analysis of primary care data on English Screening Programmes. Br. J. Cancer 2023, 129, 81–93. [Google Scholar] [CrossRef]
- Pearson, J.; Payne, D.; Yoshida, K.; Garrett, N. Access to and engagement with cervical and breast screening services for women with disabilities in Aotearoa New Zealand. Disabil. Rehabil. 2022, 44, 1984–1995. [Google Scholar] [CrossRef]
- Yang, S.; Bian, J.; George, T.J.; Daily, K.; Zhang, D.; Braithwaite, D.; Guo, Y. The association between cognitive impairment and breast and colorectal cancer screening utilization. BMC Cancer 2021, 21, 539. [Google Scholar] [CrossRef]
- Murphy, K.A.; Daumit, G.L.; Bandara, S.N.; Stone, E.M.; Kennedy-Hendricks, A.; Stuart, E.A.; Pollack, C.E.; McGinty, E.E. Association Between the Maryland Medicaid Behavioral Health Home Program and Cancer Screening in People With Serious Mental Illness. Psychiatr Serv. 2020, 71, 608–611. [Google Scholar] [CrossRef]
- Kushalnagar, P.; Engelman, A.; Simons, A.N. Deaf Women's Health: Adherence to Breast and Cervical Cancer Screening Recommendations. Am. J. Prev. Med. 2019, 57, 346–354. [Google Scholar] [CrossRef]
- Xu, X.; Mann, J.R.; McDermott, S.W.; Deroche, C.B.; Gustafson, E.; Hardin, J.W. Women with Visual Impairment and Insured by Medicaid or Medicare Are Less Likely to Receive Recommended Screening for Breast and Cervical Cancers. Ophthalmic Epidemiol. 2017, 24, 168–173. [Google Scholar] [CrossRef] [PubMed]
- Horner-Johnson, W.; Dobbertin, K.; Iezzoni, L.I. Disparities in receipt of breast and cervical cancer screening for rural women age 18 to 64 with disabilities. Women’s Health Issues 2015, 25, 246–253. [Google Scholar] [CrossRef] [PubMed]
- Sanz-Barbero, B.; Sopacua, M.; Otero-García, L.; Borda-Olivas, A.; Zunzunegui, M.V. Inequalities in the use of mammography in Spain: Effect of caring for disabled family. Int. J. Public Health 2012, 57, 953–957. [Google Scholar] [CrossRef] [PubMed]
- Liu, S.Y.; Clark, M.A. Breast and cervical cancer screening practices among disabled women aged 40–75: Does quality of the experience matter? J. Women’s Health 2008, 17, 1321–1329. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Almohammed, H.I. A Systematic Review to Evaluate the Barriers to Breast Cancer Screening in Women with Disability. J. Clin. Med. 2024, 13, 3283. https://doi.org/10.3390/jcm13113283
Almohammed HI. A Systematic Review to Evaluate the Barriers to Breast Cancer Screening in Women with Disability. Journal of Clinical Medicine. 2024; 13(11):3283. https://doi.org/10.3390/jcm13113283
Chicago/Turabian StyleAlmohammed, Huda I. 2024. "A Systematic Review to Evaluate the Barriers to Breast Cancer Screening in Women with Disability" Journal of Clinical Medicine 13, no. 11: 3283. https://doi.org/10.3390/jcm13113283
APA StyleAlmohammed, H. I. (2024). A Systematic Review to Evaluate the Barriers to Breast Cancer Screening in Women with Disability. Journal of Clinical Medicine, 13(11), 3283. https://doi.org/10.3390/jcm13113283





