Abstract
Background: We aimed to assess the effectiveness and safety of transcatheter arterial embolization (TAE) in the management of spontaneous or traumatic psoas and/or retroperitoneal hemorrhage. Methods: This single-center retrospective study enrolled 36 patients who underwent TAE for the treatment of psoas and/or retroperitoneal hemorrhage between May 2016 and February 2024. Results: The patients’ mean age was 61.3 years. The spontaneous group (SG, 47.1%) showed higher rates of anticoagulation therapy use compared with the trauma group (TG, 15.8%) (p = 0.042). The TG (94.7%) demonstrated higher survival rates compared with the SG (64.7%; p = 0.023). Clinical failure was significantly associated with the liver cirrhosis (p = 0.001), prothrombin time (p = 0.004), and international normalized ratio (p = 0.007) in SG and pRBC transfusion (p = 0.008) in TG. Liver cirrhosis (OR (95% CI): 55.055 (2.439–1242.650), p = 0.012) was the only identified independent risk factor for primary clinical failure in the multivariate logistic regression analysis. Conclusions: TAE was a safe and effective treatment for psoas and/or retroperitoneal hemorrhage, regardless of the cause of bleeding. However, liver cirrhosis or the need for massive transfusion due to hemorrhage increased the risk of clinical failure and mortality, necessitating aggressive monitoring and treatment.
1. Introduction
Psoas and retroperitoneal hemorrhages are critical medical conditions characterized by hypotension, abdominal/flank tenderness, and sensorimotor deficits, often secondary to nerve compression by a retroperitoneal hematoma [1,2]. Spontaneous retroperitoneal hemorrhage (SRH) occurs without an incident cause and predominantly affects elderly patients receiving anticoagulation therapy. Despite its rarity, SRH is associated with a high mortality rate, reaching up to 22% as reported [3,4,5]. Patients with this condition often present with multiple comorbidities that complicate their management.
Additionally, retroperitoneal hemorrhage can result from traumatic or iatrogenic injuries [6]. The complexity of managing retroperitoneal hemorrhage following blunt trauma is often accompanied by multiple traumatic injuries. This underscores the need for a nuanced treatment approach that takes into account the unique etiologies and patient factors involved [7]. However, the transcatheter arterial embolization (TAE) as a minimally invasive endovascular treatment option has shifted the treatment paradigm, particularly for patients who exhibit hemodynamic instability despite receiving the aforementioned conservative measures [3,4,5,8,9,10].
Our study evaluated the effectiveness and safety of TAE in managing bleeding due to trauma or spontaneous events in patients with psoas and/or retroperitoneal space. By assessing the efficacy of TAE and determining the factors that affect clinical outcomes, this study aimed to provide significant insights into the development of optimal strategies for addressing this complex and potentially critical condition.
2. Materials and Methods
This retrospective single-center study was approved by the institutional review board of Ewha Womans University (IRB No. EUMC 2024-03-040), which waived the need for obtaining informed consent from the patients.
2.1. Patient Population
The information system of the authors’ hospital was retrospectively reviewed between May 2016 and February 2024. All methods were performed in accordance with the relevant guidelines and regulations. A total of 36 consecutive patients (21 men and 15 women) with a mean age of 61.3 years (range: 16–89 years) who underwent TAE as a treatment for psoas or retroperitoneal hemorrhage were enrolled in this study. The patients’ electronic medical records and images were thoroughly examined. The decision to perform TAE was based on computed tomography (CT) findings and clinical and laboratory evidence of continued bleeding despite adequate conservative therapy. Patients aged 10–90 years who underwent TAE owing to a suspicion of active bleeding in the psoas or retroperitoneal space, with or without traumatic injury, were included in this study. The exclusion criteria were trauma patients whose main bleeding site was not in the psoas or retroperitoneal space, like the spleen or liver, and also excluded were those without TAE.
2.2. Procedure
The right common femoral artery was accessed under local anesthesia, and the main target vessels visualized as potential bleeding sources on CT were explored. In addition, all arteries within the same anatomical territory surrounding the hematoma were systematically catheterized to determine other bleeding arteries or blood flow through collaterals from the primary bleeding site. If the hematoma was located in the psoas muscle, selective catheterization and opacification of the iliolumbar and homolateral lumbar arteries were performed. A 1.7- or 1.9-F microcatheter was advanced into all identifiable target vessels, which were subsequently embolized. Embolic agents included polyvinyl alcohol (PVA; Contour; Boston Scientific, Marlborough, MA, USA), n-butyl cyanoacrylate (NBCA; Histoacryl; B. Braun, Melsungen, Germany), detachable vascular microcoils (Interlock; Boston Scientific, Marlborough, MA, USA and Concerto; Medtronic, Minneapolis, MN, USA), and gelatin sponge particles (GSPs; Nexsphere, Next Biomedical, Incheon, Republic of Korea) or their combinations. Embolic materials were selected intraoperatively on a case-by-case basis at the discretion of the interventional radiologist. Subsequently, arteriography after embolization was performed to confirm the successful occlusion of the target vessel with no further bleeding (Figure 1).
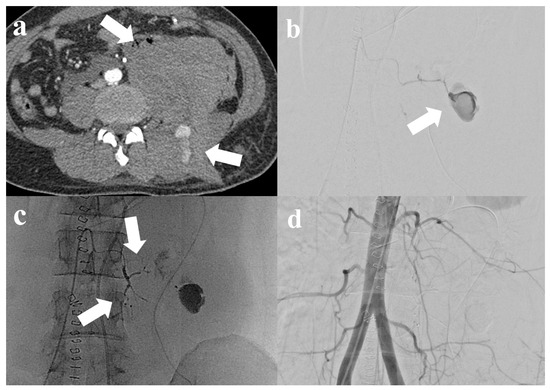
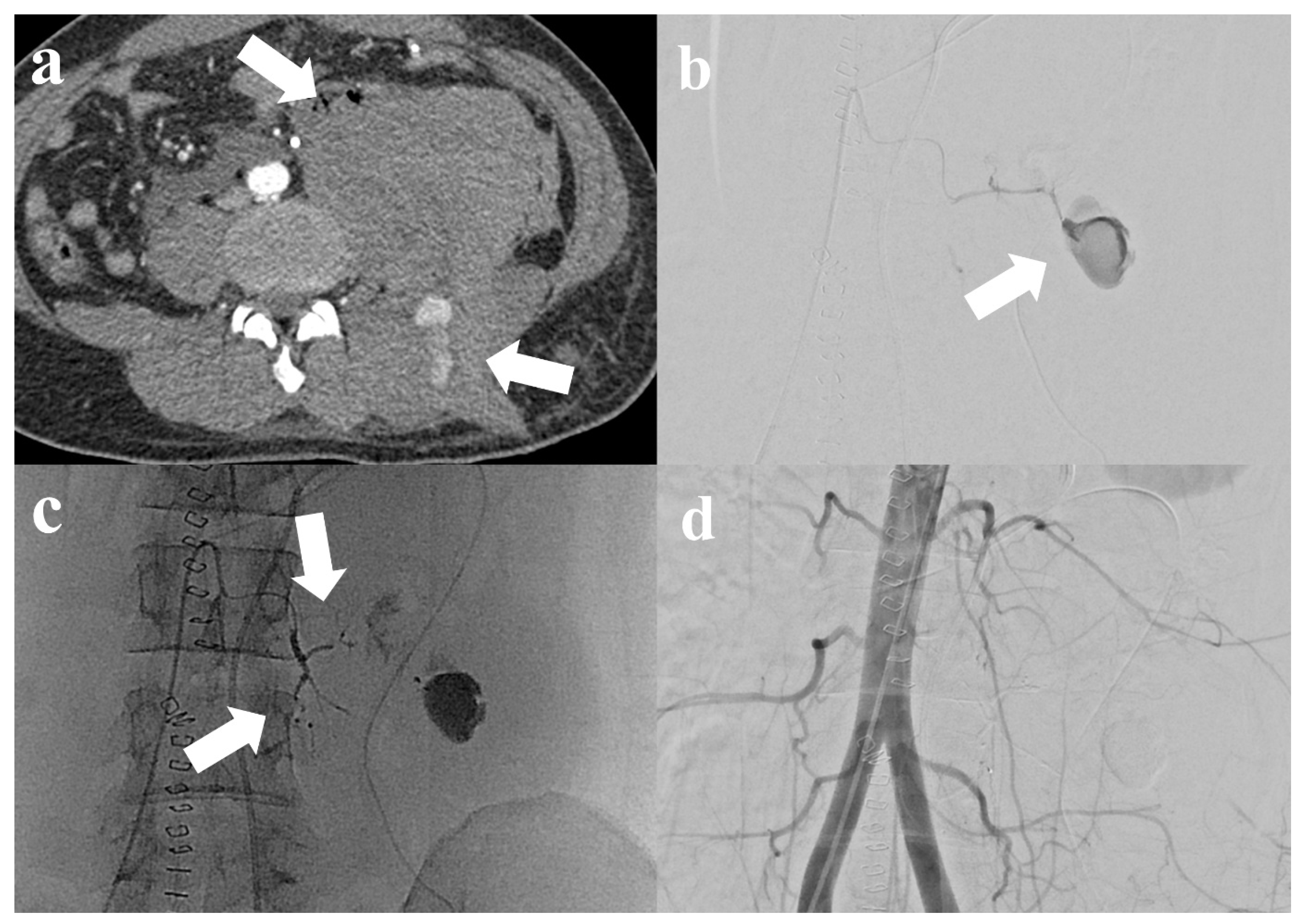
Figure 1.
A 32-year-old male patient with blunt trauma. (a) Computed tomography (CT) shows huge hematoma at left retroperitoneal space and paravertebral space with contrast media extravasation (arrow). (b) Selective left 3rd lumbar artery angiograms show huge pseudoaneurysm (arrow), consistent with CT. (c) Embolization was performed using n-butyl cyanoacrylate at the left 3rd lumbar artery (arrow). (d) After successful embolization, abdominal aortography shows the well-embolized left 3rd lumbar artery without definite residual active bleeding.
2.3. Study Endpoints
Technical success was defined as the complete occlusion of the bleeding vessel and the absence of visible signs of active bleeding, such as contrast media extravasation (CME) or pseudoaneurysm, on immediate post-embolization angiography. Additionally, in cases where CME or pseudoaneurysm was not clearly identifiable on angiography, occlusion was performed on the vessel supplying the same anatomical territory surrounding the hematoma. Primary clinical success was defined as the resolution of the signs and symptoms of bleeding with no requirement for interventional or surgical hemostasis. The complications were classified as either major or minor according to the Society of Interventional Radiology Standards of Practice Committee guidelines [11]. In the present study, the abnormal platelet count (<5 × 104/μL) and/or international normalized ratio (INR > 1.5) indicated coagulopathy as these values require correction through the infusion of platelets or fresh frozen plasma [12,13].
2.4. Statistical Analysis
Categorical variables were compared using the chi-square test or Fisher’s exact test, as appropriate. Continuous variables were expressed as the mean ± standard deviation and were compared using Student’s t-test. A multivariate analysis was performed to identify independent factors using binomial logistic regression. All statistical analyses were performed using SPSS software version 20.0, with a p value of <0.05 indicating statistical significance.
3. Results
The baseline demographic and clinical data of the patients included in this study are outlined in Table 1. Among the study patients, 11 (30.6%) received anticoagulation therapy. On CT scans, CME was identified in 91.7% (33/36) of patients. Among these patients, 69.4% (25/36) showed active bleeding in the form of CME or pseudoaneurysm on angiography. Meanwhile, 52.8% of patients (19/36) experienced bleeding from multiple sites. Technical success was achieved in all patients, with a clinical success rate of 77.8% (28/36) and an overall mortality rate of 19.4% (7/36). In the present study, which compared two groups, the spontaneous group (SG) comprised 17 patients, while the trauma group (TG) comprised 19 patients. The use of oral anticoagulation therapy (p = 0.042), underlying conditions (p < 0.001), multiple bleeding sites (p = 0.047), average systolic blood pressure (p = 0.045), initial hemoglobin levels (p = 0.018), and mortality rate (p = 0.023) were found to be significantly different between the groups.

Table 1.
Overall group comparison between traumatic and spontaneous psoas and/or retroperitoneal hemorrhage in patients treated with transcatheter arterial embolization.
Notably, all five patients with liver cirrhosis experienced clinical failure, while seven patients receiving oral anticoagulation therapy achieved clinical success. Clinical failure occurred in 8 patients, of whom 62.5% (5/8) had underlying liver cirrhosis, while 20.0% (2/8) sustained trauma. Only one patient received anticoagulation therapy. The signs of active bleeding, such as CME or pseudoaneurysm, were observed in all patients on CT scans and in 75.0% (6/8) on angiography. Furthermore, 62.5% (5/8) of patients had bleeding from multiple vessels. The average pre-treatment hemoglobin level was 6.03 ± 0.97 g/dL, while the average number of packed red blood cell (pRBC) units transfused was 5.6 ± 2.8 units. Among the total of eight patients who experienced clinical failure, one patient with neurofibromatosis suffered hemorrhage after a collision. This patient underwent a second session of TAE due to unstable vital signs following the first TAE. During the second session, another arterial bleeding site that had not previously been identified was discovered and successfully embolized, leading to clinical improvement. The remaining seven patients (87.5%) expired (Table 2).

Table 2.
Primary clinical failure after transcatheter arterial embolization in patients with psoas and retroperitoneal hemorrhage.
In 17 SG patients, 6 patients experienced clinical failure. Among the SG patients with liver cirrhosis, there were a total of six patients, five of whom experienced clinical failure (83.3%, p = 0.001). Additionally, prothrombin time (13.5 ± 1.8 vs. 23.4 ± 5.5, p = 0.004) and INR (1.18 ± 0.17 vs. 2.03 ± 0.51, p = 0.007) were statistically significant (Table 3). Among the 19 TG patients, there were 2 cases of clinical failure. Among the variables, only pRBC transfusion was significant (clinical success: 3.65 ± 1.87 vs. clinical failure: 8.00 ± 2.83; p = 0.008) (Table 4).

Table 3.
Clinical outcome in patients with spontaneous psoas and/or retroperitoneal hemorrhage treated with transcatheter arterial embolization.

Table 4.
Clinical outcome in patients with traumatic psoas and/or retroperitoneal hemorrhage treated with transcatheter arterial embolization.
The univariate logistic regression analysis demonstrated that liver cirrhosis (OR (95% CI): 43.333 (3.712–505.806), p = 0.003), hemoglobin levels (OR (95% CI): 12.600 (1.350–117.570), p = 0.026), and pRBC transfusion (OR (95% CI): 1.459 (1.024–2.078), p = 0.037) were risk factors associated with primary clinical failure in patients with psoas and/or retroperitoneal hemorrhage. However, liver cirrhosis (OR (95% CI): 55.055 (2.439–1242.650), p = 0.012) was the only identified independent risk factor for primary clinical failure in the multivariate logistic regression analysis (Table 5).

Table 5.
Multivariable logistic regression analysis of independent factors for primary clinical failure in all patients with psoas and retroperitoneal hemorrhage.
One patient developed motor weakness in the ipsilateral lower extremity after TAE. The patient experienced left spontaneous psoas hemorrhage and underwent TAE. Although active bleeding was not observed on angiography, superselective embolization was performed prophylactically using GSP in the left third and fourth lumbar arteries. However, the patient later developed weakness in the lower limbs on the same side. Subsequent magnetic resonance imaging (MRI) showed diffusion restriction from the lower thoracic spinal cord to the conus medullaris, suggesting spinal cord ischemia (Figure 2). Meanwhile, other patients only developed minor complications, which included mild fever (four patients, 11.1%). These symptoms improved following conservative treatment within 2–3 days postoperatively.
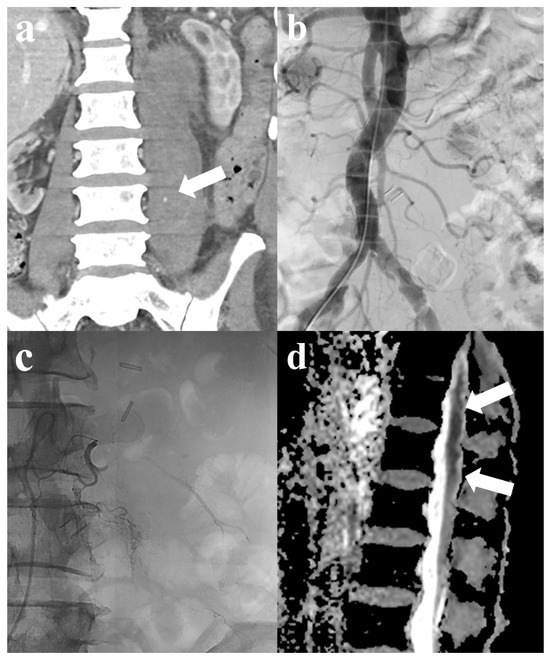
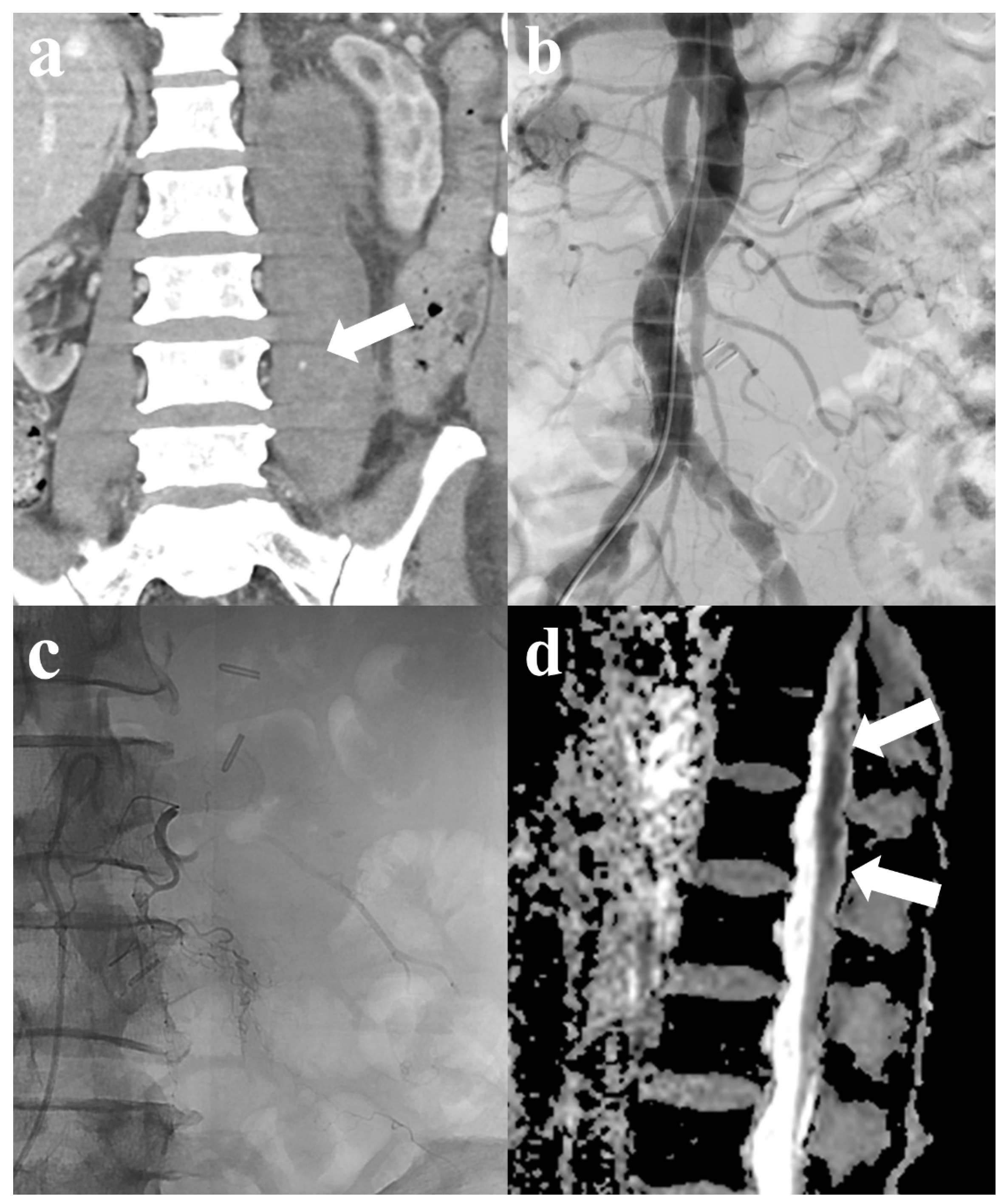
Figure 2.
A 76-year-old male patient with spontaneous psoas hemorrhage. (a) Computed tomography (CT) shows contrast media extravasation with hematoma in the left psoas muscle (arrow). (b) Abdominal aortography reveals no definite active bleeding. Subsequent selective multilevel left lumbar artery angiography also shows no active bleeding. (c) Selective embolization was performed using gelatin sponge particles in the left 3rd and 4th lumbar arteries for prophylactic purposes. (d) After embolization, motor weakness in the ipsilateral lower extremity developed; magnetic resonance imaging (MRI) suggests spinal cord infarction, indicated by suspected diffusion restriction in the lower thoracic spinal cord through the conus medullaris (arrows).
4. Discussion
The retroperitoneum is a highly vascular area with numerous collateral supplies to any given region [14]. Hence, accessing this area poses a significant challenge. Once the bleeding artery is controlled, collateral supply to the same territory may trigger new bleeding episodes. Moreover, surgical intervention in the retroperitoneal space can often escalate the risk of catastrophic hemorrhage due to the dissection and loss of the passive tamponade effect of a hematoma [15]. Compared with surgical methods, endovascular procedures, including the transcatheter embolization of the bleeding vessel, are safe, quick, and minimally invasive, and provide immediate treatment [16]. The univariate logistic regression analysis showed that pRBC transfusion was a statistically significant factor associated with clinical failure (OR (95% CI): 1.459 (1.024–2.078), p = 0.037). Previous studies have shown that a higher number of pRBC transfusions before embolization is significantly linked to poorer clinical outcomes and increased mortality within 30 days [17,18]. Patidar et al. suggested that the development of transfusion-related disseminated intravascular coagulopathy prior to the embolization procedure could be the most likely explanation for clinical failure associated with massive blood transfusion [18]. Research on the risk factors of clinical failure during TAE for traumatic and spontaneous psoas or retroperitoneal hemorrhages remains limited. Hence, further investigations with a larger cohort are warranted.
Among the 37 patients examined in our study, 36 achieved technical success, with clinical success observed in 28 patients (77.8%). Notably, the clinical success rate was lower in the SG (64.7% (11/17)). The overall mortality rate was 19.4% (7/36), which is consistent with the reports of previous studies that documented mortality rates ranging from 12% to 22% with similar embolization outcomes [3,4,6]. However, the SG exhibited a significantly higher mortality rate of 35.3% (6/17), while the TG demonstrated a mortality rate of only 5.3% (1/19) (p = 0.023), surpassing previously reported figures. This increase in the mortality rate in the SG was attributed to the presence of liver cirrhosis in six patients in our cohort, five of whom experienced spontaneous hemorrhage, clinical failure, and eventually death within days. This outcome starkly aligns with the findings of previous studies, which reported a mortality rate between 71% and 83% in such patients, underscoring a poor prognosis [19]. Patients with liver cirrhosis are predisposed to bleeding due to the occurrence of complications such as thrombocytopenia, platelet dysfunction, and decreased levels of coagulation factors. In our study, the multivariate logistic regression analysis showed that liver cirrhosis was the only independent factor associated with clinical failure (OR (95% CI): 55.055 (2.439–1242.650), p = 0.012). Gastrointestinal hemorrhage is the most prevalent bleeding complication, although a significant association between retroperitoneal hemorrhage and alcoholic liver disease has been documented [19]. This association further exacerbates the risk through various mechanisms beyond the typical effects of cirrhosis, such as vascular fragility and impaired platelet functionality [20,21]. Although retroperitoneal hemorrhage typically occurs in response to trauma or oral anticoagulation therapy, spontaneous arterial bleeding rarely occurs [20]. Nonetheless, individuals with severe hepatic coagulopathy may develop hematomas even from minor incidents. TAE has been widely recognized for its potential to enhance survival among patients with cirrhosis who developed retroperitoneal hemorrhage [19]. Takamura et al. reported a survival rate of 50% (2/4) in patients undergoing TAE [19], while other studies have reported successful embolization in patients with end-stage liver disease with subsequent survival to discharge [22]. However, another report highlighted that despite the successful embolization in four TAE-treated patients, 75% (3/4) died within a few days. Our findings align with the challenging prognosis observed in patients with liver cirrhosis and SRH, suggesting the need for larger cohort studies owing to the limited sample used in these studies.
The incidence of retroperitoneal hematoma has been reported to range from 0.6% to 6.6% in patients undergoing therapeutic anticoagulation [23,24]. Although oral anticoagulation therapy is a common risk factor for retroperitoneal hemorrhage, our study found that eight patients (47.1%) with SRH received anticoagulation therapy. The management of life-threatening psoas hematomas and, more broadly, soft tissue hemorrhages in patients under anticoagulation therapy remains controversial. Conservative treatment is recommended for hemodynamically stable patients with no signs of ongoing bleeding; however, the efficacy of embolization or surgery in these scenarios has not been fully established. In general, hemodynamically unstable patients receiving anticoagulation therapy can be treated with arterial embolization, which is a minimally invasive method with a rapid therapeutic effect compared with surgical treatment [25]. In the study by M. Lukies et al., conservative management was reported to be successful in 13.2% of initially unstable patients, all of whom were receiving therapeutic anticoagulation therapy. They suggested that embolization in SRH may be most appropriate for patients with ongoing bleeding despite adequate reversal of anticoagulation agents or those who have not initially received anticoagulation therapy and are hemodynamically unstable [26]. However, conservative treatment is typically adequate for managing the majority of patients with mild retroperitoneal hemorrhages. The psoas muscle is capable of accumulating up to ten times its volume. Consequently, a psoas hematoma or retroperitoneal hemorrhage can present with hypotension, abdominal pain, or a decrease in hemoglobin levels. In our study, all patients (n = 8) under oral anticoagulation therapy who showed active bleeding on CT underwent aggressive TAE regardless of their hemodynamic status. The patients demonstrated a mean shock index of 0.98 (range: 0.47–1.53), with 50% (four out of eight) exhibiting a shock index of >1.0 and the remainder below this threshold. Notably, this strategy resulted in clinical success in 87.5% of the patients (seven out of eight), thereby indicating a favorable prognosis without major complications. Therefore, aggressive angiography and embolization are recommended in patients receiving anticoagulation therapy when CT reveals active bleeding in the retroperitoneal and/or psoas muscle areas.
In the literature, the mortality rate in patients with unstable traumatic retroperitoneal hemorrhage is approximately 17.6% to 47% [6,27]. A previous study utilized TAE to manage life-threatening bleeding resulting from blunt trauma or iatrogenic injury, achieving hemostasis in all patients, with an overall clinical success rate of 87.5%. Specifically, for bleeding originating from the lumbar artery, a clinical success rate of 80% (4/5) was reported [27]. Our study corroborated these findings in trauma patients, demonstrating a technical success rate of 100% and a clinical success rate of 84.2%, with mortality limited to only one patient (5.3%). These results are consistent with those of previous studies. However, contrasting findings were reported by another study that examined patients with lumbar artery injuries following blunt trauma [28]. Of the 21 bleeding sites identified, successful embolization was achieved in 16 (76.2%), while technical failure occurred in 2 (9.5%); meanwhile, conservative treatment was chosen for three sites (14.3%) due to concerns over an unintentional embolization of the artery of Adamkiewicz. Notably, 50% of patients (8/16) died due to severe brain injury, hypovolemic shock, or stroke and did not undergo embolization [28]. Our study likely yielded more favorable clinical outcomes as it focused on patients with retroperitoneal bleeding as the primary concern, excluding those whose condition was significantly affected by bleeding from other sites.
In our study, aside from fever, which resolved within a few days following conservative treatment in 11.1% of patients who underwent TAE, no significant complications occurred. However, one patient exhibited motor weakness in the ipsilateral lower extremity following embolization, raising suspicion of a complication involving the spinal cord, such as the Brown-Séquard syndrome (BSS). BSS is observed in patients with incomplete spinal cord injuries and affects a hemisection of the spinal cord. BSS with a vascular origin rarely occurs as the large vascular territories are not divided hemilaterally. Only a few cases of vascular-related BSS have been reported. Neurological damage due to spinal cord ischemia is an extremely rare adverse event of peripheral embolization procedures. It occurs following TAE using TAGM for a vertebral hemangioma involving the eighth and ninth intercostal arteries [29], as well as after thoracic endovascular aortic repair for aortic dissection [30]. In addition to BSS, a case similar to ours was reported by Grigoriadis et al., wherein a coronavirus disease 19-positive patient receiving anticoagulation therapy developed SRH and underwent TAE using NBCA after superselecting the lumbar artery, leading to paralysis of both lower extremities. Subsequent MRI revealed ischemia and edema in the anterior part of the spinal cord from T11 to L5 [31]. There may occasionally be a collateral network to a radiculomedullary artery originating from the lower lumbar artery, necessitating utmost caution during the procedures [31]. Thus, in patients with psoas or retroperitoneal hemorrhage, if evident bleeding from the lumbar artery is observed on angiography, superselective embolization should be carefully performed. If embolization is deemed necessary, and a connection to the radiculomedullary artery is suspected, it is crucial to superselect the target arterial branch to prevent the reflux of embolic materials and proceed with caution.
This study has some limitations. It has a small sample size and retrospective design. Furthermore, due to the small sample size, we were unable to perform separate multivariate analyses for each group. This limitation hindered our ability to thoroughly investigate potential interactions and covariate adjustments, thereby reducing the robustness and reliability of our findings. Studies with larger patient cohorts and longer follow-up periods are warranted to further validate the findings. There was heterogeneity in the patient groups and angiographic findings, with potential confounding factors. The selection of the target vessel and embolic agent varied and was dependent on the operator’s preference, which could have affected the outcomes. Some complications after the procedure may not have been detected due to the lack of a standardized follow-up protocol after TAE.
5. Conclusions
TAE for psoas and/or retroperitoneal hemorrhage was safe and effective, regardless of whether the bleeding was spontaneous or trauma-related. However, patients with liver cirrhosis or requiring massive transfusion due to hemorrhage may have an increased risk of clinical failure and mortality, necessitating aggressive monitoring and treatment.
Author Contributions
Conceptualization, C.H.O.; methodology, C.H.O. and S.B.C.; data curation, C.H.O. and H.K.; writing—original draft preparation, C.H.O. and S.B.C.; writing—review and editing, C.H.O. and S.B.C.; visualization, C.H.O. and H.K.; supervision, C.H.O. and S.B.C.; project administration, C.H.O. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki and approved by the institutional review board (or Ethics Committee) of Ewha Womans Mokdong University Hospital (protocol code: EUMC 2024-03-040; date of approval: 27 March 2024).
Informed Consent Statement
This retrospective, single-center study was approved by the institutional review board, which waived the need for obtaining informed consent from the patients.
Data Availability Statement
All data are available through the corresponding authors.
Conflicts of Interest
The authors declare that they have no competing interests.
References
- Maleux, G.; Stockx, L.; Wilms, G.; Bogaert, G.; Marchal, G. Postoperative retroperitoneal hemorrhage due to a bleeding ureteric artery: Treatment by transcatheter embolization. Eur. Radiol. 2001, 11, 34–36. [Google Scholar] [CrossRef]
- Lumsden, A.B.; Miller, J.M.; Kosinski, A.S.; Allen, R.C.; Dodson, T.F.; Salam, A.A.; Smith, R.B., 3rd. A prospective evaluation of surgically treated groin complications following percutaneous cardiac procedures. Am. Surg. 1994, 60, 132–137. [Google Scholar] [PubMed]
- Warren, M.H.; Bhattacharya, B.; Maung, A.A.; Davis, K.A. Contemporary management of spontaneous retroperitoneal and rectus sheath hematomas. Am. J. Surg. 2020, 219, 707–710. [Google Scholar] [CrossRef] [PubMed]
- Baekgaard, J.S.; Eskesen, T.G.; Lee, J.M.; Yeh, D.D.; Kaafarani, H.M.; Fagenholz, P.J.; Avery, L.; Saillant, N.; King, D.R.; Velmahos, G.C. Spontaneous retroperitoneal and rectus sheath hemorrhage—Management, risk factors and outcomes. World J. Surg. 2019, 43, 1890–1897. [Google Scholar] [CrossRef] [PubMed]
- Sahu, K.K.; Mishra, A.K.; Lal, A.; George, S.V. Retroperitoneal and rectus sheath hematomas: Challenges in diagnosis and management. Am. J. Surg. 2020, 219, 726–727. [Google Scholar] [CrossRef] [PubMed]
- Akpinar, E.; Peynircioglu, B.; Turkbey, B.; Cil, B.E.; Balkanci, F. Endovascular management of life-threatening retroperitoneal bleeding. ANZ J. Surg. 2008, 78, 683–687. [Google Scholar] [CrossRef]
- Domenicucci, M.; Ramieri, A.; Lenzi, J.; Fontana, E.; Martini, S. Pseudo-aneurysm of a lumbar artery after flexion-distraction injury of the thoraco-lumbar spine and surgical realignment: Rupture treated by endovascular embolization. Spine 2008, 33, E81–E84. [Google Scholar] [CrossRef]
- Chan, Y.; Morales, J.P.; Reidy, J.F.; Taylor, P.R. Management of spontaneous and iatrogenic retroperitoneal haemorrhage: Conservative management, endovascular intervention or open surgery? Int. J. Clin. Pract. 2008, 62, 1604–1613. [Google Scholar] [CrossRef] [PubMed]
- Ekici, Y.; Aydogan, C.; Yagmurdur, M.C.; Kirnap, M.; Harman, A.; Moray, G.; Karakayali, H.; Haberal, M. Treatment approaches for spontaneous retroperitoneal bleeding. Int. Surg. 2009, 94, 171–175. [Google Scholar]
- Klausenitz, C.; Kuehn, J.P.; Noeckler, K.; Radosa, C.G.; Hoffmann, R.T.; Teichgraeber, U.; Mensel, B. Efficacy of transarterial embolisation in patients with life-threatening spontaneous retroperitoneal haematoma. Clin. Radiol. 2021, 76, 157.e11–157.e18. [Google Scholar] [CrossRef]
- Sacks, D. Society of interventional radology clinical practice guidelines. J. Vasc. Interv. Radiol. 2003, 14, S199–S202. [Google Scholar] [CrossRef] [PubMed]
- Stainsby, D.; MacLennan, S.; Hamilton, P. Management of massive blood loss: A template guideline. Br. J. Anaesth. 2000, 85, 487–491. [Google Scholar] [CrossRef] [PubMed]
- Spahn, D.R.; Cerny, V.; Coats, T.J.; Duranteau, J.; Fernández-Mondéjar, E.; Gordini, G.; Stahel, P.F.; Hunt, B.J.; Komadina, R.; Neugebauer, E.; et al. Management of bleeding following major trauma: A European guideline. Crit. Care 2007, 11, 1–22. [Google Scholar] [CrossRef]
- Marty, B.; Sanchez, L.A.; Wain, R.A.; Ohki, T.; Marin, M.L.; Bakal, C.; Veith, F.J. Endovascular treatment of a ruptured lumbar artery aneurysm: Case report and review of the literature. Ann. Vasc. Surg. 1998, 12, 379–383. [Google Scholar] [CrossRef]
- Dondelinger, R.; Trotteur, G.; Ghaye, B.; Szapiro, D. Traumatic injuries: Radiological hemostatic intervention at admission. Eur. Radiol. 2002, 12, 979–993. [Google Scholar] [CrossRef] [PubMed]
- Janík, V.; Martínek, V.; Padr, R.; Lisý, J.; Neuwirth, J.; Pafčugová, J.; Vaněček, T.; Stejskal, J. Embolization of lumbar artery due to retroperitonal bleeding following renal biopsy. Nephrol. Dial. Transplant. 2005, 20, 820–822. [Google Scholar] [CrossRef] [PubMed]
- Jawhari, R.; Chevallier, O.; Falvo, N.; d’Athis, P.; Gehin, S.; Charles, P.E.; Midulla, M.; Loffroy, R. Outcomes of transcatheter arterial embolization with a modified N-butyl cyanoacrylate glue for spontaneous iliopsoas and rectus sheath hematomas in anticoagulated patients. J. Vasc. Interv. Radiol. 2018, 29, 210–217. [Google Scholar] [CrossRef] [PubMed]
- Patidar, Y.; Srinivasan, S.V.; Singh, J.; Patel, R.K.; Chandel, K.; Mukund, A.; Sharma, M.K.; Sarin, S.K. Clinical Outcomes of Transcatheter Arterial Embolization Using N-butyl-2-cyanoacrylate (NBCA) in Cirrhotic Patients. J. Clin. Exp. Hepatol. 2022, 12, 353–361. [Google Scholar] [CrossRef] [PubMed]
- Takamura, M.; Watanabe, J.; Sakamaki, A.; Honda, Y.; Kamimura, K.; Tsuchiya, A.; Yamagiwa, S.; Suda, T.; Matsuda, Y.; Aoyagi, Y. Alcoholic liver disease complicated by deep bleeding into the muscles or retroperitoneum: Report of three cases and a review of the literature. Intern. Med. 2014, 53, 1763–1768. [Google Scholar] [CrossRef]
- Tripodi, A.; Mannucci, P.M. The coagulopathy of chronic liver disease. N. Engl. J. Med. 2011, 365, 147–156. [Google Scholar] [CrossRef]
- Yoshida, H.; Tsuji, K.; Kawakami, H.; Katanuma, A.; Sakurai, Y.; Jong-Hon, K.; Koizumi, K.; Mitsui, S.; Gotoh, M.; Yoshida, A.; et al. Two cases of alcoholic liver cirrhosis associated with intramuscular hematoma. Nihon Shokakibyo Gakkai Zasshi Jpn. J. Gastro-Enterol. 2002, 99, 1350–1354. [Google Scholar]
- Best, J.A.; Smith, M.W. Spontaneous retroperitoneal hematoma originating at lumbar arteries in context of cirrhosis. J. Hosp. Med. 2010, 5, E4–E5. [Google Scholar] [CrossRef] [PubMed]
- Pallejà, X.E.; Domingo, P.; Fontcuberta, J.; Felez, J. Spontaneous retroperitoneal hemorrhage during oral anticoagulant therapy. Arch. Intern. Med. 1985, 145, 1531–1534. [Google Scholar] [CrossRef] [PubMed]
- Mant, M.; Thong, K.L.; Birtwhistle, R.; O’Brien, B.; Hammond, G.; Grace, M. Haemorrhagic complications of heparin therapy. Lancet 1977, 309, 1133–1135. [Google Scholar] [CrossRef] [PubMed]
- Patel, I.; Akoluk, A.; Douedi, S.; Upadhyaya, V.; Mazahir, U.; Costanzo, E.; Flynn, D. Life-threatening psoas hematoma due to retroperitoneal hemorrhage in a COVID-19 patient on enoxaparin treated with arterial embolization: A case report. J. Clin. Med. Res. 2020, 12, 458. [Google Scholar] [CrossRef] [PubMed]
- Lukies, M.; Gipson, J.; Tan, S.Y.; Clements, W. Spontaneous retroperitoneal haemorrhage: Efficacy of conservative management and embolisation. CardioVascular Interv. Radiol. 2023, 46, 488–495. [Google Scholar] [CrossRef] [PubMed]
- Boufi, M.; Bordon, S.; Dona, B.; Hartung, O.; Sarran, A.; Nadeau, S.; Maurin, C.; Alimi, Y.S. Unstable patients with retroperitoneal vascular trauma: An endovascular approach. Ann. Vasc. Surg. 2011, 25, 352–358. [Google Scholar] [CrossRef] [PubMed]
- Yuan, K.-C.; Hsu, Y.P.; Wong, Y.C.; Fang, J.F.; Lin, B.C.; Chen, H.W. Management of complicated lumbar artery injury after blunt trauma. Ann. Emerg. Med. 2011, 58, 531–535. [Google Scholar] [CrossRef] [PubMed]
- Fernandez-Torron, R.; Palma, J.A.; Riverol, M.; Irimia, P.; Martinez-Vila, E. Brown-sequard syndrome after endovascular embolization of vertebral hemangioma. Spinal Cord 2012, 50, 636–637. [Google Scholar] [CrossRef]
- Klijn, A.J.; Heida, J.; Burger, D.H.; Heyligers, J.M.; Pouwels, S. Brown–Séquard Syndrome after Thoracic Endovascular Aortic Repair for a Stanford Type B Aortic Dissection. Vasc. Spec. Int. 2022, 38, 12. [Google Scholar] [CrossRef]
- Grigoriadis, S.; Georgiadi, E.; Sidiropoulos, T.A.; Efthimiou, E.; Spiliopoulos, S. Spinal Cord Ischemia after Lumbar Artery Embolization for Retroperitoneal Hemorrhage. J. Vasc. Interv. Radiol. JVIR 2024, 35, 329–330. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).