Reverse Shoulder Arthroplasty versus Non-Operative Treatment of Three-Part and Four-Part Proximal Humerus Fractures in the Elderly Patient: A Pooled Analysis and Systematic Review
Abstract
1. Introduction
2. Methods
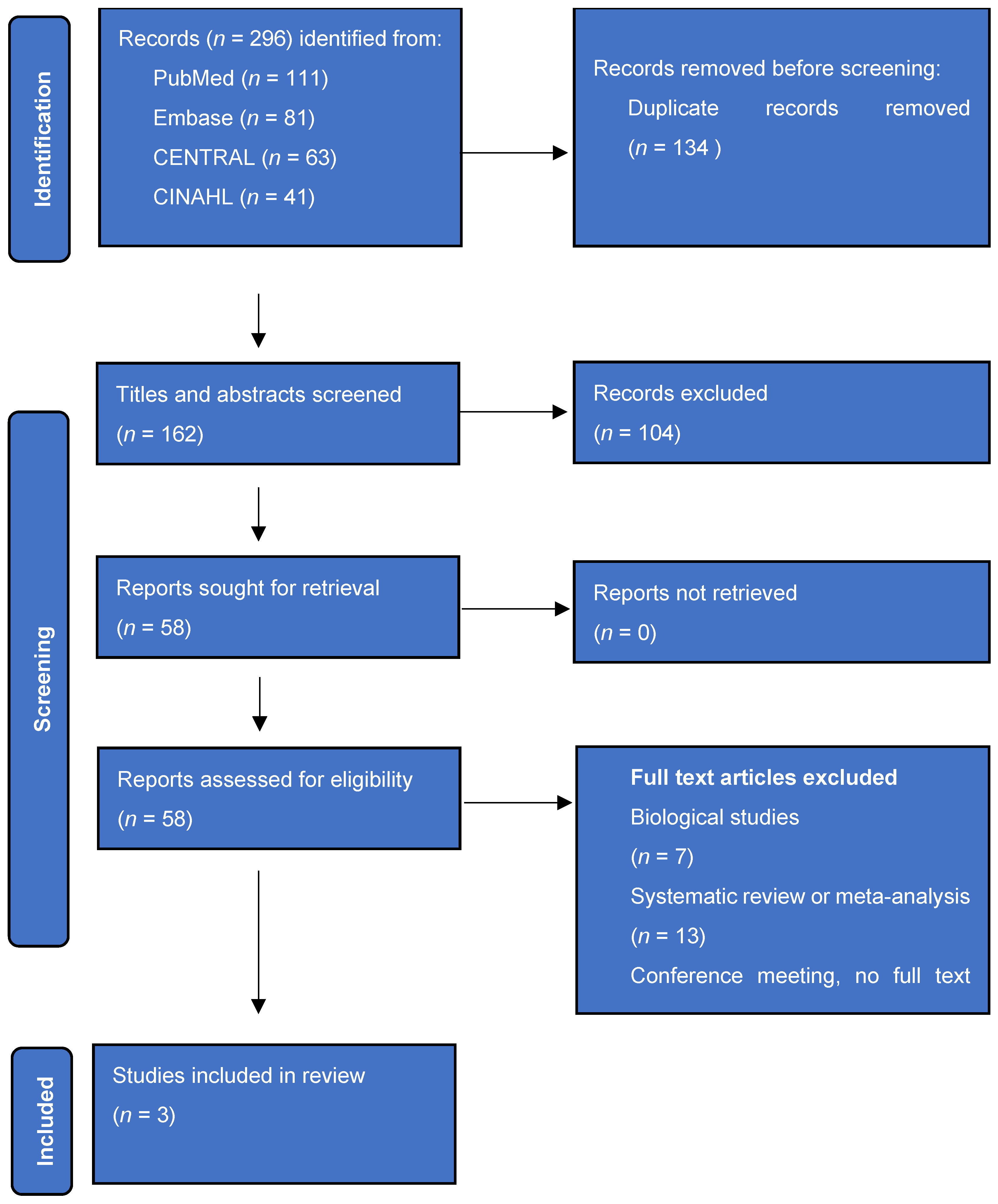
2.1. Search Strategy and Selection Criteria
2.2. Data Extraction
2.3. Quality Assessment
2.4. Study Outcome
2.5. Statistical Analysis
3. Results
3.1. Comparative Studies
3.1.1. Study Characteristics and Quality Assessment
3.1.2. Functional Outcomes
3.1.3. Range of Motion
3.1.4. Complications
3.1.5. Pain and Satisfaction
3.1.6. Case Series and Non-Comparative Studies on RSA and NOT
4. Discussion
5. Limitations
6. Conclusions
7. Future Directions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
References
- Court-Brown, C.M.; Caesar, B. Epidemiology of Adult Fractures: A Review. Injury 2006, 37, 691–697. [Google Scholar] [CrossRef]
- Carofino, B.C.; Leopold, S.S. Classifications in Brief: The Neer Classification for Proximal Humerus Fractures. Clin. Orthop. Relat. Res. 2013, 471, 39–43. [Google Scholar] [CrossRef]
- Grammont, P.; Trouilloud, P.; Laffay, J.; Deries, X. Study and Development of a New Shoulder Prosthesis. Rhumatologie 1987, 39, 407–418. [Google Scholar]
- Olerud, P.; Ahrengart, L.; Ponzer, S.; Saving, J.; Tidermark, J. Hemiarthroplasty Versus Nonoperative Treatment of Displaced 4-Part Proximal Humeral Fractures in Elderly Patients: A Randomized Controlled Trial. J. Shoulder Elb. Surg. 2011, 20, 1025–1033. [Google Scholar] [CrossRef]
- Olerud, P.; Ahrengart, L.; Ponzer, S.; Saving, J.; Tidermark, J. Internal Fixation Versus Nonoperative Treatment of Displaced 3-Part Proximal Humeral Fractures in Elderly Patients: A Randomized Controlled Trial. J. Shoulder Elb. Surg. 2011, 20, 747–755. [Google Scholar] [CrossRef]
- Orman, S.; Mohamadi, A.; Serino, J.; Murphy, J.; Hanna, P.; Weaver, M.J.; Dyer, G.; Nazarian, A.; von Keudell, A. Comparison of Surgical and Non-Surgical Treatments for 3- and 4-Part Proximal Humerus Fractures: A Network Meta-Analysis. Shoulder Elb. 2020, 12, 99–108. [Google Scholar] [CrossRef]
- Cuff, D.J.; Pupello, D.R. Comparison of Hemiarthroplasty and Reverse Shoulder Arthroplasty for the Treatment of Proximal Humeral Fractures in Elderly Patients. J. Bone Jt. Surg. Am. 2013, 95, 2050–2055. [Google Scholar] [CrossRef]
- Fraser, A.N.; Bjørdal, J.; Wagle, T.M.; Karlberg, A.C.; Lien, O.A.; Eilertsen, L.; Mader, K.; Apold, H.; Larsen, L.B.; Madsen, J.E.; et al. Reverse Shoulder Arthroplasty Is Superior to Plate Fixation at 2 Years for Displaced Proximal Humeral Fractures in the Elderly: A Multicenter Randomized Controlled Trial. J. Bone Jt. Surg. Am. 2020, 102, 477–485. [Google Scholar] [CrossRef]
- Dillon, M.T.; Prentice, H.A.; Burfeind, W.E.; Chan, P.H.; Navarro, R.A. The Increasing Role of Reverse Total Shoulder Arthroplasty in the Treatment of Proximal Humerus Fractures. Injury 2019, 50, 676–680. [Google Scholar] [CrossRef]
- Zyto, K. Non-Operative Treatment of Comminuted Fractures of the Proximal Humerus in Elderly Patients. Injury 1998, 29, 349–352. [Google Scholar] [CrossRef]
- Clement, N.D.; Aitken, S.A.; Duckworth, A.D.; McQueen, M.M.; Court-Brown, C.M. The Outcome of Fractures in Very Elderly Patients. J. Bone Jt. Surg. Br. Vol. 2011, 93-B, 806–810. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The Prisma Statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef] [PubMed]
- Stroup, D.F.; Berlin, J.A.; Morton, S.C.; Olkin, I.; Williamson, G.D.; Rennie, D.; Moher, D.; Becker, B.J.; Sipe, T.A.; Thacker, S.B.; et al. Meta-Analysis of Observational Studies in Epidemiologya Proposal for Reporting. JAMA 2000, 283, 2008–2012. [Google Scholar] [CrossRef] [PubMed]
- Lopiz, Y.; Alcobía-Díaz, B.; Galán-Olleros, M.; García-Fernández, C.; Picado, A.L.; Marco, F. Reverse Shoulder Arthroplasty Versus Nonoperative Treatment for 3- or 4-Part Proximal Humeral Fractures in Elderly Patients: A Prospective Randomized Controlled Trial. J. Shoulder Elb. Surg. 2019, 28, 2259–2271. [Google Scholar] [CrossRef] [PubMed]
- Chivot, M.; Lami, D.; Bizzozero, P.; Galland, A.; Argenson, J.-N. Three- and Four-Part Displaced Proximal Humeral Fractures in Patients Older Than 70 Years: Reverse Shoulder Arthroplasty or Nonsurgical Treatment? J. Shoulder Elb. Surg. 2019, 28, 252–259. [Google Scholar] [CrossRef]
- Roberson, T.A.; Granade, C.M.; Hunt, Q.; Griscom, J.T.; Adams, K.J.; Momaya, A.M.; Kwapisz, A.; Kissenberth, M.J.; Tolan, S.J.; Hawkins, R.J.; et al. Nonoperative Management Versus Reverse Shoulder Arthroplasty for Treatment of 3- and 4-Part Proximal Humeral Fractures in Older Adults. J. Shoulder Elb. Surg. 2017, 26, 1017–1022. [Google Scholar] [CrossRef]
- Grassi, F.A.; Zorzolo, I. Reverse Shoulder Arthroplasty without Subscapularis Repair for the Treatment of Proximal Humeral Fractures in the Elderly. Musculoskelet. Surg. 2014, 98 (Suppl. 1), 5–13. [Google Scholar] [CrossRef]
- Grubhofer, F.; Wieser, K.; Meyer, D.C.; Catanzaro, S.; Beeler, S.; Riede, U.; Gerber, C. Reverse Total Shoulder Arthroplasty for Acute Head-Splitting, 3- and 4-Part Fractures of the Proximal Humerus in the Elderly. J. Shoulder Elb. Surg. 2016, 25, 1690–1698. [Google Scholar] [CrossRef] [PubMed]
- Klein, M.; Juschka, M.; Hinkenjann, B.; Scherger, B.; Ostermann, P.A. Treatment of Comminuted Fractures of the Proximal Humerus in Elderly Patients with the Delta Iii Reverse Shoulder Prosthesis. J. Orthop. Trauma 2008, 22, 698–704. [Google Scholar] [CrossRef]
- Klug, A.; Harth, J.; Hoffmann, R.; Gramlich, Y. Surgical Treatment of Complex Proximal Humeral Fractures in Elderly Patients: A Matched-Pair Analysis of Angular-Stable Plating Vs. Reverse Shoulder Arthroplasty. J. Shoulder Elb. Surg. 2020, 29, 1796–1803. [Google Scholar] [CrossRef]
- Lenarz, C.; Shishani, Y.; McCrum, C.; Nowinski, R.J.; Edwards, T.B.; Gobezie, R. Is Reverse Shoulder Arthroplasty Appropriate for the Treatment of Fractures in the Older Patient? Early Observations. Clin. Orthop. Relat. Res. 2011, 469, 3324–3331. [Google Scholar] [CrossRef]
- Lopiz, Y.; García-Coiradas, J.; Serrano-Mateo, L.; García-Fernández, C.; Marco, F. Reverse Shoulder Arthroplasty for Acute Proximal Humeral Fractures in the Geriatric Patient: Results, Health-Related Quality of Life and Complication Rates. Int. Orthop. 2016, 40, 771–781. [Google Scholar] [CrossRef]
- Luciani, P.; Farinelli, L.; Procaccini, R.; Verducci, C.; Gigante, A. Primary Reverse Shoulder Arthroplasty for Acute Proximal Humerus Fractures: A 5-Year Long Term Retrospective Study of Elderly Patients. Injury 2019, 50, 1974–1977. [Google Scholar] [CrossRef]
- Ohl, X.; Bonnevialle, N.; Gallinet, D.; Ramdane, N.; Valenti, P.; Decroocq, L.; Boileau, P. How the Greater Tuberosity Affects Clinical Outcomes after Reverse Shoulder Arthroplasty for Proximal Humeral Fractures. J. Shoulder Elb. Surg. 2018, 27, 2139–2144. [Google Scholar] [CrossRef] [PubMed]
- Repetto, I.; Alessio-Mazzola, M.; Cerruti, P.; Sanguineti, F.; Formica, M.; Felli, L. Surgical Management of Complex Proximal Humeral Fractures: Pinning, Locked Plate and Arthroplasty: Clinical Results and Functional Outcome on Retrospective Series of Patients. Musculoskelet. Surg. 2017, 101, 153–158. [Google Scholar] [CrossRef] [PubMed]
- Schmalzl, J.; Jessen, M.; Holschen, M.; Cohen, B.C.; Steinbeck, J.; Lehmann, L.-J.; Denard, P.J. Tuberosity Healing Improves Functional Outcome Following Primary Reverse Shoulder Arthroplasty for Proximal Humeral Fractures with a 135° Prosthesis. Eur. J. Orthop. Surg. Traumatol. 2020, 30, 909–916. [Google Scholar] [CrossRef]
- Baudi, P.; Campochiaro, G.; Serafini, F.; Gazzotti, G.; Matino, G.; Rovesta, C.; Catani, F. Hemiarthroplasty Versus Reverse Shoulder Arthroplasty: Comparative Study of Functional and Radiological Outcomes in the Treatment of Acute Proximal Humerus Fracture. Musculoskelet. Surg. 2014, 98 (Suppl. 1), 19–25. [Google Scholar] [CrossRef] [PubMed]
- Sebastiá-Forcada, E.; Cebrián-Gómez, R.; Lizaur-Utrilla, A.; Gil-Guillén, V. Reverse Shoulder Arthroplasty Versus Hemiarthroplasty for Acute Proximal Humeral Fractures. A Blinded, Randomized, Controlled, Prospective Study. J. Shoulder Elb. Surg. 2014, 23, 1419–1426. [Google Scholar] [CrossRef]
- Simovitch, R.W.; Roche, C.P.; Jones, R.B.; Routman, H.D.; Marczuk, Y.; Wright, T.W.; Zuckerman, J.D. Effect of Tuberosity Healing on Clinical Outcomes in Elderly Patients Treated with a Reverse Shoulder Arthroplasty for 3- and 4-Part Proximal Humerus Fractures. J. Orthop. Trauma 2019, 33, e39–e45. [Google Scholar] [CrossRef]
- Solomon, J.A.; Joseph, S.M.; Shishani, Y.; Victoroff, B.N.; Wilber, J.H.; Gobezie, R.; Gillespie, R.J. Cost Analysis of Hemiarthroplasty Versus Reverse Shoulder Arthroplasty for Fractures. Orthopedics 2016, 39, 230–234. [Google Scholar] [CrossRef]
- Torrens, C.; Alentorn-Geli, E.; Mingo, F.; Gamba, C.; Santana, F. Reverse Shoulder Arthroplasty for the Treatment of Acute Complex Proximal Humeral Fractures: Influence of Greater Tuberosity Healing on the Functional Outcomes. J. Orthop. Surg. 2018, 26, 2309499018760132. [Google Scholar] [CrossRef] [PubMed]
- Valenti, P.; Katz, D.; Kilinc, A.; Elkholti, K.; Gasiunas, V. Mid-Term Outcome of Reverse Shoulder Prostheses in Complex Proximal Humeral Fractures. Acta Orthop. Belg. 2012, 78, 442–449. [Google Scholar]
- van der Merwe, M.; Boyle, M.J.; Frampton, C.M.A.; Ball, C.M. Reverse Shoulder Arthroplasty Compared with Hemiarthroplasty in the Treatment of Acute Proximal Humeral Fractures. J. Shoulder Elb. Surg. 2017, 26, 1539–1545. [Google Scholar] [CrossRef] [PubMed]
- Wolfensperger, F.; Grüninger, P.; Dietrich, M.; Völlink, M.; Benninger, E.; Schläppi, M.; Meier, C. Reverse Shoulder Arthroplasty for Complex Fractures of the Proximal Humerus in Elderly Patients: Impact on the Level of Independency, Early Function, and Pain Medication. J. Shoulder Elb. Surg. 2017, 26, 1462–1468. [Google Scholar] [CrossRef] [PubMed]
- Wright, J.O.; Ho, A.; Kalma, J.; Koueiter, D.; Esterle, J.; Marcantonio, D.; Wiater, J.M.; Wiater, B. Uncemented Reverse Total Shoulder Arthroplasty as Initial Treatment for Comminuted Proximal Humerus Fractures. J. Orthop. Trauma 2019, 33, e263–e269. [Google Scholar] [CrossRef] [PubMed]
- Young, S.W.; Segal, B.S.; Turner, P.C.; Poon, P.C. Comparison of Functional Outcomes of Reverse Shoulder Arthroplasty Versus Hemiarthroplasty in the Primary Treatment of Acute Proximal Humerus Fracture. ANZ J. Surg. 2010, 80, 789–793. [Google Scholar] [CrossRef] [PubMed]
- Bogner, R.; Resch, H.; Moroder, P. Functional and Quality-of-Life Results of Displaced and Nondisplaced Proximal Humeral Fractures Treated Conservatively. J. Orthop. Trauma 2014, 28, e178. [Google Scholar] [CrossRef] [PubMed]
- Bonnevialle, N.; Tournier, C.; Clavert, P.; Ohl, X.; Sirveaux, F.; Saragaglia, D. Hemiarthroplasty Versus Reverse Shoulder Arthroplasty in 4-Part Displaced Fractures of the Proximal Humerus: Multicenter Retrospective Study. Orthop. Traumatol. Surg. Res. 2016, 102, 569–573. [Google Scholar] [CrossRef]
- Boyle, M.J.; Youn, S.-M.; Frampton, C.M.A.; Ball, C.M. Functional Outcomes of Reverse Shoulder Arthroplasty Compared with Hemiarthroplasty for Acute Proximal Humeral Fractures. J. Shoulder Elb. Surg. 2013, 22, 32–37. [Google Scholar] [CrossRef]
- Cazeneuve, J.F.; Cristofari, D.J. The Reverse Shoulder Prosthesis in the Treatment of Fractures of the Proximal Humerus in the Elderly. J. Bone Jt. Surg. Br. 2010, 92, 535–539. [Google Scholar] [CrossRef]
- Gallinet, D.; Cazeneuve, J.F.; Boyer, E.; Menu, G.; Obert, L.; Ohl, X.; Bonnevialle, N.; Valenti, P.; Boileau, P. Reverse Shoulder Arthroplasty for Recent Proximal Humerus Fractures: Outcomes in 422 Cases. Orthop. Traumatol. Surg. Res. 2019, 105, 805–811. [Google Scholar] [CrossRef] [PubMed]
- Garrigues, G.E.; Johnston, P.S.; Pepe, M.D.; Tucker, B.S.; Ramsey, M.L.; Austin, L.S. Hemiarthroplasty Versus Reverse Total Shoulder Arthroplasty for Acute Proximal Humerus Fractures in Elderly Patients. Orthopedics 2012, 35, e703–e708. [Google Scholar] [CrossRef] [PubMed]
- Barbosa, L.; Pires, L.; Rego, P.; Alonso, R. Reverse Total Shoulder Arthroplasty for Treatment of 3- and 4-Part Proximal Humeral Fractures: Clinical and Radiological Analysis with Minimum Follow-up of 2 Years. Geriatr. Orthop. Surg. Rehabil. 2020, 11, 2151459320915321. [Google Scholar] [CrossRef] [PubMed]
- Boons, H.W.; Goosen, J.H.; van Grinsven, S.; van Susante, J.L.; van Loon, C.J. Hemiarthroplasty for Humeral Four-Part Fractures for Patients 65 Years and Older: A Randomized Controlled Trial. Clin. Orthop. Relat. Res. 2012, 470, 3483–3491. [Google Scholar] [CrossRef] [PubMed]
- Brouwer, M.E.; Reininga, I.H.F.; El Moumni, M.; Wendt, K.W. Outcomes of Operative and Nonoperative Treatment of 3- and 4-Part Proximal Humeral Fractures in Elderly: A 10-Year Retrospective Cohort Study. Eur. J. Trauma. Emerg. Surg. 2019, 45, 131–138. [Google Scholar] [CrossRef] [PubMed]
- Clement, N.D.; Duckworth, A.D.; McQueen, M.M.; Court-Brown, C.M. The Outcome of Proximal Humeral Fractures in the Elderly: Predictors of Mortality and Function. Bone Jt. J. 2014, 96-B, 970–977. [Google Scholar] [CrossRef] [PubMed]
- Rangan, A.; Handoll, H.; Brealey, S.; Jefferson, L.; Keding, A.; Martin, B.C.; Goodchild, L.; Chuang, L.H.; Hewitt, C.; Torgerson, D. Surgical vs. Nonsurgical Treatment of Adults with Displaced Fractures of the Proximal Humerus: The Profher Randomized Clinical Trial. JAMA 2015, 313, 1037–1047. [Google Scholar] [CrossRef] [PubMed]
- Dezfuli, B.; King, J.J.; Farmer, K.W.; Struk, A.M.; Wright, T.W. Outcomes of Reverse Total Shoulder Arthroplasty as Primary Versus Revision Procedure for Proximal Humerus Fractures. J. Shoulder Elb. Surg. 2016, 25, 1133–1137. [Google Scholar] [CrossRef] [PubMed]
- Panagopoulos, G.N.; Pugliese, M.; Leonidou, A.; Butt, F.; Jaibaji, M.; Megaloikonomos, P.D.; Consigliere, P.; Sforza, G.; Atoun, E.; Levy, O. Acute Versus Delayed Reverse Total Shoulder Arthroplasty for Proximal Humeral Fractures: A Consecutive Cohort Study. J. Shoulder Elb. Surg. 2022, 31, 276–285. [Google Scholar] [CrossRef]
- Kang, J.R.; Dubiel, M.J.; Cofield, R.H.; Steinmann, S.P.; Elhassan, B.T.; Morrey, M.E.; Sperling, J.W.; Sanchez-Sotelo, J. Primary Reverse Shoulder Arthroplasty Using Contemporary Implants Is Associated with Very Low Reoperation Rates. J. Shoulder Elb. Surg. 2019, 28, S175–S180. [Google Scholar] [CrossRef]
- Simovitch, R.; Flurin, P.-H.; Wright, T.; Zuckerman, J.D.; Roche, C.P. Quantifying Success after Total Shoulder Arthroplasty: The Minimal Clinically Important Difference. J. Shoulder Elb. Surg. 2018, 27, 298–305. [Google Scholar] [CrossRef]
- Wijgman, A.J.; Roolker, W.; Patt, T.W.; Raaymakers, E.L.F.B.; Marti, R.K. Open Reduction and Internal Fixation of Three and Four-Part Fractures of the Proximal Part of the Humerus. JBJS 2002, 84, 1919–1925. [Google Scholar] [CrossRef]
- Bacle, G.; Nové-Josserand, L.; Garaud, P.; Walch, G. Long-Term Outcomes of Reverse Total Shoulder Arthroplasty: A Follow-up of a Previous Study. J. Bone Jt. Surg. Am. 2017, 99, 454–461. [Google Scholar] [CrossRef] [PubMed]
- Ascione, F.; Domos, P.; Guarrella, V.; Chelli, M.; Boileau, P.; Walch, G. Long-Term Humeral Complications after Grammont-Style Reverse Shoulder Arthroplasty. J. Shoulder Elb. Surg. 2018, 27, 1065–1071. [Google Scholar] [CrossRef]
- United Nations. World Population Prospects 2019: Highlights; United Nations, Department of Economic and Social Affairs, Population Division: New York, NY, USA, 2019. [Google Scholar]
- Polinder, S.; Haagsma, J.; Panneman, M.; Scholten, A.; Brugmans, M.; Van Beeck, E. The Economic Burden of Injury: Health Care and Productivity Costs of Injuries in the Netherlands. Accid. Anal. Prev. 2016, 93, 92–100. [Google Scholar] [CrossRef] [PubMed]
- Erixon, F.; van der Marel, E. What Is Driving the Rise in Health Care Expenditures? An Inquiry into the Nature and Causes of the Cost Disease; European Centre for International Political Economy: Brussels, Belgium, 2011. [Google Scholar]
- Abdel Khalik, H.; Humphries, B.; Zoratti, M.; Axelrod, D.; Kruse, C.; Ristevski, B.; Rajaratnam, K.; Gardner, M.; Tarride, J.-E.; Johal, H. Reverse Total Shoulder Arthroplasty Is the Most Cost-Effective Treatment Strategy for Proximal Humerus Fractures in Older Adults: A Cost-Utility Analysis. Clin. Orthop. Relat. Res. 2022, 480, 2013–2026. [Google Scholar] [CrossRef]
| Author | Design | Number of Patients | Age Mean in Years (Sd) | % Female | % Neer 4-part | Tuberculum Management | Prothesis Used | Follow-Up Months | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| RSA | NOT | RSA | NOT | RSA | NOT | RSA | NOT | Average | ||||
| Lopiz | RCT | 29 | 30 | 82 (3.4) | 85 (4.8) | 86% | 87% | 87% | 83% | Reattachment | Delta SMR | 12 |
| Chivot | Retro | 28 | 32 | 77 (70–92) | 79 (70–92) | 78.6% | 93.8% | 35.7% | 25% | Reattachment | Zimmer | 32 |
| Roberson | Retro | 20 | 19 | 71 (NR) | 71 (NR) | 95% | 78.9% | 75% | 21% | NR | DJO Zimmer | 29/53 ^ |
| 77 | 81 | |||||||||||
| Randomized Clinical Trials | Lopiz 2019 [14] | Retrospective Studies | Chivot 2018 [15] | Roberson 2017 [16] | |
|---|---|---|---|---|---|
| Clearly stated aim | 2 | 2 | 2 | ||
| Inclusion of consecutive patients | 2 | 2 | 1 | ||
| Prospective data collection | 2 | 1 | 0 | ||
| Appropriate endpoints | 2 | 2 | 1 | ||
| Unbiased assessment endpoints | 2 | 0 | 0 | ||
| Appropriate follow-up (>1 year) | 2 | 2 | 2 | ||
| Loss to follow-up <5% | 2 | 1 | 0 | ||
| Prospective calculation study size | 2 | 0 | 0 | ||
| Adequate control group | 2 | 2 | 2 | ||
| Contemporary groups | 2 | 2 | 2 | ||
| Baseline quivalence of groups | 2 | 2 | 2 | ||
| Adequate statistical analysis | 2 | 2 | 1 | ||
| Total score | 24 | 18 | 13 |
| Functional Outcome Score | Study | RSA | NOT | p-Value |
|---|---|---|---|---|
| CMS * | Lopiz et al. [14] | 61.7 | 55.7 | 0.07 |
| Chivot et al. [15] | 56.5 | 50.5 | 0.03 ^ | |
| DASH ** | Lopiz et al. [14] | 20.7 | 28.8 | 0.08 |
| Chivot et al. [15] | 38.7 | 31.2 | 0.11 | |
| PENN * | Roberson et al. [16] | 70 | 73 | 0.7 |
| ASES * | Roberson et al. [16] | 72 | 72 | 0.99 |
| Range of Motion | Study | RSA | NOT | p-Value |
|---|---|---|---|---|
| Forward flexion | Lopiz et al. [14] | 133 | 115 | 0.028 ^ |
| Chivot et al. [15] | 110 | 98 | 0.0005 ^ | |
| Roberson et al. [16] | 119 | 120 | 0.87 | |
| Weighted average | 120.8 | 109.8 | ||
| External rotation | Lopiz et al. * [14] | 5.2 | 4.4 | 0.293 |
| Chivot et al. [15] | 19 | 9 | 0.0002 ^ | |
| Roberson et al. [16] | 31 | 23 | 0.06 | |
| Internal rotation ** | Lopiz et al. [14] | 65% (41/24) | 48% (34/14) | 0.211 |
| Chivot et al. [15] | 46% (17/28) | 22% (9/13) | 0.04 ^ |
| RSA | NOT | |
|---|---|---|
| N | 77 | 81 |
| RSA complications | ||
| Dislocation | 2 (2.6%) | |
| Nerve injury | 2 (2.6%) | |
| Infection | 2 (2.6%) | |
| Iatrogenic fracture | 0 | |
| Anatomic greater tuberosity healing | 40 (52%) | |
| Greater tuberosity non-anatomic healing or resorption | 17 (22%) | |
| Scapular notching | 0 | |
| Baseplate loosening | 0 | |
| Humeral stem loosening | 0 | |
| Revision or subsequent operation | 4 (5.2%) | 0 |
| NOT complications | ||
| Osteonecrosis | 20 (24.7%) | |
| Malunion | 34 (42%) | |
| Nonunion | 2 (2.5%) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bosch, T.P.; Beeres, F.J.P.; Ferree, S.; Schipper, I.B.; Camenzind, R.S.; Hoepelman, R.J.; Link, B.-C.; Rompen, I.F.; Babst, R.; van de Wall, B.J.M. Reverse Shoulder Arthroplasty versus Non-Operative Treatment of Three-Part and Four-Part Proximal Humerus Fractures in the Elderly Patient: A Pooled Analysis and Systematic Review. J. Clin. Med. 2024, 13, 3344. https://doi.org/10.3390/jcm13113344
Bosch TP, Beeres FJP, Ferree S, Schipper IB, Camenzind RS, Hoepelman RJ, Link B-C, Rompen IF, Babst R, van de Wall BJM. Reverse Shoulder Arthroplasty versus Non-Operative Treatment of Three-Part and Four-Part Proximal Humerus Fractures in the Elderly Patient: A Pooled Analysis and Systematic Review. Journal of Clinical Medicine. 2024; 13(11):3344. https://doi.org/10.3390/jcm13113344
Chicago/Turabian StyleBosch, Thomas P., Frank J. P. Beeres, Steven Ferree, Inger B. Schipper, Roland S. Camenzind, Ruben J. Hoepelman, Björn-Christian Link, Ingmar F. Rompen, Reto Babst, and Bryan J. M. van de Wall. 2024. "Reverse Shoulder Arthroplasty versus Non-Operative Treatment of Three-Part and Four-Part Proximal Humerus Fractures in the Elderly Patient: A Pooled Analysis and Systematic Review" Journal of Clinical Medicine 13, no. 11: 3344. https://doi.org/10.3390/jcm13113344
APA StyleBosch, T. P., Beeres, F. J. P., Ferree, S., Schipper, I. B., Camenzind, R. S., Hoepelman, R. J., Link, B.-C., Rompen, I. F., Babst, R., & van de Wall, B. J. M. (2024). Reverse Shoulder Arthroplasty versus Non-Operative Treatment of Three-Part and Four-Part Proximal Humerus Fractures in the Elderly Patient: A Pooled Analysis and Systematic Review. Journal of Clinical Medicine, 13(11), 3344. https://doi.org/10.3390/jcm13113344






