Impact of the Coronavirus Pandemic on Patients Requiring Tracheal Intubation by Helicopter Emergency Medical Services: A Retrospective, Single-Center, Observational Study
Abstract
1. Introduction
2. Materials and Methods
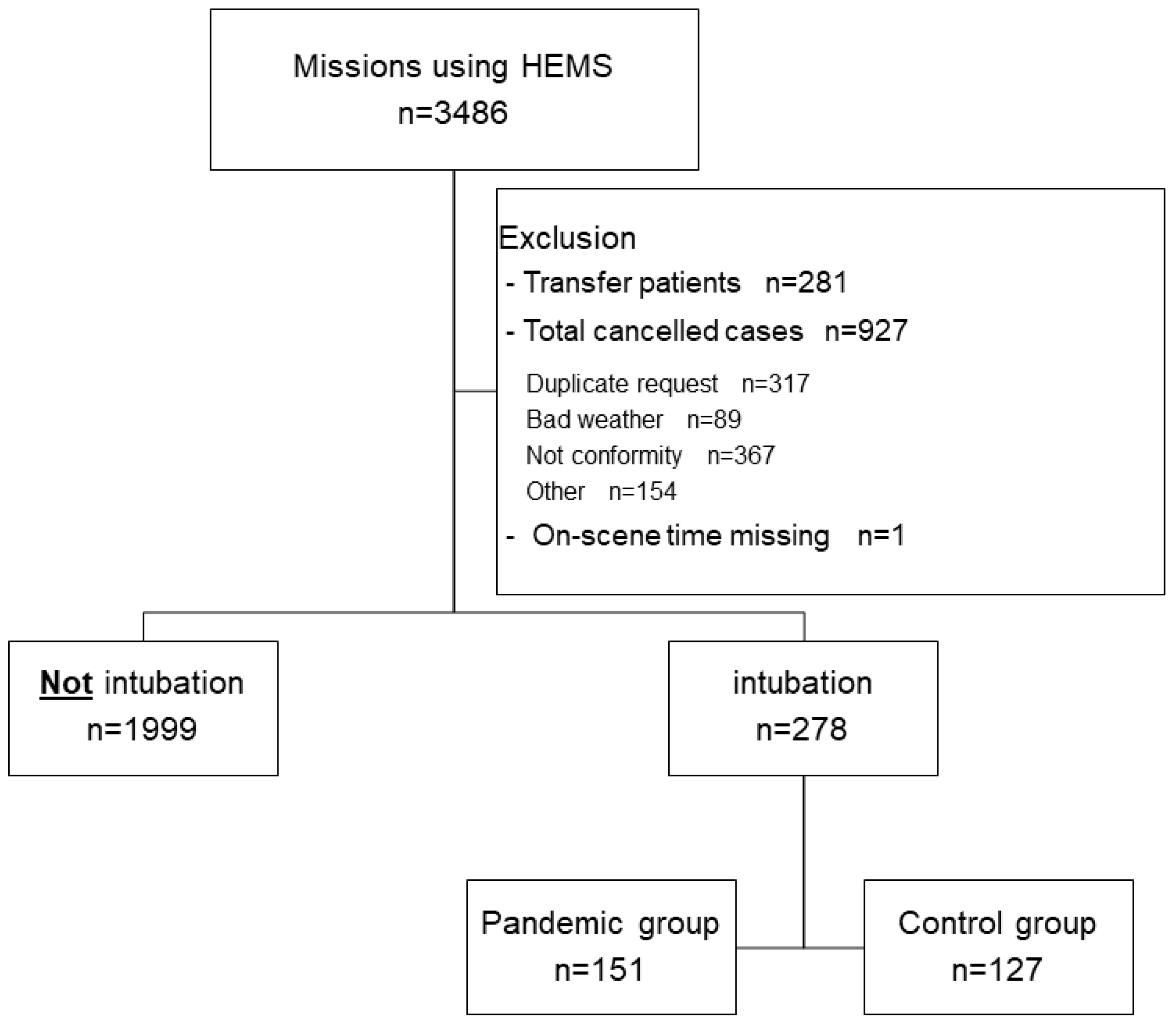
2.1. Study Design, Setting, Patient Selection
2.2. Main Exposure: COVID-19 Pandemic
2.3. Patient Background and Other HEMS Operation Characteristics
2.4. Outcomes
2.5. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Thomas, S.H.; Thomas, S.W.; Thomas, S.A.; Pathan, S. Helicopter emergency medical services literature 1972–2017: Characteristics and trends. Air Med. J. 2019, 38, 115–124. [Google Scholar] [CrossRef] [PubMed]
- Airbus. A History of Helicopter Emergency Medical Services. Available online: https://www.airbus.com/en/newsroom/stories/2020-12-a-history-of-helicopter-emergency-medical-services (accessed on 11 April 2024).
- Emergency Medical Network of Helicopter and Hospital (Nonprofit Organization). Doctor Helicopter Service Began in Japan after Overseas Countries. Available online: https://hemnet.jp/en-know-history (accessed on 11 April 2024).
- Wake, K.; Noguchi, T.; Hishinuma, H.; Zaitsu, M.; Kikuchi, J.; Uchida, M.; Hayashi, K.; Machida, M.; Houzumi, H.; Hoshiyama, E.; et al. Characteristics of patients who received helicopter emergency medical services in Japan from 2012 to 2019: A retrospective analysis of data from Tochigi Prefecture. Scand. J. Trauma Resusc. Emerg. Med. 2022, 30, 25. [Google Scholar] [CrossRef] [PubMed]
- Furuse, Y.; Ko, Y.K.; Saito, M.; Shobugawa, Y.; Jindai, K.; Saito, T.; Nishiura, H.; Sunagawa, T.; Suzuki, M.; Oshitani, H.; et al. Epidemiology of COVID-19 outbreak in Japan, from January–March 2020. Jpn. J. Infect. Dis. 2020, 73, 391–393. [Google Scholar] [CrossRef] [PubMed]
- Ohsaka, H.; Nagasawa, H.; Ota, S.; Muramatsu, K.I.; Jitsuiki, K.; Ishikawa, K.; Yanagawa, Y. Analysis of the activities of a physician-staffed helicopter in the coronavirus disease 2019 pandemic phase. Air Med. J. 2022, 41, 376–379. [Google Scholar] [CrossRef] [PubMed]
- Weissman, D.N.; de Perio, M.A.; Radonovich, L.J., Jr. COVID-19 and risks posed to personnel during endotracheal intubation. JAMA 2020, 323, 2027–2028. [Google Scholar] [CrossRef] [PubMed]
- Ross, A.M.; Lombardi, B.; Zerden, L.S. Introduction to the special issue: Social work practice in the era of the COVID-19 pandemic—Challenges and innovations. Soc. Work Health Care 2021, 60, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Mertens, G.; Lodder, P.; Smeets, T.; Duijndam, S. Fear of COVID-19 predicts vaccination willingness 14 months later. J. Anxiety Disord. 2022, 88, 102574. [Google Scholar] [CrossRef]
- Avery, P.; McAleer, S.; Rawlinson, D.; Gil, S.; Lockey, D. Maintaining prehospital intubation success with COVID-19 personal protective precautions. Prehosp. Disaster Med. 2022, 37, 783–787. [Google Scholar] [CrossRef] [PubMed]
- Stawicki, S.P.; Jeanmonod, R.; Miller, A.C.; Paladino, L.; Gaieski, D.F.; Yaffee, A.Q.; De Wulf, A.; Grover, J.; Papadimos, T.J.; Bloem, C.; et al. The 2019–2020 Novel Coronavirus (Severe Acute Respiratory Syndrome Coronavirus 2) Pandemic: A Joint American College of Academic International Medicine-World Academic Council of Emergency Medicine Multidisciplinary COVID-19 Working Group Consensus Paper. J. Glob. Infect. Dis. 2020, 12, 47–93. [Google Scholar] [CrossRef]
- Stawicki, S.P.; Brisendine, C.; Levicoff, L.; Ford, F.; Snyder, B.; Eid, S.; Worrilow, K.C. Comprehensive and Live Air Purification as a Key Environmental, Clinical, and Patient Safety Factor: A Prospective Evaluation. In Vignettes in Patient Safety; IntechOpen: London, UK, 2019; Volume 4. [Google Scholar] [CrossRef]
- Machida, M.; Koji, W. Public health responses to COVID-19 in Japan. Glob. Health Med. 2022, 4, 78–82. [Google Scholar] [CrossRef]
- Liu, Y.; Ning, Z.; Chen, Y.; Guo, M.; Liu, Y.; Gali, N.K.; Sun, L.; Duan, Y.; Cai, J.; Westerdahl, D.; et al. Aerodynamic analysis of SARS-CoV-2 in two Wuhan hospitals. Nature 2020, 582, 557–560. [Google Scholar] [CrossRef] [PubMed]
- Brown, J.; Gregson, F.K.A.; Shrimpton, A.; Cook, T.M.; Bzdek, B.R.; Reid, J.P.; Pickering, A.E. A quantitative evaluation of aerosol generation during tracheal intubation and extubation. Anesthesia 2021, 76, 174–181. [Google Scholar] [CrossRef] [PubMed]
- Dhillon, R.S.; Rowin, W.A.; Humphries, R.S.; Kevin, K.; Ward, J.D.; Phan, T.D.; Nguyen, L.V.; Wynne, D.D.; Scott, D.A.; Clinical Aerosolisation Study Group. Aerosolisation during tracheal intubation and extubation in an operating theatre setting. Anaesthesia 2021, 76, 182–188. [Google Scholar] [CrossRef] [PubMed]
- Tran, D.T.; Newton, E.K.; Mount, V.A.; Lee, J.S.; Wells, G.A.; Perry, J.J. Rocuronium versus succinylcholine for rapid sequence induction intubation. Cochrane Database Syst. Rev. 2015, 2015, CD002788. [Google Scholar] [CrossRef] [PubMed]
- Welch, J.L.; Seupaul, R.A. Update: Does rocuronium create better intubating conditions than succinylcholine for rapid sequence intubation? Ann. Emerg. Med. 2017, 69, e55–e56. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Black, H.; Hall, T.; Hrymak, C.; Funk, D.; Siddiqui, F.; Sokal, J.; Satoudian, J.; Foster, K.; Kowalski, S.; Dufault, B.; et al. A prospective observational study comparing outcomes before and after the introduction of an intubation protocol during the COVID-19 pandemic. CJEM 2023, 25, 123–133. [Google Scholar] [CrossRef] [PubMed]
- Jang, W.; Kang, H.; Shin, H.; Kim, C.; Lee, H.; Choi, H. Introduction of infection prevention tracheal intubation protocol during the COVID-19 pandemic is not associated with first-pass success rates of endotracheal intubation in the emergency department: A before-and-after comparative study. J. Pers. Med. 2023, 13, 1017. [Google Scholar] [CrossRef] [PubMed]
- McKeage, K.; Perry, C.M. Propofol: A review of its use in intensive care sedation of adults. CNS Drugs 2003, 17, 235–272. [Google Scholar] [CrossRef] [PubMed]
- Schmidt, M.; Pedersen, L.; Sørensen, H.T. The Danish Civil Registration System as a tool in epidemiology. Eur. J. Epidemiol. 2014, 29, 541–549. [Google Scholar] [CrossRef]
- Andruszkow, H.; Schweigkofler, U.; Lefering, R.; Frey, M.; Horst, K.; Pfeifer, R.; Beckers, S.K.; Pape, H.C.; Hildebrand, F. Impact of Helicopter Emergency Medical Service in Traumatized Patients: Which Patient Benefits Most? PLoS ONE 2016, 15, e0146897. [Google Scholar] [CrossRef]
- Galvagno, S.M., Jr.; Sikorski, R.; Hirshon, J.M.; Floccare, D.; Stephens, C.; Beecher, D.; Thomas, S. Helicopter emergency medical services for adults with major trauma. Cochrane Database Syst. Rev. 2015, 15, CD009228. [Google Scholar] [CrossRef] [PubMed]
- Tsuchiya, A.; Tsutsumi, Y.; Yasunaga, H. Outcomes after helicopter versus ground emergency medical services for major trauma—Propensity score and instrumental variable analyses: A retrospective nationwide cohort study. Scand. J. Trauma Resusc. Emerg. Med. 2016, 24, 140. [Google Scholar] [CrossRef] [PubMed]
- Ota, S.; Jitsuiki, K.; Muramatsu, K.; Kushida, Y.; Nagasawa, H.; Yasuda, K.; Ohsaka, H.; Omori, K.; Yanagawa, Y. Analysis of the dispatch of physician staffed-helicopters in the COVID-19 pandemic. Am. J. Emerg. Med. 2022, 54, 306–308. [Google Scholar] [CrossRef] [PubMed]
- Yasin, Y.J.; Grivna, M.; Abu-Zidan, F.M. Global impact of COVID-19 pandemic on road traffic collisions. World J. Emerg. Surg. 2021, 16, 51. [Google Scholar] [CrossRef] [PubMed]
- Shimizu, K.; Ueda, P.; Ghaznavi, C.; Sakamoto, H.; Nomura, S. Assessment of traffic accidents in Japan during the COVID-19 pandemic vs. previous years: A preliminary report. Healthcare 2022, 10, 860. [Google Scholar] [CrossRef]
- Lossius, H.M.; Røislien, J.; Lockey, D.J. Patient safety in pre-hospital emergency tracheal intubation: A comprehensive meta-analysis of the intubation success rates of EMS providers. Crit. Care 2012, 16, R24. [Google Scholar] [CrossRef]
- Stassen, W.; Lithgow, A.; Wylie, C.; Stein, C. A descriptive analysis of endotracheal intubation in a South African Helicopter Emergency Medical Service. Afr. J. Emerg. Med. 2018, 8, 140–144. [Google Scholar] [CrossRef]

| Total | Control Group | Pandemic Group | p-Value | |
|---|---|---|---|---|
| N = 278 | n = 151 | n = 127 | ||
| Age (years), mean ± SD | 61.05 ± 20.23 | 60.46 ± 20.80 | 61.76 ± 19.58 | 0.595 |
| Sex (male), n (%) | 189 (68.0) | 103 (68.2) | 86 (67.7) | 0.930 |
| Number of physicians (mean ± SD) | 1.53 ± 0.50 | 1.50 ± 0.50 | 1.57 ± 0.50 | 0.244 |
| Pre-hospital severity, n (%) | 0.831 | |||
| Mild | 0 (0.0) | 0 (0.0) | 0 (0.0) | |
| Moderate | 16 (5.8) | 9 (6.0) | 7 (5.5) | |
| Severe | 258 (92.8) | 140 (92.7) | 118 (92.9) | |
| Death | 2 (0.7) | 1 (0.7) | 1 (0.8) | |
| Missing | 2 (0.7) | 1 (0.7) | 1 (0.8) | |
| Diagnosis, n (%) | 0.808 | |||
| Trauma | 82 (29.5) | 48 (31.8) | 34 (26.8) | |
| Neurology | 24 (8.6) | 16 (10.6) | 8 (6.3) | |
| Cardiovascular disease | ||||
| Ischemic heart disease | 10 (3.6) | 7 (4.6) | 3 (2.4) | |
| Aortic disease | 9 (3.2) | 4 (2.6) | 5 (3.9) | |
| Stroke | 63 (22.7) | 31 (20.5) | 32 (25.2) | |
| Others | 8 (2.9) | 4 (2.6) | 4 (3.1) | |
| Cardiopulmonary arrest | 54 (19.4) | 26 (17.2) | 28 (22) | |
| Respiratory disease | 5 (1.8) | 3 (2.0) | 2 (1.6) | |
| Gastroenterology | 0 (0.0) | 0 (0.0) | 0 (0.0) | |
| Allergies | 2 (0.7) | 1 (0.7) | 1 (0.8) | |
| Toxicosis | 4 (1.4) | 3 (2.0) | 1 (0.8) | |
| Other disease | 17 (6.1) | 8 (5.3) | 9 (7.1) | |
| Vital signs | ||||
| GCS score, n (%) | 0.143 | |||
| 3–8 | 230 (82.7) | 119 (78.8) | 111 (87.4) | |
| 9–13 | 29 (10.4) | 19 (12.6) | 10 (7.9) | |
| 14–15 | 17 (6.1) | 12 (7.9) | 5 (3.9) | |
| Missing | 2 (0.7) | 1 (0.7) | 1 (0.8) | |
| BP < 80 mmHg, n (%) | 63 (22.7) | 40 (26.5) | 23 (18.1) | 0.096 |
| Missing | 0 (0.0) | 0 (0.0) | 0 (0.0) | |
| HR > 130 bpm, n (%) | 62 (22.3) | 27 (17.9) | 35 (27.6) | 0.053 |
| Missing | 0 (0.0) | 0 (0.0) | 0 (0.0) | |
| SpO2 < 80%, n (%) | 7 (2.5) | 3 (2.0) | 4 (3.1) | 0.613 |
| Missing | 35 (12.6) | 24 (15.9) | 11 (8.7) | |
| RR > 35 or <8 breaths/min, n (%) | 106 (38.1) | 59 (39.1) | 47 (37.0) | 0.724 |
| Missing | 0 (0.0) | 0 (0.0) | 0 (0.0) | |
| O2 administration, n (%) | 246 (88.5) | 134 (88.7) | 112 (88.2) | 0.622 |
| Missing | 13 (4.7) | 6 (4.0) | 7 (5.5) | |
| BT (°C), mean ± SD | 36.67 ± 2.25 | 36.67 ± 2.29 | 36.67 ± 2.24 | 0.997 |
| Missing | 131 (47.1) | 86 (57.0) | 45 (35.4) |
| Total | Control | Pandemic | p-Value | |
|---|---|---|---|---|
| n = 278 | n = 151 | n = 127 | ||
| Interval (min), mean ± SD | ||||
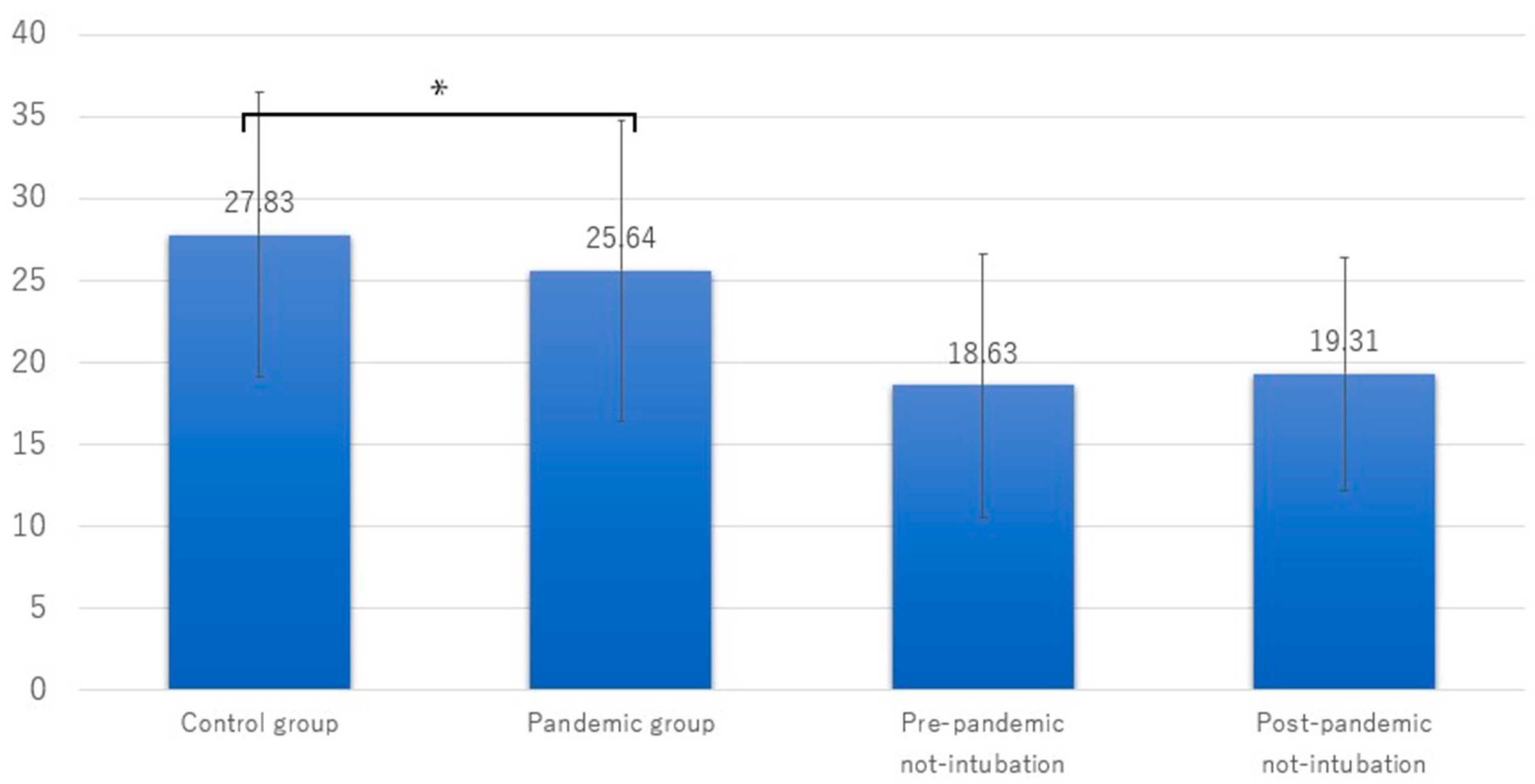
| Phase 2 (on-scene time) | 26.83 ± 9.00 | 27.83 ± 8.74 | 25.64 ± 9.19 | 0.043 |
| Drugs used, n (%) | ||||
| Propofol | 124 (44.6) | 65 (43) | 59 (46.5) | 0.569 |
| Midazolam | 49 (17.6) | 34 (22.5) | 15 (11.8) | 0.020 |
| Rocuronium bromide | 46 (16.5) | 9 (6.0) | 37 (29.1) | <0.001 |
| Buprenorphine hydrochloride | 10 (3.6) | 6 (4.0) | 4 (3.1) | 0.759 |
| Ketamine | 18 (6.5) | 12 (7.9) | 6 (4.7) | 0.277 |
| Other interventions, n (%) | ||||
| Intravenous drip | 270 (97.1) | 149 (98.7) | 121 (95.3) | 0.148 |
| Oxygen administration | 249 (89.6) | 139 (92.1) | 110 (86.6) | 0.139 |
| Ultrasound examination | 192 (69.1) | 109 (72.2) | 83 (65.4) | 0.220 |
| Pleural drainage | 13 (4.7) | 8 (5.3) | 5 (3.9) | 0.777 |
| Chest compression | 42 (15.1) | 19 (12.6) | 23 (18.1) | 0.200 |
| External defibrillation | 38 (13.7) | 21 (13.9) | 17 (13.4) | 0.900 |
| Type of transportation, n (%) | 0.056 | |||
| To the base hospital by HEMS with physician | 152 (54.7) | 82 (54.3) | 70 (55.1) | |
| To the base hospital by GEMS with physician | 15 (5.4) | 3 (2.0) | 12 (9.4) | |
| To another hospital by HEMS with physician | 91 (32.7) | 56 (37.1) | 35 (27.6) | |
| To another hospital by GEMS with physician | 14 (5.0) | 7 (4.6) | 7 (5.5) | |
| To another hospital by GEMS without physician | 5 (1.8) | 3 (2.0) | 2 (1.6) | |
| Missing | 1 (0.4) | 0 (0.0) | 1 (0.8) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hayashi, K.; Kikuchi, J.; Hishinuma, H.; Noguchi, T.; Zaitsu, M.; Wake, K. Impact of the Coronavirus Pandemic on Patients Requiring Tracheal Intubation by Helicopter Emergency Medical Services: A Retrospective, Single-Center, Observational Study. J. Clin. Med. 2024, 13, 3694. https://doi.org/10.3390/jcm13133694
Hayashi K, Kikuchi J, Hishinuma H, Noguchi T, Zaitsu M, Wake K. Impact of the Coronavirus Pandemic on Patients Requiring Tracheal Intubation by Helicopter Emergency Medical Services: A Retrospective, Single-Center, Observational Study. Journal of Clinical Medicine. 2024; 13(13):3694. https://doi.org/10.3390/jcm13133694
Chicago/Turabian StyleHayashi, Kentaro, Jin Kikuchi, Hidekazu Hishinuma, Takafumi Noguchi, Masayoshi Zaitsu, and Koji Wake. 2024. "Impact of the Coronavirus Pandemic on Patients Requiring Tracheal Intubation by Helicopter Emergency Medical Services: A Retrospective, Single-Center, Observational Study" Journal of Clinical Medicine 13, no. 13: 3694. https://doi.org/10.3390/jcm13133694
APA StyleHayashi, K., Kikuchi, J., Hishinuma, H., Noguchi, T., Zaitsu, M., & Wake, K. (2024). Impact of the Coronavirus Pandemic on Patients Requiring Tracheal Intubation by Helicopter Emergency Medical Services: A Retrospective, Single-Center, Observational Study. Journal of Clinical Medicine, 13(13), 3694. https://doi.org/10.3390/jcm13133694






