Dry Needling and Acupuncture for Scars—A Systematic Review
Abstract
:1. Introduction
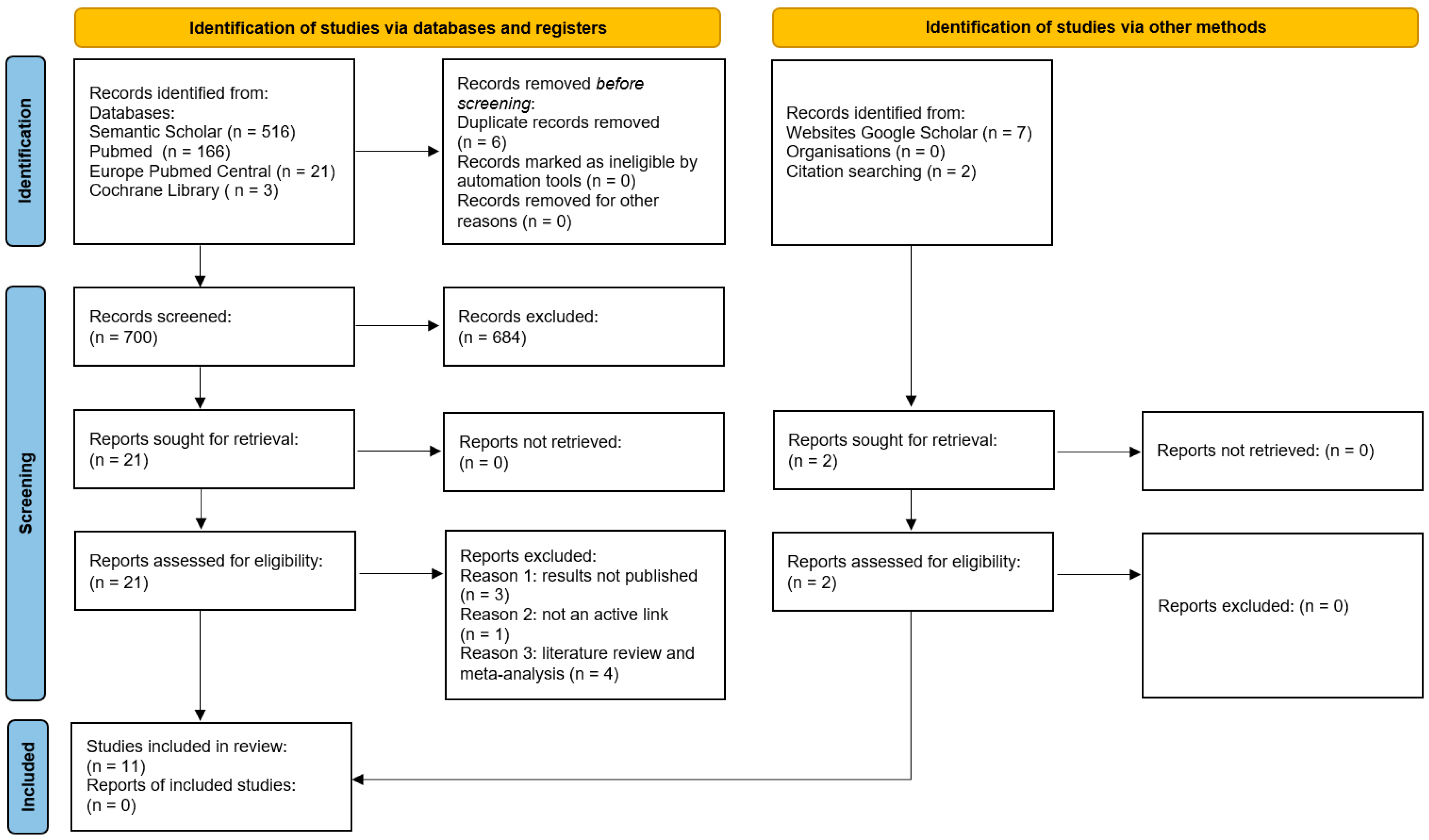
2. Materials and Methods
2.1. Registration
2.2. Eligibility Criteria
2.3. Information Sources
2.4. Search Strategy
2.5. Selection Process
2.6. Data Collection Process
2.7. Risk of Bias Assessment
2.8. Data Elements
2.9. Data Synthesis Methods
3. Results
4. Discussion
5. Limitations
6. Conclusions
7. Supporting Data
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Amici, J.M.; Taïeb, C.; LeFloc’h, C.; Demessant-Flavigny, A.L.; Seité, S.; Cogrel, O. Prevalence of scars: An international epidemiological survey in adults. J. Eur. Acad. Dermatol. Venereol. 2022, 36, e799. [Google Scholar] [CrossRef]
- Bahramian, M.; Dabbaghipour, N.; Aria, A.; Tehrani, B.S.M.F.; Dommerholt, J. Efficacy of Dry Needling in Treating Scars following Total Hip Arthroplasty: A Case Report. Med. J. Islam. Repub. Iran 2022, 36, 1208–1212. [Google Scholar] [CrossRef]
- Tuckey, C.R.; Kohut, S.H.; Edgar, D.W. Case study: Pilot testing of a local acupuncture intervention protocol for burn scars. Scars Burn. Heal. 2022, 8, 205951312110584. [Google Scholar] [CrossRef]
- Skochdopole, A.; Dibbs, R.P.; Sarrami, S.M.; Dempsey, R.F. Scar Revision. Semin. Plast. Surg. 2023, 35, 130–138. [Google Scholar] [CrossRef]
- Rei, O. Keloids and Hypertrophic Scars-UpToDate. UpToDate. 2024. Available online: https://www.uptodate.com/contents/keloids-and-hypertrophic-scars (accessed on 4 June 2024).
- Mathew-Steiner, S.S.; Roy, S.; Sen, C.K. Collagen in Wound Healing. Bioengineering 2021, 8, 63. [Google Scholar] [CrossRef]
- Berman, B.; Maderal, A.; Raphael, B. Keloids and Hypertrophic Scars: Pathophysiology, Classification, and Treatment. Dermatol. Surg. 2017, 43 (Suppl. 1), S3–S18. [Google Scholar] [CrossRef]
- Lin, J.-G.; Kotha, P.; Chen, Y.-H. Understandings of acupuncture application and mechanisms. Am. J. Transl. Res. 2022, 14, 1469–1481. Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8991130/ (accessed on 4 June 2024).
- Rapson, L.M. Acupuncture for Pain Management. Available online: https://www.medscape.com/viewarticle/573858?scode=msp&st=fpf&anfErrHint=true&icd=login_error_gg_mismatch_fpf&client=205502&urlCache=aHR0cHM6Ly93d3cubWVkc2NhcGUuY29tL3ZpZXdhcnRpY2xlLzU3Mzg1OD9mb3JtPWZwZiZzY29kZT1tc3Amc3Q9ZnBmJnNvY2lhbFNpdGU9Z29vZ2xl&su=l0YnKRHNuckw7hIxcbf5lFZLGoZsw5IxoCJP5K6ch1yJLdxgctZMydvbLLaTNBiq&form=fpf (accessed on 4 June 2024).
- Dunning, J.; Butts, R.; Mourad, F.; Young, I.; Flannagan, S.; Perreault, T. Dry needling: A literature review with implications for clinical practice guidelines. Phys. Ther. Rev. 2014, 19, 252–265. [Google Scholar] [CrossRef]
- Boyles, R.; Fowler, R.; Ramsey, D.; Burrows, E. Effectiveness of trigger point dry needling for multiple body regions: A systematic review. J. Man. Manip. Ther. 2015, 23, 276–292. [Google Scholar] [CrossRef]
- Unverzagt, C.; Berglund, K.; Thomas, J.J. DRY needling for myofascial trigger point pain: A clinical commentary. Int. J. Sports Phys. Ther. 2015, 10, 402–418. Available online: https://pubmed.ncbi.nlm.nih.gov/26075156/ (accessed on 4 June 2024).
- Kalichman, L.; Vulfsons, S. Dry needling in the management of musculoskeletal pain. J. Am. Board Fam. Med. 2010, 23, 640–646. [Google Scholar] [CrossRef] [PubMed]
- Gattie, E.; Cleland, J.A.; Snodgrass, S. The Effectiveness of Trigger Point Dry Needling for Musculoskeletal Conditions by Physical Therapists: A Systematic Review and Meta-analysis. J. Orthop. Sports Phys. Ther. 2017, 47, 133–149. [Google Scholar] [CrossRef] [PubMed]
- Sandberg, M.; Lundeberg, T.; Lindberg, L.G.; Gerdle, B. Effects of acupuncture on skin and muscle blood flow in healthy subjects. Eur. J. Appl. Physiol. 2003, 90, 114–119. [Google Scholar] [CrossRef] [PubMed]
- Rozenfeld, E.; Sebakhutu, E.S.; Krieger, Y.; Kalichman, L. Dry needling for scar treatment. Acupunct. Med. 2020, 38, 435–439. [Google Scholar] [CrossRef] [PubMed]
- Ishak, A.; Jusuf, A.A.; Simadibrata, C.L.; Barasila, A.C.; Novita, R. Effect of Manual Acupuncture and Laser Acupuncture on Wound Closure in Rat with Deep Partial Thickness Burn Injury. Med. Acupunct. 2022, 34, 240–250. [Google Scholar] [CrossRef] [PubMed]
- Abali, A.E.; Cabioglu, T.; Bayraktar, N.; Ozdemir, B.H.; Moray, G.; Haberal, M. Efficacy of Acupuncture on Pain Mechanisms, Inflammatory Responses, and Wound Healing in the Acute Phase of Major Burns: An Experimental Study on Rats. J. Burn Care Res. 2022, 43, 389–398. [Google Scholar] [CrossRef] [PubMed]
- Han, S. The role of mechanoreceptors in acupuncture. Med. Nov. Technol. Devices 2023, 17, 100207. [Google Scholar] [CrossRef]
- Chmielewska, D.; Malá, J.; Opala-Berdzik, A.; Nocuń, M.; Dolibog, P.; Dolibog, P.T.; Stania, M.; Kuszewski, M.; Kobesova, A. Acupuncture and dry needling for physical therapy of scar: A systematic review. BMC Complement. Med. Ther. 2024, 24, 1–16. [Google Scholar] [CrossRef]
- Michalska, A.; Mierzwa-Molenda, M.; Bielasik, K.; Pogorzelska, J.; Wolder, D.P.; Swiercz, G. Optimization of the cosmetic appearance of skin scar after caesarean section—Part II physiotherapy practice. Ginekol. Pol. 2024, 95, 156–166. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- Higgins, J.P.T.; Thomas, J.; Chandler, J.; Cumpston, M.; Li, T.; Page, M.J.; Welch, V.A. Cochrane Handbook for Systematic Reviews of Interventions, 2nd ed.; John Wiley & Sons: Chichester, UK, 2019. [Google Scholar]
- Anderson, A.F. Acupuncture in the treatment of scar tissue following surgery for Dupuytren’s contracture. J. Acupunct. Assoc. Chart. Physiother. 2014, 30, 73–78. Available online: https://scholar.google.com/scholar_lookup?journal=J+Acupunct+Assoc+Chart+Physiother&title=Acupuncture+in+the+treatment+of+scar+tissue+following+Surgery+for+Dupuytren’s+contracture&author=F+Anderson&volume=30&publication_year=2014&pages=73-8& (accessed on 4 June 2024).
- Huang, H.; Liu, J.; Fu, M.; Lin, I.W.; Chou, L.W. Fu’s subcutaneous needling for subcutaneous adhesions and scar hyperplasia in the neck region: A case report. Medicine 2020, 99, e21103. [Google Scholar] [CrossRef] [PubMed]
- Pourahmadi, M.A.M. The Effectiveness of Dry Needling in Treating Linear Hypertrophic Scar Tissue: A Randomized Sham-Controlled Trial. In ClinicalTrials.gov IR.IUMS.REC.1401.540; 2023. Available online: https://clinicaltrials.gov/study/NCT06033430 (accessed on 8 June 2024).
- Liu, Y.-H.; Xiang, J.; Han, P.-P.; Yang, C.; Wang, Y.-Z.; Wang, W.; Zhang, P.-A. Clinical observation for acupuncture treatment of a small area of hyperplastic scars in young and middle-aged women. Medicine 2020, 99, e20790. [Google Scholar] [CrossRef] [PubMed]
- Dale, E.L.; Hultman, C.S. Patient Safety in Burn Care: Application of Evidence-based Medicine to Improve Outcomes. Clin. Plast. Surg. 2017, 44, 611–618. [Google Scholar] [CrossRef] [PubMed]
- Hunter, J. Acupuncture for keloid scar. Acupunct. Med. 2011, 29, 2. [Google Scholar] [CrossRef] [PubMed]
- Lubczyńska, A.; Garncarczyk, A.; Wcisło-Dziadecka, D. Effectiveness of various methods of manual scar therapy. Skin Res. Technol. 2023, 29, 3. [Google Scholar] [CrossRef] [PubMed]
- Tuckey, C.; Kohut, S.; Edgar, D.W. Efficacy of acupuncture in treating scars following tissue trauma. Scars Burn. Heal. 2019, 5, 205951311983191. [Google Scholar] [CrossRef] [PubMed]
- Kotani, N.; Kushikata, T.; Suzuki, A.; Hashimoto, H.; Muraoka, M.; Matsuki, A. Insertion of Intradermal Needles Into Painful Points Provides Analgesia for Intractable Abdominal Scar Pain. Reg. Anesth. Pain Med. 2001, 26, 532–538. [Google Scholar] [CrossRef] [PubMed]
- Bintoro, D.A.; Helianthi, D.R. Combination of Battlefield Acupuncture and Local Point Acupuncture for Post Laparotomy Scar Pain. Med. Acupunct. 2022, 34, 66–70. [Google Scholar] [CrossRef]
- Fang, S. The successful treatment of pain associated with scar tissue using acupuncture. J. Acupunct. Meridian Stud. 2014, 7, 262–264. [Google Scholar] [CrossRef]
- Khan, K. Dry Needling a Novel Treatment Option for Post-scar Neuralgia: A Case Report. J. Recent Adv. Pain 2019, 5, 29–31. [Google Scholar] [CrossRef]
- Song, H.; Mu, J.; Wang, J. Clinical study on treatment of hypertrophic scar by acupuncture. J. Acupunct. Tuina Sci. 2011, 9, 159–161. [Google Scholar] [CrossRef]
- Tuck, C.M. A 54-year-old woman with degenerative back pain. Acupunct. Med. 2010, 28, 46–48. [Google Scholar] [CrossRef]
- Wang, M.; Liu, L.; Zhang, C.S.; Liao, Z.; Jing, X.; Fishers, M.; Zhao, L.; Xu, X.; Li, B. Mechanism of Traditional Chinese Medicine in Treating Knee Osteoarthritis. J. Pain Res. 2020, 13, 1421. [Google Scholar] [CrossRef] [PubMed]
- Li, P.; Luo, C.; Xu, Y.; Xu, D. Effect of acupuncture therapy on VEGF and endostatin in hypertrophic scar. Jiangsu Med. J. 2010, 16, 1888–1891. [Google Scholar] [CrossRef]
- Wilgus, T.A. Vascular Endothelial Growth Factor and Cutaneous Scarring. Adv. Wound Care 2019, 8, 671. [Google Scholar] [CrossRef]
- Liddle, C.E.; Harris, R.E. Cellular Reorganization Plays a Vital Role in Acupuncture Analgesia. Med. Acupunct. 2018, 30, 15. [Google Scholar] [CrossRef]
- Wang, B.G.; Xu, L.L.; Yang, H.Y.; Xie, J.; Xu, G.; Tang, W.C. Manual acupuncture for neuromusculoskeletal disorders: The selection of stimulation parameters and corresponding effects. Front. Neurosci. 2023, 17, 1096339. [Google Scholar] [CrossRef] [PubMed]
- Potenzieri, C.; Undem, B.J. Basic Mechanisms of Itch. Clin. Exp. Allergy 2012, 42, 8–19. [Google Scholar] [CrossRef]
- PDQ Integrative, Alternative, and Complementary Therapies Editorial Board. Acupuncture (PDQ®): Health Professional Version. In PDQ Cancer Information Summaries; National Cancer Institute (US): Bethesda, MD, USA, 2002. [Google Scholar] [PubMed]
- Chang, S.; Kwon, O.S.; Bang, S.K.; Kim, D.-H.; Baek, M.W.; Ryu, Y.; Bae, J.H.; Fan, Y.; Lee, S.M.; Kim, H.K.; et al. Peripheral sensory nerve tissue but not connective tissue is involved in the action of acupuncture. Front. Neurosci. 2019, 13, 110. [Google Scholar] [CrossRef]
- Langevin, H.M.; Yandow, J.A. Relationship of acupuncture points and meridians to connective tissue planes. Anat. Rec. 2002, 269, 257–265. [Google Scholar] [CrossRef] [PubMed]
- MacPherson, H.; Altman, D.G.; Hammerschlag, R.; Youping, L.; Taixiang, W.; White, A.; Moher, D.; on behalf of the STRICTA Revision Group. Revised standards for reporting interventions in clinical trials of acupuncture (stricta): Extending the consort statement. PLoS Med. 2010, 7, e1000261. [Google Scholar] [CrossRef] [PubMed]


| Name of the Author and Year | DN | ACU | ACU and DN or Else | |
|---|---|---|---|---|
| 1 | Bahramian, 2022 [2] | case report | ||
| 2 | Chmielewska, 2024 [20] | meta-analysis | ||
| 3 | Rozenfeld, 2020 [16] | literature review | ||
| 4 | Dunning, 2014 [10] | literature review | ||
| 5 | Pourahmadi, 2023 [26] | results not published | ||
| 6 | Lubczyńska, 2023 [30] | case series | ||
| 7 | Tuckey, 2019 [31] | literature review | ||
| 8 | Tuckey, 2022 [3] | case report | ||
| 9 | Kotani, 2001 [32] | RCT | ||
| 10 | Huang, 2020 [25] | Fu’s subcutaneous needling, case report | ||
| 11 | Bintoro, 2022 [33] | case report | ||
| 12 | Fang, 2014 [34] | case report | ||
| 13 | Liu, 2020 [27] | results not published | ||
| 14 | Khan, 2019 [35] | case report | ||
| 15 | Song, 2011 [36] | RCT | ||
| 16 | Dale, 2017 [28] | no results | ||
| 17 | Tuck, 2010 [37] | case report | ||
| 18 | Anderson, 2014 [24] | case report | ||
| 19 | Hunter, 2011 [29] | not an active link |
| Name of the Author and Year | A | B | C | D | E | F | G | H | ST |
|---|---|---|---|---|---|---|---|---|---|
| Bahramian, 2022 [2] | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 7 |
| Huang, 2020 [25] | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 7 |
| Bintoro, 2022 [33] | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 7 |
| Fang, 2014 [34] | 1 | 0 | 1 | 1 | 1 | 0 | 0 | 1 | 5 |
| Khan, 2019 [35] | 1 | 1 | 1 | 1 | 0 | 0 | 0 | 0 | 4 |
| Tuck, 2010 [37] | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 7 |
| Anderson, 2014 [24] | 1 | 1 | 1 | 1 | 0 | 1 | 0 | 1 | 6 |
| Tuckey, 2022 [3] | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 8 |
| Name of the Author and Year | A | B | C | D | E | F | G | H | I | J | ST |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Lubczyńska, 2023 [30] | 1 | 1 | 1 | 0 | 0 | 0 | 1 | 1 | 0 | 1 | 6 |
| Name of the Author and Year | A | B | C | D | E | F | G | H | I | J | K | ST |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Kotani, 2001 [32] | 1 | 1 | 1 | 1 | 0 | 0 | 1 | 1 | 1 | 1 | 1 | 8 |
| Song, 2011 [36] | 1 | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 0 | 5 |
| Name of the Author, Year, Type of Research | Type of Scar | Study Objectives | Intervention |
|---|---|---|---|
| Bahramian, 2022 [2], case reports | Mature scar after hip joint surgery, longitudinal scar on the right measuring 51 × 4.8 cm, pink, firm, very sensitive to touch; on the left—38 × 3.6 cm, 2 months | Assessment of the effectiveness of DN in the treatment of scars regarding pain, range of motion, and functionality after hip joint replacement. | The needle 0.30 × 50 mm was inserted into the scar area, needles sized 0.25 × 25 mm were positioned above the proximal border of the scar strip at angles of 15° to 30° perpendicular to the surface of the scar. The needle was moved back and forth 2–3 times per session, 2 times/week for 3 weeks, for 30 min. Additionally, infrared radiation was applied for 20 min at a distance of 40 cm away from the body. |
| Tuckey, 2022 [3], case reports | Hypertrophic burn scar (pain, itching), skin graft on the left lateral surface of the chest, 3 months | Evaluation of clinical outcomes using local ACU for treating scar symptoms in a patient who has already recovered from a burn injury. | 5 min of scar massage and 15 min of ACU, 12 sessions over 7 weeks. A maximum of 20 needles, each 2 cm around the scar, were inserted subcutaneously to a depth of 10 mm at a 45° angle, with the 20 mm needle shaft inserted at an angle under the edge of the scar. A maximum of 20 needles, each 2 cm around the scar, were inserted subcutaneously to a depth of 10 mm around the scar, positioned at a 45° angle. Additionally, a needle shaft measuring 20 mm was inserted beneath the edge of the scar at an angle. |
| Huang, 2020 [25], case reports | Curved surgical incision, 15 cm in length, with significant scarring on the neck, 8 years | Report a case of subcutaneous adhesions and scar tissue on the neck. | The doctor selected the “taut muscle” and inserted a needle into the taut subcutaneous tissue, either parallel or perpendicular to the muscle fibers. The needle was secured, and a “rocking motion” was performed for 2 min at a 40° angle, during which the patient actively or passively contracted the affected muscle. Treatment was administered 2–3 times per week for 1 month. |
| Bintoro, 2022 [33], case reports | Transverse dark-brown firm scar at the midlevel between the xiphoid process and the navel, measuring 30 × 0.3 cm, following laparoscopy, 4 years | Evaluate the effectiveness of the combination of BFA and ACU for treating scar pain after laparotomy. | ACU using BFA points on the ears, additional needles 0.15 × 15 mm were placed along the scar at a depth of 1–2 mm without further manual or electrical stimulation; for 12 sessions over 8 weeks, 30 min each. |
| Fang, 2014 [34], case reports | Surgical scar at the upper part of the right thigh along the gallbladder channel, 3 inches in length, 1/4 inch in width, red in color, and firm and hard, 1 year | Demonstrate the analgesic properties of ACU in scars. | Needles were used for insertion into local points: Wei Ci (8 needles at a 45° angle into the scar area), Hegu-LI-4, Taichong-LIV-3 (perpendicular to a depth of half cun, without De Qi sensation), and Zusanli-ST-36 (perpendicular to a depth of 1 cun, rapidly turning back and forth), 2/3 weeks, then 1/week for 2 weeks. Needles were single-use and remained in the body for 20 min for each procedure; 8 sessions over 5 weeks, 0.20 mm × 40 mm. |
| Khan, 2019 [35], case reports | Scar on the left thigh, 8 years | Present the treatment of DN for postscar neuralgia. | 8 sessions of 1 h each, needles inserted into the scar tissue and around it. |
| Tuck, 2010 [37], case reports | Scar after mastectomy, 4 months | Assessing the effectiveness of acupuncture in managing lower back pain and neuropathic scar pain. | 6 needles, with sizes of 0.16 × 30 mm, inserted perpendicular to the skin at a depth of 0.5 mm, 1–2 inches away from the scar line after mastectomy, using the “dragon surrounding” technique, for 30 min. Morphine per os 1 session. |
| Anderson, 2014 [24], case reports | Postoperative keloid scar on the palm of the right hand, 5 weeks | Present the impact of ACU on the postoperative scar. | Support points are located extrasegmentally. Over 3 months, 7 procedures involved inserting needles into the scar tissue for 20 min each. With ACU, ultrasound, stretching exercises, and splinting were applied. Needle sizes used: 0.20 × 40 mm, 0.3 × 50 mm. |
| Kotani, 2001 [32], RCT | Surgical scar ≥ 12 weeks | Testing the hypothesis that the introduction of intradermal needles reduces pain in scar tissue. | In the main group (n = 23), needles were inserted into painful areas, as determined using a pressure device (pain ≤ 2.5 kg/cm2). In the sham treatment group (n = 23), needles were inserted into nonpainful points, and in the control group (n = 24), no needles were inserted. Needles (0.16 mm × 5 mm) were left in throughout the day for a total of 20 sessions over 4 weeks. Diclofenac was taken as needed. |
| Song, 2011 [36], RCT | Hypertrophic scars on the abdomen, chest, limbs, and face, from 3 months to 4 years | To observe the outcomes of acupuncture therapy on scars. | Main group (n = 40) ACU + ultrasound therapy, control group (n = 40) Mebo Scareducer ointment + ultrasound therapy. Needles: 0.30 × 40–60 mm, inserted subcutaneously near the scars/around them; needles were manipulated 2–3 times and held for 30 min. |
| Lubczyńska, 2023 [30], case series | Postoperative scars on the elbow joint (1), abdominal cavity surgeries (3), and C-sections (7). Average age of 5 months (±2.9) | Assess the effectiveness of manual therapy in combination with other methods for treating postoperative scars. | n = 11, manual scar manipulation, massage, mobilization, DN (2 sessions/entire protocol, “dragon wrapping”), taping, 30 min each for 8 weeks, “dragon wrapping”. |
| Name of the Author, Year, Type of Research | Pain Assessment | Itching Assessment | Scar Assessment | |
|---|---|---|---|---|
| Before Treatment | After Treatment | |||
| Bahramian, 2022 [2], case reports | VAS 8/10 before, 3/10 after | Not conducted | MMT: Flexion Rt. (Right): 4/5—Lt. (Left): 4+/5, Extension Rt.: 4/5—Lt.: 4−/5, Abduction Rt.: 4−/5—Lt.: 4/5, Adduction Rt.: 4−/5—Lt.: 4/5, External Rotation Rt.: 4/5—Lt.: 4−/5, Internal Rotation Rt.: 4/5—Lt.: 4−/5. Up and go test time: 7.49 s; 30 s chair stand test: 8 repetitions; SF-36 physical capabilities = 40%; psychological wellness 44%; social functioning 37.5%. | MMT: flexion Rt. (Right): 5−/5—Lt. (Left): 5−/5, extension Rt.: 5/5—Lt.: 5−/5, abduction Rt.: 4+/5—Lt.: 4+/5, adduction Rt.: 5/5—Lt.: 5−/5, external rotation Rt.: 5/5—Lt.: 5/5, internal rotation Rt.: 5/5—Lt.: 5/5. Up and go test time: 5.19 s; 30 s chair stand test: 12 repetitions; SF-36 physical capabilities = 65%; psychological wellness 56%; social functioning 62.5%. |
| Tuckey, 2022 [3], case reports | NRS = 7/10 before, NRS = 4.5/10; seven months after the injury NRS = 6/10 | NRS = 5/10 before, NRS = 4/10 after | POSAS = 57/70 (81%). Summary scores (%): PCS—29, MCS—46. Domain scores (%): PF—15 (74), RP—44 (71), BP—31 (75), GH—45 (81), VT—44 (60), SF—63 (91), RE—38 (88), MH—75 (87). | POSAS = 27/70 (38%). After 7 weeks of treatment, the patient declined to complete treatment. After 7 months postinjury, it was not possible to complete over the phone. |
| Huang, 2020 [25], case reports | Not conducted. | Not conducted | VSS: M1, V0, H2, and P4, resulting in a total score of 7 points. The extent of neck movements in every directions was as outlined below: flexion: 30.67° ± 7.87°; extension: 38.83° ± 7.25°; right lateral flexion: 27.83° ± 3.66°; left lateral flexion: 26.00° ± 2.97°; right rotation: 54.83° ± 9.09°; left rotation: 53.67° ± 10.82°. | VSS was M1, V0, H2, and P2, resulting in a total score of 5 points. The extent of neck movements in all directions was as outlined below: Flexion: 38.83° ± 3.82°; extension: 41.83° ± 7.33°; right lateral flexion: 33.33° ± 2.50°; left lateral flexion: 28.33° ± 1.63°; right rotation: 58.33° ± 9.00°; left rotation: 62.00° ± 6.54°. |
| Bintoro, 2022 [33], case reports | NRS = 8/11 | Not conducted | Transverse dark-brown firm scar at the midlevel between the xiphoid process and the navel, measuring 30 × 0.3 cm, following laparoscopy. | The scar is not described. |
| Fang, 2014 [34], case reports | 7/10 on a Likert scale before, 1–2/10 after | Not conducted | Surgical scar in the upper part of the right thigh along the gallbladder channel, 3 inches in length, 1/4 inch in width, red in color, firm, and hard. | Less red than before the treatment. |
| Khan, 2019 [35], case reports | Not reported | Not reported | Not reported. | 50% pain relief, in the patient’s words. |
| Tuck, 2010 [37], case reports | VAS 3–4/10 before, VAS 3–4/10 after | Not conducted | Not reported. | Not reported. |
| Anderson, 2014 [24], case reports | Not conducted | Not conducted | Cold and numbness in the pinky finger. | The finger became warm to the touch, and the skin color was normalized. |
| Kotani, 2001 [32], RCT | Continuous, sharp scar pain resistant to conventional treatment. After treatment—pain reduction by >70%, VAS = 0 in >40% of the treatment group; sham treatment group—pain reduction < 15%; no change in the control group | Not reported | Not reported. | Not reported. |
| Song, 2011 [36], RCT | Specifically not described | Specifically not described | The therapy assessment included treatment, outcomes, and failures. A 3-point scale was used to assess color, itching, and hardness, with severely scarred areas receiving 9 points (out of 80), moderate indications scoring 6–9 points (23 areas), and mild assessments scoring 1–5 points (15 areas). | Treatment criteria: in the treatment group—cure: n = 31; improvement: n = 15; failure: n = 3; in the control group—cure: n = 23; improvement: n = 12; failure: n = 10. |
| Lubczyńska, 2023 [30], case series | Following the treatment, a noteworthy disparity existed in the POSAS scores. Treatment had a significant positive influence on pain, pigmentation, pliability, pruritus, surface area, and scar stiffness. Improvement in skin parameters (scar elasticity, thickness, regularity, color) was also noticed | A noteworthy disparity existed in thePOSAS after treatment | Discomfort and pain in the scar area, hydration (37.8 ± 7.7), TEWL (g/m2/h) (13 ± 4), elasticity (mm) (0.003 ± 0.0003), and erythema level (352.1 ± 103.1). POSAS. | Hydration (48.6 ± 1.2), TEWL (9.7 ± 2.4), elasticity (0.05 ± 0.01), and erythema level (249.9 ± 89.8). Melanin level unchanged. POSAS shows a statistically significant difference. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Trybulski, R.; Kawczyński, A.; Muracki, J.; Lovecchio, N.; Kużdżał, A. Dry Needling and Acupuncture for Scars—A Systematic Review. J. Clin. Med. 2024, 13, 3994. https://doi.org/10.3390/jcm13143994
Trybulski R, Kawczyński A, Muracki J, Lovecchio N, Kużdżał A. Dry Needling and Acupuncture for Scars—A Systematic Review. Journal of Clinical Medicine. 2024; 13(14):3994. https://doi.org/10.3390/jcm13143994
Chicago/Turabian StyleTrybulski, Robert, Adam Kawczyński, Jarosław Muracki, Nicola Lovecchio, and Adrian Kużdżał. 2024. "Dry Needling and Acupuncture for Scars—A Systematic Review" Journal of Clinical Medicine 13, no. 14: 3994. https://doi.org/10.3390/jcm13143994







