A Review of Myositis-Associated Interstitial Lung Disease
Abstract
1. Introduction
2. Clinical Cases
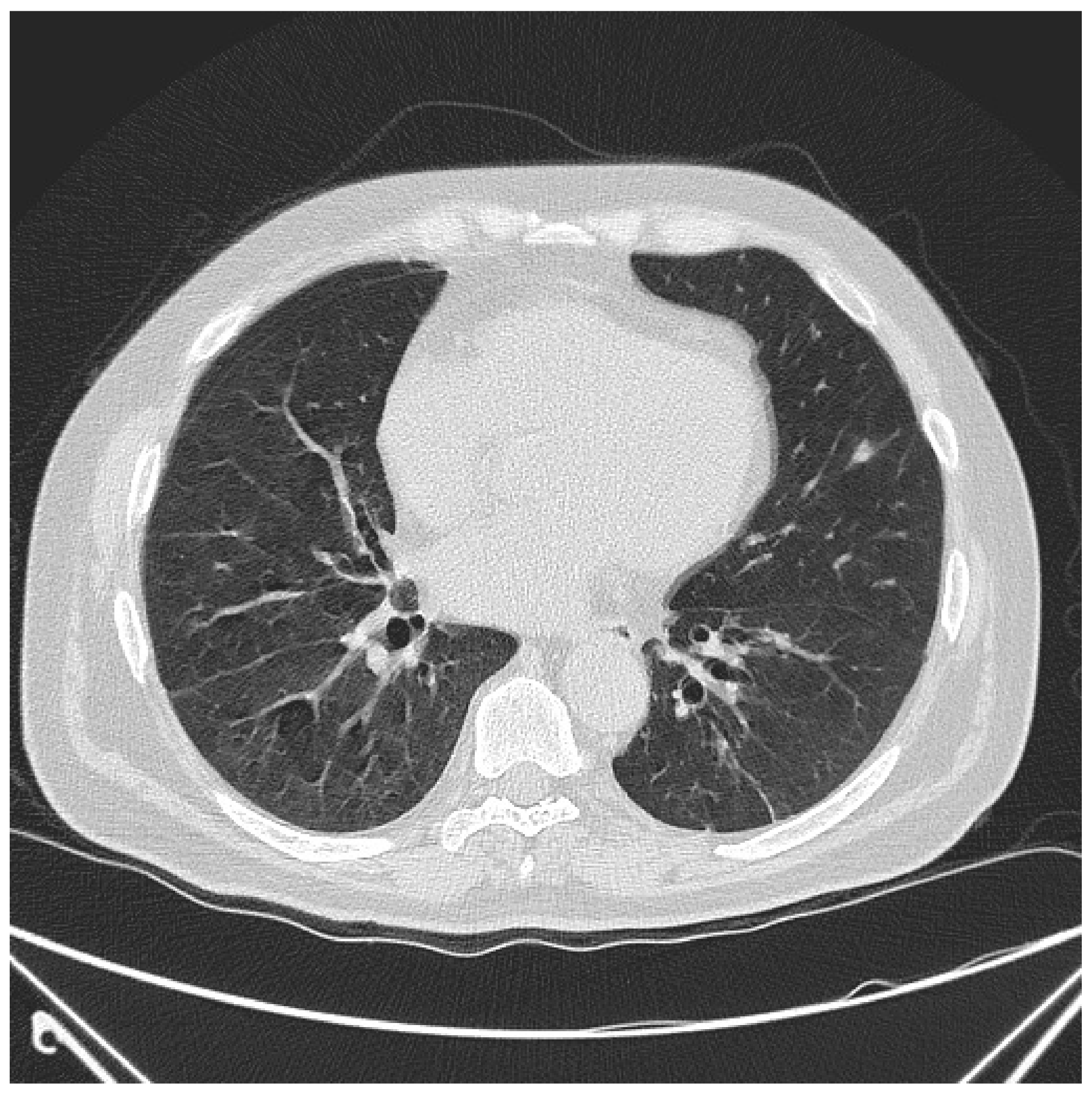
2.1. Case Report 1
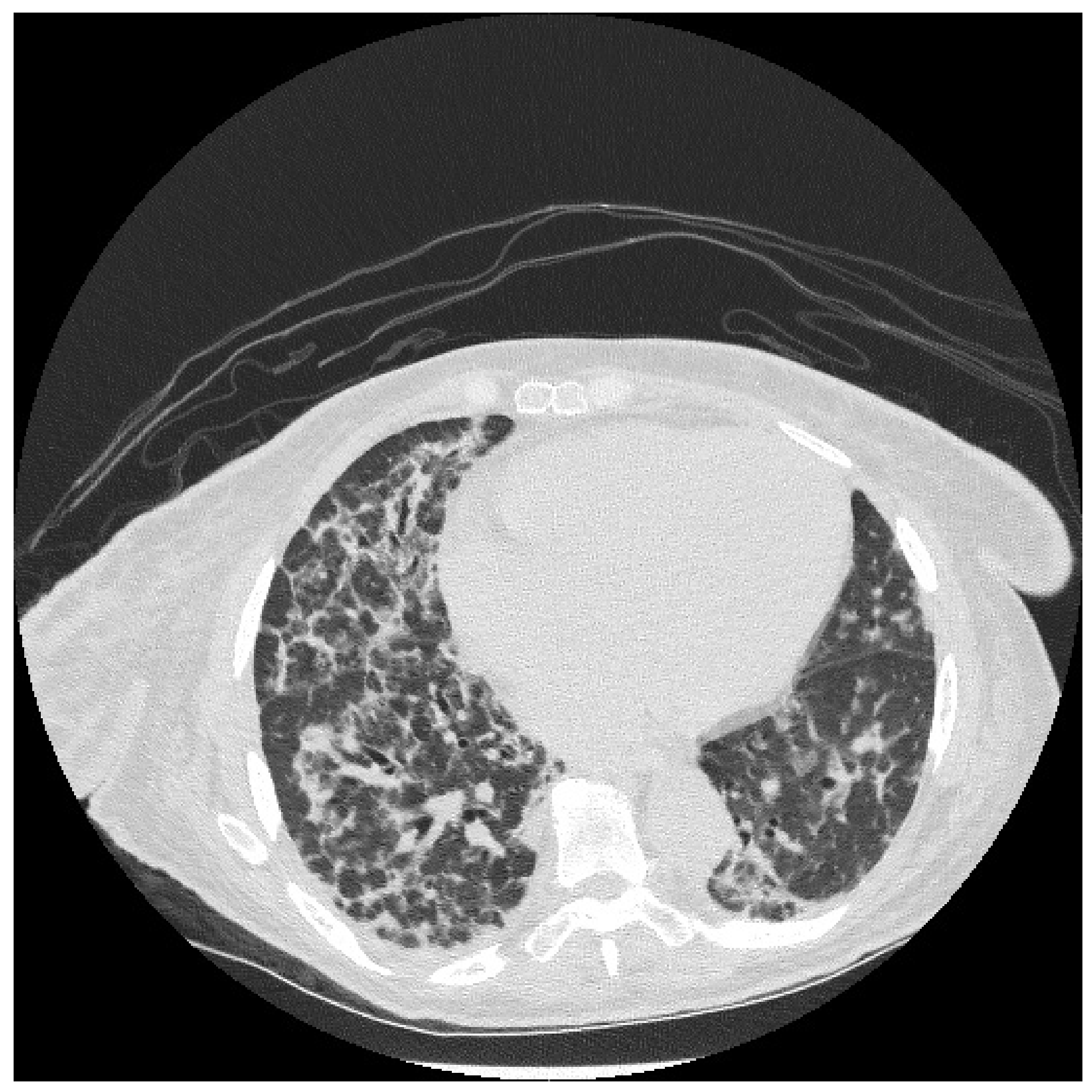
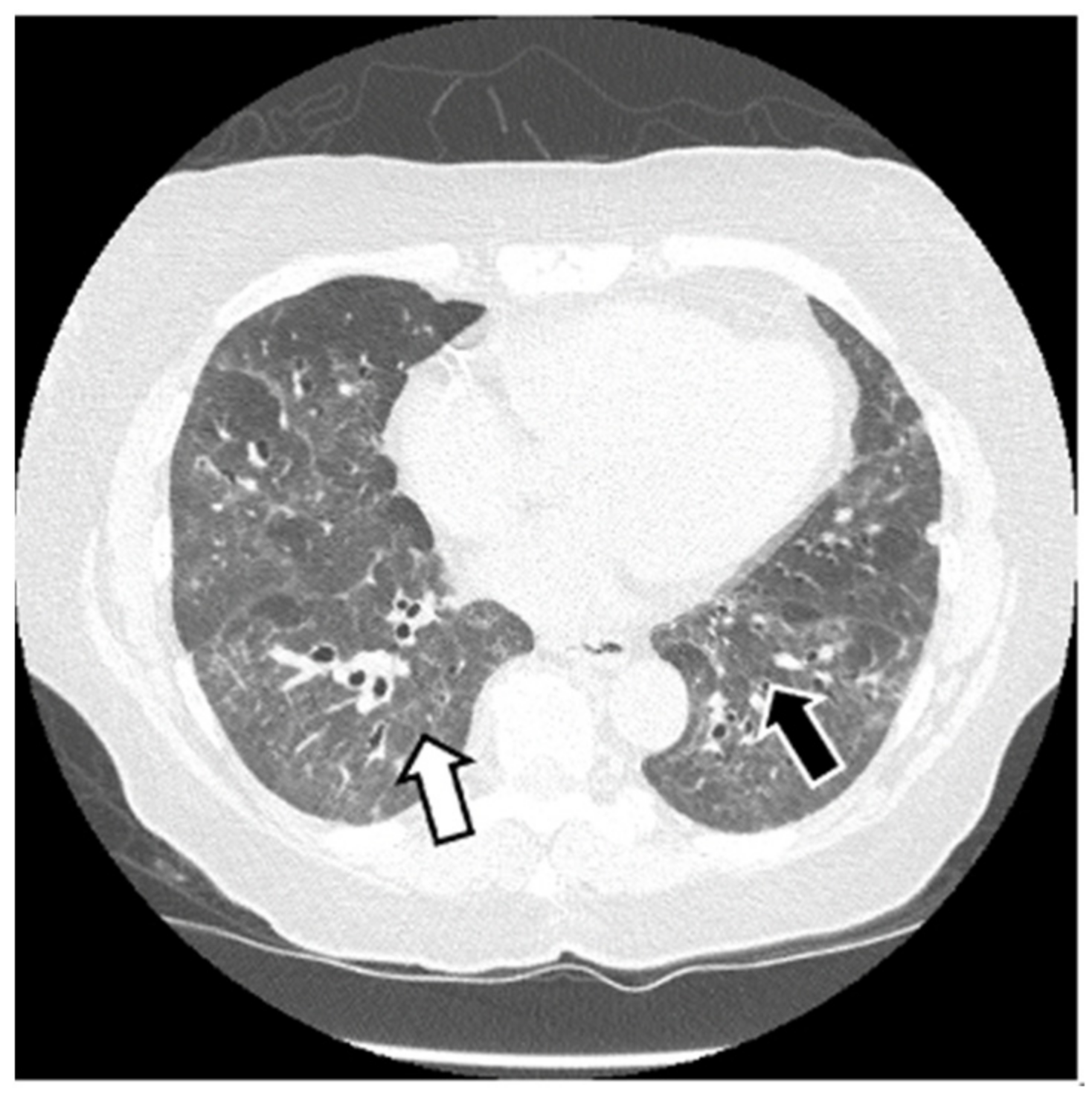
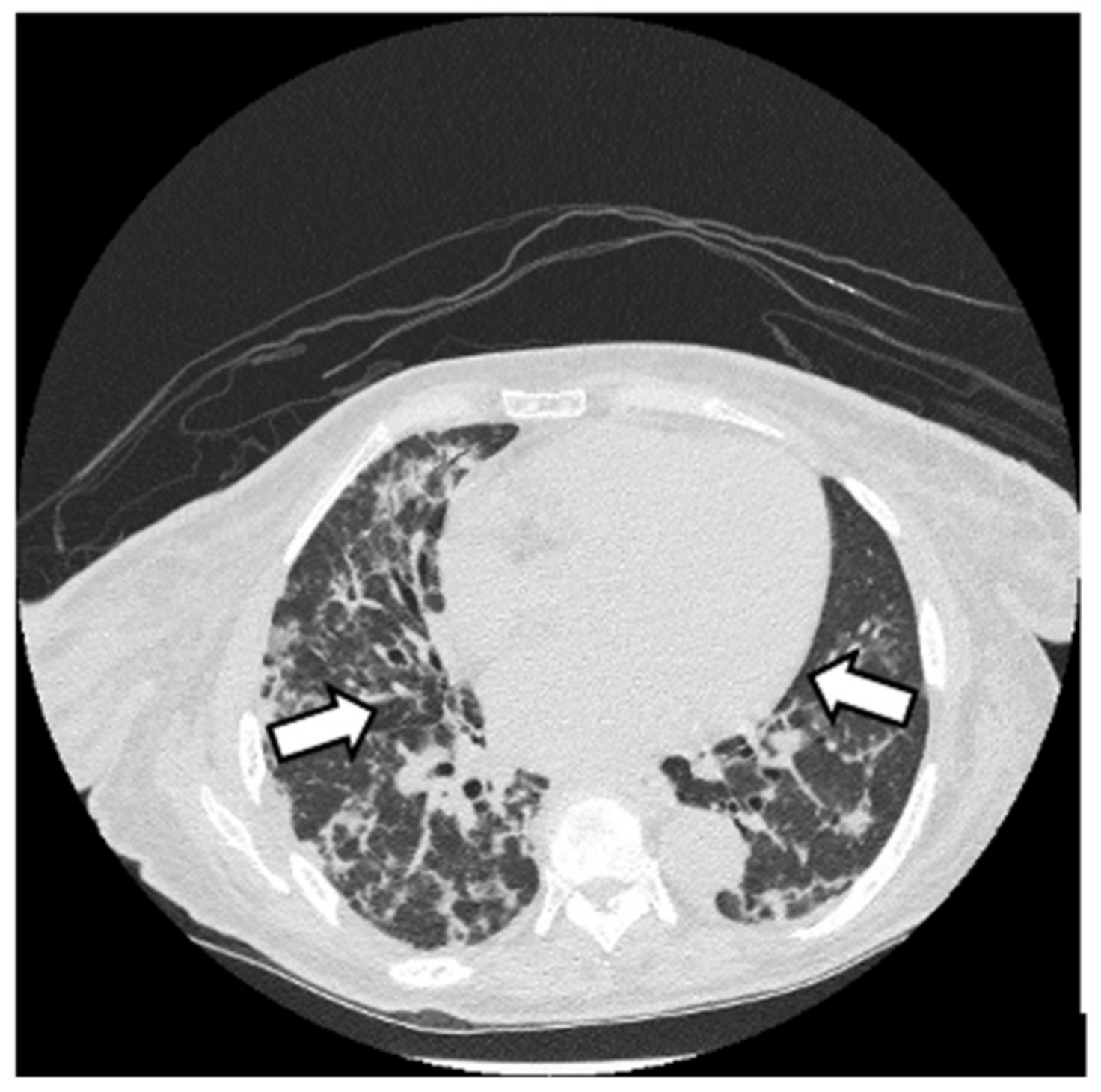
2.2. Case Report 2
2.3. Case Report 3
3. Myositis: Polymyositis and Dermatomyositis
3.1. Classification of Idiopathic Inflammatory Myopathies (Myositis)
3.2. Epidemiology
3.3. Etiology and Pathogenesis
3.4. Diagnostic Criteria
- Symmetric proximal muscle weakness
- Muscle biopsy evidence of necrosis and inflammation
- Elevation of serum skeletal-muscle enzymes
- Electromyographic myopathic changes
- Pathognomonic rashes of DM
3.5. Clinical Features
4. Antisynthetase Syndrome
4.1. Epidemiology
4.2. Etiology and Pathogenesis
4.3. Diagnostic Criteria
4.4. Clinical Features
5. Anti-MDA5 Amyopathic DM
5.1. Epidemiology
5.2. Etiology and Pathogenesis
5.3. Diagnostic Criteria
5.4. Clinical Features
6. Interstitial Lung Disease in Myositis
6.1. Clinical Presentation in Myositis-Associated ILD
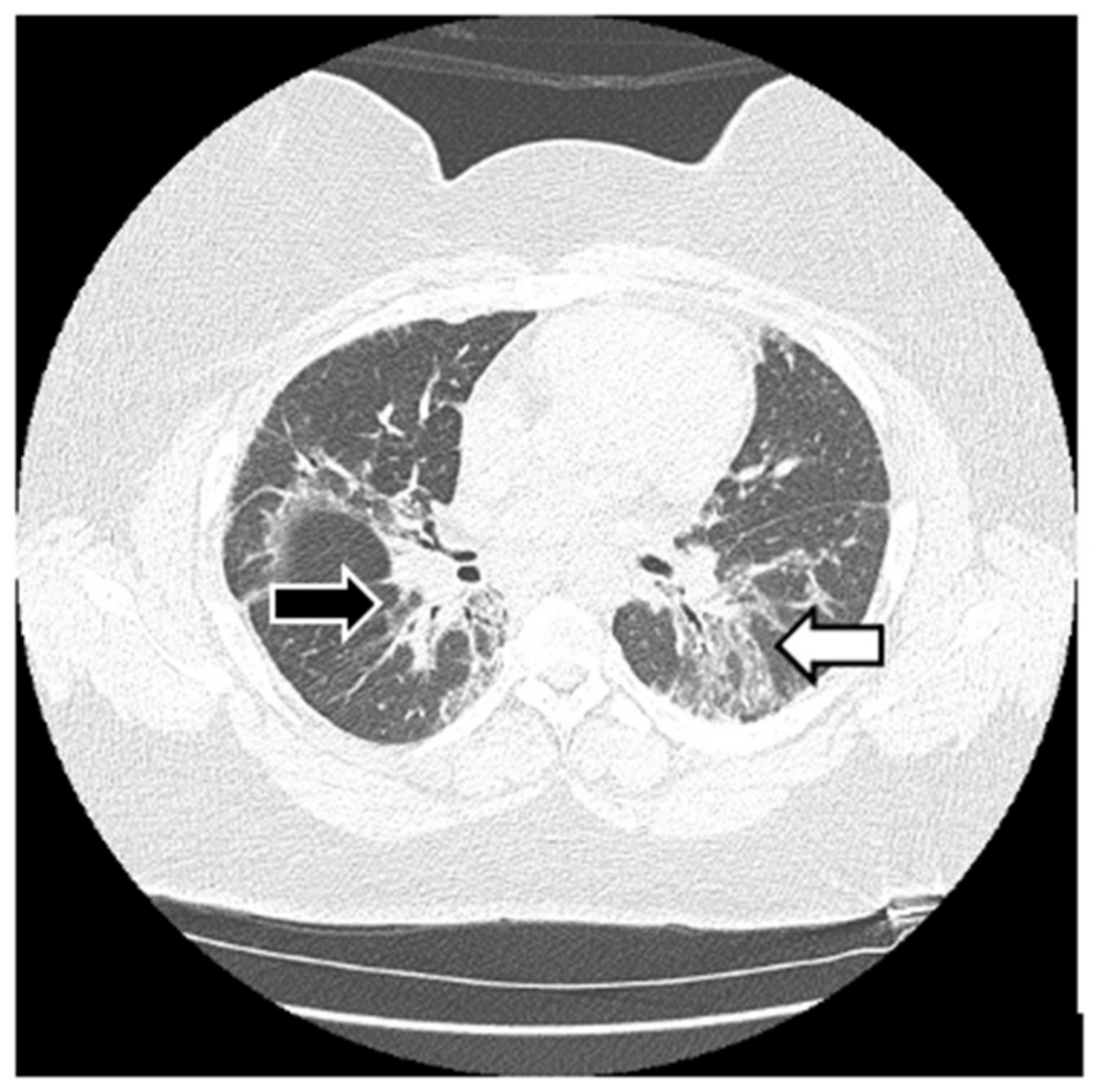
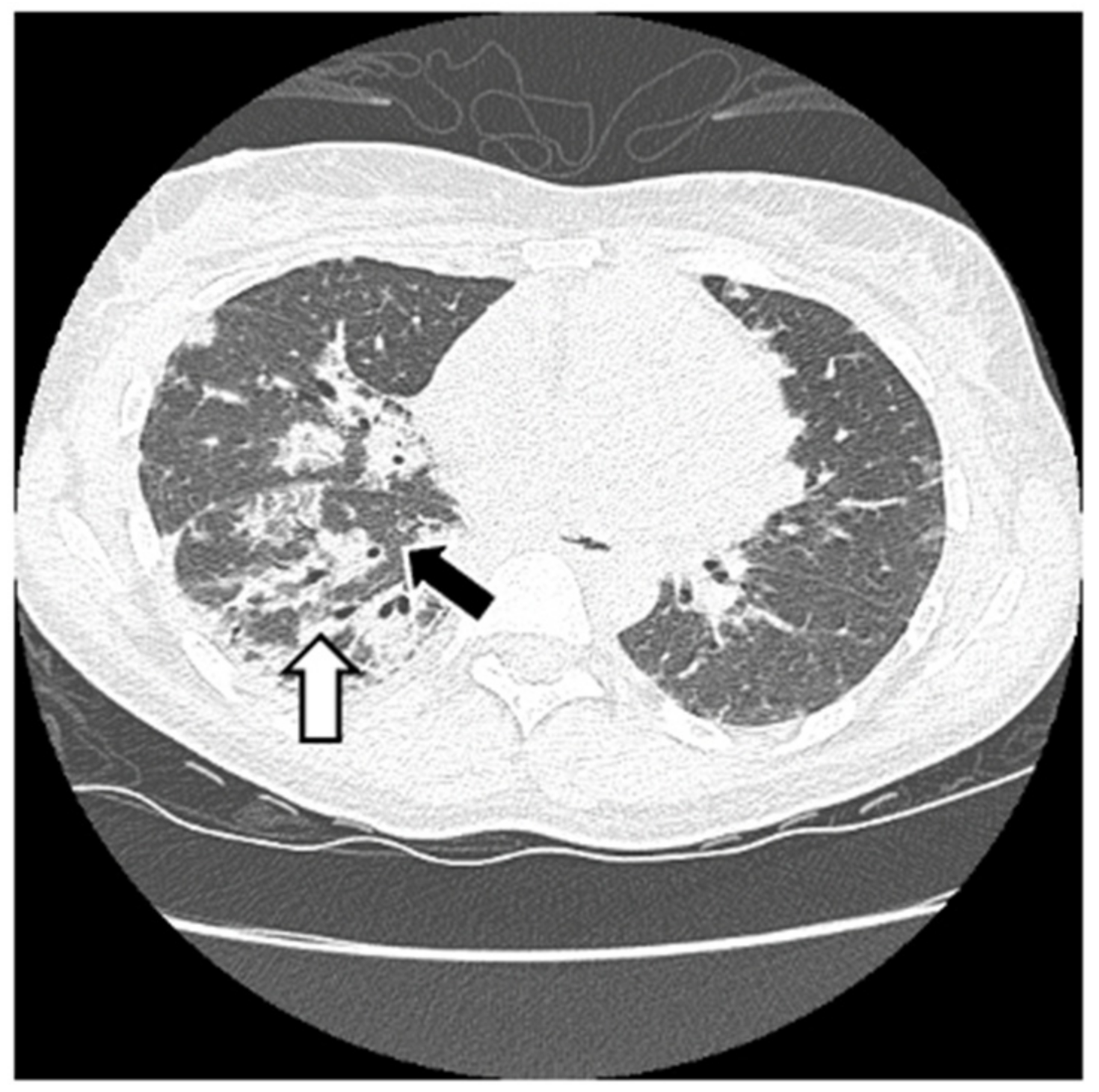
6.2. Histopathologic and Radiographic Findings in Myositis-Associated ILD
6.3. Treatment of Myositis-Associated ILD
6.3.1. Glucocorticoids
6.3.2. Mycophenolate Mofetil
6.3.3. Azathioprine
6.3.4. Calcineurin Inhibitors
6.3.5. Rituximab
6.3.6. Intravenous Immunoglobulin
6.3.7. Cyclophosphamide
6.3.8. Anti-Fibrotic Agents
6.3.9. Janus Kinase Inhibitors
6.3.10. CD-19-Targeted Chimeric Antigen Receptor T cells
6.3.11. Plasmapheresis
7. Conclusions
Author Contributions
Funding
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Long, K.; Danoff, S.K. Interstitial Lung Disease in Polymyositis and Dermatomyositis. Clin. Chest Med. 2019, 40, 561–572. [Google Scholar] [CrossRef] [PubMed]
- Hallowell, R.W.; Danoff, S.K. Diagnosis and Management of Myositis-Associated Lung Disease. Chest 2023, 163, 1476–1491. [Google Scholar] [CrossRef] [PubMed]
- Bohan, A.; Peter, J.B. Polymyositis and Dermatomyositis—(First of Two Parts). N. Engl. J. Med. 1975, 292, 344–347. [Google Scholar] [CrossRef] [PubMed]
- Schnabel, A.; Hellmich, B.; Gross, W.G.L. Interstitial lung disease in polymyositis and dermatomyositis. Curr. Rheumatol. Rep. 2005, 7, 99–105. [Google Scholar] [CrossRef] [PubMed]
- Lu, X.; Peng, Q.; Wang, G. Anti-MDA5 antibody-positive dermatomyositis: Pathogenesis and clinical progress. Nat. Rev. Rheumatol. 2024, 20, 48–62. [Google Scholar] [CrossRef] [PubMed]
- Huang, K.; Aggarwal, R. Antisynthetase syndrome: A distinct disease spectrum. J. Scleroderma Relat. Disord. 2020, 5, 178–191. [Google Scholar] [CrossRef] [PubMed]
- Lundberg, I.E.; Tjärnlund, A.; Bottai, M.; Werth, V.P.; Pilkington, C.; de Visser, M.; Alfredsson, L.; Amato, A.A.; Barohn, R.J.; Liang, M.H.; et al. 2017 European League against Rheumatism/American College of Rheumatology classification criteria for adult and juvenile idiopathic inflammatory myopathies and their major subgroups. Ann. Rheum. Dis. 2017, 76, 1955–1964. [Google Scholar] [CrossRef] [PubMed]
- Vu, T.T.; Brown, K.K.; Solomon, J.J. Myositis-associated interstitial lung disease. Curr. Opin. Pulm. Med. 2023, 29, 427–435. [Google Scholar] [CrossRef] [PubMed]
- Dalakas, M.C.; Hohlfeld, R. Polymyositis and dermatomyositis. Lancet 2003, 362, 971–982. [Google Scholar] [CrossRef] [PubMed]
- Palmucci, S.; Di Mari, A.; Cancemi, G.; Pennisi, I.; Mauro, L.A.; Sambataro, G.; Sambataro, D.; Galioto, F.; Fazio, G.; Ferlito, A.; et al. Clinical and Radiological Features of Interstitial Lung Diseases Associated with Polymyositis and Dermatomyositis. Medicina 2022, 58, 1757. [Google Scholar] [CrossRef] [PubMed]
- Dalakas, M.C. Inflammatory muscle diseases. N. Engl. J. Med. 2015, 372, 1734–1747. [Google Scholar] [CrossRef]
- Senécal, J.; Raynauld, J.; Troyanov, Y. Editorial: A New Classification of Adult Autoimmune Myositis. Arthritis Rheumatol. 2017, 69, 878–884. [Google Scholar] [CrossRef]
- Findlay, A.R.; Goyal, N.A.; Mozaffar, T. An overview of polymyositis and dermatomyositis. Muscle Nerve 2015, 51, 638–656. [Google Scholar] [CrossRef] [PubMed]
- van der Meulen, M.F.; Bronner, I.M.; Hoogendijk, J.E.; Burger, H.; van Venrooij, W.J.; Voskuyl, A.E.; Dinant, H.J.; Linssen, W.H.; Wokke, J.H.; de Visser, M. Polymyositis: An overdiagnosed entity. Neurology 2003, 61, 316–321. [Google Scholar] [CrossRef] [PubMed]
- Arshanapalli, A.; Shah, M.; Veerula, V.; Somani, A.-K. The role of type I interferons and other cytokines in dermatomyositis. Cytokine 2015, 73, 319–325. [Google Scholar] [CrossRef]
- Bolko, L.; Jiang, W.; Tawara, N.; Landon-Cardinal, O.; Anquetil, C.; Benveniste, O.; Allenbach, Y. The role of interferons type I, II and III in myositis: A review. Brain Pathol. 2021, 31, e12955. [Google Scholar] [CrossRef] [PubMed]
- Grundtman, C.; Lundberg, I.E. Pathogenesis of idiopathic inflammatory myopathies. Curr. Rheumatol. Rep. 2006, 8, 188–195. [Google Scholar] [CrossRef] [PubMed]
- Kim, G.-T.; Cho, M.-L.; Park, Y.-E.; Yoo, W.H.; Kim, J.-H.; Oh, H.-J.; Kim, D.-S.; Baek, S.-H.; Lee, S.-H.; Lee, J.-H.; et al. Expression of TLR2, TLR4, and TLR9 in dermatomyositis and polymyositis. Clin. Rheumatol. 2010, 29, 273–279. [Google Scholar] [CrossRef] [PubMed]
- Mammen, A.L. Dermatomyositis and polymyositis: Clinical presentation, autoantibodies, and pathogenesis. Ann. N. Y. Acad. Sci. 2010, 1184, 134–153. [Google Scholar] [CrossRef] [PubMed]
- Lahouti, A.H.; Christopher-Stine, L. Polymyositis and dermatomyositis: Novel insights into the pathogenesis and potential therapeutic targets. Discov. Med. 2015, 19, 463–470. [Google Scholar] [PubMed]
- Bohan, A.; Peter, J.B. Polymyositis and Dermatomyositis— (Second of Two Parts). N. Engl. J. Med. 1975, 292, 403–407. [Google Scholar] [CrossRef] [PubMed]
- Cheeti, A.; Brent, L.H.; Panginikkod, S. Autoimmune Myopathies; StatPearls Publishing LLC.: Treasure Island, FL, USA, 2024. [Google Scholar]
- Chu, L.L.; Rohekar, G. Dermatomyositis. Can. Med. Assoc. J. 2019, 191, E340. [Google Scholar] [CrossRef] [PubMed]
- Ghirardello, A.; Borella, E.; Beggio, M.; Franceschini, F.; Fredi, M.; Doria, A. Myositis autoantibodies and clinical phenotypes. Autoimmun. Highlights 2014, 5, 69–75. [Google Scholar] [CrossRef] [PubMed]
- Cox, N.H. Dermatomyositis. Disease associations and an evaluation of screening investigations for malignancy. Arch. Dermatol. 1990, 126, 61–65. [Google Scholar] [CrossRef] [PubMed]
- Cojocaru, M.; Cojocaru, I.M.; Chicos, B. New Insights into Antisynthetase Syndrome. Maedica 2016, 11, 130–135. [Google Scholar] [PubMed]
- Chatterjee, S.; Prayson, R.; Farver, C. Antisynthetase syndrome: Not just an inflammatory myopathy. Clevel. Clin. J. Med. 2013, 80, 655–666. [Google Scholar] [CrossRef]
- Cavagna, L.; Nuño, L.; Scirè, C.A.; Govoni, M.; Longo, F.J.L.; Franceschini, F.; Neri, R.; Castañeda, S.; Giraldo, W.A.S.; Caporali, R.; et al. Clinical Spectrum Time Course in Anti Jo-1 Positive Antisynthetase Syndrome: Results from an International Retrospective Multicenter Study. Medicine 2015, 94, e1144. [Google Scholar] [CrossRef] [PubMed]
- Gasparotto, M.; Gatto, M.; Saccon, F.; Ghirardello, A.; Iaccarino, L.; Doria, A. Pulmonary involvement in antisynthetase syndrome. Curr. Opin. Rheumatol. 2019, 31, 603–610. [Google Scholar] [CrossRef] [PubMed]
- Opinc, A.H.; Makowska, J.S. Antisynthetase syndrome–much more than just a myopathy. Semin. Arthritis Rheum. 2020, 51, 72–83. [Google Scholar] [CrossRef] [PubMed]
- Zhao, N.; Jiang, W.; Wu, H.; Wang, P.; Wang, X.; Bai, Y.; Li, Y.; Tang, Y.; Liu, Y. Clinical features, prognostic factors, and survival of patients with antisynthetase syndrome and interstitial lung disease. Front. Immunol. 2022, 13, 872615. [Google Scholar] [CrossRef] [PubMed]
- De Souza, F.; De Araújo, D.; Hoff, L.; Baldi, B.; Faria, M.; Junior, L.D.R.; Da Silva, L.; Pinto, G.B.; Bezerra, M.; Miossi, R.; et al. Diagnosis and treatment of interstitial lung disease related to systemic autoimmune myopathies: A narrative review. Reumatismo 2023, 75, 1–14. [Google Scholar] [CrossRef]
- Katsumata, Y.; Ridgway, W.M.; Oriss, T.; Gu, X.; Chin, D.; Wu, Y.; Fertig, N.; Oury, T.; Vandersteen, D.; Clemens, P.; et al. Species-specific immune responses generated by histidyl-tRNA synthetase immunization are associated with muscle and lung inflammation. J. Autoimmun. 2007, 29, 174–186. [Google Scholar] [CrossRef] [PubMed]
- Soejima, M.; Kang, E.H.; Gu, X.; Katsumata, Y.; Clemens, P.R.; Ascherman, D.P. Role of innate immunity in a murine model of histidyl–transfer RNA synthetase (Jo-1)–mediated myositis. Arthritis Rheum. 2010, 63, 479–487. [Google Scholar] [CrossRef] [PubMed]
- Howard, O.Z.; Dong, H.F.; Yang, D.; Raben, N.; Nagaraju, K.; Rosen, A.; Casciola-Rosen, L.; Härtlein, M.; Kron, M.; Yang, D.; et al. Histidyl-tRNA synthetase and asparaginyl-tRNA synthetase, autoantigens in myositis, activate chemokine receptors on T lymphocytes and immature dendritic cells. J. Exp. Med. 2002, 196, 781–791. [Google Scholar] [CrossRef] [PubMed]
- Gono, T.; Kaneko, H.; Kawaguchi, Y.; Hanaoka, M.; Kataoka, S.; Kuwana, M.; Takagi, K.; Ichida, H.; Katsumata, Y.; Ota, Y.; et al. Cytokine profiles in polymyositis and dermatomyositis complicated by rapidly progressive or chronic interstitial lung disease. Rheumatology 2014, 53, 2196–2203. [Google Scholar] [CrossRef] [PubMed]
- Zhou, J.J.; Wang, F.; Xu, Z.; Lo, W.-S.; Lau, C.-F.; Chiang, K.P.; Nangle, L.A.; Ashlock, M.A.; Mendlein, J.D.; Yang, X.-L.; et al. Secreted histidyl-tRNA synthetase splice variants elaborate major epitopes for autoantibodies in inflammatory myositis. J. Biol. Chem. 2014, 289, 19269–19275. [Google Scholar] [CrossRef] [PubMed]
- Marco, J.L.; Collins, B.F. Clinical manifestations and treatment of antisynthetase syndrome. Best Pract. Res. Clin. Rheumatol. 2020, 34, 101503. [Google Scholar] [CrossRef] [PubMed]
- Connors, G.R.; Christopher-Stine, L.; Oddis, C.V.; Danoff, S.K. Interstitial lung disease associated with the idiopathic inflammatory myopathies: What progress has been made in the past 35 years? Chest 2010, 138, 1464–1474. [Google Scholar] [CrossRef] [PubMed]
- Solomon, J.; Swigris, J.J.; Brown, K.K. Myositis-related interstitial lung disease and antisynthetase syndrome. J. Bras. Pneumol. 2011, 37, 100–109. [Google Scholar] [CrossRef] [PubMed]
- Baccaro, A.; Pinto, G.B.; Carboni, R.; Shinjo, S. The clinical manifestations at the onset of antisynthetase syndrome: A chameleon with multiple faces. Reumatismo 2020, 72, 86–92. [Google Scholar] [CrossRef] [PubMed]
- Nombel, A.; Fabien, N.; Coutant, F. Dermatomyositis with Anti-MDA5 Antibodies: Bioclinical Features, Pathogenesis and Emerging Therapies. Front. Immunol. 2021, 12, 773352. [Google Scholar] [CrossRef] [PubMed]
- Betteridge, Z.; Tansley, S.; Shaddick, G.; Chinoy, H.; Cooper, R.; New, R.; Lilleker, J.; Vencovsky, J.; Chazarain, L.; Danko, K.; et al. Frequency, mutual exclusivity and clinical associations of myositis autoantibodies in a combined European cohort of idiopathic inflammatory myopathy patients. J. Autoimmun. 2019, 101, 48–55. [Google Scholar] [CrossRef] [PubMed]
- Chen, Z.; Hu, W.; Wang, Y.; Guo, Z.; Sun, L.; Kuwana, M. Distinct profiles of myositis-specific autoantibodies in Chinese and Japanese patients with polymyositis/dermatomyositis. Clin. Rheumatol. 2015, 34, 1627–1631. [Google Scholar] [CrossRef]
- Waseda, Y.; Johkoh, T.; Egashira, R.; Sumikawa, H.; Saeki, K.; Watanabe, S.; Matsunuma, R.; Takato, H.; Ichikawa, Y.; Hamaguchi, Y.; et al. Antisynthetase syndrome: Pulmonary computed tomography findings of adult patients with antibodies to aminoacyl-tRNA synthetases. Eur. J. Radiol. 2016, 85, 1421–1426. [Google Scholar] [CrossRef] [PubMed]
- Wu, W.; Guo, L.; Fu, Y.; Wang, K.; Zhang, D.; Xu, W.; Chen, Z.; Ye, S. Interstitial Lung Disease in Anti-MDA5 Positive Dermatomyositis. Clin. Rev. Allergy Immunol. 2021, 60, 293–304. [Google Scholar] [CrossRef] [PubMed]
- Nishina, N.; Sato, S.; Masui, K.; Gono, T.; Kuwana, M. Seasonal and residential clustering at disease onset of anti-MDA5-associated interstitial lung disease. RMD Open 2020, 6, e001202. [Google Scholar] [CrossRef] [PubMed]
- Chen, Z.; Wang, Y.; Kuwana, M.; Xu, X.; Hu, W.; Feng, X.; Wang, H.; Kimura, A.; Sun, L. HLA-DRB1 Alleles as Genetic Risk Factors for the Development of Anti-MDA5 Antibodies in Patients with Dermatomyositis. J. Rheumatol. 2017, 44, 1389–1393. [Google Scholar] [CrossRef] [PubMed]
- Lin, J.; Zhang, Y.; Peng, Q.; Yang, H.; Shi, J.; Gu, M.; Zhao, W.; Wang, G. Genetic association of HLA-DRB1 multiple polymorphisms with dermatomyositis in Chinese population. HLA 2017, 90, 354–359. [Google Scholar] [CrossRef] [PubMed]
- Gono, T.; Kawaguchi, Y.; Kuwana, M.; Sugiura, T.; Furuya, T.; Takagi, K.; Ichida, H.; Katsumata, Y.; Hanaoka, M.; Ota, Y.; et al. Brief Report: Association of HLA–DRB1*0101/*0405 with susceptibility to anti–melanoma differentiation–associated gene 5 antibody–positive dermatomyositis in the Japanese population. Arthritis Rheum. 2012, 64, 3736–3740. [Google Scholar] [CrossRef] [PubMed]
- Gono, T.; Masui, K.; Nishina, N.; Kawaguchi, Y.; Kawakami, A.; Ikeda, K.; Kirino, Y.; Sugiyama, Y.; Tanino, Y.; Nunokawa, T.; et al. Risk Prediction Modeling Based on a Combination of Initial Serum Biomarker Levels in Polymyositis/Dermatomyositis–Associated Interstitial Lung Disease. Arthritis Rheumatol. 2021, 73, 677–686. [Google Scholar] [CrossRef] [PubMed]
- Kurtzman, D.J.; Vleugels, R.A. Anti-melanoma differentiation–associated gene 5 (MDA5) dermatomyositis: A concise review with an emphasis on distinctive clinical features. J. Am. Acad. Dermatol. 2018, 78, 776–785. [Google Scholar] [CrossRef] [PubMed]
- Bobirca, A.; Alexandru, C.; Musetescu, A.E.; Bobirca, F.; Florescu, A.T.; Constantin, M.; Tebeica, T.; Florescu, A.; Isac, S.; Bojinca, M.; et al. Anti-MDA5 Amyopathic Dermatomyositis—A Diagnostic and Therapeutic Challenge. Life 2022, 12, 1108. [Google Scholar] [CrossRef]
- Dobloug, G.C.; Svensson, J.; Lundberg, I.E.; Holmqvist, M. Mortality in idiopathic inflammatory myopathy: Results from a Swedish nationwide population-based cohort study. Ann. Rheum. Dis. 2017, 77, 40–47. [Google Scholar] [CrossRef] [PubMed]
- Marie, I.; Hatron, P.Y.; Dominique, S.; Cherin, P.; Mouthon, L.; Menard, J. Short-term and long-term outcomes of interstitial lung disease in polymyositis and dermatomyositis: A series of 107 patients. Arthritis Rheum. 2011, 63, 3439–3447. [Google Scholar] [CrossRef] [PubMed]
- Nuño-Nuño, L.; Joven, B.E.; Carreira, P.E.; Maldonado-Romero, V.; Larena-Grijalba, C.; Cubas, I.L.; Tomero, E.G.; Barbadillo-Mateos, M.C.; Lefebvre, P.G.D.l.P.; Ruiz-Gutiérrez, L.; et al. Mortality and prognostic factors in idiopathic inflammatory myositis: A retrospective analysis of a large multicenter cohort of Spain. Rheumatol. Int. 2017, 37, 1853–1861. [Google Scholar] [CrossRef] [PubMed]
- Jin, Q.; Fu, L.; Yang, H.; Chen, X.; Lin, S.; Huang, Z.; Gao, B.; Tian, X.; Jiang, W.; Shu, X.; et al. Peripheral lymphocyte count defines the clinical phenotypes and prognosis in patients with anti-MDA5-positive dermatomyositis. J. Intern. Med. 2023, 293, 494–507. [Google Scholar] [CrossRef] [PubMed]
- Pinal-Fernandez, I.; Casal-Dominguez, M.; Huapaya, J.A.; Albayda, J.; Paik, J.J.; Johnson, C.; Silhan, L.; Christopher-Stine, L.; Mammen, A.L.; Danoff, S.K. A longitudinal cohort study of the anti-synthetase syndrome: Increased severity of interstitial lung disease in black patients and patients with anti-PL7 and anti-PL12 autoantibodies. Rheumatology 2017, 56, 999–1007. [Google Scholar] [CrossRef] [PubMed]
- Pepper, E.; Vilar, L.D.; Ward, I.M.M. Clinical Characteristics and Prognostic Value of Ro52/SSA Antibodies in Idiopathic Inflammatory Myopathies. Am. J. Clin. Oncol. 2023, 29, 347–353. [Google Scholar] [CrossRef] [PubMed]
- Bozzalla-Cassione, E.; Zanframundo, G.; Biglia, A.; Bellis, E.; Bozzini, S.; Codullo, V.; Vertui, V.; Alpini, C.; Valentini, A.; Preda, L.; et al. Anti-Ro52 antibodies positivity in antisynthetase syndrome: A single centre cohort study. Clin. Exp. Rheumatol. 2022, 40, 27–31. [Google Scholar] [CrossRef] [PubMed]
- Lv, C.; You, H.; Xu, L.; Wang, L.; Yuan, F.; Li, J.; Wu, M.; Zhou, S.; Da, Z.; Qian, J.; et al. Coexistence of Anti-Ro52 Antibodies in Anti-MDA5 Antibody–Positive Dermatomyositis Is Highly Associated with Rapidly Progressive Interstitial Lung Disease and Mortality Risk. J. Rheumatol. 2022, 50, 219–226. [Google Scholar] [CrossRef]
- Gui, X.; Shenyun, S.; Ding, H.; Wang, R.; Tong, J.; Yu, M.; Zhao, T.; Ma, M.; Ding, J.; Xin, X.; et al. Anti-Ro52 antibodies are associated with the prognosis of adult idiopathic inflammatory myopathy-associated interstitial lung disease. Rheumatology 2022, 61, 4570–4578. [Google Scholar] [CrossRef] [PubMed]
- Wells, M.; Alawi, S.; Thin, K.Y.M.; Gunawardena, H.; Brown, A.R.; Edey, A.; Pauling, J.D.; Barratt, S.L.; Adamali, H.I. A multidisciplinary approach to the diagnosis of antisynthetase syndrome. Front. Med. 2022, 9, 959653. [Google Scholar] [CrossRef] [PubMed]
- Baratella, E.; Marrocchio, C.; Cifaldi, R.; Santagiuliana, M.; Bozzato, A.M.; Crivelli, P.; Ruaro, B.; Salton, F.; Confalonieri, M.; Cova, M.A. Interstitial lung disease in patients with antisynthetase syndrome: A retrospective case series study. Jpn. J. Radiol. 2020, 39, 40–46. [Google Scholar] [CrossRef] [PubMed]
- Jiang, M.; Dong, X.; Zheng, Y. Clinical characteristics of interstitial lung diseases positive to different anti-synthetase antibodies. Medicine 2021, 100, e25816. [Google Scholar] [CrossRef] [PubMed]
- Tanizawa, K.; Handa, T.; Nakashima, R.; Kubo, T.; Hosono, Y.; Aihara, K.; Ikezoe, K.; Watanabe, K.; Taguchi, Y.; Hatta, K.; et al. The prognostic value of HRCT in myositis-associated interstitial lung disease. Respir. Med. 2013, 107, 745–752. [Google Scholar] [CrossRef] [PubMed]
- Bonnefoy, O.; Ferretti, G.; Calaque, O.; Coulomb, M.; Begueret, H.; Beylot-Barry, M.; Laurent, F. Serial chest CT findings in interstitial lung disease associated with polymyositis–dermatomyositis. Eur. J. Radiol. 2004, 49, 235–244. [Google Scholar] [CrossRef] [PubMed]
- Hozumi, H.; Fujisawa, T.; Nakashima, R.; Johkoh, T.; Sumikawa, H.; Murakami, A.; Enomoto, N.; Inui, N.; Nakamura, Y.; Hosono, Y.; et al. Comprehensive assessment of myositis-specific autoantibodies in polymyositis/dermatomyositis-associated interstitial lung disease. Respir. Med. 2016, 121, 91–99. [Google Scholar] [CrossRef] [PubMed]
- Hervier, B.; Uzunhan, Y. Inflammatory Myopathy-Related Interstitial Lung Disease: From Pathophysiology to Treatment. Front. Med. 2019, 6, 326. [Google Scholar] [CrossRef] [PubMed]
- Hallowell, R.W.; Paik, J.J. Myositis-associated interstitial lung disease: A comprehensive approach to diagnosis and management. Clin. Exp. Rheumatol. 2022, 40, 373–383. [Google Scholar] [CrossRef] [PubMed]
- Fujisawa, T. Management of Myositis-Associated Interstitial Lung Disease. Medicina 2021, 57, 347. [Google Scholar] [CrossRef] [PubMed]
- Sharma, N.; Putman, M.S.; Vij, R.; Strek, M.E.; Dua, A. Myositis-associated Interstitial Lung Disease: Predictors of Failure of Conventional Treatment and Response to Tacrolimus in a US Cohort. J. Rheumatol. 2017, 44, 1612–1618. [Google Scholar] [CrossRef] [PubMed]
- Allenbach, Y.; Guiguet, M.; Rigolet, A.; Marie, I.; Hachulla, E.; Drouot, L.; Jouen, F.; Jacquot, S.; Mariampillai, K.; Musset, L.; et al. Efficacy of Rituximab in Refractory Inflammatory Myopathies Associated with Anti-Synthetase Auto-Antibodies: An Open-Label, Phase II Trial. PLoS ONE 2015, 10, e0133702. [Google Scholar] [CrossRef]
- Kurasawa, K.; Arai, S.; Namiki, Y.; Tanaka, A.; Takamura, Y.; Owada, T.; Arima, M.; Maezawa, R. Tofacitinib for refractory interstitial lung diseases in anti-melanoma differentiation-associated 5 gene antibody-positive dermatomyositis. Rheumatology 2018, 57, 2114–2119. [Google Scholar] [CrossRef] [PubMed]
- Moreno-Torres, V.; Martín-Iglesias, D.; Vivero, F.; González-Echavarri, C.; García-Moyano, M.; Enghelmayer, J.I.; Malfante, P.; Gaser, A.; Ruiz-Irastorza, G. Intravenous cyclophosphamide improves functional outcomes in interstitial lung disease related to idiopathic inflammatory myopathies. Semin. Arthritis Rheum. 2023, 59, 152164. [Google Scholar] [CrossRef]
- Fischer, A.; Brown, K.K.; Du Bois, R.M.; Frankel, S.K.; Cosgrove, G.P.; Fernandez-Perez, E.R.; Huie, T.J.; Krishnamoorthy, M.; Meehan, R.T.; Olson, A.L.; et al. Mycophenolate mofetil improves lung function in connective tissue disease-associated interstitial lung disease. J. Rheumatol. 2013, 40, 640–646. [Google Scholar] [CrossRef] [PubMed]
- Marie, I.; Josse, S.; Hatron, P.Y.; Dominique, S.; Hachulla, E.; Janvresse, A.; Cherin, P.; Mouthon, L.; Vittecoq, O.; Menard, J.; et al. Interstitial lung disease in anti-Jo-1 patients with antisynthetase syndrome. Arthritis Care Res. 2013, 65, 800–808. [Google Scholar] [CrossRef] [PubMed]
- Huapaya, J.A.; Silhan, L.; Pinal-Fernandez, I.; Casal-Dominguez, M.; Johnson, C.; Albayda, J.; Paik, J.J.; Sanyal, A.; Mammen, A.L.; Christopher-Stine, L.; et al. Long-Term Treatment with Azathioprine and Mycophenolate Mofetil for Myositis-Related Interstitial Lung Disease. Chest 2019, 156, 896–906. [Google Scholar] [CrossRef] [PubMed]
- Cavagna, L.; Caporali, R.; Abdì-Alì, L.; Dore, R.; Meloni, F.; Montecucco, C. Cyclosporine in anti-Jo1-positive patients with corticosteroid-refractory interstitial lung disease. J. Rheumatol. 2013, 40, 484–492. [Google Scholar] [CrossRef] [PubMed]
- Bauhammer, J.; Blank, N.; Max, R.; Lorenz, H.-M.; Wagner, U.; Krause, D.; Fiehn, C. Rituximab in the Treatment of Jo1 Antibody–associated Antisynthetase Syndrome: Anti-Ro52 Positivity as a Marker for Severity and Treatment Response. J. Rheumatol. 2016, 43, 1566–1574. [Google Scholar] [CrossRef] [PubMed]
- Andersson, H.; Sem, M.; Lund, M.B.; Aaløkken, T.M.; Günther, A.; Walle-Hansen, R.; Garen, T.; Molberg, Ø. Long-term experience with rituximab in anti-synthetase syndrome-related interstitial lung disease. Rheumatology 2015, 54, 1420–1428. [Google Scholar] [CrossRef] [PubMed]
- Aggarwal, R.; Charles-Schoeman, C.; Schessl, J.; Bata-Csörgő, Z.; Dimachkie, M.M.; Griger, Z.; Moiseev, S.; Oddis, C.; Schiopu, E.; Vencovský, J.; et al. Trial of Intravenous Immune Globulin in Dermatomyositis. N. Engl. J. Med. 2022, 387, 1264–1278. [Google Scholar] [CrossRef] [PubMed]
- Huapaya, J.; Hallowell, R.; Silhan, L.; Pinal-Fernandez, I.; Casal-Dominguez, M.; Johnson, C.; Albayda, J.; Paik, J.; Lin, C.; Hussien, A.; et al. Long-term treatment with human immunoglobulin for antisynthetase syndrome-associated interstitial lung disease. Respir. Med. 2019, 154, 6–11. [Google Scholar] [CrossRef] [PubMed]
- Ma, X.; Tang, R.; Luo, M.; Zeng, Z.; Shi, Y.; Tang, B.; Xiao, R. Efficacy of mycophenolate mofetil versus cyclophosphamide in systemic sclerosis-related interstitial lung disease: A systematic review and meta-analysis. Clin. Rheumatol. 2021, 40, 3185–3193. [Google Scholar] [CrossRef] [PubMed]
- Yamasaki, Y.; Yamada, H.; Yamasaki, M.; Ohkubo, M.; Azuma, K.; Matsuoka, S.; Kurihara, Y.; Osada, H.; Satoh, M.; Ozaki, S. Intravenous cyclophosphamide therapy for progressive interstitial pneumonia in patients with polymyositis/dermatomyositis. Rheumatology 2007, 46, 124–130. [Google Scholar] [CrossRef] [PubMed]
- Tsuji, H.; Nakashima, R.; Hosono, Y.; Imura, Y.; Yagita, M.; Yoshifuji, H.; Hirata, S.; Nojima, T.; Sugiyama, E.; Hatta, K.; et al. Multicenter Prospective Study of the Efficacy and Safety of Combined Immunosuppressive Therapy with High-Dose Glucocorticoid, Tacrolimus, and Cyclophosphamide in Interstitial Lung Diseases Accompanied by Anti–Melanoma Differentiation–Associated Gene 5–Positive Dermatomyositis. Arthritis Rheumatol. 2020, 72, 488–498. [Google Scholar] [CrossRef] [PubMed]
- Distler, O.; Highland, K.B.; Gahlemann, M.; Azuma, A.; Fischer, A.; Mayes, M.D.; Raghu, G.; Sauter, W.; Girard, M.; Alves, M.; et al. Nintedanib for Systemic Sclerosis–Associated Interstitial Lung Disease. N. Engl. J. Med. 2019, 380, 2518–2528. [Google Scholar] [CrossRef]
- Maeshima, K.; Yamaoka, K.; Kubo, S.; Nakano, K.; Iwata, S.; Saito, K.; Ohishi, M.; Miyahara, H.; Tanaka, S.; Ishii, K.; et al. The JAK inhibitor tofacitinib regulates synovitis through inhibition of interferon-γ and interleukin-17 production by human CD4+ T cells. Arthritis Rheum. 2012, 64, 1790–1798. [Google Scholar] [CrossRef]
- Tanaka, Y.; Luo, Y.; O’shea, J.J.; Nakayamada, S. Janus kinase-targeting therapies in rheumatology: A mechanisms-based approach. Nat. Rev. Rheumatol. 2022, 18, 133–145. [Google Scholar] [CrossRef]
- Chen, Z.; Wang, X.; Ye, S. Tofacitinib in Amyopathic Dermatomyositis–Associated Interstitial Lung Disease. N. Engl. J. Med. 2019, 381, 291–293. [Google Scholar] [CrossRef]
- Pecher, A.-C.; Hensen, L.; Klein, R.; Schairer, R.; Lutz, K.; Atar, D.; Seitz, C.; Stanger, A.; Schneider, J.; Braun, C.; et al. CD19-Targeting CAR T Cells for Myositis and Interstitial Lung Disease Associated with Antisynthetase Syndrome. JAMA 2023, 329, 2154–2162. [Google Scholar] [CrossRef]
- Wang, J.; Alkrekshi, A.; Dasari, S.; Lin, H.-T.C.; Elantably, D.; Al Armashi, A.R. CD19-targeted chimeric antigen receptor T-cell therapy in patients with concurrent B-cell Non-Hodgkin lymphoma and rheumatic autoimmune diseases: A propensity score matching study. Bone Marrow Transplant. 2023, 58, 1223–1228. [Google Scholar] [CrossRef] [PubMed]
- Bay, P.; de Chambrun, M.P.; Rothstein, V.; Mahevas, M.; De Prost, N.; Roux, A.; Zuber, B.; Biet, D.I.; Hervier, B.; Tazi, A.; et al. Efficacy of plasma exchange in patients with anti-MDA5 rapidly progressive interstitial lung disease. J. Autoimmun. 2022, 133, 102941. [Google Scholar] [CrossRef] [PubMed]




| Classification of Myositis, 1975 |
|---|
| Primary idiopathic polymyositis (PM) |
| Primary idiopathic dermatomyositis (DM) |
| PM/DM associated with malignancy |
| Childhood myositis: DM in >90%, vasculitis is common |
| PM/DM associated with an underlying connective tissue disease (overlap myositis) |
| Classification of Myositis, 2017 | |
|---|---|
| Pure classic dermatomyositis | 30–35% |
Polymyositis phenotype
| 15–20% ≤5% 10–15% |
| Sporadic inclusion body myositis | ≤5% |
| Overlap myositis | 50% |
| Classification of Myositis Including Myositis-Specific Antibodies |
|---|
| Adult polymyositis (PM) |
Immune-mediated necrotizing myopathy (IMNM)
|
Adult dermatomyositis
|
| Antisynthetase syndrome (ASyS): can occur with PM or DM or in patients without myositis |
| Myositis associated with malignancy (DM more common than PM) |
| Myositis in overlap with other autoimmune diseases |
| Inclusion body myositis (IBM): may occur in overlap with Sjögren’s syndrome |
| Antibody | Antigen | Prevalence in Myositis (%) | Common Manifestations |
|---|---|---|---|
| Myositis-specific antibodies (MSAs) | |||
| Anti-aminoacyl tRNA synthetase antibodies (Jo1, PL-7, PL-12, EJ, OJ, Zo, YRS) | Cytoplasmic aminoacyl tRNA synthetase enzymes | Anti-Jo-1: 9–24 Other ASAb < 5 | Myositis, arthritis, Raynaud’s phenomenon, mechanic’s hands, ILD |
| Anti-MDA5 | Melanoma differentiation-associated gene 5 | 10–48 (East Asia), 0–13 (USA and Europe) | CADM, skin ulcerations, RP-ILD |
| Anti-Mi2 | Nucleosome-remodeling deacetylase complex | 11–59 | Classic DM skin findings (heliotrope rash, Gottron’s sign, shawl sign), ILD |
| Anti-SRP | Cytoplasmic signal recognition particle | 5–13 | Decreased cutaneous involvement, severe necrotizing myopathy, no increased risk of ILD |
| Anti-T1F1-γ | Transcriptional intermediary factor 1-gamma | 13–31 | Malignancy |
| Anti-NXP2 | Nuclear matrix protein 2 | 1–17 | Malignancy Calcinosis in JDM |
| Myositis-associated antibodies (MAAs) | |||
| Anti-Ro-52 | 52 kDa ribonuclear protein complex | 9–46 | ILD, arthritis, mechanic hands, overlaps with pSS, SLE, SSc |
| Anti-PM/Scl-75/100 | Nuclear exome complex (70 kDa, 100 kDa subunits) | 4–11 | PM-SSc overlap: inflammatory joint disease, Raynaud’s, mechanic hands, ILD |
| Anti-Ku | 70 kDa, 80 kDa Ku heterodimers | 1–3 | Arthralgia, Raynaud’s, mechanic hands, ILD; overlaps with SSc, SLE |
| Antibody | Antigen | Prevalence in patients with ASyS (Zhao, 2022) (%) [31] | Myositis (De Souza, 2023) (%) [32] | ILD (De Souza, 2023) (%) [32] | Arthritis (Huang, 2019) (%) [6] | Other Manifestations |
|---|---|---|---|---|---|---|
| Jo-1 | Histidyl-tRNA synthetase | 63 | 15–30 | 70–80 | 74 | Arthritis, Raynaud’s, mechanic hands |
| PL-7 | Threonyl-tRNA synthetase | 15 | 5–10 | 84 | 50 | Infrequent muscle involvement, severe arthritis |
| PL-12 | Alanyl-tRNA synthetase | 8 | <5 | 90 | 42 | Pulmonary hypertension, esophageal involvement |
| OJ | Isoleucyl-tRNA synthetase | - | 1 | 8 | 44 | ILD |
| EJ | Glycyl-tRNA synthetase | 14 | 1 | >90 | 53 | DM |
| KS | Asparaginyl-tRNA synthetase | - | 1 | 90 | - | Fever, usual interstitial pneumonia |
| Zo | Phenylalanine0tRNA synthetase | - | <1 | 4–38 | - | Rash, arthritis |
| YRS | Tyrosyl-tRNA synthetase | - | <1 | 60–100 | - | NSIP, Raynaud’s, arthralgia |
| Connors et al., 2010 [39] | Solomon et al., 2011 [40] |
|---|---|
| Antisynthetase antibody plus one or more of the following:
| Antisynthetase antibody plus two major criteria or one major and two minor criteria.
|
| Autoantibodies | Frequency in IIMs (%) | Frequency of ILD (%) |
|---|---|---|
| MSAs | ||
| Anti-Jo-1 | 15–30 | 70–80 |
| Anti-PL-7 | 5–10 | 84 |
| Anti-PL-12 | <5 | 90 |
| Anti-Mi-2 | 4–10 | 4–38 |
| Anti-NXP-2 | 2–30 | 3 |
| Anti-MDA5 | 7–14 | 60 (European) 90 (Asian) |
| Anti-TIF1-γ | 20–30 | <10 |
| Anti-SRP | 3–13 | 10–20 |
| Anti-SAE | <10 | <10 |
| MAAs | ||
| Anti-Ro52 | 10–40 | 7–50 |
| Anti-U1RNP | 6–10 | 7–50 |
| Anti-PM-Scl | 3–10 | 25–80 |
| Anti-Ku | <2 | 27–80 |
| Medication | Outcomes | References |
|---|---|---|
| Glucocorticoids | Response rate: 37.5% to 52% | Fujisawa et al., 2023 [71] |
| MMF | Response rate: 54.5% | Sharma et al., 2017 [72] |
| AZA | Response rate: 54% | Sharma et al., 2017 [72] |
| CNI | Response rate in patient who failed AZA, methotrexate and MMF: 94% | Sharma et al., 2017 [72] |
| Rituximab | 10% improvement in FVC in 50% of patients studied, no significant improvement in FVC in remaining patients | Allenbach et al., 2015 [73] |
| JAKi | Response rate: 60% | Kuraswa et al., 2018 [74] |
| CYC | Response rate: 64% | Moreno-Torres et al., 2023 [75] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kannappan, R.; Kumar, R.; Cichelli, K.; Brent, L.H. A Review of Myositis-Associated Interstitial Lung Disease. J. Clin. Med. 2024, 13, 4055. https://doi.org/10.3390/jcm13144055
Kannappan R, Kumar R, Cichelli K, Brent LH. A Review of Myositis-Associated Interstitial Lung Disease. Journal of Clinical Medicine. 2024; 13(14):4055. https://doi.org/10.3390/jcm13144055
Chicago/Turabian StyleKannappan, Renuka, Raagni Kumar, Kimberly Cichelli, and Lawrence H. Brent. 2024. "A Review of Myositis-Associated Interstitial Lung Disease" Journal of Clinical Medicine 13, no. 14: 4055. https://doi.org/10.3390/jcm13144055
APA StyleKannappan, R., Kumar, R., Cichelli, K., & Brent, L. H. (2024). A Review of Myositis-Associated Interstitial Lung Disease. Journal of Clinical Medicine, 13(14), 4055. https://doi.org/10.3390/jcm13144055





