Compassion Fatigue in a Cohort of South Italian Nurses and Hospital-Based Clinical Social Workers Following COVID-19: A Cross-Sectional Survey
Abstract
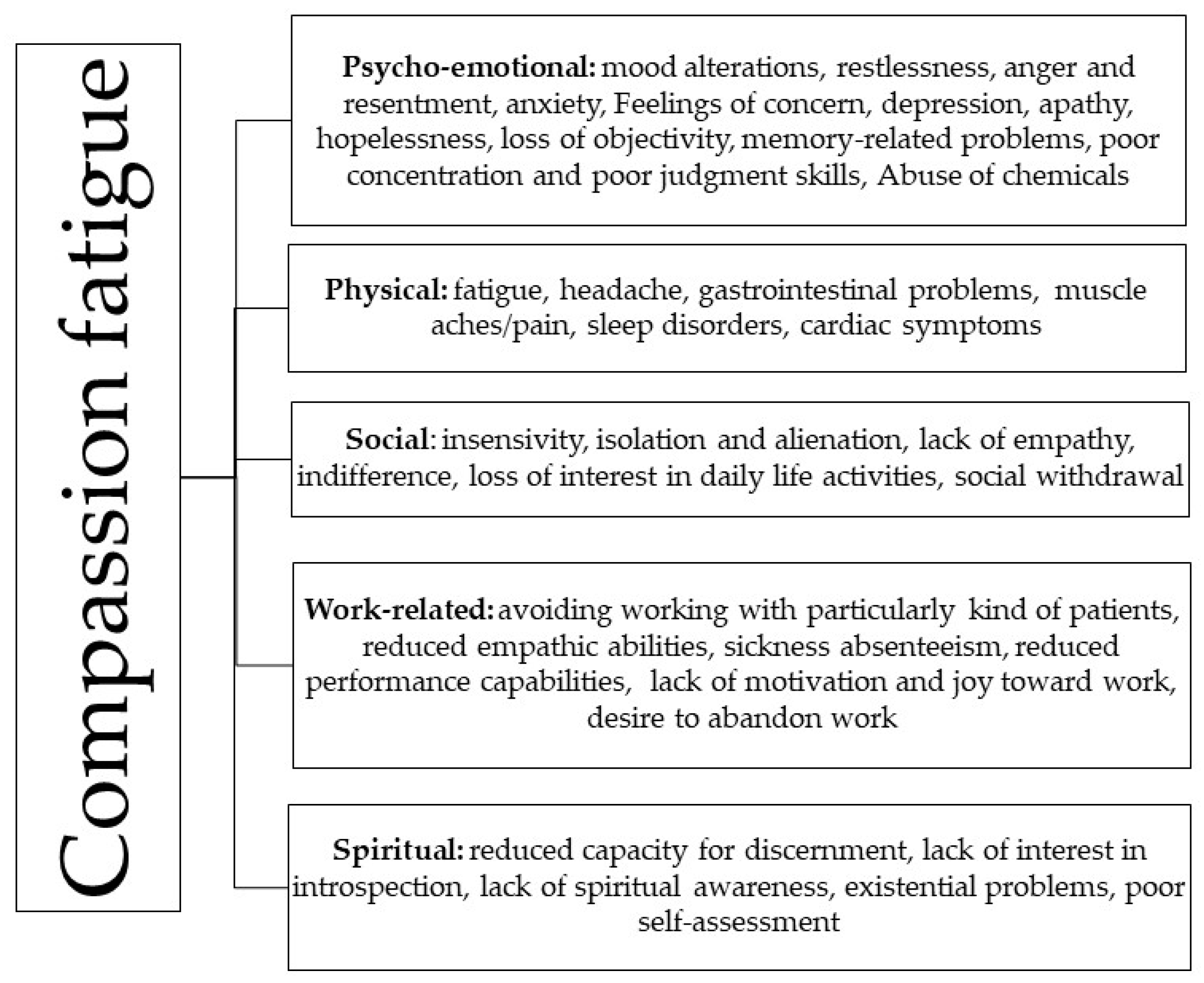
:1. Introduction
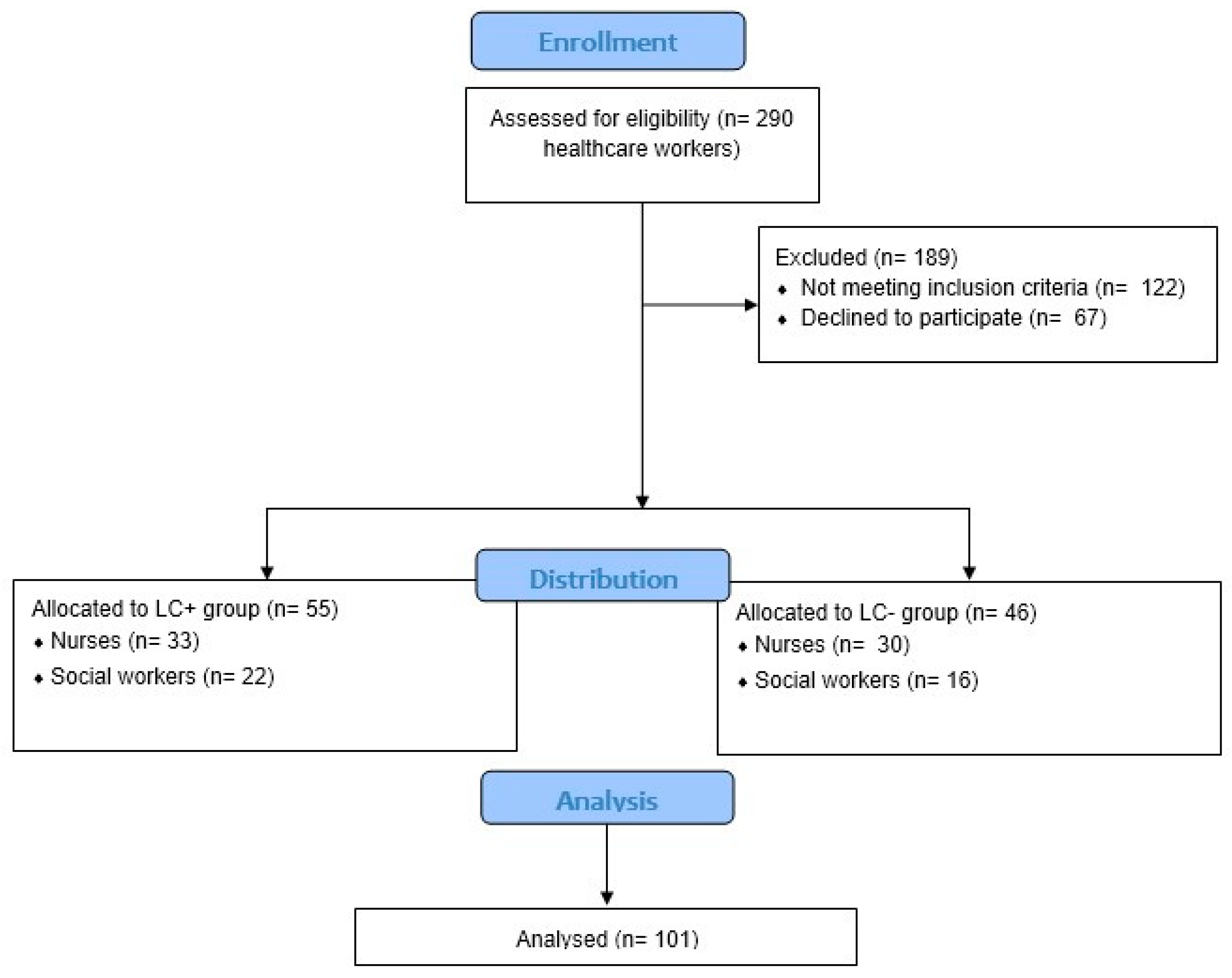
2. Materials and Methods
2.1. Study Design and Data Collection
2.2. Procedures
2.3. Ethical Considerations
2.4. Data Analysis
3. Results
3.1. Primary Aim
3.2. Secondary Aim
4. Discussion
5. Clinical Implications
6. Limitation and Future Research
7. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Joinson, C. Coping with compassion fatigue. Nursing 1992, 116, 118–119, 120. [Google Scholar] [PubMed]
- Figley, C.R. Compassion fatigue: Psychotherapists’ chronic lack of self-care. Clin. Psychol. 2002, 58, 1433–1441. [Google Scholar] [CrossRef]
- Stoewen, D.L. Moving from compassion fatigue to compassion resilience Part 2: Understanding compassion fatigue. Can. Vet. J. 2019, 60, 1004–1006. [Google Scholar] [PubMed]
- Cocker, F.; Joss, N. Compassion Fatigue among Healthcare, Emergency and Community Service Workers: A Systematic Review. Int. J. Environ. Res. Public Health 2016, 13, 618. [Google Scholar] [CrossRef]
- Peters, E. Compassion fatigue in nursing: A concept analysis. Nurs. Forum 2018, 53, 466–480. [Google Scholar] [CrossRef]
- Hinderer, K.A.; VonRueden, K.T.; Friedmann, E.; McQuillan, K.A.; Gilmore, R.; Kramer, B.; Murray, M. Burnout, compassion fatigue, compassion satisfaction, and secondary traumatic stress in trauma nurses. J. Trauma Nurs. 2014, 21, 160–169. [Google Scholar] [CrossRef] [PubMed]
- Mottaghi, S.; Poursheikhal, I.H.; Shameli, L. Empathy, compassion fatigue, guilt and secondary traumatic stress in nurses. Nurs. Ethics 2020, 27, 494–504. [Google Scholar] [CrossRef] [PubMed]
- Marshman, C.; Hansen, A.; Munro, I. Compassion fatigue in mental health nurses: A systematic review. J. Psychiatr. Ment. Health Nurs. 2022, 29, 529–543. [Google Scholar] [CrossRef]
- Ondrejková, N.; Halamová, J. Qualitative analysis of compassion fatigue and coping strategies among nurses. Int. J. Nurs. Sci. 2022, 9, 467–480. [Google Scholar] [CrossRef]
- Todaro-Franceschi, V. Critical care nurses’ perceptions of preparedness and ability to care for the dying and their professional quality of life. Dimens. Crit. Care Nurs. 2013, 32, 184–190. [Google Scholar] [CrossRef]
- Wentzel, D.L.; Brysiewicz, P. A survey of compassion satisfaction, burnout and compassion fatigue in nurses practicing in three oncology departments in Durban, South Africa. Int. J. Afr. Nurs. Sci. 2018, 8, 82–86. [Google Scholar] [CrossRef]
- Alyahya, M.S.; Hijazi, H.H.; Alolayyan, M.N.; Ajayneh, F.J.; Khader, Y.S.; Al-Sheyab, N.A. The Association between Cognitive Medical Errors and Their Contributing Organizational and Individual Factors. Risk Manag. Healthc. Policy 2021, 14, 415–430. [Google Scholar] [CrossRef] [PubMed]
- Kieny, M.P.; Bekedam, H.; Dovlo, D.; Fitzgerald, J.; Habicht, J.; Harrison, G.; Kluge, H.; Lin, V.; Menabde, N.; Mirza, Z.; et al. Strengthening health systems for universal health coverage and sustainable development. Bull. World Health Organ. 2017, 95, 537–539. [Google Scholar] [CrossRef] [PubMed]
- Ezenwaji, I.O.; Eseadi, C.; Okide, C.C.; Nwosu, N.C.; Ugwoke, S.C.; Ololo, K.O.; Oforka, T.; Oboegbulem, A. Work-related stress, burnout, and related sociodemographic factors among nurses: Implications for administrators, research, and policy. Medicine 2019, 98, e13889. [Google Scholar] [CrossRef] [PubMed]
- O’Higgins, M.; Rojas, L.A.; Echeverria, I.; Roselló-Jiménez, L.; Benito, A.; Haro, G. Burnout, psychopathology and purpose in life in healthcare workers during COVID-19 pandemic. Front. Public Health 2022, 10, 926328. [Google Scholar] [CrossRef] [PubMed]
- COVID-19 Rapid Guideline: Managing the Long-Term Effects of COVID-19; National Institute for Health and Care Excellence (NICE): London, UK, 2020.
- Haefner, J. Self-Care for Health Professionals during Coronavirus Disease 2019 Crisis. J. Nurse Pract. 2021, 17, 279–282. [Google Scholar] [CrossRef] [PubMed]
- Nayani, S.; Castanares-Zapatero, D.; De Pauw, R.; Van Cauteren, D.; Demarest, S.; Drieskens, S.; Cornelissen, L.; Devleesschauwer, B.; De Ridder, K.; Charafeddine, R. Classification of post COVID-19 condition symptoms: A longitudinal study in the Belgian population. BMJ Open 2023, 13, e072726. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Al-Oraibi, A.; Naidu, J.S.; Chaka, A.; Woolf, K.B.; Nellums, L.; Tarrant, C.; Pan, D.; Sze, S.; Martin, C.; Gogoi, M.; et al. Prevalence of long COVID-19 among healthcare workers: A systematic review and meta-analysis protocol. BMJ Open 2022, 12, e065234. [Google Scholar] [CrossRef]
- De Luca, R.; Bonanno, M.; Calabrò, R.S. Psychological and Cognitive Effects of Long COVID: A Narrative Review Focusing on the Assessment and Rehabilitative Approach. J. Clin. Med. 2022, 11, 6554. [Google Scholar] [CrossRef]
- Lombardo, B.; Eyre, C. Compassion fatigue: A nurse’s primer. Online J. Issues Nurs. 2011, 16, 3. [Google Scholar] [CrossRef] [PubMed]
- Hyassat, D.; El-Khateeb, M.; Dahbour, A.; Shunnaq, S.; Naji, D.; Bani Ata, E.; Abujbara, M.; Khawaja, N.; Batieha, A.; Ajlouni, K. post-COVID-19 syndrome among healthcare workers in Jordan. East. Mediterr. Health J. 2023, 29, 247–253. [Google Scholar] [CrossRef] [PubMed]
- Coetzee, S.K.; Klopper, H.C. Compassion fatigue within nursing practice: A concept analysis. Nurs. Health Sci. 2010, 12, 235–243. [Google Scholar] [CrossRef] [PubMed]
- Sarker, A.; Ge, Y. Mining long-COVID symptoms from Reddit: Characterizing post-COVID syndrome from patient reports. JAMIA Open 2021, 4, ooab075. [Google Scholar] [CrossRef] [PubMed]
- Klok, F.A.; Boon, G.J.A.M.; Barco, S.; Endres, M.; Geelhoed, J.J.M.; Knauss, S.; Rezek, S.A.; Spruit, M.A.; Vehreschild, J.; Siegerink, B. The Post-COVID-19 Functional Status scale: A tool to measure functional status over time after COVID-19. Eur. Respir. J. 2020, 56, 2001494. [Google Scholar] [CrossRef] [PubMed]
- Raciti, L.; De Luca, R.; Raciti, G.; Arcadi, F.A.; Calabrò, R.S. The Use of Palmitoylethanolamide in the Treatment of Long COVID: A Real-Life Retrospective Cohort Study. Med. Sci. 2022, 10, 37. [Google Scholar] [CrossRef] [PubMed]
- Andrés, A.M.; Mato, A.S. Optimal correction for continuity and conditions for validity in the unconditional chi-squared test. Comput. Stat. Data Anal. 1996, 21, 609–626. [Google Scholar] [CrossRef]
- R Core Team. R: A Language and Environment for Statistical Computing. R Foundation for Statistical Computing: Vienna, Austria, 2022; Available online: https://www.R-project.org/ (accessed on 4 June 2023).
- Stoewen, D.L. Moving from compassion fatigue to compassion resilience Part 4: Signs and consequences of compassion fatigue. Can. Vet. J. 2020, 61, 1207–1209. [Google Scholar] [PubMed] [PubMed Central]
- Labrague, L.J.; de Los Santos, J.A.A. Resilience as a mediator between compassion fatigue, nurses’ work outcomes, and quality of care during the COVID-19 pandemic. Appl. Nurs. Res. 2021, 61, 151476. [Google Scholar] [CrossRef] [PubMed]
- Braquehais, M.D.; Vargas-Caceres, S.; Gomez-Duran, E.; Nieva, G.; Valero, S.; Casas, M.; Bruguera, E. The impact of the COVID-19 pandemic on the mental health of healthcare professionals. QJM Int. J. Med. 2020, 113, 613–617. [Google Scholar] [CrossRef]
- Waters, A. Long covid: Nearly half of doctors affected can no longer work full time, finds survey. BMJ 2023, 382, 1529. [Google Scholar] [CrossRef]
- Moreno-Jiménez, J.E.; Blanco-Donoso, L.M.; Demerouti, E.; Belda Hofheinz, S.; Chico-Fernández, M.; Moreno-Jiménez, B.; Garrosa, E. The Role of Healthcare Professionals’ Passion in Predicting Secondary Traumatic Stress and Posttraumatic Growth in the Face of COVID-19: A Longitudinal Approach. Int. J. Environ. Res. Public Health 2021, 18, 4453. [Google Scholar] [CrossRef] [PubMed]
- Tomaszewska, K.; Majchrowicz, B.; Snarska, K.; Telega, D. Stress and Occupational Burnout of Nurses Working with COVID-19 Patients. Int. J. Environ. Res. Public Health 2022, 19, 12688. [Google Scholar] [CrossRef] [PubMed]
- Fernandez, R.; Sikhosana, N.; Green, H.; Halcomb, E.J.; Middleton, R.; Alananzeh, I.; Trakis, S.; Moxham, L. Anxiety and depression among healthcare workers during the COVID-19 pandemic: A systematic umbrella review of the global evidence. BMJ Open 2021, 11, e054528. [Google Scholar] [CrossRef] [PubMed]
- Cañadas, G.R.; Membrive-Jiménez, M.J.; Martos-Cabrera, M.B.; Albendín-García, L.; Velando-Soriano, A.; Cañadas-De la Fuente, G.A.; De la Fuente-Solana, E.I. Burnout and Professional Engagement during the COVID-19 Pandemic among Nursing Students without Clinical Experience: A Cross-Sectional Study. J. Clin. Med. 2023, 12, 5144. [Google Scholar] [CrossRef] [PubMed]
- Hickling, M.T.; Barnett, S.D. Psychological impact of COVID-19 on nursing personnel: A regional online survey. J. Adv. Nurs. 2022, 78, 3025–3033. [Google Scholar] [CrossRef] [PubMed]
- Blanco-Donoso, L.M.; Moreno-Jiménez, J.; Amutio, A.; Gallego-Alberto, L.; Moreno-Jiménez, B.; Garrosa, E. Stressors, Job Resources, Fear of Contagion, and Secondary Traumatic Stress among Nursing Home Workers in Face of the COVID-19: The Case of Spain. J. Appl. Gerontol. 2021, 40, 244–256. [Google Scholar] [CrossRef] [PubMed]
- Franc-Guimond, J.; Hogues, V. Burnout among caregivers in the era of the COVID-19 pandemic: Insights and challenges. Can. Urol. Assoc. J. 2021, 15 (Suppl. S1), S16–S19. [Google Scholar] [CrossRef] [PubMed]
- De Hert, S. Burnout in Healthcare Workers: Prevalence, Impact and Preventative Strategies. Local Reg. Anesth. 2020, 13, 171–183. [Google Scholar] [CrossRef]
- Maslach, C.; Schaufeli, W.B.; Leiter, M.P. Job burnout. Ann. Rev. Psychol. 2001, 52, 397–422. [Google Scholar] [CrossRef]
- Choi, B.C.; Pak, A.W. A catalog of biases in questionnaires. Prev. Chronic Dis. 2005, 2, A13. [Google Scholar] [PubMed] [PubMed Central]
| All Nurses (N = 63) | LC− (N = 30) | LC+ (N = 33) | p-Value * | ||
|---|---|---|---|---|---|
| Nurses | Age | 43.380 ± 10.648 | 41.60 ± 10.45 | 45.69 ± 11.01 | 0.245 |
| Gender | 0.693 | ||||
| Females | 45 (71.4%) | 22 (73.3%) | 23 (69.7%) | ||
| Males | 18 (28.5%) | 8 (26.6%) | 10 (30.3%) | ||
| Educational level | 0.494 | ||||
| Middle school | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | ||
| High school | 9 (14.2%) | 5 (16.6%) | 4 (12.1%) | ||
| University | 39 (61.9%) | 18 (60.0%) | 21 (63.6%) | ||
| Master’s degree | 15 (23.8%) | 7 (23.3%) | 8 (24.2%) | ||
| Instances of SARS-CoV-2 infection | 0.061 | ||||
| Once | 57 (90.4%) | 30 (100.0%) | 27 (81.8%) | ||
| Twice | 6 (9.5%) | 0 (0.0%) | 6 (18.2%) | ||
| All Social Workers (N = 38) | LC− (N = 16) | LC+ (N = 22) | p-Value * | |
|---|---|---|---|---|
| Age | 44.34 ± 14.73 | 47.80 ± 11.29 | 46.18 ± 12.21 | 0.191 |
| Gender | 0.672 | |||
| Females | 30 (78.9%) | 11 (68.7%) | 19 (86.3%) | |
| Males | 8 (21.0%) | 5 (31.2%) | 3 (13.6%) | |
| Educational level | 0.302 | |||
| Middle school | 9 (23.6%) | 3 (18.7%) | 6 (27.2%) | |
| High school | 20 (52.6%) | 8 (50.0%) | 12 (54.5%) | |
| University | 7 (18.4%) | 4 (25.0%) | 3 (13.6%) | |
| Master’s degree | 2 (5.2%) | 1 (6.2%) | 1 (4.5%) | |
| Times of SARS-CoV-2 infection | 0.283 | |||
| Once | 30 (78.9%) | 14 (87.5%) | 16 (72.7%) | |
| Twice | 8 (21.0%) | 2 (12.5%) | 6 (27.2%) |
| Nurses * | p-Value ** | Social Workers * | p-Value ** | Whole Cohort * | p-Value ** | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| Psycho-Emotional Symptoms of Compassion Fatigue | LC− (30) N (%) | LC+ (33) N (%) | LC− (16) N (%) | LC+ (22) N (%) | LC− (46) N(%) | LC+(55) N (%) | ||||
| Psycho-emotional symptoms of compassion fatigue | Mood alteration | 14 (46.7) | 29 (87.9) | <0.001 *** | 11 (68.8) | 22 (100.0) | 0.004 *** | 25 (54.3) | 51 (92.7) | <0.001 *** |
| Restlessness | 8 (26.7) | 27 (81.8) | <0.001 *** | 6 (37.5) | 20 (90.9) | <0.001 *** | 14 (30.4) | 47 (85.4) | <0.001 *** | |
| Irritability | 8 (26.7) | 25 (80.6) | <0.001 *** | 4 (25.0) | 17 (77.3) | 0.001 *** | 12 (26.0) | 42 (76.4) | <0.001 *** | |
| Anger and resentment | 7 (23.3) | 16 (48.5) | <0.001 *** | 2 (12.5) | 11 (50) | 0.161 | 9 (19.5) | 27 (49.0) | <0.001 *** | |
| Anxiety | 6 (20) | 17 (51.5) | <0.001 *** | 6 (37.5) | 19 (86.4) | 0.001 *** | 12 (26.0) | 36 (65.4) | <0.001 *** | |
| Feelings of concern | 6 (20) | 17 (51.5) | <0.001 *** | 7 (43.8) | 10 (43.8) | 0.912 | 13 (28.2) | 27 (49.0) | <0.001 *** | |
| Depression | 0 | 15 (45.5) | <0.001 *** | 0 | 4 (18.2) | 0.713 | 0 | 19 (34.5) | <0.001 | |
| Apathy | 1 (3.3) | 6 (18.2) | <0.001 *** | 2 (12.5) | 4 (18.2) | 0.631 | 3 (6.5) | 10 (18.1) | 0.080 | |
| Hopelessness | 0 | 4 (12.1) | 0.040 | 0 | 1 (4.5) | 0.362 | 0 | 5 (9.0) | 0.040 | |
| Loss of objectivity | 2 (6.7) | 8 (24.2) | <0.001 *** | 0 | 5 (22.7) | 0.041 | 2 (4.3) | 13 (23.6) | 0.010 | |
| Memory-related problems | 6 (20) | 32 (97.0) | <0.001 *** | 2 (12.5) | 22 (100) | <0.001 *** | 8 (17.4) | 54 (98.1) | <0.001 *** | |
| Poor concentration and poor judgment skills | 3 (10) | 25 (75.8) | <0.001 *** | 1 (6.2) | 22 (100) | <0.001 *** | 4 (8.7) | 47 (85.4) | <0.001 *** | |
| Abuse of chemicals | 0 | 5 (15.2) | <0.001 | 0 | 1 (4.5) | 0.382 | 0 | 6 (10.9) | 0.020 | |
| Physical symptoms of compassion fatigue | Fatigue | 13 (61.9) | 22 (66.7) | 0.720 | 0 | 8 (50.0) | <0.001 *** | 13 (28.2) | 30 (54.5) | <0.001 *** |
| Headache | 15 (45.5) | 27 (81.8) | 0.002 *** | 7 (43.8) | 21 (95.5) | <0.001 *** | 22 (47.8) | 48 (87.2) | <0.001 *** | |
| Gastrointestinal problems | 1 (3.3) | 9 (25.0) | 0.014 | 2 (12.5) | 7 (31.8) | 0.163 | 3 (6.5) | 16 (29.0) | <0.001 *** | |
| Muscle aches/pain | 7 (23.3) | 18 (54.5) | 0.011 | 3 (18.8) | 13 (59.1) | 0.0124 | 10 (21.7) | 31 (56.3) | <0.001 *** | |
| Sleep disorders | 6 (20) | 23 (69.7) | <0.001 *** | 4 (25.0) | 14 (87.5) | <0.001 *** | 10 (21.7) | 37 (67.2) | <0.001 *** | |
| Cardiac symptoms | 0 | 14 (42.4) | <0.001 *** | 1 (6.2) | 6 (27.3) | 0.98 1 | 1 (2.2) | 22 (40.0) | <0.001 *** | |
| Social symptoms of compassion fatigue | Insensivity | 1 (3.3) | 3 (9.1) | 0.360 | 0 | 2 (9.1) | 0.213 | 1 (2.2) | 5 (9.0) | 0.150 |
| Isolation and alienation | 1 (3.3) | 10 (30.3) | 0.004 *** | 1 (6.2) | 7 (31.8) | 0.055 | 2 (4.3) | 17 (30.9) | <0.001 *** | |
| Lack of empathy | 0 | 3 (9.1) | 0.090 | 0 | 3 (13.6) | 0.12 1 | 0 | 6 (10.9) | 0.020 | |
| Indifference | 2 (6.7) | 6 (18.2) | 0.170 | 0 | 2 (9.1) | 0.211 | 2 (4.3) | 8 (14.5) | 0.090 | |
| Loss of interest in daily life activities | 3 (10) | 8 (24.2) | 0.130 | 0 | 9 (40.9) | 0.003 *** | 3 (6.5) | 17 (30.9) | <0.001 *** | |
| Social withdrawal | 5 (16.6) | 9 (25.0) | 0.310 | 2 (12.5) | 9 (40.9) | 0.056 | 7 (15.2) | 18 (32.7) | 0.040 | |
| Work-related symptoms of compassion fatigue | Avoiding working with particularly kind of patients | 0 | 6 (18.2) | 0.01 | 1 (6.2) | 2 (9.1) | 0.742 | 1 (2.2) | 8 (14.5) | 0.030 |
| Reduced empathic abilities | 2 (6.7) | 2 (6.0) | 0.920 | 0 | 4 (25.0) | 0.071 | 2 (4.3) | 6 (10.9) | 0.230 | |
| Sickness absenteeism | 0 | 2 (6.0) | 0.170 | 0 | 3 (13.6) | 0.782 | 0 | 5 (9.0) | 0.040 | |
| Reduced performance capabilities | 0 | 5 (15.2) | 0.02 | 0 | 2 (9.1) | 0.21 2 | 0 | 7 (12.7) | 0.010 | |
| Lack of motivation and joy toward work | 0 | 12 (36.3) | <0.001 | 0 | 4 (25) | 0.0713 | 0 | 16 (29.0) | <0.001 *** | |
| Desire to abandon work | 2 (6.7) | 12 (36.3) | 0.004 | 0 | 7 (31.8) | 0.0124 | 2 (4.3) | 19 (34.5) | <0.001 *** | |
| Spiritual symptoms of compassion fatigue | Reduced capacity for discernment | 0 | 6 (18.2) | 0.0100 | 1 (6.2) | 6 (27.3) | 0.098 | 1 (2.2) | 12 (21.8) | <0.001 *** |
| Lack of interest in introspection | 0 | 4 (12.1) | 0.040 | 0 | 6 (27.3) | 0.022 | 0 | 10 (18.1) | <0.001 *** | |
| Lack of spiritual awareness | 0 | 1 (3.03) | 0.320 | 0 | 5 (22.7) | 0.044 | 0 | 6 (10.9) | 0.020 | |
| Existential problems and poor self-assessment | 1 (3.3) | 5 (15.2) | 0.110 | 1 (6.2) | 6 (27.3) | 0.98 2 | 2 (4.3) | 11 (20.0) | 0.020 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
De Luca, R.; Bonanno, M.; Maggio, M.G.; Todaro, A.; Rifici, C.; Mento, C.; Muscatello, M.R.A.; Castorina, M.V.; Tonin, P.; Quartarone, A.; et al. Compassion Fatigue in a Cohort of South Italian Nurses and Hospital-Based Clinical Social Workers Following COVID-19: A Cross-Sectional Survey. J. Clin. Med. 2024, 13, 4200. https://doi.org/10.3390/jcm13144200
De Luca R, Bonanno M, Maggio MG, Todaro A, Rifici C, Mento C, Muscatello MRA, Castorina MV, Tonin P, Quartarone A, et al. Compassion Fatigue in a Cohort of South Italian Nurses and Hospital-Based Clinical Social Workers Following COVID-19: A Cross-Sectional Survey. Journal of Clinical Medicine. 2024; 13(14):4200. https://doi.org/10.3390/jcm13144200
Chicago/Turabian StyleDe Luca, Rosaria, Mirjam Bonanno, Maria Grazia Maggio, Antonino Todaro, Carmela Rifici, Carmela Mento, Maria Rosaria Anna Muscatello, Milva Veronica Castorina, Paolo Tonin, Angelo Quartarone, and et al. 2024. "Compassion Fatigue in a Cohort of South Italian Nurses and Hospital-Based Clinical Social Workers Following COVID-19: A Cross-Sectional Survey" Journal of Clinical Medicine 13, no. 14: 4200. https://doi.org/10.3390/jcm13144200
APA StyleDe Luca, R., Bonanno, M., Maggio, M. G., Todaro, A., Rifici, C., Mento, C., Muscatello, M. R. A., Castorina, M. V., Tonin, P., Quartarone, A., Pugliese, M. E., & Calabrò, R. S. (2024). Compassion Fatigue in a Cohort of South Italian Nurses and Hospital-Based Clinical Social Workers Following COVID-19: A Cross-Sectional Survey. Journal of Clinical Medicine, 13(14), 4200. https://doi.org/10.3390/jcm13144200










