Charting Proficiency: The Learning Curve in Robotic Hysterectomy for Large Uteri Exceeding 1000 g
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. Surgical Procedure
2.3. Definitions of Terms
2.4. Statistical Analysis
3. Results
3.1. Patient Characteristics
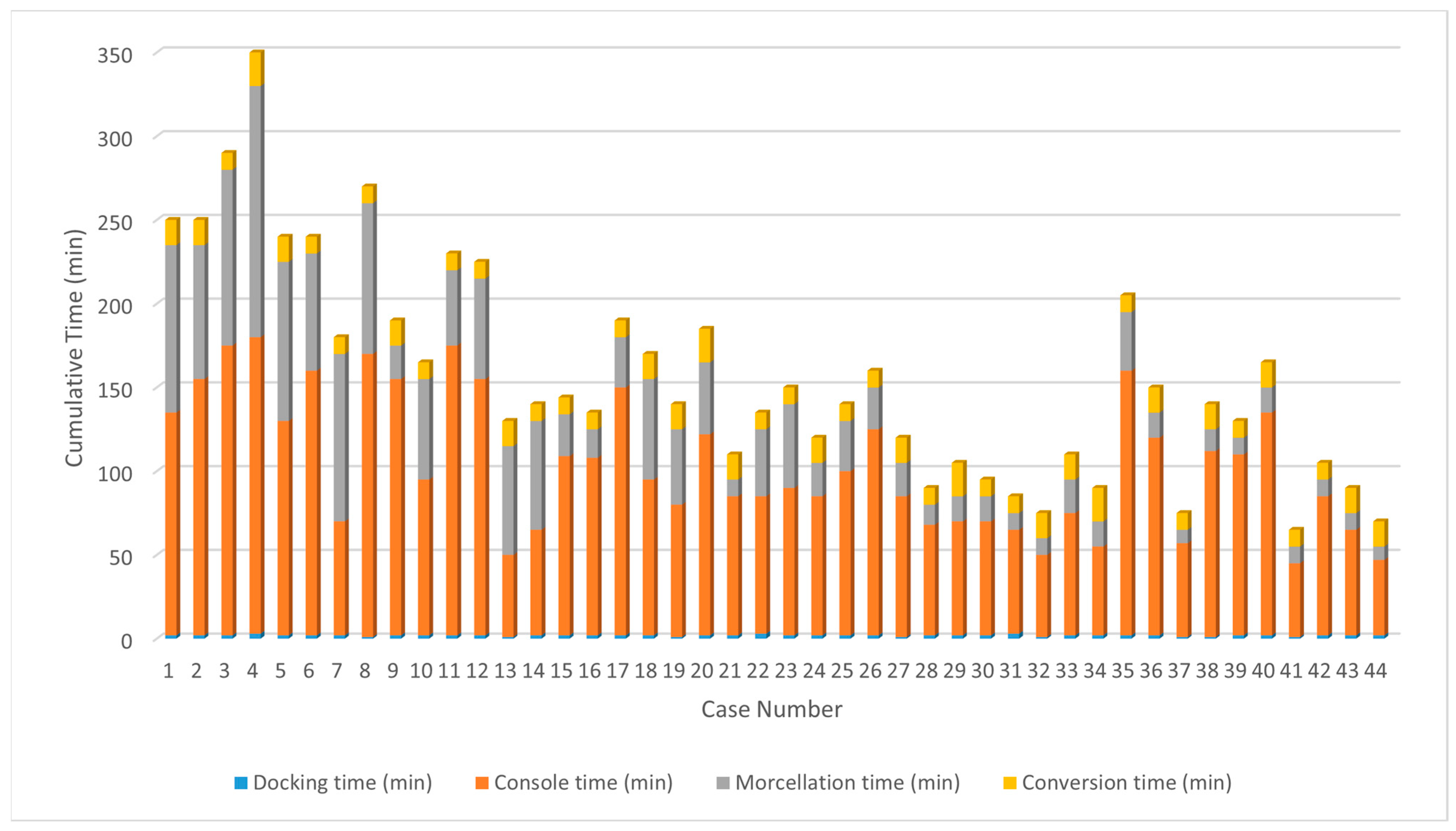
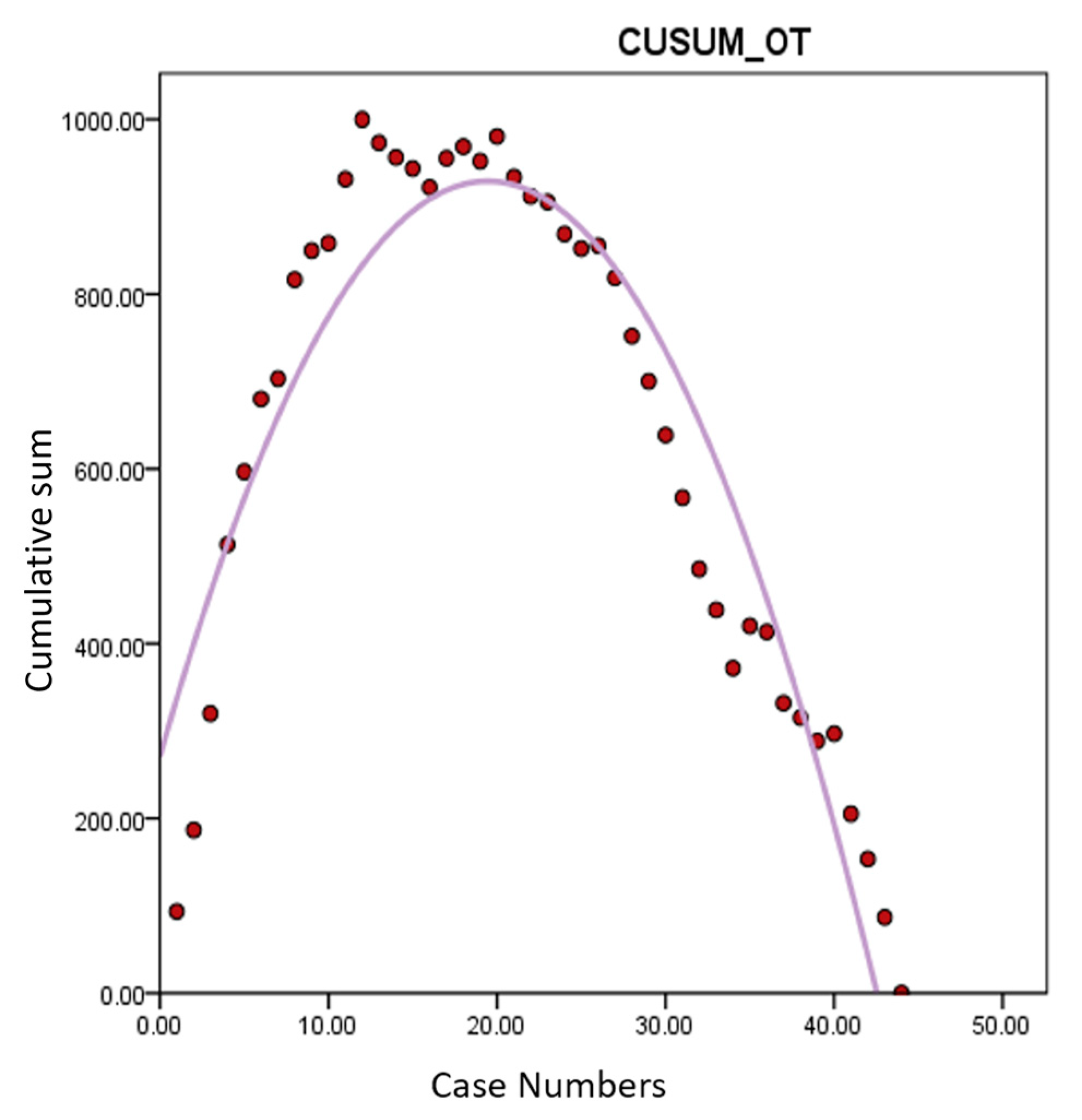
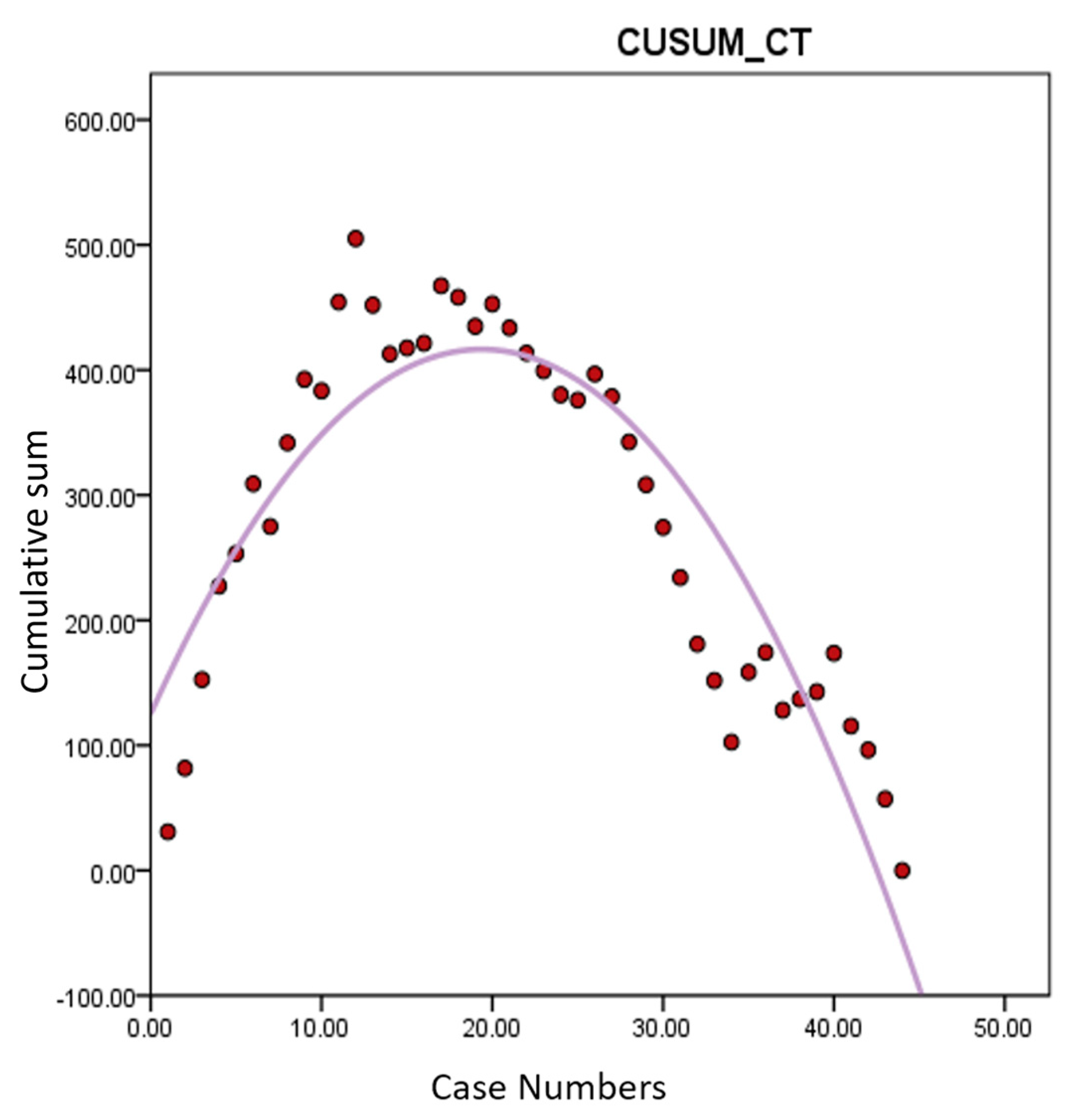
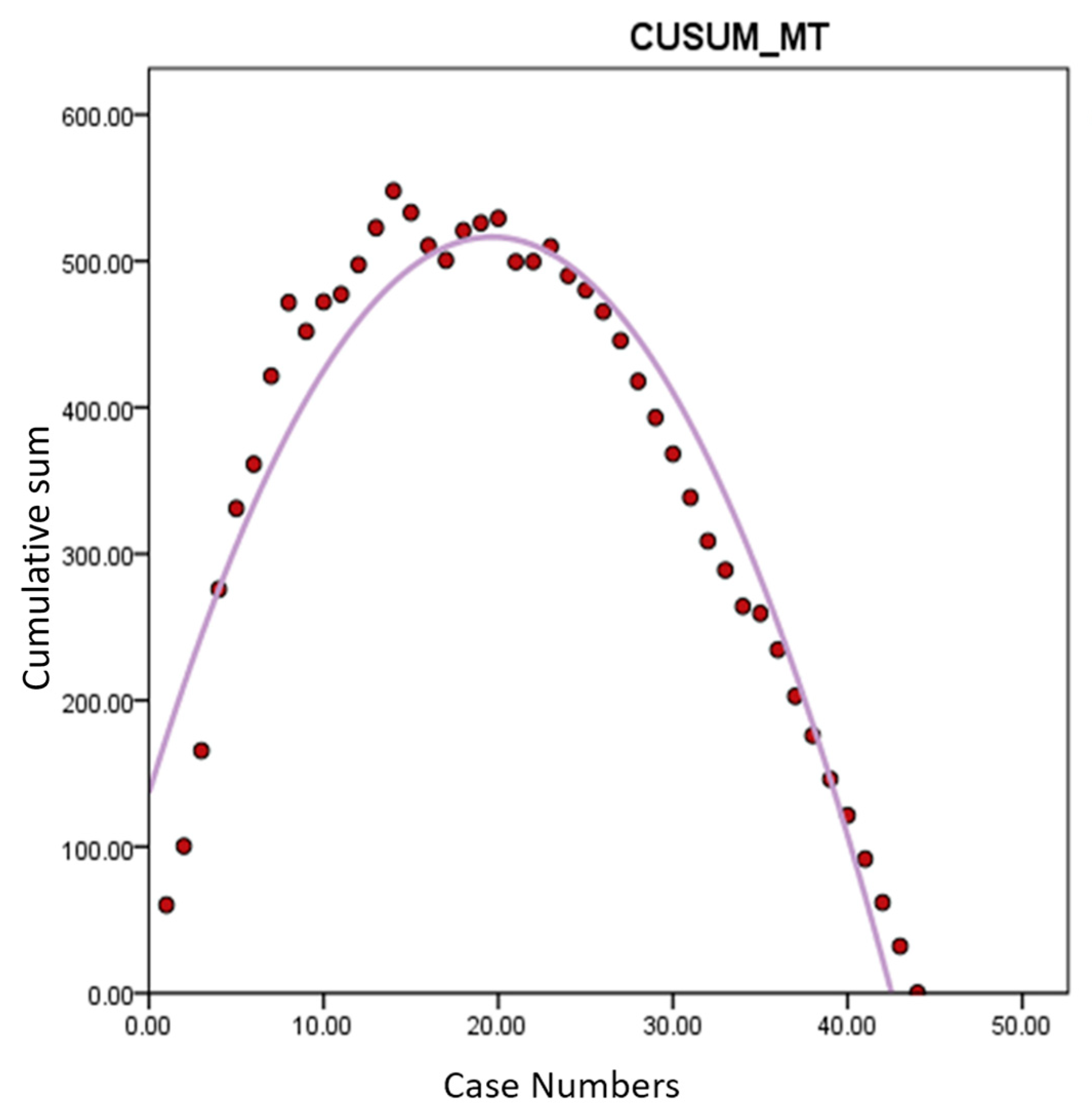
3.2. Learning Curve Analysis
3.3. Comparison of Surgical Outcomes
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Lou, Z.; Huang, Y.; Li, S.; Luo, Z.; Li, C.; Chu, K.; Zhang, T.; Song, P.; Zhou, J. Global, regional, and national time trends in incidence, prevalence, years lived with disability for uterine fibroids, 1990–2019: An age-period-cohort analysis for the global burden of disease 2019 study. BMC Public Health 2023, 23, 916. [Google Scholar] [CrossRef] [PubMed]
- Johnson, N.; Barlow, D.; Lethaby, A.; Tavender, E.; Curr, L.; Garry, R. Methods of hysterectomy: Systematic review and meta-analysis of randomised controlled trials. BMJ 2005, 330, 1478. [Google Scholar] [CrossRef] [PubMed]
- Lambat Emery, S.; Jeannot, E.; Dallenbach, P.; Petignat, P.; Dubuisson, J. Minimally invasive outpatient hysterectomy for a benign indication: A systematic review. J. Gynecol. Obstet. Hum. Reprod. 2024, 53, 102804. [Google Scholar] [CrossRef] [PubMed]
- Luchristt, D.; Brown, O.; Kenton, K.; Bretschneider, C.E. Trends in operative time and outcomes in minimally invasive hysterectomy from 2008 to 2018. Am. J. Obstet. Gynecol. 2021, 224, 202.e1–202.e12. [Google Scholar] [CrossRef] [PubMed]
- Rivero-Moreno, Y.; Echevarria, S.; Vidal-Valderrama, C.; Pianetti, L.; Cordova-Guilarte, J.; Navarro-Gonzalez, J.; Acevedo-Rodriguez, J.; Dorado-Avila, G.; Osorio-Romero, L.; Chavez-Campos, C.; et al. Robotic Surgery: A Comprehensive Review of the Literature and Current Trends. Cureus 2023, 15, e42370. [Google Scholar] [CrossRef] [PubMed]
- Bramhe, S.; Pathak, S.S. Robotic Surgery: A Narrative Review. Cureus 2022, 14, e29179. [Google Scholar] [CrossRef] [PubMed]
- Ngu, J.C.; Tsang, C.B.; Koh, D.C. The da Vinci Xi: A review of its capabilities, versatility, and potential role in robotic colorectal surgery. Robot Surg. 2017, 4, 77–85. [Google Scholar] [CrossRef] [PubMed]
- Sinha, R.; Bana, R.; Mohanty, G.; Sampurna, S. Robotic Hysterectomy for Large Fibroid Uterus–5 Strategies. J. Minim. Invasive Gynecol. 2021, 28, S41. [Google Scholar] [CrossRef]
- Silasi, D.A.; Gallo, T.; Silasi, M.; Menderes, G.; Azodi, M. Robotic versus abdominal hysterectomy for very large uteri. JSLS 2013, 17, 400–406. [Google Scholar] [CrossRef] [PubMed]
- Sinha, R.; Bana, R.; Sanjay, M. Comparison of Robotic and Laparoscopic Hysterectomy for the Large Uterus. JSLS 2019, 23, e2018.00068. [Google Scholar] [CrossRef] [PubMed]
- Nozaki, T.; Matsuda, K.; Kagami, K.; Sakamoto, I. Comparison of surgical outcomes between robot-assisted and conventional laparoscopic hysterectomy for large uterus. J. Robot. Surg. 2023, 17, 2415–2419. [Google Scholar] [CrossRef] [PubMed]
- Lin, P.-L.; Zheng, F.; Shin, M.; Liu, X.; Oh, D.; D’Attilio, D. CUSUM learning curves: What they can and can’t tell us. Surg. Endosc. 2023, 37, 7991–7999. [Google Scholar] [CrossRef] [PubMed]
- Mark, J.R.; Kelly, D.C.; Trabulsi, E.J.; Shenot, P.J.; Lallas, C.D. The effects of fatigue on robotic surgical skill training in Urology residents. J. Robot. Surg. 2014, 8, 269–275. [Google Scholar] [CrossRef] [PubMed]
- Thorarinsson, A.; Fröjd, V.; Kölby, L.; Modin, A.; Lewin, R.; Elander, A.; Mark, H. Blood loss and duration of surgery are independent risk factors for complications after breast reconstruction. J. Plast. Surg. Hand Surg. 2017, 51, 352–357. [Google Scholar] [CrossRef] [PubMed]
- Alshowaikh, K.; Karpinska-Leydier, K.; Amirthalingam, J.; Paidi, G.; Jayarathna, A.I.I.; Salibindla, D.B.A.M.R.; Ergin, H.E. Surgical and patient outcomes of robotic versus conventional laparoscopic hysterectomy: A systematic review. Cureus 2021, 13, e16828. [Google Scholar] [CrossRef] [PubMed]
- Uccella, S.; Kho, R.; Garzon, S.; Casarin, J.; Zorzato, P.C.; Ghezzi, F. The large uterus classification system: A prospective observational study. BJOG Int. J. Obstet. Gynaecol. 2021, 128, 1526–1533. [Google Scholar] [CrossRef] [PubMed]
- Yoder, L.; Elson, N.; Fellner, A.N.; Meister, K.; Guend, H. Residents underestimate their robotic performance: Evaluating resident robotic console participation time. J. Robot. Surg. 2024, 18, 211. [Google Scholar] [CrossRef] [PubMed]
- Roediger, H.L.; Smith, M.A. The “pure-study” learning curve: The learning curve without cumulative testing. Mem. Cogn. 2012, 40, 989–1002. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.; Min, K.J.; Lee, S.; Hong, J.H.; Song, J.Y.; Lee, J.K.; Lee, N.W. Learning curve could affect oncologic outcome of minimally invasive radical hysterectomy for cervical cancer. Asian J. Surg. 2021, 44, 174–180. [Google Scholar] [CrossRef] [PubMed]
| Characteristics | Population (n = 44) |
|---|---|
| Age | 47.18 ± 4.77 |
| BMI (kg/m2) | 25.43 ± 4.74 |
| Parity | |
| Nulliparous | 2 (4.50) |
| Multiparous | 42 (95.50) |
| History of previous abdominal surgery | |
| None | 27 (61.40) |
| C/S only | 13 (29.55) |
| Other MIS | 3 (6.18) |
| Other open surgery | 1 (2.27) |
| Main indication for hysterectomy | |
| Myoma | 33 (75.00) |
| Adenomyosis | 8 (18.20) |
| Endometrial Hyperplasia | 1 (2.27) |
| Malignancy | 2 (4.50) |
| Surgical Outcomes | Group A (n = 20) | Group B (n = 24) | p-Value |
|---|---|---|---|
| BMI (kg/m2) | 25.5 ± 4.80 | 25.4 ± 4.69 | 0.891 |
| Uterine weight (g) | 1268.05 ± 432.14 | 1309.54 ± 328.45 | 0.719 |
| Docking time (min) | 1.90 ± 0.45 | 1.88 ± 0.54 | 0.869 |
| Console time (min) | 124.8 ± 40.41 | 83.29 ± 29.52 | <0.001 |
| Morcellation time (min) | 66.25 ± 33.66 | 17.75 ± 10.94 | <0.001 |
| Conversion time (min) | 12.75 ± 3.43 | 12.92 ± 3.27 | 0.871 |
| Total operation time (min) | 205.7 ± 59.38 | 115.83 ± 34.97 | <0.001 |
| Estimated blood loss (ml) | 310.00 ± 172.14 | 216.67 ± 144.21 | 0.057 |
| Hb difference (g/dL) | 1.68 ± 0.79 | 1.13 ± 0.60 | 0.013 |
| Transfusion | 2 (10.00) | 0 (0.00) | 0.221 |
| PK0 (times) | 0.50 ± 0.61 | 0.5 ± 0.59 | 1 |
| PK1 (times) | 0.35 ± 0.49 | 0.33 ± 0.48 | 0.91 |
| Febrile event (≥37.5 °C) | 5 (25.00) | 7 (29.17) | 0.757 |
| Complications | 0.086 | ||
| Bladder damage | 0 (0.00) | 0 (0.00) | |
| Ureter injury | 0 (0.00) | 0 (0.00) | |
| Bowel injury | 0 (0.00) | 0 (0.00) | |
| Thromboembolic event | 0 (0.00) | 0 (0.00) | |
| Wound problem | 2 (10.00) | 0 (0.00) | |
| Cuff dehiscence | 1 (5.00) | 0 (0.00) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lee, J.; Kim, S. Charting Proficiency: The Learning Curve in Robotic Hysterectomy for Large Uteri Exceeding 1000 g. J. Clin. Med. 2024, 13, 4347. https://doi.org/10.3390/jcm13154347
Lee J, Kim S. Charting Proficiency: The Learning Curve in Robotic Hysterectomy for Large Uteri Exceeding 1000 g. Journal of Clinical Medicine. 2024; 13(15):4347. https://doi.org/10.3390/jcm13154347
Chicago/Turabian StyleLee, Jihyun, and Seongmin Kim. 2024. "Charting Proficiency: The Learning Curve in Robotic Hysterectomy for Large Uteri Exceeding 1000 g" Journal of Clinical Medicine 13, no. 15: 4347. https://doi.org/10.3390/jcm13154347






