Navigating Life with Posterior Urethral Valves—Sexual Health and Lower Urinary Tract Symptoms
Abstract
1. Introduction
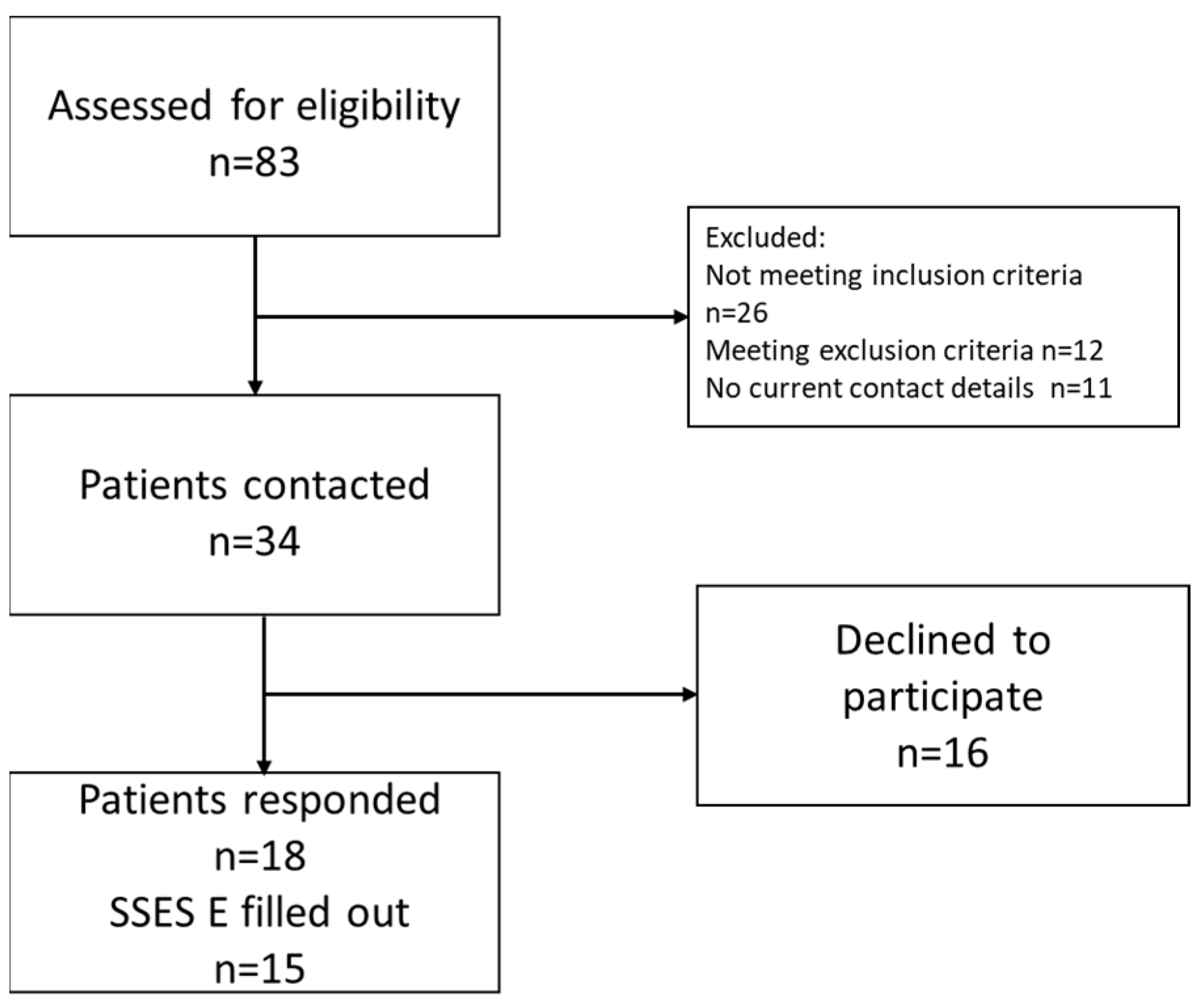
2. Materials and Methods
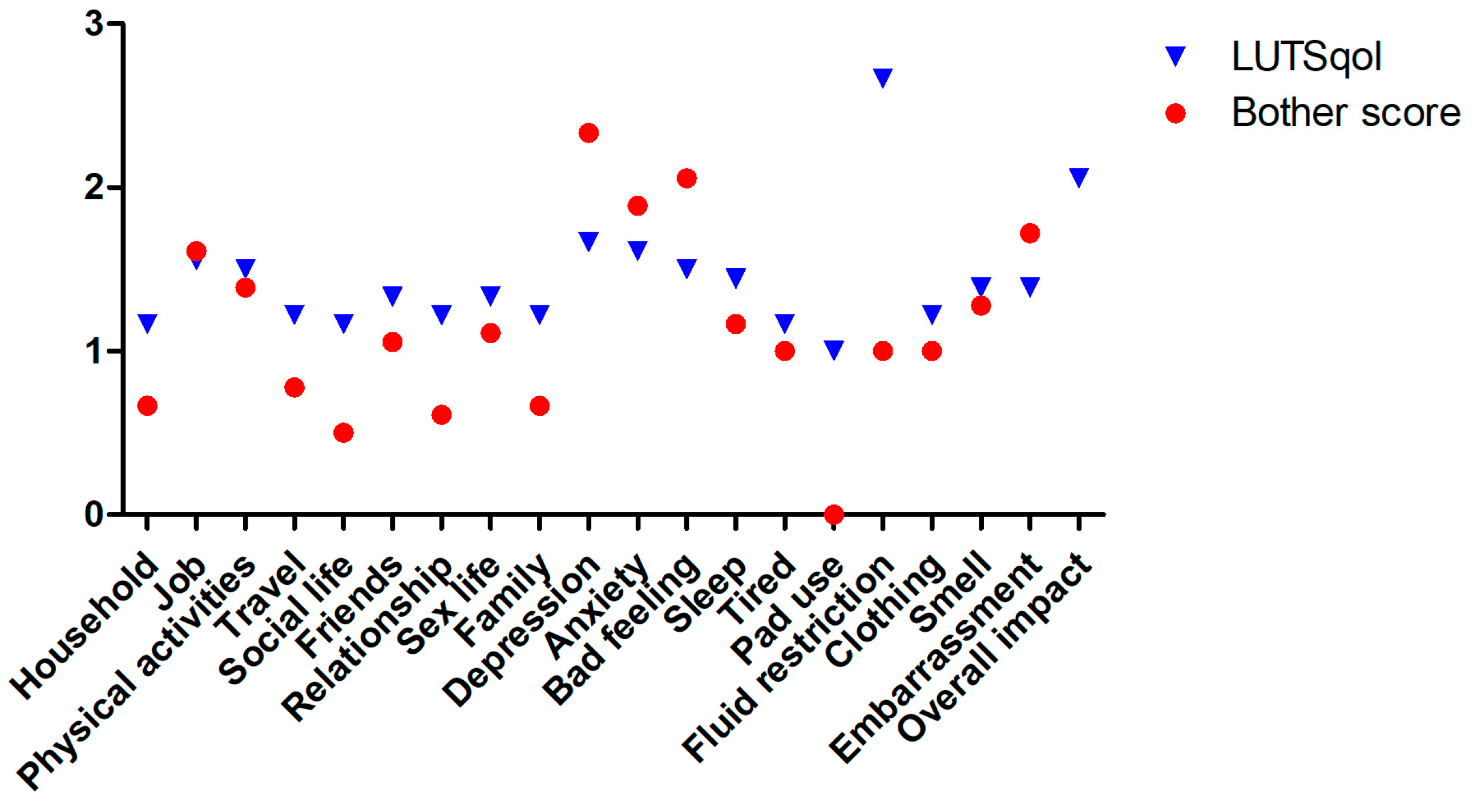
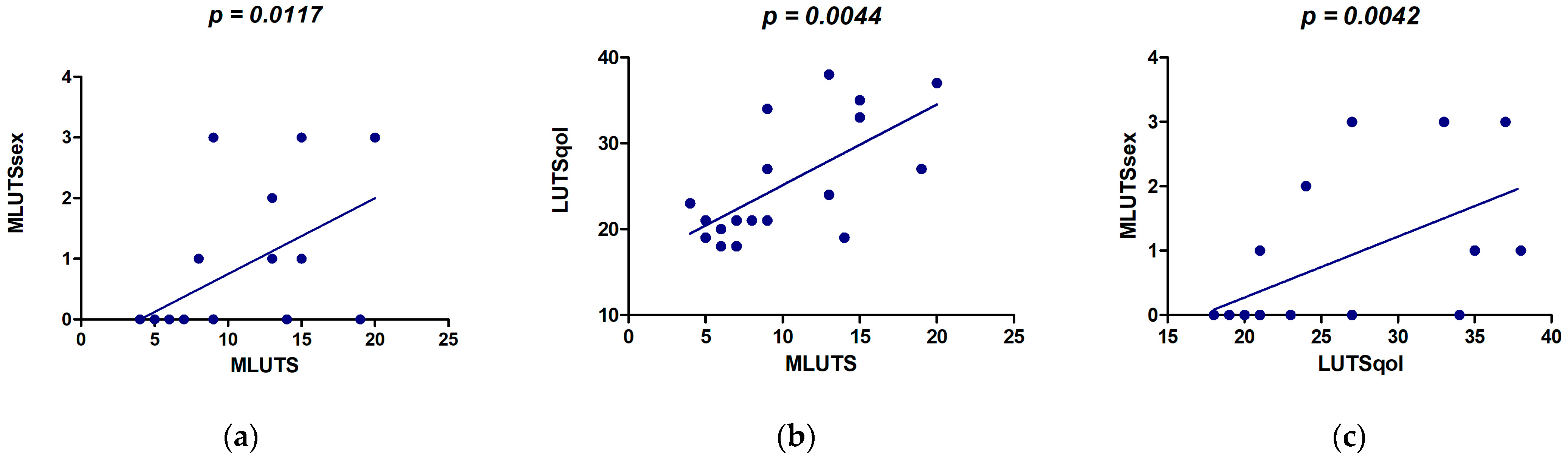
3. Results
4. Discussion
4.1. Lower Urinary Tract Symptoms
4.2. Lower Urinary Tract Symptoms and QoL
4.3. Lower Urinary Tract Symptoms and Sex
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Holmdahl, G.; Sillén, U. Boys with posterior urethral valves: Outcome concerning renal function, bladder function and paternity at ages 31 to 44 years. J. Urol. 2005, 174, 1031–1034; discussion 1034. [Google Scholar] [CrossRef]
- Holmdahl, G.; Sillén, U.; Hanson, E.; Hermansson, G.; Hjälmås, K. Bladder dysfunction in boys with posterior urethral valves before and after puberty. J. Urol. 1996, 155, 694–698. [Google Scholar] [CrossRef] [PubMed]
- Tikkinen, K.A.; Heikkilä, J.; Rintala, R.J.; Tammela, T.L.; Taskinen, S. Lower urinary tract symptoms in adults treated for posterior urethral valves in childhood: Matched cohort study. J. Urol. 2011, 186, 660–666. [Google Scholar] [CrossRef] [PubMed]
- López Pereira, P.; Miguel, M.; Martínez Urrutia, M.J.; Moreno, J.A.; Marcos, M.; Lobato, R.; Jaureguízar, E. Long-term bladder function, fertility and sexual function in patients with posterior urethral valves treated in infancy. J. Pediatr. Urol. 2013, 9, 38–41. [Google Scholar] [CrossRef]
- Jalkanen, J.; Mattila, A.K.; Heikkilä, J.; Roine, R.P.; Sintonen, H.; Taskinen, S. The impact of posterior urethral valves on adult quality of life. J. Pediatr. Urol. 2013, 9, 579–584. [Google Scholar] [CrossRef] [PubMed]
- Zimmer-Gembeck, M.J.; French, J. Associations of Sexual Subjectivity with Global and Sexual Well-Being: A New Measure for Young Males and Comparison to Females. Arch. Sex. Behav. 2016, 45, 315–327. [Google Scholar] [CrossRef]
- Suominen, J.S.; Santtila, P.; Taskinen, S. Sexual Function in Patients Operated on for Bladder Exstrophy and Epispadias. J. Urol. 2015, 194, 195–199. [Google Scholar] [CrossRef] [PubMed]
- Chan, S.W. Chronic Disease Management, Self-Efficacy and Quality of Life. J. Nurs. Res. 2021, 29, e129. [Google Scholar] [CrossRef] [PubMed]
- Villwock, P. Erfassung der Sexuellen Selbstwirksamkeit von Männern und Frauen: Evaluation der Deutschen Versionen der Sexual Self-Efficacy Scale Erectile Functioning (Sexuelle Selbstwirksamkeitsskala für Erektile Funktionsfähigkeit SSES-E-D) und der Sexual Self-Efficacy Scale for Female Functioning (Sexuelle Selbstwirksamkeitsskala für Weibliche Funktionsfähigkeit SSES-F-D). Ph.D. Thesis, University Hospital Jena, Institute of Psychosocial Medicine, Psychotherapy and Psychooncology, Jena, Germany, 2018. [Google Scholar] [CrossRef]
- Ito, H.; Young, G.J.; Lewis, A.L.; Blair, P.S.; Cotterill, N.; Lane, J.A.; Sakamaki, K.; Drake, M.J.; Abrams, P. Grading Severity and Bother Using the International Prostate Symptom Score and International Consultation on Incontinence Questionnaire Male Lower Urinary Tract Symptoms Score in Men Seeking Lower Urinary Tract Symptoms Therapy. J. Urol. 2020, 204, 1003–1011. [Google Scholar] [CrossRef]
- McKown, S.; Abraham, L.; Coyne, K.; Gawlicki, M.; Piault, E.; Vats, V. Linguistic validation of the N-QOL (ICIQ), OAB-q (ICIQ), PPBC, OAB-S and ICIQ-MLUTSsex questionnaires in 16 languages. Int. J. Clin. Pract. 2010, 64, 1643–1652. [Google Scholar] [CrossRef]
- Libman, E.; Rothenberg, I.; Fichten, C.S.; Amsel, R. The SSES-E: A measure of sexual self-efficacy in erectile functioning. J. Sex. Marital. Ther. 1985, 11, 233–247. [Google Scholar] [CrossRef] [PubMed]
- Kluth, L.A.; Dahlem, R.; Becker, A.; Schmid, M.; Soave, A.; Rosenbaum, C.; Ludwig, T.A.; Christ, N.; Rink, M.; Reiss, P.; et al. Psychometric validation of a German language version of a PROM for urethral stricture surgery and preliminary testing of supplementary ED and UI constructs. World J. Urol. 2016, 34, 369–375. [Google Scholar] [CrossRef] [PubMed]
- Schober, J.M.; Dulabon, L.M.; Gor, R.A.; Woodhouse, C.R. Pyospermia in an adult cohort with persistent lower urinary tract symptoms and a history of ablated posterior urethral valve. J. Pediatr. Urol. 2010, 6, 614–618. [Google Scholar] [CrossRef] [PubMed]
- Taskinen, S.; Heikkilä, J.; Rintala, R. Effects of posterior urethral valves on long-term bladder and sexual function. Nat. Rev. Urol. 2012, 9, 699–706. [Google Scholar] [CrossRef] [PubMed]
- De Gennaro, M.; Capitanucci, M.L.; Mosiello, G.; Caione, P.; Silveri, M. The changing urodynamic pattern from infancy to adolescence in boys with posterior urethral valves. BJU Int. 2000, 85, 1104–1108. [Google Scholar] [CrossRef] [PubMed]
- Duckett, J.W. Are ‘valve bladders’ congenital or iatrogenic? Br. J. Urol. 1997, 79, 271–275. [Google Scholar] [CrossRef]
- Coyne, K.S.; Sexton, C.C.; Irwin, D.E.; Kopp, Z.S.; Kelleher, C.J.; Milsom, I. The impact of overactive bladder, incontinence and other lower urinary tract symptoms on quality of life, work productivity, sexuality and emotional well-being in men and women: Results from the EPIC study. BJU Int. 2008, 101, 1388–1395. [Google Scholar] [CrossRef] [PubMed]
- Sacco, E.; Bientinesi, R.; Marangi, F.; D’Addessi, A.; Racioppi, M.; Gulino, G.; Pinto, F.; Totaro, A.; Bassi, P. Overactive bladder syndrome: The social and economic perspective. Urologia 2011, 78, 241–256. [Google Scholar] [CrossRef] [PubMed]
- Himmler, M.; Mühlbauer, J.; Schwarzer, N.; Stein, R.; Younsi, N. Urinary and Fecal Continence in Adolescent and Adult Patients with Cloacal Exstrophy. Urology 2022, 164, 293–299. [Google Scholar] [CrossRef]
- Rickard, M.; Lorenzo, A.J.; Goraya, N.; Kim, J.J.; Khondker, A.; Yadav, P.; Richter, J.; Chua, M.; Santos, J.D. The impact of posterior urethral valves on pediatric quality of life and family function: Prospective analysis of serial patients managed in a dedicated multidisciplinary clinic. J. Pediatr. Urol. 2024, 20, 18–25. [Google Scholar] [CrossRef]
- Hofmann, A.; Ioannou, A.; Zöhrer, P.I.; Rösch, W.H. Ureterocystoplasty in Boys with Valve Bladder Syndrome-Is This Method Still up to Date? Children 2023, 10, 692. [Google Scholar] [CrossRef] [PubMed]
- Çetin, B.; Dönmez, M.; Erdem, S.; Ziylan, O.; Oktar, T. Renal, Bladder and Sexual Outcomes in Adult Men with History of Posterior Urethral Valves Treated in Childhood. Urology 2021, 153, 301–306. [Google Scholar] [CrossRef] [PubMed]
- Taskinen, S.; Heikkilä, J.; Santtila, P.; Rintala, R. Posterior urethral valves and adult sexual function. BJU Int. 2012, 110, E392–E396. [Google Scholar] [CrossRef] [PubMed]
- Keihani, S.; Kajbafzadeh, A.M.; Kameli, S.M.; Abbasioun, R. Long-term Impacts of Concurrent Posterior Urethral Valve Ablation and Bladder Neck Incision on Urinary Continence and Ejaculation. Urology 2017, 99, 278–280. [Google Scholar] [CrossRef] [PubMed]
- Alloussi, S.H.; Lang, C.; Eichel, R.; Alloussi, S. Ejaculation-preserving transurethral resection of prostate and bladder neck: Short- and long-term results of a new innovative resection technique. J. Endourol. 2014, 28, 84–89. [Google Scholar] [CrossRef] [PubMed]
- Yilmaz Sezer, N.; Aker, M.N.; Öner Cengiz, H.; Ersöz, Ş.; Uçar, S. The effect of stoma self-efficacy of people with stoma on their sexual function and satisfaction. Color. Dis. 2023, 25, 2064–2070. [Google Scholar] [CrossRef] [PubMed]
- Edison, B.; Coulter, R.W.S.; Miller, E.; Stokes, L.R.; Hill, A.V. Sexual Communication and Sexual Consent Self-Efficacy among College Students: Implications for Sexually Transmitted Infection Prevention. J. Adolesc. Health 2022, 70, 282–289. [Google Scholar] [CrossRef]
- Swahn, M.H.; Culbreth, R.E.; Gilmore, A.K.; Parrott, D.J.; Daigle, L.E.; Kasirye, R.; Bukuluki, P. Sexual Victimization, Self-Efficacy to Refuse Sex while Drinking, and Regretting Alcohol-Involved Sex among Underserved Youth in Kampala, Uganda. Int. J. Environ. Res. Public Health 2022, 19, 1915. [Google Scholar] [CrossRef]



| n (%) | |
|---|---|
| SSES-E filled out | 15 (83) |
| Age median (IQR) | 23 years (18–26) |
| Micturition via naturalis | 13 (72) |
| ISC | 5 (28) |
| KTx planned | 1 (6) |
| KTx done | 2 (11) |
| Hypertension known | 6 (33) |
| Hypertension treated | 2 (11) |
| In relationship | 10 (56) |
| Follow-up operations | 7 (39) |
| Desire to have children | 0 (0) |
| Fatherhood | 1 (6) |
| Subgroups | ICIQ MLUTS | ICIQ MLUTSsex | ICIQ LUTSqol | SSES-E | SSES-E Erection | SSES-E Ego | SSES-E Interpersonal |
|---|---|---|---|---|---|---|---|
| Age: | |||||||
| ≥24y | 10.7 | 0.6 | 26.3 | 81.65 | 84.2 | 82.71 | 77.34 |
| <24y | 9.625 | 1 | 24.13 | 78.46 | 84.42 | 73.33 | 74.11 |
| p-value | 0.829 | 0.515 | 0.237 | 0.694 | 0.694 | 0.281 | 0.694 |
| Partnership: | |||||||
| yes | 10.7 | 0.8 | 25.9 | 85.64 | 87 | 86.33 | 83.25 |
| no | 9.63 | 0.75 | 24.63 | 69.2 | 78.91 | 62.33 | 61 |
| p-value | 0.829 | 0.965 | 0.696 | 0.099 | 0.371 | 0.003 | 0.055 |
| Hypertension: | |||||||
| yes | 9.5 | 1.3 | 26.5 | 77.44 | 84.73 | 72 | 71,50 |
| no | 10.58 | 0.5 | 24.75 | 81.52 | 84.09 | 81.5 | 78 |
| p-value | 0.82 | 0.18 | 0.494 | 0.594 | 1 | 0.206 | 0.594 |
| Operations: | |||||||
| yes | 10.14 | 1.14 | 30 | 81.76 | 87.1 | 77.33 | 77.75 |
| no | 10.27 | 0.55 | 22.36 | 79.36 | 82.91 | 78.83 | 74.88 |
| p-value | 0.86 | 0.328 | 0.027 | 1 | 0.768 | 0.768 | 0.953 |
| Voiding | 10 | 0.54 | 23.62 | 78.7 | 82.5 | 78.2 | 73.9 |
| ISC | 10.8 | 1.4 | 29.8 | 86 | 91.5 | 78.9 | 83.8 |
| p-value | 0.443 | 0.289 | 0.143 | 0.448 | 0.295 | 1 | 0.448 |
| KTx: | |||||||
| yes | 10 | 0.67 | 24.33 | 80.2 | 82.73 | 84.17 | 73.75 |
| no | 11.3 | 1.3 | 30.33 | 80.15 | 84.55 | 77.44 | 76.15 |
| p-value | 0.654 | 0.426 | 0.36 | 0.933 | 0.686 | 0.476 | 0.476 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zöhrer, P.I.; Vauth, F.; Jaekel, A.K.; Rösch, W.H.; Hofmann, A. Navigating Life with Posterior Urethral Valves—Sexual Health and Lower Urinary Tract Symptoms. J. Clin. Med. 2024, 13, 4380. https://doi.org/10.3390/jcm13154380
Zöhrer PI, Vauth F, Jaekel AK, Rösch WH, Hofmann A. Navigating Life with Posterior Urethral Valves—Sexual Health and Lower Urinary Tract Symptoms. Journal of Clinical Medicine. 2024; 13(15):4380. https://doi.org/10.3390/jcm13154380
Chicago/Turabian StyleZöhrer, Pirmin I., Franziska Vauth, Anke K. Jaekel, Wolfgang H. Rösch, and Aybike Hofmann. 2024. "Navigating Life with Posterior Urethral Valves—Sexual Health and Lower Urinary Tract Symptoms" Journal of Clinical Medicine 13, no. 15: 4380. https://doi.org/10.3390/jcm13154380
APA StyleZöhrer, P. I., Vauth, F., Jaekel, A. K., Rösch, W. H., & Hofmann, A. (2024). Navigating Life with Posterior Urethral Valves—Sexual Health and Lower Urinary Tract Symptoms. Journal of Clinical Medicine, 13(15), 4380. https://doi.org/10.3390/jcm13154380





