Advances in Psychotropic Treatment for Pregnant Women: Efficacy, Adverse Outcomes, and Therapeutic Monitoring
Abstract
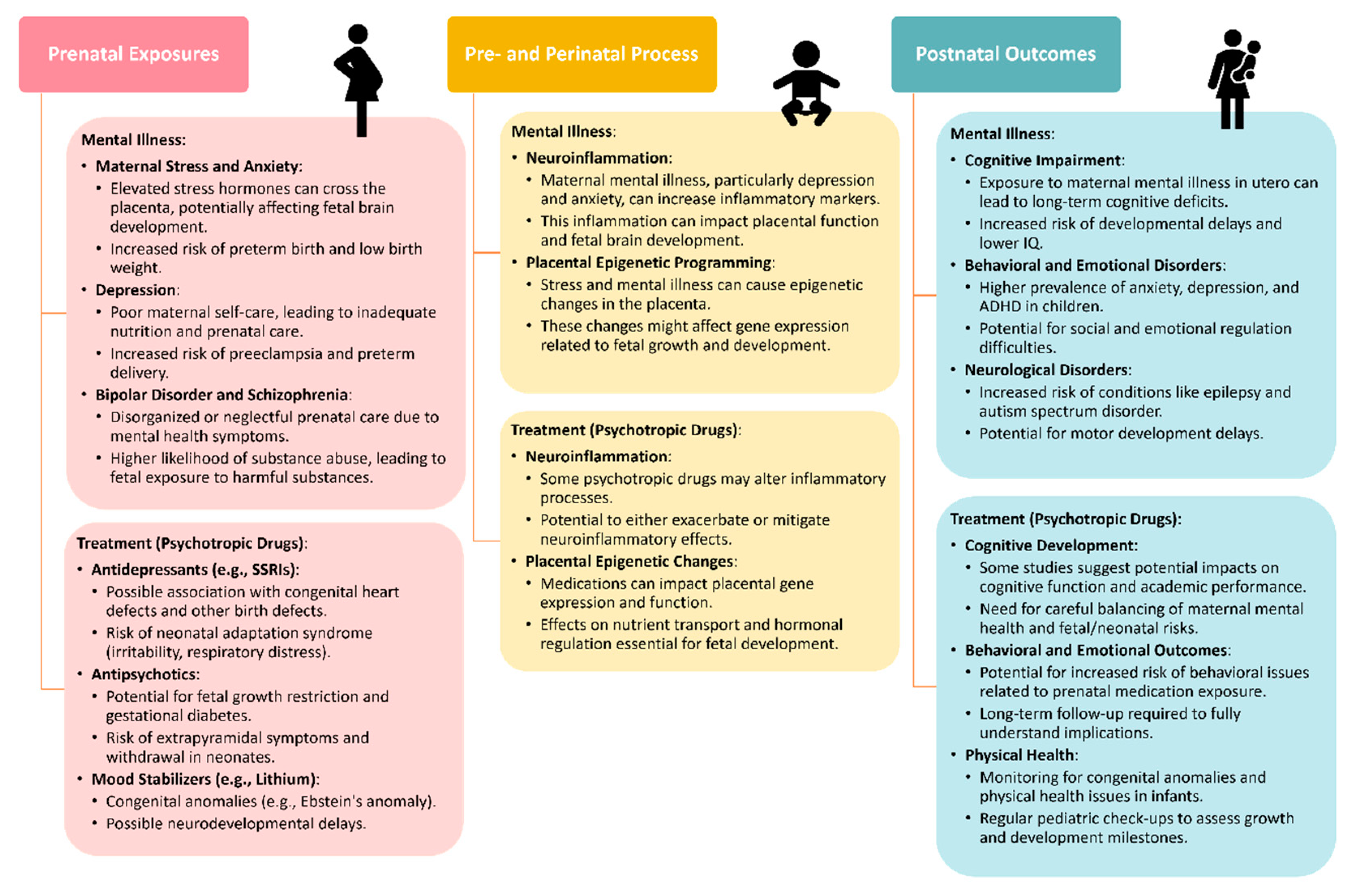
1. Current State of Perinatal Psychiatric Disorders
2. Psychotropic Therapy for Pregnant Women
2.1. Antidepressants
2.2. Mood Stabilizers
2.3. Antipsychotics
2.4. Adverse Outcomes and Risks of Psychotropic Medication Use
3. Individualized Dosing and Therapeutic Monitoring
3.1. The Need for Personalized Treatment in Pregnancy
3.2. Therapeutic Drug Monitoring in Pregnant Women
3.2.1. Sampling and Methods for Drug Level Measurement
3.2.2. Wearable Sensors for Pregnancy
3.3. Methods for Individualized Dosing
3.3.1. Population-Based and Physiologically Based Pharmacokinetic Modelling and Simulation
3.3.2. Real-World Evidence to Improve Decision Making of Best Therapeutic Approaches in Psychotropic Drugs in Pregnant Women
4. Implications on Neonatal Health Outcomes
5. Future Directions and Challenges in Antipsychotic Therapy for Pregnant Women
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Vliegen, N.; Casalin, S.; Luyten, P.; Docx, R.; Lenaerts, M.; Tang, E.; Kempke, S. Hospitalization-Based Treatment for Postpartum Depressed Mothers and Their Babies: Rationale, Principles, and Preliminary Follow-Up Data. Psychiatry Interpers. Biol. Process. 2013, 76, 150–168. [Google Scholar] [CrossRef] [PubMed]
- Darcy, J.M.; Grzywacz, J.G.; Stephens, R.L.; Leng, I.; Clinch, C.R.; Arcury, T.A. Maternal Depressive Symptomatology: 16-Month Follow-up of Infant and Maternal Health-Related Quality of Life. J. Am. Board Fam. Med. 2011, 24, 249–257. [Google Scholar] [CrossRef]
- Pope, C.J.; Xie, B.; Sharma, V.; Campbell, M.K. A Prospective Study of Thoughts of Self-Harm and Suicidal Ideation during the Postpartum Period in Women with Mood Disorders. Arch. Womens Ment. Health 2013, 16, 483–488. [Google Scholar] [CrossRef] [PubMed]
- Dadi, A.F.; Akalu, T.Y.; Wolde, H.F.; Baraki, A.G. Effect of Perinatal Depression on Birth and Infant Health Outcomes: A Systematic Review and Meta-Analysis of Observational Studies from Africa. Arch. Public Health 2022, 80, 34. [Google Scholar] [CrossRef] [PubMed]
- Guintivano, J.; Manuck, T.; Meltzer-Brody, S. Predictors of Postpartum Depression: A Comprehensive Review of the Last Decade of Evidence. Clin. Obstet. Gynecol. 2018, 61, 591–603. [Google Scholar] [CrossRef] [PubMed]
- Dimcea, D.A.-M.; Petca, R.-C.; Dumitrașcu, M.C.; Șandru, F.; Mehedințu, C.; Petca, A. Postpartum Depression: Etiology, Treatment, and Consequences for Maternal Care. Diagnostics 2024, 14, 865. [Google Scholar] [CrossRef]
- McKee, K.; Admon, L.K.; Winkelman, T.N.A.; Muzik, M.; Hall, S.; Dalton, V.K.; Zivin, K. Perinatal Mood and Anxiety Disorders, Serious Mental Illness, and Delivery-Related Health Outcomes, United States, 2006–2015. BMC Womens Health 2020, 20, 150. [Google Scholar] [CrossRef] [PubMed]
- Roddy Mitchell, A.; Gordon, H.; Atkinson, J.; Lindquist, A.; Walker, S.P.; Middleton, A.; Tong, S.; Hastie, R. Prevalence of Perinatal Anxiety and Related Disorders in Low- and Middle-Income Countries. JAMA Netw. Open 2023, 6, e2343711. [Google Scholar] [CrossRef] [PubMed]
- Hernandez, N.D.; Francis, S.; Allen, M.; Bellamy, E.; Sims, O.T.; Oh, H.; Guillaume, D.; Parker, A.; Chandler, R. Prevalence and Predictors of Symptoms of Perinatal Mood and Anxiety Disorders among a Sample of Urban Black Women in the South. Matern. Child Health J. 2022, 26, 770–777. [Google Scholar] [CrossRef]
- Gupta, A.; Pajai, S.; Gupta, A.; Singh Thakur, A.; Muneeba, S.; Batra, N.; Patel, D.J. In the Shadows of Motherhood: A Comprehensive Review of Postpartum Depression Screening and Intervention Practices. Cureus 2024, 16, e54245. [Google Scholar] [CrossRef]
- Horakova, A.; Nemcova, H.; Hrdlickova, K.; Kalli, S.; Davletova, A.; Duarte, M.F.R.S.; Molodina, D.; Riekki, T.; Sebela, A. State of Perinatal Mental Health Care in the WHO Region of Europe: A Scoping Review. Front. Psychiatry 2024, 15, 1350036. [Google Scholar] [CrossRef]
- Sūdžiūtė, K.; Murauskienė, G.; Jarienė, K.; Jaras, A.; Minkauskienė, M.; Adomaitienė, V.; Nedzelskienė, I. Pre-Existing Mental Health Disorders Affect Pregnancy and Neonatal Outcomes: A Retrospective Cohort Study. BMC Pregnancy Childbirth 2020, 20, 419. [Google Scholar] [CrossRef]
- Hagatulah, N.; Bränn, E.; Oberg, A.S.; Valdimarsdóttir, U.A.; Shen, Q.; Lu, D. Perinatal Depression and Risk of Mortality: Nationwide, Register Based Study in Sweden. BMJ 2024, 384, e075462. [Google Scholar] [CrossRef] [PubMed]
- Wohrer, F.; Ngo, H.; DiDomenico, J.; Ma, X.; Roberts, M.H.; Bakhireva, L.N. Potentially Modifiable Risk and Protective Factors Affecting Mental and Emotional Wellness in Pregnancy. Front. Hum. Neurosci. 2024, 18, 1323297. [Google Scholar] [CrossRef] [PubMed]
- Taylor, C.L.; Broadbent, M.; Khondoker, M.; Stewart, R.J.; Howard, L.M. Predictors of Severe Relapse in Pregnant Women with Psychotic or Bipolar Disorders. J. Psychiatr. Res. 2018, 104, 100–107. [Google Scholar] [CrossRef] [PubMed]
- Bergink, V.; Laursen, T.M.; Johannsen, B.M.W.; Kushner, S.A.; Meltzer-Brody, S.; Munk-Olsen, T. Pre-Eclampsia and First-Onset Postpartum Psychiatric Episodes: A Danish Population-Based Cohort Study. Psychol. Med. 2015, 45, 3481–3489. [Google Scholar] [CrossRef] [PubMed]
- Mohamed, M.A.; Elhelbawy, A.; Khalid, M.; AbdAllatif, L.A.; Lialy, H.E. Effects of Bipolar Disorder on Maternal and Fetal Health during Pregnancy: A Systematic Review. BMC Pregnancy Childbirth 2023, 23, 617. [Google Scholar] [CrossRef] [PubMed]
- Chan, J.; Natekar, A.; Einarson, A.; Koren, G. Risks of Untreated Depression in Pregnancy. Can. Fam. Physician 2014, 60, 242–243. [Google Scholar] [PubMed]
- Boisvert, C.; Talarico, R.; Gandhi, J.; Kaluzienski, M.; Dingwall-Harvey, A.L.; White, R.R.; Sampsel, K.; Wen, S.W.; Walker, M.; Muldoon, K.A.; et al. Screening for Postpartum Depression and Risk of Suicidality with Obstetrical Patients: A Cross-Sectional Survey. BMC Pregnancy Childbirth 2023, 23, 635. [Google Scholar] [CrossRef]
- Jarde, A.; Morais, M.; Kingston, D.; Giallo, R.; MacQueen, G.M.; Giglia, L.; Beyene, J.; Wang, Y.; McDonald, S.D. Neonatal Outcomes in Women with Untreated Antenatal Depression Compared with Women Without Depression. JAMA Psychiatry 2016, 73, 826. [Google Scholar] [CrossRef]
- Grote, N.K.; Bridge, J.A.; Gavin, A.R.; Melville, J.L.; Iyengar, S.; Katon, W.J. A Meta-Analysis of Depression During Pregnancy and the Risk of Preterm Birth, Low Birth Weight, and Intrauterine Growth Restriction. Arch. Gen. Psychiatry 2010, 67, 1012. [Google Scholar] [CrossRef]
- Chauhan, A.; Potdar, J. Maternal Mental Health during Pregnancy: A Critical Review. Cureus 2022, 14, e30656. [Google Scholar] [CrossRef] [PubMed]
- McAllister-Williams, R.H.; Baldwin, D.S.; Cantwell, R.; Easter, A.; Gilvarry, E.; Glover, V.; Green, L.; Gregoire, A.; Howard, L.M.; Jones, I.; et al. British Association for Psychopharmacology Consensus Guidance on the Use of Psychotropic Medication Preconception, in Pregnancy and Postpartum 2017. J. Psychopharmacol. 2017, 31, 519–552. [Google Scholar] [CrossRef] [PubMed]
- Cantwell, R. Mental Disorder in Pregnancy and the Early Postpartum. Anaesthesia 2021, 76, 76–83. [Google Scholar] [CrossRef] [PubMed]
- Massoudi, P.; Strömwall, L.A.; Åhlen, J.; Kärrman Fredriksson, M.; Dencker, A.; Andersson, E. Women’s Experiences of Psychological Treatment and Psychosocial Interventions for Postpartum Depression: A Qualitative Systematic Review and Meta-Synthesis. BMC Womens Health 2023, 23, 604. [Google Scholar] [CrossRef] [PubMed]
- Kittel-Schneider, S.; Felice, E.; Buhagiar, R.; Lambregtse-van den Berg, M.; Wilson, C.A.; Banjac Baljak, V.; Vujovic, K.S.; Medic, B.; Opankovic, A.; Fonseca, A.; et al. Treatment of Peripartum Depression with Antidepressants and Other Psychotropic Medications: A Synthesis of Clinical Practice Guidelines in Europe. Int. J. Environ. Res. Public Health 2022, 19, 1973. [Google Scholar] [CrossRef] [PubMed]
- Ward, R.K.; Zamorski, M.A. Benefits and Risks of Psychiatric Medications during Pregnancy. Am. Fam. Physician 2002, 66, 629–636. [Google Scholar] [PubMed]
- Cutler, A.J.; Mattingly, G.W.; Maletic, V. Understanding the Mechanism of Action and Clinical Effects of Neuroactive Steroids and GABAergic Compounds in Major Depressive Disorder. Transl. Psychiatry 2023, 13, 228. [Google Scholar] [CrossRef]
- Jarończyk, M.; Walory, J. Novel Molecular Targets of Antidepressants. Molecules 2022, 27, 533. [Google Scholar] [CrossRef]
- Heal, D.J.; Smith, S.L.; Gosden, J.; Nutt, D.J. Amphetamine, Past and Present—A Pharmacological and Clinical Perspective. J. Psychopharmacol. 2013, 27, 479–496. [Google Scholar] [CrossRef]
- Himmerich, H.; Hamilton, A. Mood Stabilizers: Side Effects, Contraindications, and Interactions. In NeuroPsychopharmacotherapy; Springer International Publishing: Cham, Switzerland, 2022; pp. 1447–1467. [Google Scholar]
- Vinkers, C.H.; Kupka, R.W.; Penninx, B.W.; Ruhé, H.G.; van Gaalen, J.M.; van Haaren, P.C.F.; Schellekens, A.F.A.; Jauhar, S.; Ramos-Quiroga, J.A.; Vieta, E.; et al. Discontinuation of Psychotropic Medication: A Synthesis of Evidence across Medication Classes. Mol. Psychiatry 2024. [Google Scholar] [CrossRef] [PubMed]
- Poweleit, E.A.; Cinibulk, M.A.; Novotny, S.A.; Wagner-Schuman, M.; Ramsey, L.B.; Strawn, J.R. Selective Serotonin Reuptake Inhibitor Pharmacokinetics during Pregnancy: Clinical and Research Implications. Front. Pharmacol. 2022, 13, 833217. [Google Scholar] [CrossRef] [PubMed]
- Griffin, C.E.; Kaye, A.M.; Bueno, F.R.; Kaye, A.D. Benzodiazepine Pharmacology and Central Nervous System-Mediated Effects. Ochsner J. 2013, 13, 214–223. [Google Scholar] [PubMed]
- Edinoff, A.N.; Sathivadivel, N.; McNeil, S.E.; Ly, A.I.; Kweon, J.; Kelkar, N.; Cornett, E.M.; Kaye, A.M.; Kaye, A.D. Antipsychotic Use in Pregnancy: Patient Mental Health Challenges, Teratogenicity, Pregnancy Complications, and Postnatal Risks. Neurol. Int. 2022, 14, 62–74. [Google Scholar] [CrossRef] [PubMed]
- Grover, S.; Avasthi, A. Mood Stabilizers in Pregnancy and Lactation. Indian J. Psychiatry 2015, 57, 308. [Google Scholar] [CrossRef] [PubMed]
- Kieviet, N.; Honig, A.; Dolman, K.M. The Use of Psychotropic Medication during Pregnancy: How about the Newborn? Neuropsychiatr. Dis. Treat. 2013, 9, 1257–1266. [Google Scholar] [CrossRef]
- Mojtabai, R.; Olfson, M. National Trends in Psychotropic Medication Polypharmacy in Office-Based Psychiatry. Arch. Gen. Psychiatry 2010, 67, 26. [Google Scholar] [CrossRef] [PubMed]
- Luo, Y.; Kataoka, Y.; Ostinelli, E.G.; Cipriani, A.; Furukawa, T.A. National Prescription Patterns of Antidepressants in the Treatment of Adults with Major Depression in the US Between 1996 and 2015: A Population Representative Survey Based Analysis. Front. Psychiatry 2020, 11, 35. [Google Scholar] [CrossRef] [PubMed]
- Ram, D.; Gowdappa, B.; Ashoka, H.; Eiman, N. Psychopharmacoteratophobia: Excessive Fear of Malformation Associated with Prescribing Psychotropic Drugs during Pregnancy: An Indian Perspective. Indian. J. Pharmacol. 2015, 47, 484. [Google Scholar] [CrossRef]
- Denton, L.K.; Creeley, C.E.; Stavola, B.; Hall, K.; Foltz, B.D. An Analysis of Online Pregnancy Message Boards: Mother-to-Mother Advice on Medication Use. Women Birth 2020, 33, e48–e58. [Google Scholar] [CrossRef]
- Abdelhafez, M.M.A.; Ahmed, K.A.M.; Ahmed, N.A.M.; Ismail, M.; Mohd Daud, M.N.B.; Ping, N.P.T.; Eldiasty, A.M.; Amri, M.F.B.; Jeffree, M.S.; Kadir, F.; et al. Psychiatric Illness and Pregnancy: A Literature Review. Heliyon 2023, 9, e20958. [Google Scholar] [CrossRef] [PubMed]
- Albertini, E.; Ernst, C.L.; Tamaroff, R.S. Psychopharmacological Decision Making in Bipolar Disorder During Pregnancy and Lactation: A Case-by-Case Approach to Using Current Evidence. Focus 2019, 17, 249–258. [Google Scholar] [CrossRef] [PubMed]
- Caffrey, A.R.; Borrelli, E.P. The Art and Science of Drug Titration. Ther. Adv. Drug Saf. 2020, 11, 204209862095891. [Google Scholar] [CrossRef]
- Jerjes, W.; Ramsay, D.; Stevenson, H.; Lalji, K. Mental Health Polypharmacy in “Non-Coded” Primary Care Patients: The Effect of Deprescribing. J. Clin. Med. 2024, 13, 958. [Google Scholar] [CrossRef]
- Baryakova, T.H.; Pogostin, B.H.; Langer, R.; McHugh, K.J. Overcoming Barriers to Patient Adherence: The Case for Developing Innovative Drug Delivery Systems. Nat. Rev. Drug Discov. 2023, 22, 387–409. [Google Scholar] [CrossRef]
- Weld, E.D.; Bailey, T.C.; Waitt, C. Ethical Issues in Therapeutic Use and Research in Pregnant and Breastfeeding Women. Br. J. Clin. Pharmacol. 2022, 88, 7–21. [Google Scholar] [CrossRef] [PubMed]
- Orsolini, L.; Bellantuono, C. Serotonin Reuptake Inhibitors and Breastfeeding: A Systematic Review. Hum. Psychopharmacol. Clin. Exp. 2015, 30, 4–20. [Google Scholar] [CrossRef]
- Rodieux, F.; Wilbaux, M.; van den Anker, J.N.; Pfister, M. Effect of Kidney Function on Drug Kinetics and Dosing in Neonates, Infants, and Children. Clin. Pharmacokinet. 2015, 54, 1183–1204. [Google Scholar] [CrossRef] [PubMed]
- Arbitman, L.; Chen, S.; Kim, B.; Lee, M.; Zou, P.; Doughty, B.; Li, Y.; Zhang, T. Assessment of Infant Exposure to Antidepressants through Breastfeeding: A Literature Review of Currently Available Approaches. Pharmaceutics 2024, 16, 847. [Google Scholar] [CrossRef]
- Schoretsanitis, G.; Westin, A.A.; Stingl, J.C.; Deligiannidis, K.M.; Paulzen, M.; Spigset, O. Antidepressant Transfer into Amniotic Fluid, Umbilical Cord Blood & Breast Milk: A Systematic Review & Combined Analysis. Prog. Neuropsychopharmacol. Biol. Psychiatry 2021, 107, 110228. [Google Scholar] [CrossRef]
- Lanza Di Scalea, T.; Wisner, K.L. Antidepressant Medication Use during Breastfeeding. Clin. Obstet. Gynecol. 2009, 52, 483–497. [Google Scholar] [CrossRef] [PubMed]
- Fatima, Z.; Zahra, A.; Ghouse, M.; Wang, X.; Yuan, Z. Maternal SSRIs Experience and Risk of ASD in Offspring: A Review. Toxicol. Res. 2018, 7, 1020–1028. [Google Scholar] [CrossRef] [PubMed]
- Bérard, A.; Sheehy, O.; Zhao, J.; Vinet, É.; Bernatsky, S.; Abrahamowicz, M. SSRI and SNRI Use during Pregnancy and the Risk of Persistent Pulmonary Hypertension of the Newborn. Br. J. Clin. Pharmacol. 2017, 83, 1126–1133. [Google Scholar] [CrossRef] [PubMed]
- Nikfar, S.; Rahimi, R.; Hendoiee, N.; Abdollahi, M. Increasing the Risk of Spontaneous Abortion and Major Malformations in Newborns Following Use of Serotonin Reuptake Inhibitors during Pregnancy: A Systematic Review and Updated Meta-Analysis. DARU J. Pharm. Sci. 2012, 20, 75. [Google Scholar] [CrossRef] [PubMed]
- Uguz, F. A New Safety Scoring System for the Use of Psychotropic Drugs During Lactation. Am. J. Ther. 2021, 28, e118–e126. [Google Scholar] [CrossRef]
- Gentile, S. Tricyclic Antidepressants in Pregnancy and Puerperium. Expert. Opin. Drug Saf. 2014, 13, 207–225. [Google Scholar] [CrossRef]
- Betcher, H.K.; Wisner, K.L. Psychotropic Treatment during Pregnancy: Research Synthesis and Clinical Care Principles. J. Womens Health 2020, 29, 310–318. [Google Scholar] [CrossRef]
- Burke, M.; Fillion, M.; Mejia, J.; Ervin, F.; Palmour, R. Perinatal MAO Inhibition Produces Long-Lasting Impairment of Serotonin Function in Offspring. Brain Sci. 2018, 8, 106. [Google Scholar] [CrossRef]
- Edinoff, A.N.; Odisho, A.S.; Lewis, K.; Kaskas, A.; Hunt, G.; Cornett, E.M.; Kaye, A.D.; Kaye, A.; Morgan, J.; Barrilleaux, P.S.; et al. Brexanolone, a GABAA Modulator, in the Treatment of Postpartum Depression in Adults: A Comprehensive Review. Front. Psychiatry 2021, 12, 699740. [Google Scholar] [CrossRef]
- Dacarett-Galeano, D.J.; Diao, X.Y. Brexanolone: A Novel Therapeutic in the Treatment of Postpartum Depression. Am. J. Psychiatry Resid. J. 2019, 15, 2–4. [Google Scholar] [CrossRef]
- Leader, L.D.; O’Connell, M.; VandenBerg, A. Brexanolone for Postpartum Depression: Clinical Evidence and Practical Considerations. Pharmacother. J. Hum. Pharmacol. Drug Ther. 2019, 39, 1105–1112. [Google Scholar] [CrossRef] [PubMed]
- Licheri, V.; Talani, G.; Gorule, A.A.; Mostallino, M.C.; Biggio, G.; Sanna, E. Plasticity of GABAA Receptors during Pregnancy and Postpartum Period: From Gene to Function. Neural Plast. 2015, 2015, 170435. [Google Scholar] [CrossRef] [PubMed]
- Pinna, G. Allopregnanolone, the Neuromodulator Turned Therapeutic Agent: Thank You, Next? Front. Endocrinol. 2020, 11, 236. [Google Scholar] [CrossRef]
- FDA. Approves First Treatment for Post-Partum Depression. Available online: https://www.fda.gov/news-events/press-announcements/fda-approves-first-treatment-post-partum-depression (accessed on 16 July 2024).
- Reddy, D.S.; Mbilinyi, R.H.; Estes, E. Preclinical and Clinical Pharmacology of Brexanolone (Allopregnanolone) for Postpartum Depression: A Landmark Journey from Concept to Clinic in Neurosteroid Replacement Therapy. Psychopharmacology 2023, 240, 1841–1863. [Google Scholar] [CrossRef] [PubMed]
- Cornett, E.M.; Rando, L.; Labbé, A.M.; Perkins, W.; Kaye, A.M.; Kaye, A.D.; Viswanath, O.; Urits, I. Brexanolone to Treat Postpartum Depression in Adult Women. Psychopharmacol. Bull. 2021, 51, 115–130. [Google Scholar]
- Cipolla, S.; Catapano, P.; Messina, M.; Pezzella, P.; Giordano, G.M. Safety of Electroconvulsive Therapy (ECT) in Pregnancy: A Systematic Review of Case Reports and Case Series. Arch. Womens Ment. Health 2024, 27, 157–178. [Google Scholar] [CrossRef]
- Rose, S.; Dotters-Katz, S.K.; Kuller, J.A. Electroconvulsive Therapy in Pregnancy: Safety, Best Practices, and Barriers to Care. Obstet. Gynecol. Surv. 2020, 75, 199–203. [Google Scholar] [CrossRef]
- Galbally, M.; Frayne, J.; Watson, S.J.; Snellen, M. Psychopharmacological Prescribing Practices in Pregnancy for Women with Severe Mental Illness: A Multicentre Study. Eur. Neuropsychopharmacol. 2019, 29, 57–65. [Google Scholar] [CrossRef]
- Poels, E.M.P.; Bijma, H.H.; Galbally, M.; Bergink, V. Lithium during Pregnancy and after Delivery: A Review. Int. J. Bipolar Disord. 2018, 6, 26. [Google Scholar] [CrossRef]
- Viguera, A.C. Risk of Recurrence of Bipolar Disorder in Pregnant and Nonpregnant Women after Discontinuing Lithium Maintenance. Am. J. Psychiatry 2000, 157, 179–184. [Google Scholar] [CrossRef]
- Fornaro, M.; Maritan, E.; Ferranti, R.; Zaninotto, L.; Miola, A.; Anastasia, A.; Murru, A.; Solé, E.; Stubbs, B.; Carvalho, A.F.; et al. Lithium Exposure During Pregnancy and the Postpartum Period: A Systematic Review and Meta-Analysis of Safety and Efficacy Outcomes. Am. J. Psychiatry 2020, 177, 76–92. [Google Scholar] [CrossRef] [PubMed]
- Patorno, E.; Huybrechts, K.F.; Bateman, B.T.; Cohen, J.M.; Desai, R.J.; Mogun, H.; Cohen, L.S.; Hernandez-Diaz, S. Lithium Use in Pregnancy and the Risk of Cardiac Malformations. N. Engl. J. Med. 2017, 376, 2245–2254. [Google Scholar] [CrossRef] [PubMed]
- Hastie, R.; Tong, S.; Hiscock, R.; Lindquist, A.; Lindström, L.; Wikström, A.-K.; Sundström-Poromaa, I. Maternal Lithium Use and the Risk of Adverse Pregnancy and Neonatal Outcomes: A Swedish Population-Based Cohort Study. BMC Med. 2021, 19, 291. [Google Scholar] [CrossRef]
- Wiggs, K.K.; Rickert, M.E.; Quinn, P.D.; D’Onofrio, B.M.; Sara Öberg, A. Specific Birth Defects Following Antiseizure Medications Used by Pregnant Women with Epilepsy. Neurol. Clin. Pract. 2024, 14, e200289. [Google Scholar] [CrossRef] [PubMed]
- Holmes, L.B.; Baldwin, E.J.; Smith, C.R.; Habecker, E.; Glassman, L.; Wong, S.L.; Wyszynski, D.F. Increased Frequency of Isolated Cleft Palate in Infants Exposed to Lamotrigine during Pregnancy. Neurology 2008, 70, 2152–2158. [Google Scholar] [CrossRef]
- Ornoy, A.; Weinstein-Fudim, L.; Ergaz, Z. Antidepressants, Antipsychotics, and Mood Stabilizers in Pregnancy: What Do We Know and How Should We Treat Pregnant Women with Depression. Birth Defects Res. 2017, 109, 933–956. [Google Scholar] [CrossRef] [PubMed]
- Wang, M.-L.; Tao, Y.-Y.; Sun, X.-Y.; Guo, Y.; Wang, Z.-Y.; Cao, Y.-F.; Zhao, L. Estrogen Profile- and Pharmacogenetics-Based Lamotrigine Dosing Regimen Optimization: Recommendations for Pregnant Women with Epilepsy. Pharmacol. Res. 2021, 169, 105610. [Google Scholar] [CrossRef] [PubMed]
- Matlow, J.; Koren, G. Is Carbamazepine Safe to Take during Pregnancy? Can. Fam. Physician 2012, 58, 163–164. [Google Scholar] [PubMed]
- Schäfer, M.; Brandl, E.J. Mood Stabilizers: Valproate. In NeuroPsychopharmacotherapy; Springer International Publishing: Cham, Switzerland, 2022; pp. 1549–1557. [Google Scholar]
- Güveli, B.T.; Rosti, R.Ö.; Güzeltaş, A.; Tuna, E.B.; Ataklı, D.; Sencer, S.; Yekeler, E.; Kayserili, H.; Dirican, A.; Bebek, N.; et al. Teratogenicity of Antiepileptic Drugs. Clin. Psychopharmacol. Neurosci. 2017, 15, 19–27. [Google Scholar] [CrossRef]
- Macfarlane, A.; Greenhalgh, T. Sodium Valproate in Pregnancy: What Are the Risks and Should We Use a Shared Decision-Making Approach? BMC Pregnancy Childbirth 2018, 18, 200. [Google Scholar] [CrossRef]
- Carli, M.; Weiss, F.; Grenno, G.; Ponzini, S.; Kolachalam, S.; Vaglini, F.; Viaggi, C.; Pardini, C.; Tidona, S.; Longoni, B.; et al. Pharmacological Strategies for Bipolar Disorders in Acute Phases and Chronic Management with a Special Focus on Lithium, Valproic Acid, and Atypical Antipsychotics. Curr. Neuropharmacol. 2023, 21, 935–950. [Google Scholar] [CrossRef] [PubMed]
- Galappatthy, P.; Liyanage, C.K.; Lucas, M.N.; Jayasekara, D.T.L.M.; Abhayaratna, S.A.; Weeraratne, C.; De Abrew, K.; Gunaratne, P.S.; Gamage, R.; Wijeyaratne, C.N. Obstetric Outcomes and Effects on Babies Born to Women Treated for Epilepsy during Pregnancy in a Resource Limited Setting: A Comparative Cohort Study. BMC Pregnancy Childbirth 2018, 18, 230. [Google Scholar] [CrossRef] [PubMed]
- Smolinski, N.E.; Sarayani, A.; Thai, T.N.; Jugl, S.; Ewig, C.L.Y.; Winterstein, A.G. Prenatal Exposure to Valproic Acid across Various Indications for Use. JAMA Netw. Open 2024, 7, e2412680. [Google Scholar] [CrossRef]
- Smith, C.J.; Payne, V.M. Epidemiology Studies on Effects of Lithium Salts in Pregnancy Are Confounded by the Inability to Control for Other Potentially Teratogenic Factors. Hum. Exp. Toxicol. 2024, 43, 1–16. [Google Scholar] [CrossRef] [PubMed]
- Diav-Citrin, O.; Shechtman, S.; Tahover, E.; Finkel-Pekarsky, V.; Arnon, J.; Kennedy, D.; Erebara, A.; Einarson, A.; Ornoy, A. Pregnancy Outcome Following in Utero Exposure to Lithium: A Prospective, Comparative, Observational Study. Am. J. Psychiatry 2014, 171, 785–794. [Google Scholar] [CrossRef] [PubMed]
- Heinonen, E.; Forsberg, L.; Nörby, U.; Wide, K.; Källén, K. Antipsychotic Use During Pregnancy and Risk for Gestational Diabetes: A National Register-Based Cohort Study in Sweden. CNS Drugs 2022, 36, 529–539. [Google Scholar] [CrossRef] [PubMed]
- Stamou, G.; García-Palacios, A.; Botella, C. Cognitive-Behavioural Therapy and Interpersonal Psychotherapy for the Treatment of Post-Natal Depression: A Narrative Review. BMC Psychol. 2018, 6, 28. [Google Scholar] [CrossRef]
- Betcher, H.K.; Montiel, C.; Clark, C.T. Use of Antipsychotic Drugs during Pregnancy. Curr. Treat. Options Psychiatry 2019, 6, 17–31. [Google Scholar] [CrossRef] [PubMed]
- Reutfors, J.; Cesta, C.E.; Cohen, J.M.; Bateman, B.T.; Brauer, R.; Einarsdóttir, K.; Engeland, A.; Furu, K.; Gissler, M.; Havard, A.; et al. Antipsychotic Drug Use in Pregnancy: A Multinational Study from Ten Countries. Schizophr. Res. 2020, 220, 106–115. [Google Scholar] [CrossRef]
- Ennis, Z.N.; Damkier, P. Pregnancy Exposure to Olanzapine, Quetiapine, Risperidone, Aripiprazole and Risk of Congenital Malformations. A Systematic Review. Basic Clin. Pharmacol. Toxicol. 2015, 116, 315–320. [Google Scholar] [CrossRef]
- Chatterjee, K.; Dangi, A.; Sharma, R.; Yadav, P.; Chauhan, V.; Prakash, J. Adding Pre-Emptive Anticholinergics to Antipsychotics: Is It Justified? Ind. Psychiatry J. 2022, 31, 370–373. [Google Scholar] [CrossRef] [PubMed]
- Traugott, P.; Medina, A.; Parker, J.M. Navigating the Complexity of a Bipolar Pregnant Patient with Multiple Comorbidities. Cureus 2024, 16, e51510. [Google Scholar] [CrossRef] [PubMed]
- Sadowski, A.; Todorow, M.; Yazdani Brojeni, P.; Koren, G.; Nulman, I. Pregnancy Outcomes Following Maternal Exposure to Second-Generation Antipsychotics given with Other Psychotropic Drugs: A Cohort Study. BMJ Open 2013, 3, e003062. [Google Scholar] [CrossRef]
- Subramanian, A.; Azcoaga-Lorenzo, A.; Anand, A.; Phillips, K.; Lee, S.I.; Cockburn, N.; Fagbamigbe, A.F.; Damase-Michel, C.; Yau, C.; McCowan, C.; et al. Polypharmacy during Pregnancy and Associated Risk Factors: A Retrospective Analysis of 577 Medication Exposures among 1.5 Million Pregnancies in the UK, 2000-2019. BMC Med. 2023, 21, 21. [Google Scholar] [CrossRef]
- Costa, G.d.A.; Galvão, T.C.; Bacchi, A.D.; Moreira, E.G.; Salles, M.J.S. Investigation of Possible Teratogenic Effects in the Offspring of Mice Exposed to Methylphenidate during Pregnancy. Reprod. Biomed. Online 2016, 32, 170–177. [Google Scholar] [CrossRef] [PubMed]
- Anderson, K.N.; Dutton, A.C.; Broussard, C.S.; Farr, S.L.; Lind, J.N.; Visser, S.N.; Ailes, E.C.; Shapira, S.K.; Reefhuis, J.; Tinker, S.C. ADHD Medication Use During Pregnancy and Risk for Selected Birth Defects: National Birth Defects Prevention Study, 1998–2011. J. Atten. Disord. 2020, 24, 479–489. [Google Scholar] [CrossRef] [PubMed]
- Li, L.; Sujan, A.C.; Butwicka, A.; Chang, Z.; Cortese, S.; Quinn, P.; Viktorin, A.; Öberg, A.S.; D’Onofrio, B.M.; Larsson, H. Associations of Prescribed ADHD Medication in Pregnancy with Pregnancy-Related and Offspring Outcomes: A Systematic Review. CNS Drugs 2020, 34, 731–747. [Google Scholar] [CrossRef] [PubMed]
- Dolovich, L.R.; Addis, A.; Vaillancourt, J.M.R.; Power, J.D.B.; Koren, G.; Einarson, T.R. Benzodiazepine Use in Pregnancy and Major Malformations or Oral Cleft: Meta-Analysis of Cohort and Case-Control Studies. BMJ 1998, 317, 839–843. [Google Scholar] [CrossRef]
- Iqbal, S.; Jubeen, F.; Sher, F. Future of 5-Fluorouracil in Cancer Therapeutics, Current Pharmacokinetics Issues and a Way Forward. J. Cancer Res. Pract. 2019, 6, 155. [Google Scholar] [CrossRef]
- Ghiasi, N.; Bhansali, R.K.; Marwaha, R. Lorazepam. In StatPearls [Internet]; StatPearls Publishing: Treasure Island, FL, USA, 2023. [Google Scholar]
- Payne, J.L. Psychiatric Medication Use in Pregnancy and Breastfeeding. Obstet. Gynecol. Clin. N. Am. 2021, 48, 131–149. [Google Scholar] [CrossRef]
- Bouchette, D.; Akhondi, H.; Quick, J. Zolpidem.[Updated 2022 Oct 1]. In StatPearls [Internet; StatPearls Publishing: Treasure Island, FL, USA, 2022. [Google Scholar]
- Glover, V. Prenatal Mental Health and the Effects of Stress on the Foetus and the Child. Should Psychiatrists Look beyond Mental Disorders? World Psychiatry 2020, 19, 331–332. [Google Scholar] [CrossRef] [PubMed]
- Howard, L.M.; Khalifeh, H. Perinatal Mental Health: A Review of Progress and Challenges. World Psychiatry 2020, 19, 313–327. [Google Scholar] [CrossRef] [PubMed]
- Garr Barry, V.; Johnson, T.N.; Herrick, C.; Lindley, K.; Carter, E.B. Adverse Pregnancy Outcomes and Postpartum Care as a Pathway to Future Health. Clin. Obstet. Gynecol. 2022, 65, 632–647. [Google Scholar] [CrossRef] [PubMed]
- Christensen, J.; Zoega, H.; Leinonen, M.K.; Gilhus, N.E.; Gissler, M.; Igland, J.; Sun, Y.; Tomson, T.; Alvestad, S.; Bjørk, M.-H.; et al. Prenatal Exposure to Antiseizure Medications and Fetal Growth: A Population-Based Cohort Study from the Nordic Countries. Lancet Reg. Health-Eur. 2024, 38, 100849. [Google Scholar] [CrossRef] [PubMed]
- Belete, H.; Ali, T.; Legas, G.; Pavon, L. Relapse and Clinical Characteristics of Patients with Bipolar Disorders in Central Ethiopia: A Cross-Sectional Study. Psychiatry J. 2020, 2020, 8986014. [Google Scholar] [CrossRef] [PubMed]
- Chow, R.T.S.; Whiting, D.; Favril, L.; Ostinelli, E.; Cipriani, A.; Fazel, S. An Umbrella Review of Adverse Effects Associated with Antipsychotic Medications: The Need for Complementary Study Designs. Neurosci. Biobehav. Rev. 2023, 155, 105454. [Google Scholar] [CrossRef]
- Jagtap, A.; Jagtap, B.; Jagtap, R.; Lamture, Y.; Gomase, K. Effects of Prenatal Stress on Behavior, Cognition, and Psychopathology: A Comprehensive Review. Cureus 2023, 15, e47044. [Google Scholar] [CrossRef]
- Newport, D.J.; Calamaras, M.R.; DeVane, C.L.; Donovan, J.; Beach, A.J.; Winn, S.; Knight, B.T.; Gibson, B.B.; Viguera, A.C.; Owens, M.J.; et al. Atypical Antipsychotic Administration during Late Pregnancy: Placental Passage and Obstetrical Outcomes. Am. J. Psychiatry 2007, 164, 1214–1220. [Google Scholar] [CrossRef]
- Hrdličková, K.; Němcová, H.; Horáková, A.; Šebela, A. Use of Antipsychotics during Pregnancy and Their Impact on Congenital Malformations and Early Neonatal Adaptation. Ceska Gynekol. 2023, 88, 221–230. [Google Scholar] [CrossRef]
- Gastaldon, C.; Arzenton, E.; Raschi, E.; Spigset, O.; Papola, D.; Ostuzzi, G.; Moretti, U.; Trifirò, G.; Barbui, C.; Schoretsanitis, G. Neonatal Withdrawal Syndrome Following in Utero Exposure to Antidepressants: A Disproportionality Analysis of VigiBase, the WHO Spontaneous Reporting Database. Psychol. Med. 2023, 53, 5645–5653. [Google Scholar] [CrossRef]
- Khan, L. Neonatal Abstinence Syndrome. Pediatr. Ann. 2020, 49, e3–e7. [Google Scholar] [CrossRef] [PubMed]
- Cornet, M.-C.; Wu, Y.W.; Forquer, H.; Avalos, L.A.; Sriram, A.; Scheffler, A.W.; Newman, T.B.; Kuzniewicz, M.W. Maternal Treatment with Selective Serotonin Reuptake Inhibitors during Pregnancy and Delayed Neonatal Adaptation: A Population-Based Cohort Study. Arch. Dis. Child. Fetal Neonatal Ed. 2024, 109, 294–300. [Google Scholar] [CrossRef]
- Lebin, L.G.; Novick, A.M. Selective Serotonin Reuptake Inhibitors (SSRIs) in Pregnancy: An Updated Review on Risks to Mother, Fetus, and Child. Curr. Psychiatry Rep. 2022, 24, 687–695. [Google Scholar] [CrossRef] [PubMed]
- Wisner, K.L.; Bogen, D.L.; Sit, D.; McShea, M.; Hughes, C.; Rizzo, D.; Confer, A.; Luther, J.; Eng, H.; Wisniewski, S.W. Does Fetal Exposure to SSRIs or Maternal Depression Impact Infant Growth? Am. J. Psychiatry 2013, 170, 485–493. [Google Scholar] [CrossRef] [PubMed]
- Bluett-Duncan, M.; Kishore, M.T.; Patil, D.M.; Satyanarayana, V.A.; Sharp, H. A Systematic Review of the Association between Perinatal Depression and Cognitive Development in Infancy in Low and Middle-Income Countries. PLoS ONE 2021, 16, e0253790. [Google Scholar] [CrossRef] [PubMed]
- van der Veere, C.N.; de Vries, N.K.S.; van Braeckel, K.N.J.A.; Bos, A.F. Intra-Uterine Exposure to Selective Serotonin Reuptake Inhibitors (SSRIs), Maternal Psychopathology, and Neurodevelopment at Age 2.5years—Results from the Prospective Cohort SMOK Study. Early Hum. Dev. 2020, 147, 105075. [Google Scholar] [CrossRef] [PubMed]
- Handal, M.; Skurtveit, S.; Furu, K.; Hernandez-Diaz, S.; Skovlund, E.; Nystad, W.; Selmer, R. Motor Development in Children Prenatally Exposed to Selective Serotonin Reuptake Inhibitors: A Large Population-based Pregnancy Cohort Study. BJOG 2016, 123, 1908–1917. [Google Scholar] [CrossRef]
- Bruno, C.; Cesta, C.E.; Hjellvik, V.; Ulrichsen, S.P.; Bjørk, M.-H.; Esen, B.Ö.; Gillies, M.B.; Gissler, M.; Havard, A.; Karlstad, Ø.; et al. Antipsychotic Use during Pregnancy and Risk of Specific Neurodevelopmental Disorders and Learning Difficulties in Children: A Multinational Cohort Study. eClinicalMedicine 2024, 70, 102531. [Google Scholar] [CrossRef] [PubMed]
- Yonkers, K.A.; Wisner, K.L.; Stewart, D.E.; Oberlander, T.F.; Dell, D.L.; Stotland, N.; Ramin, S.; Chaudron, L.; Lockwood, C. The Management of Depression during Pregnancy: A Report from the American Psychiatric Association and the American College of Obstetricians and Gynecologists. Gen. Hosp. Psychiatry 2009, 31, 403–413. [Google Scholar] [CrossRef] [PubMed]
- Mughal, S.; Azhar, Y.; Siddiqui, W. Postpartum depression. In StatPearls [Internet]; StatPearls Publishing: Treasure Island, FL, USA, 2018. [Google Scholar]
- Karrouri, R.; Hammani, Z.; Benjelloun, R.; Otheman, Y. Major Depressive Disorder: Validated Treatments and Future Challenges. World J. Clin. Cases 2021, 9, 9350–9367. [Google Scholar] [CrossRef]
- Chang, Q.; Ma, X.-Y.; Xu, X.-R.; Su, H.; Wu, Q.-J.; Zhao, Y.-H. Antidepressant Use in Depressed Women During Pregnancy and the Risk of Preterm Birth: A Systematic Review and Meta-Analysis of 23 Cohort Studies. Front. Pharmacol. 2020, 11, 659. [Google Scholar] [CrossRef] [PubMed]
- Amit, G.; Yanover, C.; Bivas-Benita, M.; Girshovitz, I.; Helbitz, T.; Sudry, T.; Bar, V.; Tang, A.S.; Le, B.L.; Roger, J.; et al. Antidepressant Use during Pregnancy and the Risk of Preterm Birth—A Cohort Study. npj Women’s Health 2024, 2, 5. [Google Scholar] [CrossRef]
- Schoretsanitis, G.; Spigset, O.; Stingl, J.C.; Deligiannidis, K.M.; Paulzen, M.; Westin, A.A. The Impact of Pregnancy on the Pharmacokinetics of Antidepressants: A Systematic Critical Review and Meta-Analysis. Expert. Opin. Drug Metab. Toxicol. 2020, 16, 431–440. [Google Scholar] [CrossRef]
- Cochran, G.T.; Hruschak, V.; Abdullah, W.; Krans, E.; Douaihy, A.B.; Bobby, S.; Fusco, R.; Tarter, R. Optimizing Pregnancy Treatment Interventions for Moms (OPTI-Mom): A Pilot Study. J. Addict. Med. 2018, 12, 72–79. [Google Scholar] [CrossRef] [PubMed]
- Charron, E.; White, A.; Carlston, K.; Abdullah, W.; Baylis, J.D.; Pierce, S.; Businelle, M.S.; Gordon, A.J.; Krans, E.E.; Smid, M.C.; et al. Prospective Acceptability of Digital Phenotyping among Pregnant and Parenting People with Opioid Use Disorder: A Multisite Qualitative Study. Front. Psychiatry 2023, 14, 1137071. [Google Scholar] [CrossRef] [PubMed]
- Pariente, G.; Leibson, T.; Carls, A.; Adams-Webber, T.; Ito, S.; Koren, G. Pregnancy-Associated Changes in Pharmacokinetics: A Systematic Review. PLoS Med. 2016, 13, e1002160. [Google Scholar] [CrossRef]
- Feghali, M.; Venkataramanan, R.; Caritis, S. Pharmacokinetics of Drugs in Pregnancy. Semin. Perinatol. 2015, 39, 512–519. [Google Scholar] [CrossRef] [PubMed]
- Westin, A.A.; Brekke, M.; Molden, E.; Skogvoll, E.; Castberg, I.; Spigset, O. Treatment with Antipsychotics in Pregnancy: Changes in Drug Disposition. Clin. Pharmacol. Ther. 2018, 103, 477–484. [Google Scholar] [CrossRef]
- Westin, A.A.; Brekke, M.; Molden, E.; Skogvoll, E.; Aadal, M.; Spigset, O. Changes in Drug Disposition of Lithium during Pregnancy: A Retrospective Observational Study of Patient Data from Two Routine Therapeutic Drug Monitoring Services in Norway. BMJ Open 2017, 7, e015738. [Google Scholar] [CrossRef]
- Gerlach, A.T.; Saliba, L. Practical Pharmacokinetics and Pharmacodynamics. In Principles of Adult Surgical Critical Care; Springer International Publishing: Cham, Switzerland, 2016; pp. 473–482. [Google Scholar]
- Mittal, A.; Ghai, R.; Srivastava, A.; Ghosh, D.P.; Nagarajan, K. Pharmacokinetics and Pharmacodynamics: Fundamentals and Role(s) in Drug Discovery and Development. In Recent Advances in Pharmaceutical Innovation and Research; Springer Nature: Singapore, 2023; pp. 357–393. [Google Scholar]
- Tyson, R.J.; Park, C.C.; Powell, J.R.; Patterson, J.H.; Weiner, D.; Watkins, P.B.; Gonzalez, D. Precision Dosing Priority Criteria: Drug, Disease, and Patient Population Variables. Front. Pharmacol. 2020, 11, 420. [Google Scholar] [CrossRef]
- Moreira, F.d.L.; Benzi, J.R.d.L.; Pinto, L.; Thomaz, M.d.L.; Duarte, G.; Lanchote, V.L. Optimizing Therapeutic Drug Monitoring in Pregnant Women: A Critical Literature Review. Ther. Drug Monit. 2023, 45, 159–172. [Google Scholar] [CrossRef] [PubMed]
- Matsui, D.M. Therapeutic Drug Monitoring in Pregnancy. Ther. Drug Monit. 2012, 34, 507–511. [Google Scholar] [CrossRef] [PubMed]
- Kacirova, I.; Grundmann, M. Importance of TDM during Pregnancy and Breastfeeding. Clin. Ther. 2017, 39, e92–e93. [Google Scholar] [CrossRef]
- Kang, J.-S.; Lee, M.-H. Overview of Therapeutic Drug Monitoring. Korean J. Intern. Med. 2009, 24, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Liang, W.S.; Beaulieu-Jones, B.; Smalley, S.; Snyder, M.; Goetz, L.H.; Schork, N.J. Emerging Therapeutic Drug Monitoring Technologies: Considerations and Opportunities in Precision Medicine. Front. Pharmacol. 2024, 15, 1348112. [Google Scholar] [CrossRef] [PubMed]
- Wang, Q.; Li, S.; Chen, J.; Yang, L.; Qiu, Y.; Du, Q.; Wang, C.; Teng, M.; Wang, T.; Dong, Y. A Novel Strategy for Therapeutic Drug Monitoring: Application of Biosensors to Quantify Antimicrobials in Biological Matrices. J. Antimicrob. Chemother. 2023, 78, 2612–2629. [Google Scholar] [CrossRef]
- Tovar-Lopez, F.J. Recent Progress in Micro- and Nanotechnology-Enabled Sensors for Biomedical and Environmental Challenges. Sensors 2023, 23, 5406. [Google Scholar] [CrossRef]
- Meneghello, A.; Tartaggia, S.; Alvau, M.D.; Polo, F.; Toffoli, G. Biosensing Technologies for Therapeutic Drug Monitoring. Curr. Med. Chem. 2018, 25, 4354–4377. [Google Scholar] [CrossRef] [PubMed]
- Sanavio, B.; Krol, S. On the Slow Diffusion of Point-of-Care Systems in Therapeutic Drug Monitoring. Front. Bioeng. Biotechnol. 2015, 3, 20. [Google Scholar] [CrossRef]
- Eadie, M.J.; Lander, C.M.; Tyrer, J.H. Plasma Drug Level Monitoring in Pregnancy. Clin. Pharmacokinet. 1977, 2, 427–436. [Google Scholar] [CrossRef]
- Coppola, P.; Butler, A.; Cole, S.; Kerwash, E. Total and Free Blood and Plasma Concentration Changes in Pregnancy for Medicines Highly Bound to Plasma Proteins: Application of Physiologically Based Pharmacokinetic Modelling to Understand the Impact on Efficacy. Pharmaceutics 2023, 15, 2455. [Google Scholar] [CrossRef] [PubMed]
- Bian, S.; Zhu, B.; Rong, G.; Sawan, M. Towards Wearable and Implantable Continuous Drug Monitoring: A Review. J. Pharm. Anal. 2021, 11, 1–14. [Google Scholar] [CrossRef] [PubMed]
- Janghorban, M.; Aradanas, I.; Kazemi, S.; Ngaju, P.; Pandey, R. Recent Advances, Opportunities, and Challenges in Developing Nucleic Acid Integrated Wearable Biosensors for Expanding the Capabilities of Wearable Technologies in Health Monitoring. Biosensors 2022, 12, 986. [Google Scholar] [CrossRef] [PubMed]
- Bhatia, D.; Paul, S.; Acharjee, T.; Ramachairy, S.S. Biosensors and Their Widespread Impact on Human Health. Sens. Int. 2024, 5, 100257. [Google Scholar] [CrossRef]
- Coppola, P.; Kerwash, E.; Nooney, J.; Omran, A.; Cole, S. Pharmacokinetic Data in Pregnancy: A Review of Available Literature Data and Important Considerations in Collecting Clinical Data. Front. Med. 2022, 9, 940644. [Google Scholar] [CrossRef] [PubMed]
- Sharma, S.; Tharani, L. Photonics for AI and AI for Photonics: Material and Characteristics Integration. In Fiber Optics—Technology and Applications; IntechOpen: London, UK, 2021. [Google Scholar]
- Oprescu, A.M.; Miro-Amarante, G.; Garcia-Diaz, L.; Beltran, L.M.; Rey, V.E.; Romero-Ternero, M. Artificial Intelligence in Pregnancy: A Scoping Review. IEEE Access 2020, 8, 181450–181484. [Google Scholar] [CrossRef]
- Saylam, B.; İncel, Ö.D. Quantifying Digital Biomarkers for Well-Being: Stress, Anxiety, Positive and Negative Affect via Wearable Devices and Their Time-Based Predictions. Sensors 2023, 23, 8987. [Google Scholar] [CrossRef]
- Krizea, M.; Gialelis, J.; Protopsaltis, G.; Mountzouris, C.; Theodorou, G. Empowering People with a User-Friendly Wearable Platform for Unobtrusive Monitoring of Vital Physiological Parameters. Sensors 2022, 22, 5226. [Google Scholar] [CrossRef] [PubMed]
- Shajari, S.; Kuruvinashetti, K.; Komeili, A.; Sundararaj, U. The Emergence of AI-Based Wearable Sensors for Digital Health Technology: A Review. Sensors 2023, 23, 9498. [Google Scholar] [CrossRef] [PubMed]
- Alim, A.; Imtiaz, M.H. Wearable Sensors for the Monitoring of Maternal Health—A Systematic Review. Sensors 2023, 23, 2411. [Google Scholar] [CrossRef]
- Li, J.; Silvera-Tawil, D.; Varnfield, M.; Hussain, M.S.; Math, V. Users’ Perceptions Toward MHealth Technologies for Health and Well-Being Monitoring in Pregnancy Care: Qualitative Interview Study. JMIR Form. Res. 2021, 5, e28628. [Google Scholar] [CrossRef]
- Le Merdy, M.; Szeto, K.X.; Perrier, J.; Bolger, M.B.; Lukacova, V. PBPK Modeling Approach to Predict the Behavior of Drugs Cleared by Metabolism in Pregnant Subjects and Fetuses. Pharmaceutics 2024, 16, 96. [Google Scholar] [CrossRef]
- Alnezary, F.S.; Almutairi, M.S.; Gonzales-Luna, A.J.; Thabit, A.K. The Significance of Bayesian Pharmacokinetics in Dosing for Critically Ill Patients: A Primer for Clinicians Using Vancomycin as an Example. Antibiotics 2023, 12, 1441. [Google Scholar] [CrossRef]
- Marques, L.; Costa, B.; Pereira, M.; Silva, A.; Santos, J.; Saldanha, L.; Silva, I.; Magalhães, P.; Schmidt, S.; Vale, N. Advancing Precision Medicine: A Review of Innovative In Silico Approaches for Drug Development, Clinical Pharmacology and Personalized Healthcare. Pharmaceutics 2024, 16, 332. [Google Scholar] [CrossRef]
- Yue, M.; Kus, L.; Katta, S.; Su, I.; Li, L.; Haas, D.M.; Quinney, S.K. Pharmacokinetics of Antidepressants in Pregnancy. J. Clin. Pharmacol. 2023, 63, S137–S158. [Google Scholar] [CrossRef]
- George, B.; Lumen, A.; Nguyen, C.; Wesley, B.; Wang, J.; Beitz, J.; Crentsil, V. Application of Physiologically Based Pharmacokinetic Modeling for Sertraline Dosing Recommendations in Pregnancy. NPJ Syst. Biol. Appl. 2020, 6, 36. [Google Scholar] [CrossRef] [PubMed]
- Alenezi, M.; Badhan, R.K.S. Precision Dosing of Venlafaxine during Pregnancy: A Pharmacokinetics Modelling Approach. J. Pharm. Pharmacol. 2024, 76, 122–137. [Google Scholar] [CrossRef] [PubMed]
- Besag, F.M.C.; Vasey, M.J.; Sharma, A.N.; Lam, I.C.H. Efficacy and Safety of Lamotrigine in the Treatment of Bipolar Disorder across the Lifespan: A Systematic Review. Ther. Adv. Psychopharmacol. 2021, 11, 204512532110458. [Google Scholar] [CrossRef] [PubMed]
- Polepally, A.R.; Pennell, P.B.; Brundage, R.C.; Stowe, Z.N.; Newport, D.J.; Viguera, A.C.; Ritchie, J.C.; Birnbaum, A.K. Model-based Lamotrigine Clearance Changes during Pregnancy: Clinical Implication. Ann. Clin. Transl. Neurol. 2014, 1, 99–106. [Google Scholar] [CrossRef]
- Berezowska, M.; Coppola, P.; Pilla Reddy, V.; Sharma, P. Physiologically Based Pharmacokinetic Modelling of UGT Substrate Drugs Lamotrigine and Raltegravir during Pregnancy. Future Pharmacol. 2024, 4, 317–335. [Google Scholar] [CrossRef]
- Silva, L.L.; Silvola, R.M.; Haas, D.M.; Quinney, S.K. Physiologically Based Pharmacokinetic Modelling in Pregnancy: Model Reproducibility and External Validation. Br. J. Clin. Pharmacol. 2022, 88, 1441–1451. [Google Scholar] [CrossRef]
- Zheng, L.; Yang, H.; Dallmann, A.; Jiang, X.; Wang, L.; Hu, W. Physiologically Based Pharmacokinetic Modeling in Pregnant Women Suggests Minor Decrease in Maternal Exposure to Olanzapine. Front. Pharmacol. 2022, 12, 793346. [Google Scholar] [CrossRef]
- Mahdy, W.Y.B.; Yamamoto, K.; Ito, T.; Fujiwara, N.; Fujioka, K.; Horai, T.; Otsuka, I.; Imafuku, H.; Omura, T.; Iijima, K.; et al. Physiologically-based Pharmacokinetic Model to Investigate the Effect of Pregnancy on Risperidone and Paliperidone Pharmacokinetics: Application to a Pregnant Woman and Her Neonate. Clin. Transl. Sci. 2023, 16, 618–630. [Google Scholar] [CrossRef]
- Leutritz, A.L.; van Braam, L.; Preis, K.; Gehrmann, A.; Scherf-Clavel, M.; Fiedler, K.; Unterecker, S.; Kittel-Schneider, S. Psychotropic Medication in Pregnancy and Lactation and Early Development of Exposed Children. Br. J. Clin. Pharmacol. 2023, 89, 737–750. [Google Scholar] [CrossRef] [PubMed]
- Yamamoto, K.; Fukushima, S.; Mishima, Y.; Hashimoto, M.; Yamakawa, K.; Fujioka, K.; Iijima, K.; Yano, I. Pharmacokinetic Assessment of Alprazolam-Induced Neonatal Abstinence Syndrome Using Physiologically Based Pharmacokinetic Model. Drug Metab. Pharmacokinet. 2019, 34, 400–402. [Google Scholar] [CrossRef] [PubMed]
- Meng, L.-C.; Lin, C.-W.; Lin, Y.-C.; Huang, S.-T.; Chen, Y.-Y.; Shang, C.-Y.; Wu, C.-Y.; Chen, L.-K.; Chan, K.A.; Hsiao, F.-Y. Association between Maternal Benzodiazepine or Z-Hypnotic Use in Early Pregnancy and the Risk of Stillbirth, Preterm Birth, and Small for Gestational Age: A Nationwide, Population-Based Cohort Study in Taiwan. Lancet Psychiatry 2023, 10, 499–508. [Google Scholar] [CrossRef]
- Munger Clary, H.M. Caution: Benzodiazepines in Pregnancy and Risk of Adverse Perinatal Outcomes. Epilepsy Curr. 2024, 24, 105–107. [Google Scholar] [CrossRef]
- Noh, Y.; Lee, H.; Choi, A.; Kwon, J.S.; Choe, S.-A.; Chae, J.; Kim, D.-S.; Shin, J.-Y. First-Trimester Exposure to Benzodiazepines and Risk of Congenital Malformations in Offspring: A Population-Based Cohort Study in South Korea. PLoS Med. 2022, 19, e1003945. [Google Scholar] [CrossRef]
- Robiyanto, R.; Schuiling-Veninga, C.C.M.; Bos, J.H.J.; Hak, E.; van Puijenbroek, E.P. Exposure to Psychotropic Drugs before and during Pregnancy: What Has Changed over the Last Two Decades? Arch. Womens Ment. Health 2023, 26, 39–48. [Google Scholar] [CrossRef]
- Hanley, G.E.; Mintzes, B. Patterns of Psychotropic Medicine Use in Pregnancy in the United States from 2006 to 2011 among Women with Private Insurance. BMC Pregnancy Childbirth 2014, 14, 242. [Google Scholar] [CrossRef]
- Kan, A.C.O.; Chan, J.K.N.; Wong, C.S.M.; Chen, E.Y.H.; Chang, W.C. Psychotropic Drug Utilization Patterns in Pregnant Women with Bipolar Disorder: A 16-Year Population-Based Cohort Study. Eur. Neuropsychopharmacol. 2022, 57, 75–85. [Google Scholar] [CrossRef] [PubMed]
- Huybrechts, K.F.; Bateman, B.T.; Hernández-Díaz, S. Use of Real-world Evidence from Healthcare Utilization Data to Evaluate Drug Safety during Pregnancy. Pharmacoepidemiol. Drug Saf. 2019, 28, 906–922. [Google Scholar] [CrossRef]
- Stevenson, F.; Hamilton, S.; Pinfold, V.; Walker, C.; Dare, C.R.J.; Kaur, H.; Lambley, R.; Szymczynska, P.; Nicolls, V.; Petersen, I. Decisions about the Use of Psychotropic Medication during Pregnancy: A Qualitative Study. BMJ Open 2016, 6, e010130. [Google Scholar] [CrossRef] [PubMed]
- Brumbaugh, J.E.; Ball, C.T.; Crook, J.E.; Stoppel, C.J.; Carey, W.A.; Bobo, W.V. Poor Neonatal Adaptation after Antidepressant Exposure during the Third Trimester in a Geographically Defined Cohort. Mayo Clin. Proc. Innov. Qual. Outcomes 2023, 7, 127–139. [Google Scholar] [CrossRef] [PubMed]
- Koren, G.; Moretti, M.; Kapur, B. Can Venlafaxine in Breast Milk Attenuate the Norepinephrine and Serotonin Reuptake Neonatal Withdrawal Syndrome? J. Obstet. Gynaecol. Can. 2006, 28, 299–301. [Google Scholar] [CrossRef] [PubMed]
- Finnegan, L.P.; Connaughton, J.F.; Kron, R.E.; Emich, J.P. Neonatal Abstinence Syndrome: Assessment and Management. Addict. Dis. 1975, 2, 141–158. [Google Scholar] [PubMed]
- Schiff, D.M.; Grossman, M.R. Beyond the Finnegan Scoring System: Novel Assessment and Diagnostic Techniques for the Opioid-Exposed Infant. Semin. Fetal Neonatal Med. 2019, 24, 115–120. [Google Scholar] [CrossRef] [PubMed]
- Mwenge, M.M.; Figge, C.J.; Metz, K.; Kane, J.C.; Kohrt, B.A.; Pedersen, G.A.; Sikazwe, I.; Van Wyk, S.S.; Mulemba, S.M.; Murray, L.K. Improving Inter-Rater Reliability of the Enhancing Assessment of Common Therapeutic Factors (ENACT) Measure through Training of Raters. J. Public Health Afr. 2022, 13, 12. [Google Scholar] [CrossRef] [PubMed]
- McElhatton, P.R. The Effects of Benzodiazepine Use during Pregnancy and Lactation. Reprod. Toxicol. 1994, 8, 461–475. [Google Scholar] [CrossRef]
- Nishimura, A.; Furugen, A.; Umazume, T.; Kitamura, S.; Soma, M.; Noshiro, K.; Takekuma, Y.; Sugawara, M.; Iseki, K.; Kobayashi, M. Benzodiazepine Concentrations in the Breast Milk and Plasma of Nursing Mothers: Estimation of Relative Infant Dose. Breastfeed. Med. 2021, 16, 424–431. [Google Scholar] [CrossRef]
- George, T.T.; Tripp, J. Alprazolam. In StatPearls [Internet]; StatPearls Publishing: Treasure Island, FL, USA, 2023. [Google Scholar]
- Parpinel, G.; Rosso, G.; Galante, A.; Germano, C.; Aragno, E.; Girlando, F.; Messina, A.; Laudani, M.E.; Rolfo, A.; Attini, R.; et al. Effect of Depressive Disorders and Their Pharmacological Treatment during Pregnancy on Maternal and Neonatal Outcome. J. Clin. Med. 2022, 11, 1486. [Google Scholar] [CrossRef] [PubMed]
- Tharp, M.A.; Silvola, R.M.; Marks, C.; Teal, E.; Quinney, S.K.; Haas, D.M. Does Lack of Exposure to Individual Antidepressants at Different Points during Pregnancy Associate with Reduced Risk of Adverse Newborn Outcomes? BMC Pregnancy Childbirth 2022, 22, 926. [Google Scholar] [CrossRef] [PubMed]
- Lupattelli, A.; Spigset, O.; Nordeng, H. Learning the Effects of Psychotropic Drugs during Pregnancy Using Real-World Safety Data: A Paradigm Shift toward Modern Pharmacovigilance. Int. J. Clin. Pharm. 2018, 40, 783–786. [Google Scholar] [CrossRef]
- Wang, Z.; Chan, A.Y.L.; Coghill, D.; Ip, P.; Lau, W.C.Y.; Simonoff, E.; Brauer, R.; Wei, L.; Wong, I.C.K.; Man, K.K.C. Association Between Prenatal Exposure to Antipsychotics and Attention-Deficit/Hyperactivity Disorder, Autism Spectrum Disorder, Preterm Birth, and Small for Gestational Age. JAMA Intern. Med. 2021, 181, 1332–1340. [Google Scholar] [CrossRef] [PubMed]
| Category | Description | Examples of Medications | Challenges and Considerations | Technologies and Innovations |
|---|---|---|---|---|
| Importance of TDM in Pregnancy | Monitoring is crucial due to physiological changes that affect drug pharmacokinetics. | Antiepileptics, Antidepressants, Antibiotics | Changes in drug disposition, treatment efficacy, toxicity. | Physiologically based pharmacokinetic models. |
| Medications of Interest | Drugs requiring careful dose adjustments due to individual variability and narrow therapeutic indices. | Phenytoin, Carbamazepine, Antipsychotics, Antidepressants. | Need for specific clinical studies in pregnant women, ethical challenges. | Nucleic acid assays, wearable technologies. |
| Monitoring Technologies | Advanced tools for accurately and real-time monitoring plasma drug levels. | CGM for glucose, Bio-nanochip devices, DBS. | Cost-effectiveness, accessibility, integration with healthcare systems. | Smartphone integration, genomic and proteomic microarrays. |
| Recent Innovations | Advances improving the sensitivity and usability of monitoring technologies. | Enzyme-based biosensors, wearable for L-Dopa. | Long-term stability, accuracy in real-world environments. | Smartphone-integrated sensors, paper-based lateral flow devices. |
| Clinical and Economic Impact | Evaluation of TDM effectiveness in improving maternal and fetal outcomes and reducing perinatal complications. | Anticonvulsant monitoring, gestational diabetes management. | Need for more research on cost-effectiveness and impact on clinical practice. | Development of automated, low-cost PoC systems. |
| Considerations in Breastfeeding | Importance of monitoring medication levels during breastfeeding to minimize infant exposure. | Antidepressants, Antipsychotics, Antibiotics. | Monitoring of mother and baby, dose adjustments. | Home DBS collection, real-time analysis. |
| Implementation Challenges | Barriers to widespread adoption of TDM, including complexity, costs, and clinical consensus. | Antiepileptics, Psychotropic medications. | Lack of clear cost-effectiveness data, limited funding. | PoC technologies, saliva monitoring with bio-nanochips. |
| Accessibility and Usability | Perspectives of pregnant women and healthcare providers on the accessibility and usability of mobile technologies for monitoring during pregnancy. | Monitoring apps, wearable devices. | Usability, additional workload for healthcare providers. | User feedback, technological acceptance studies. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Costa, B.; Vale, N. Advances in Psychotropic Treatment for Pregnant Women: Efficacy, Adverse Outcomes, and Therapeutic Monitoring. J. Clin. Med. 2024, 13, 4398. https://doi.org/10.3390/jcm13154398
Costa B, Vale N. Advances in Psychotropic Treatment for Pregnant Women: Efficacy, Adverse Outcomes, and Therapeutic Monitoring. Journal of Clinical Medicine. 2024; 13(15):4398. https://doi.org/10.3390/jcm13154398
Chicago/Turabian StyleCosta, Bárbara, and Nuno Vale. 2024. "Advances in Psychotropic Treatment for Pregnant Women: Efficacy, Adverse Outcomes, and Therapeutic Monitoring" Journal of Clinical Medicine 13, no. 15: 4398. https://doi.org/10.3390/jcm13154398
APA StyleCosta, B., & Vale, N. (2024). Advances in Psychotropic Treatment for Pregnant Women: Efficacy, Adverse Outcomes, and Therapeutic Monitoring. Journal of Clinical Medicine, 13(15), 4398. https://doi.org/10.3390/jcm13154398







