Impact of Molecular Profiling on Therapy Management in Breast Cancer
Abstract
:1. Introduction
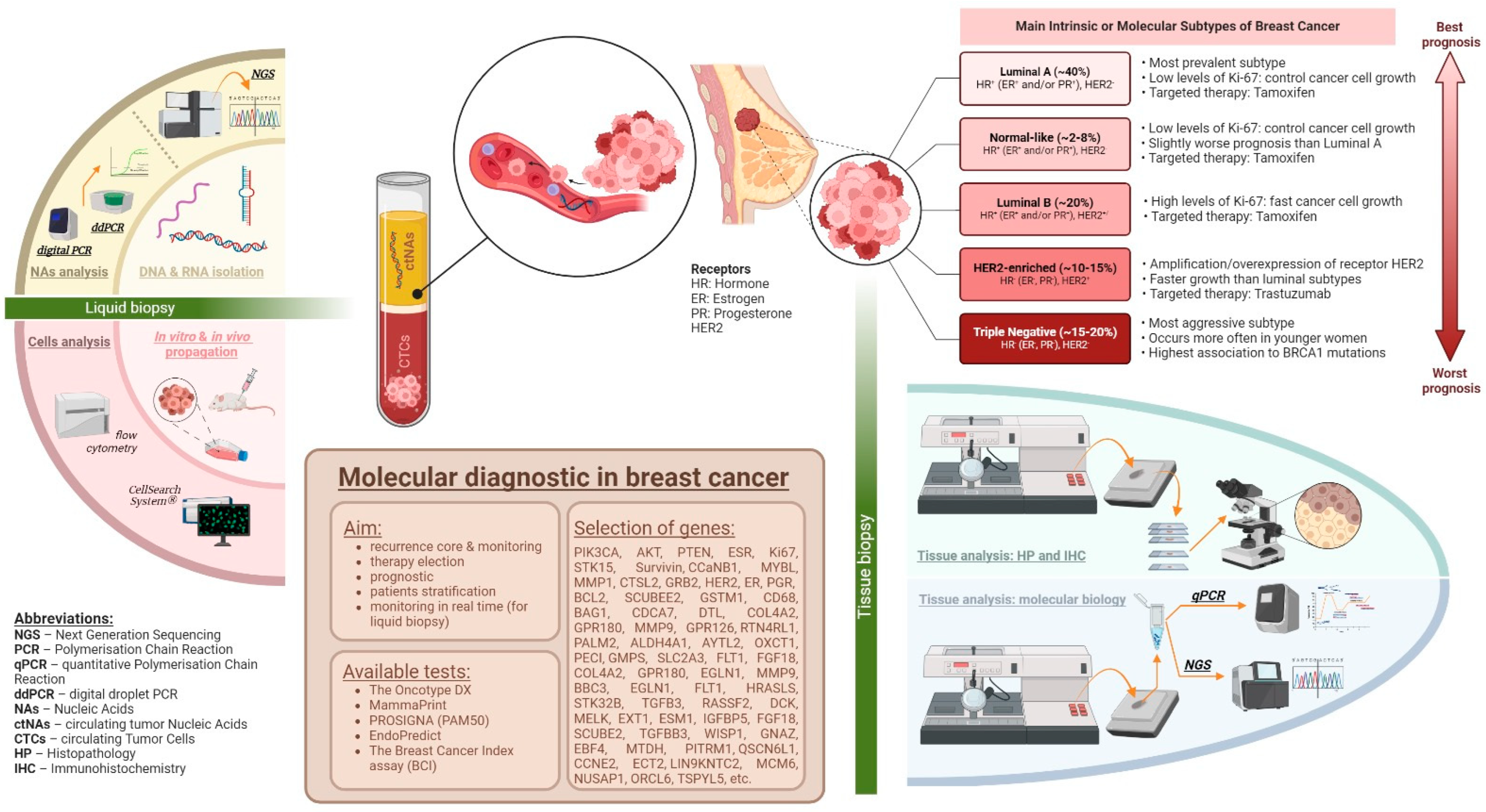
2. Current Approaches in Diagnosis and Therapeutic Management of Breast Cancer
2.1. Immunohistochemistry in Molecular Profiling of Breast Cancer and Therapy
Luminal-Like Breast Cancer Types
2.2. Gene Expression Profiling in Breast Cancer and Its Impact on Therapy Selection
2.3. Immune-Related Gene Signatures
2.4. The Synergy between Genomic Testing and Ki-67 in Personalized Breast Cancer Surveillance
2.5. Chemotherapy in Premenopausal Women: Evidence-Based Approach
2.6. Epithelial-to-Mesenchymal (EMT) Transition in Breast Carcinoma: Molecular Insights and Therapeutic Targets
2.7. Adaptive Molecular Subtyping in Breast Cancer: An Emerging Concept
3. Molecular Profiling of Breast Cancer and Its Impact on Therapy Management
3.1. Her2 Monoclonal Antibodies: Clinical Impact and Future Directions in Breast Cancer Treatment
3.2. Her2 Antibody–Drug Conjugates: Advances and Future Directions in Breast Cancer Therapy
3.3. Her2 Tyrosine Kinase Inhibitors in Breast Cancer Treatment
4. Liquid Biopsy as a Modern Tool for the Management of Breast Cancer
4.1. Circulating Tumor Cells (CTCs)
4.2. Circulating Tumor Nucleic Acids (ctNAs)
4.3. Tumor-Educated Platelets (TEPs)
5. Conclusions and Perspectives
Author Contributions
Funding
Conflicts of Interest
References
- Siegel, R.L.; Giaquinto, A.N.; Jemal, A. Cancer Statistics, 2024. CA Cancer J. Clin. 2024, 74, 12–49. [Google Scholar] [CrossRef]
- Siegel, R.L.; Miller, K.D.; Wagle, N.S.; Jemal, A. Cancer Statistics, 2023. CA Cancer J. Clin. 2023, 73, 17–48. [Google Scholar] [CrossRef] [PubMed]
- Feng, Y.; Spezia, M.; Huang, S.; Yuan, C.; Zeng, Z.; Zhang, L.; Ji, X.; Liu, W.; Huang, B.; Luo, W. Breast Cancer Development and Progression: Risk Factors, Cancer Stem Cells, Signaling Pathways, Genomics, and Molecular Pathogenesis. Genes Dis. 2018, 5, 77–106. [Google Scholar] [CrossRef] [PubMed]
- Tsang, J.Y.; Gary, M.T. Molecular Classification of Breast Cancer. Adv. Anat. Pathol. 2020, 27, 27–35. [Google Scholar] [CrossRef] [PubMed]
- Vuong, D.; Simpson, P.T.; Green, B.; Cummings, M.C.; Lakhani, S.R. Molecular Classification of Breast Cancer. Virchows Arch. 2014, 465, 1–14. [Google Scholar] [CrossRef] [PubMed]
- Acs, B.; Fredriksson, I.; Rönnlund, C.; Hagerling, C.; Ehinger, A.; Kovács, A.; Røge, R.; Bergh, J.; Hartman, J. Variability in Breast Cancer Biomarker Assessment and the Effect on Oncological Treatment Decisions: A Nationwide 5-Year Population-Based Study. Cancers 2021, 13, 1166. [Google Scholar] [CrossRef] [PubMed]
- Freedman, R.A.; Ko, N.Y.; Lederman, R.I.; Gagnon, H.; Fikre, T.; Gundersen, D.A.; Revette, A.C.; Odai-Afotey, A.; Kantor, O.; Hershman, D.L. Breast Cancer Knowledge and Understanding Treatment Rationales among Diverse Breast Cancer Survivors. Breast Cancer Res. Treat. 2022, 196, 623–633. [Google Scholar] [CrossRef]
- Untch, M.; Gerber, B.; Harbeck, N.; Jackisch, C.; Marschner, N.; Möbus, V.; Von Minckwitz, G.; Loibl, S.; Beckmann, M.W.; Blohmer, J.-U. 13th St. Gallen International Breast Cancer Conference 2013: Primary Therapy of Early Breast Cancer Evidence, Controversies, Consensus-Opinion of a German Team of Experts (Zurich 2013). Breast Care 2013, 8, 221–229. [Google Scholar] [CrossRef]
- Johnson, K.S.; Conant, E.F.; Soo, M.S. Molecular Subtypes of Breast Cancer: A Review for Breast Radiologists. J. Breast Imaging 2021, 3, 12–24. [Google Scholar] [CrossRef]
- Bayraktar, S.; Glück, S. Molecularly Targeted Therapies for Metastatic Triple-Negative Breast Cancer. Breast Cancer Res. Treat. 2013, 138, 21–35. [Google Scholar] [CrossRef]
- Tan, P.H.; Ellis, I.; Allison, K.; Brogi, E.; Fox, S.B.; Lakhani, S.; Lazar, A.J.; Morris, E.A.; Sahin, A.; Salgado, R. The 2019 WHO Classification of Tumours of the Breast. Histopathology 2020, 77, 181–185. [Google Scholar] [CrossRef]
- Dias, K.; Dvorkin-Gheva, A.; Hallett, R.M.; Wu, Y.; Hassell, J.; Pond, G.R.; Levine, M.; Whelan, T.; Bane, A.L. Claudin-Low Breast Cancer; Clinical & Pathological Characteristics. PLoS ONE 2017, 12, e0168669. [Google Scholar]
- Huang, Z.; Qin, Q.; Xia, L.; Lian, B.; Tan, Q.; Yu, Y.; Mo, Q. Significance of Oncotype DX 21-Gene Test and Expression of Long Non-Coding RNA MALAT1 in Early and Estrogen Receptor-Positive Breast Cancer Patients. Cancer Manag. Res. 2021, 13, 587–593. [Google Scholar] [CrossRef]
- Güler, E.N. Gene Expression Profiling in Breast Cancer and Its Effect on Therapy Selection in Early-Stage Breast Cancer. Eur. J. Breast Health 2017, 13, 168. [Google Scholar] [CrossRef] [PubMed]
- Kittaneh, M.; Montero, A.J.; Glück, S. Molecular Profiling for Breast Cancer: A Comprehensive Review. Biomark. Cancer 2013, 5, BIC-S9455. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Chen, H.; Koenig, J.; Wu, Y.; Bedrosian, I.; Arun, B.; Ding, Q.; Khazai, L.; Resetkova, E.; Huo, L. Discordance of Oncotype DX Scores in Synchronous Bilateral and Unilateral Multifocal Breast Cancers. Breast Cancer Res. Treat. 2024, 203, 73–83. [Google Scholar] [CrossRef]
- Tian, S.; Roepman, P.; Van’t Veer, L.J.; Bernards, R.; De Snoo, F.; Glas, A.M. Biological Functions of the Genes in the Mammaprint Breast Cancer Profile Reflect the Hallmarks of Cancer. Biomark. Insights 2010, 5, BMI-S6184. [Google Scholar] [CrossRef]
- Perou, C.M.; Parker, J.S.; Marron, J.S.; Nobel, A.; Bernard, P.S.; Ellis, M.; Mardis, E.; Nielsen, T.O.; Cheang, M. Gene Expression Profiles to Predict Breast Cancer Outcomes. International Patent Application WO 2009/158143 A1, 1 June 2009. Available online: https://patents.google.com/patent/WO2009158143A1/en (accessed on 23 April 2024).
- Prosigna Breast Cancer Prognostic Gene Signature Assay. Available online: https://www.breastcancer.org/screening-testing/prosigna-assay (accessed on 28 December 2023).
- Hequet, D.; Harrissart, G.; Krief, D.; Maumy, L.; Lerebours, F.; Menet, E.; Callens, C.; Rouzier, R. Prosigna Test in Breast Cancer: Real-Life Experience. Breast Cancer Res. Treat. 2021, 188, 141–147. [Google Scholar] [CrossRef]
- Kim, H.K.; Park, K.H.; Kim, Y.; Park, S.E.; Lee, H.S.; Lim, S.W.; Cho, J.H.; Kim, J.-Y.; Lee, J.E.; Ahn, J.S. Discordance of the PAM50 Intrinsic Subtypes Compared with Immunohistochemistry-Based Surrogate in Breast Cancer Patients: Potential Implication of Genomic Alterations of Discordance. Cancer Res. Treat. Off. J. Korean Cancer Assoc. 2019, 51, 737–747. [Google Scholar] [CrossRef]
- Soliman, H.; Wagner, S.; Flake, D.D.; Robson, M.; Schwartzberg, L.; Sharma, P.; Magliocco, A.; Kronenwett, R.; Lancaster, J.M.; Lanchbury, J.S. Evaluation of the 12-Gene Molecular Score and the 21-Gene Recurrence Score as Predictors of Response to Neo-Adjuvant Chemotherapy in Estrogen Receptor-Positive, HER2-Negative Breast Cancer. Ann. Surg. Oncol. 2020, 27, 765–771. [Google Scholar] [CrossRef]
- Sestak, I.; Martín, M.; Dubsky, P.; Kronenwett, R.; Rojo, F.; Cuzick, J.; Filipits, M.; Ruiz, A.; Gradishar, W.; Soliman, H. Prediction of Chemotherapy Benefit by EndoPredict in Patients with Breast Cancer Who Received Adjuvant Endocrine Therapy plus Chemotherapy or Endocrine Therapy Alone. Breast Cancer Res. Treat. 2019, 176, 377–386. [Google Scholar] [CrossRef]
- Jahn, S.W.; Bösl, A.; Tsybrovskyy, O.; Gruber-Rossipal, C.; Helfgott, R.; Fitzal, F.; Knauer, M.; Balic, M.; Jasarevic, Z.; Offner, F. Clinically High-Risk Breast Cancer Displays Markedly Discordant Molecular Risk Predictions between the MammaPrint and EndoPredict Tests. Br. J. Cancer 2020, 122, 1744–1746. [Google Scholar] [CrossRef] [PubMed]
- Habel, L.A.; Sakoda, L.C.; Achacoso, N.; Ma, X.-J.; Erlander, M.G.; Sgroi, D.C.; Fehrenbacher, L.; Greenberg, D.; Quesenberry, C.P. HOXB13: IL17BR and Molecular Grade Index and Risk of Breast Cancer Death among Patients with Lymph Node-Negative Invasive Disease. Breast Cancer Res. 2013, 15, R24. [Google Scholar] [CrossRef]
- Han, Y.; Wang, J.; Xu, B. Tumor Microenvironment Subtypes and Immune—Related Signatures for the Prognosis of Breast Cancer. BioMed Res. Int. 2021, 2021, 6650107. [Google Scholar] [CrossRef] [PubMed]
- Tan, W.; Liu, M.; Wang, L.; Guo, Y.; Wei, C.; Zhang, S.; Luo, C.; Liu, N. Novel Immune-Related Genes in the Tumor Microenvironment with Prognostic Value in Breast Cancer. BMC Cancer 2021, 21, 126. [Google Scholar] [CrossRef] [PubMed]
- Fernandez-Martinez, A.; Pascual, T.; Singh, B.; Nuciforo, P.; Rashid, N.U.; Ballman, K.V.; Campbell, J.D.; Hoadley, K.A.; Spears, P.A.; Pare, L. Prognostic and Predictive Value of Immune-Related Gene Expression Signatures vs Tumor-Infiltrating Lymphocytes in Early-Stage ERBB2/HER2-Positive Breast Cancer: A Correlative Analysis of the CALGB 40601 and PAMELA Trials. JAMA Oncol. 2023, 9, 490–499. [Google Scholar] [CrossRef]
- Sparano, J.A.; Gray, R.J.; Makower, D.F.; Pritchard, K.I.; Albain, K.S.; Hayes, D.F.; Geyer, C.E., Jr.; Dees, E.C.; Goetz, M.P.; Olson, J.A., Jr. Adjuvant Chemotherapy Guided by a 21-Gene Expression Assay in Breast Cancer. N. Engl. J. Med. 2018, 379, 111–121. [Google Scholar] [CrossRef]
- Cardoso, F.; van’t Veer, L.J.; Bogaerts, J.; Slaets, L.; Viale, G.; Delaloge, S.; Pierga, J.-Y.; Brain, E.; Causeret, S.; DeLorenzi, M. 70-Gene Signature as an Aid to Treatment Decisions in Early-Stage Breast Cancer. N. Engl. J. Med. 2016, 375, 717–729. [Google Scholar] [CrossRef]
- Kalinsky, K.; Barlow, W.E.; Gralow, J.R.; Meric-Bernstam, F.; Albain, K.S.; Hayes, D.F.; Lin, N.U.; Perez, E.A.; Goldstein, L.J.; Chia, S.K. 21-Gene Assay to Inform Chemotherapy Benefit in Node-Positive Breast Cancer. N. Engl. J. Med. 2021, 385, 2336–2347. [Google Scholar] [CrossRef]
- Smith, I.; Robertson, J.; Kilburn, L.; Wilcox, M.; Evans, A.; Holcombe, C.; Horgan, K.; Kirwan, C.; Mallon, E.; Sibbering, M. Long-Term Outcome and Prognostic Value of Ki67 after Perioperative Endocrine Therapy in Postmenopausal Women with Hormone-Sensitive Early Breast Cancer (POETIC): An Open-Label, Multicentre, Parallel-Group, Randomised, Phase 3 Trial. Lancet Oncol. 2020, 21, 1443–1454. [Google Scholar] [CrossRef]
- Harbeck, N.; Gluz, O.; Kuemmel, S.; Christgen, M.; Braun, M.; Aktas, B.; Luedtke-Heckenkamp, K.; Forstbauer, H.; Grischke, E.-M.; Schumacher, C. Abstract GS4-04: Endocrine Therapy Alone in Patients with Intermediate or High-Risk Luminal Early Breast Cancer (0–3 Lymph Nodes), Recurrence Score <26 and Ki67 Response after Preoperative Endocrine Therapy: Primary Outcome Results from the WSG-ADAPT HR+/HER2-Trial. Cancer Res. 2021, 81, GS4-04. [Google Scholar]
- Zhang, S.; Liu, Q.; Chang, M.; Pan, Y.; Yahaya, B.H.; Liu, Y.; Lin, J. Chemotherapy Impairs Ovarian Function through Excessive ROS-Induced Ferroptosis. Cell Death Dis. 2023, 14, 340. [Google Scholar] [CrossRef]
- Yildiz, S.; Bildik, G.; Benlioglu, C.; Turan, V.; Dilege, E.; Ozel, M.; Kim, S.; Oktem, O. Breast Cancer Treatment and Ovarian Function. Reprod. Biomed. Online 2023, 46, 313–331. [Google Scholar] [CrossRef]
- Lambertini, M.; Boni, L.; Michelotti, A.; Magnolfi, E.; Cogoni, A.A.; Mosconi, A.M.; Giordano, M.; Garrone, O.; Arpino, G.; Poggio, F. Long-Term Outcomes with Pharmacological Ovarian Suppression during Chemotherapy in Premenopausal Early Breast Cancer Patients. JNCI J. Natl. Cancer Inst. 2022, 114, 400–408. [Google Scholar] [CrossRef] [PubMed]
- Moore, H.C.; Unger, J.M.; Phillips, K.-A.; Boyle, F.; Hitre, E.; Moseley, A.; Porter, D.J.; Francis, P.A.; Goldstein, L.J.; Gomez, H.L. Final Analysis of the Prevention of Early Menopause Study (POEMS)/SWOG Intergroup S0230. JNCI J. Natl. Cancer Inst. 2019, 111, 210–213. [Google Scholar] [CrossRef]
- Leonard, R.; Adamson, D.; Bertelli, G.; Mansi, J.; Yellowlees, A.; Dunlop, J.; Thomas, G.; Coleman, R.; Anderson, R. GnRH Agonist for Protection against Ovarian Toxicity during Chemotherapy for Early Breast Cancer: The Anglo Celtic Group OPTION Trial. Ann. Oncol. 2017, 28, 1811–1816. [Google Scholar] [CrossRef]
- Pagani, O.; Walley, B.A.; Fleming, G.F.; Colleoni, M.; Láng, I.; Gomez, H.L.; Tondini, C.; Burstein, H.J.; Goetz, M.P.; Ciruelos, E.M. Adjuvant Exemestane with Ovarian Suppression in Premenopausal Breast Cancer: Long-Term Follow-up of the Combined TEXT and SOFT Trials. J. Clin. Oncol. 2023, 41, 1376–1382. [Google Scholar] [CrossRef]
- Dolmans, M.-M.; Von Wolff, M.; Poirot, C.; Diaz-Garcia, C.; Cacciottola, L.; Boissel, N.; Liebenthron, J.; Pellicer, A.; Donnez, J.; Andersen, C.Y. Transplantation of Cryopreserved Ovarian Tissue in a Series of 285 Women: A Review of Five Leading European Centers. Fertil. Steril. 2021, 115, 1102–1115. [Google Scholar] [CrossRef] [PubMed]
- Celià-Terrassa, T.; Kang, Y. How Important Is EMT for Cancer Metastasis? PLoS Biol. 2024, 22, e3002487. [Google Scholar] [CrossRef]
- Soini, Y.; Tuhkanen, H.; Sironen, R.; Virtanen, I.; Kataja, V.; Auvinen, P.; Mannermaa, A.; Kosma, V.-M. Transcription Factors Zeb1, Twist and Snai1 in Breast Carcinoma. BMC Cancer 2011, 11, 73. [Google Scholar] [CrossRef]
- Gottumukkala, S.B.; Ganesan, T.S.; Palanisamy, A. Comprehensive Molecular Interaction Map of TGFβ Induced Epithelial to Mesenchymal Transition in Breast Cancer. npj Syst. Biol. Appl. 2024, 10, 53. [Google Scholar] [CrossRef]
- Zhao, M.; Ang, L.; Huang, J.; Wang, J. MicroRNAs Regulate the Epithelial–Mesenchymal Transition and Influence Breast Cancer Invasion and Metastasis. Tumor Biol. 2017, 39, 1010428317691682. [Google Scholar] [CrossRef] [PubMed]
- Hernández-Oliveras, A.; Zarain-Herzberg, Á. Expression and Associated Epigenetic Mechanisms of the Ca2+-Signaling Genes in Breast Cancer Subtypes and Epithelial-to-Mesenchymal Transition. J. Cell Commun. Signal. 2022, 16, 461–474. [Google Scholar] [CrossRef]
- Datta, A.; Deng, S.; Gopal, V.; Yap, K.C.-H.; Halim, C.E.; Lye, M.L.; Ong, M.S.; Tan, T.Z.; Sethi, G.; Hooi, S.C. Cytoskeletal Dynamics in Epithelial-Mesenchymal Transition: Insights into Therapeutic Targets for Cancer Metastasis. Cancers 2021, 13, 1882. [Google Scholar] [CrossRef]
- Tolaney, S.M.; Tan, S.; Guo, H.; Barry, W.; Van Allen, E.; Wagle, N.; Brock, J.; Larrabee, K.; Paweletz, C.; Ivanova, E. Phase II Study of Tivantinib (ARQ 197) in Patients with Metastatic Triple-Negative Breast Cancer. Investig. New Drugs 2015, 33, 1108–1114. [Google Scholar] [CrossRef]
- Chung, A.W.; Anand, K.; Anselme, A.C.; Chan, A.A.; Gupta, N.; Venta, L.A.; Schwartz, M.R.; Qian, W.; Xu, Y.; Zhang, L. A Phase 1/2 Clinical Trial of the Nitric Oxide Synthase Inhibitor L-NMMA and Taxane for Treating Chemoresistant Triple-Negative Breast Cancer. Sci. Transl. Med. 2021, 13, eabj5070. [Google Scholar] [CrossRef] [PubMed]
- Han, D.; Wu, G.; Chang, C.; Zhu, F.; Xiao, Y.; Li, Q.; Zhang, T.; Zhang, L. Disulfiram Inhibits TGF-β-Induced Epithelial-Mesenchymal Transition and Stem-like Features in Breast Cancer via ERK/NF-κB/Snail Pathway. Oncotarget 2015, 6, 40907. [Google Scholar] [CrossRef] [PubMed]
- Robinson, T.; Pai, M.; Liu, J.; Vizeacoumar, F.; Sun, T.; Egan, S.; Datti, A.; Huang, J.; Zacksenhaus, E. High-Throughput Screen Identifies Disulfiram as a Potential Therapeutic for Triple-Negative Breast Cancer Cells: Interaction with IQ Motif-Containing Factors. Cell Cycle 2013, 12, 3013–3024. [Google Scholar] [CrossRef]
- Denkert, C.; Rachakonda, K.; Filipits, M.; Weber, K.; Marmé, F.; Untch, M.; Witkiewicz, A.K.; Im, S.-A.; DeMichele, A.; Pehl, A. Relationship of Adaptive Subtyping and Tumour Heterogeneity of Treatment Response to Neoadjuvant Therapy in Hormone Receptor–Positive HER2-Negative Early Breast Cancer: PENELOPE-B. J. Clin. Oncol. 2024, 42, 566. [Google Scholar] [CrossRef]
- Zayas-Villanueva, O.A.; Campos-Acevedo, L.D.; Lugo-Trampe, J.d.J.; Hernández-Barajas, D.; González-Guerrero, J.F.; Noriega-Iriondo, M.F.; Ramírez-Sánchez, I.A.; Martínez-de-Villarreal, L.E. Analysis of the Pathogenic Variants of BRCA1 and BRCA2 Using Next-Generation Sequencing in Women with Familial Breast Cancer: A Case–Control Study. BMC Cancer 2019, 19, 722. [Google Scholar] [CrossRef]
- Targeted Therapy Approved for Breast Cancer. Available online: https://www.cancer.gov/about-cancer/treatment/types/targeted-therapies/approved-drug-list#targeted-therapy-approved-for-breast-cancer (accessed on 10 June 2023).
- Godet, I.; Gilkes, D.M. BRCA1 and BRCA2 Mutations and Treatment Strategies for Breast Cancer. Integr. Cancer Sci. Ther. 2017, 4, 1–17. [Google Scholar] [CrossRef] [PubMed]
- Robson, M.; Im, S.-A.; Senkus, E.; Xu, B.; Domchek, S.M.; Masuda, N.; Delaloge, S.; Li, W.; Tung, N.; Armstrong, A. Olaparib for Metastatic Breast Cancer in Patients with a Germline BRCA Mutation. N. Engl. J. Med. 2017, 377, 523–533. [Google Scholar] [CrossRef] [PubMed]
- Abraham, J.E.; Pinilla, K.; Dayimu, A.; Grybowicz, L.; Demiris, N.; Harvey, C.; Drewett, L.M.; Lucey, R.; Fulton, A.; Roberts, A.N. The PARTNER Trial of Neoadjuvant Olaparib in Triple-Negative Breast Cancer. Nature 2024, 629, 1142–1148. [Google Scholar] [CrossRef] [PubMed]
- Litton, J.K.; Rugo, H.S.; Ettl, J.; Hurvitz, S.A.; Gonçalves, A.; Lee, K.-H.; Fehrenbacher, L.; Yerushalmi, R.; Mina, L.A.; Martin, M. Talazoparib in Patients with Advanced Breast Cancer and a Germline BRCA Mutation. N. Engl. J. Med. 2018, 379, 753–763. [Google Scholar] [CrossRef]
- Shimada, K.; Lynce, F.; Geng, X.; Richardson, E.T.; Mainor, C.; Wei, M.; Collins, J.M.; Pohlmann, P.R.; Heeke, A.; Zheng, K.F. 885 Characterization of the Tumor Microenvironment in Advanced Breast Cancer Patients Treated with Talazoparib Followed by Combination of Talazoparib and Avelumab. J. Immunother. Cancer 2023, 11, 986. [Google Scholar]
- Guney Eskiler, G.; Ozman, Z.; Haciefendi, A.; Cansaran-Duman, D. Novel Combination Treatment of CDK 4/6 Inhibitors with PARP Inhibitors in Triple Negative Breast Cancer Cells. Naunyn-Schmiedeberg’s Arch. Pharmacol. 2023, 396, 1031–1041. [Google Scholar] [CrossRef]
- Calabrese, A.; von Arx, C.; Tafuti, A.; Pensabene, M.; De Laurentiis, M. Prevention, Diagnosis and Clinical Management of Hereditary Breast Cancer beyond BRCA1/2 Genes. Cancer Treat. Rev. 2024, 129, 102785. [Google Scholar] [CrossRef]
- Vinayak, S.; Tolaney, S.M.; Schwartzberg, L.; Mita, M.; McCann, G.; Tan, A.R.; Wahner-Hendrickson, A.E.; Forero, A.; Anders, C.; Wulf, G.M. Open-Label Clinical Trial of Niraparib Combined with Pembrolizumab for Treatment of Advanced or Metastatic Triple-Negative Breast Cancer. JAMA Oncol. 2019, 5, 1132–1140. [Google Scholar] [CrossRef]
- Kristeleit, R.; Leary, A.; Oaknin, A.; Redondo, A.; George, A.; Chui, S.; Seiller, A.; Liste-Hermoso, M.; Willis, J.; Shemesh, C.S. PARP Inhibition with Rucaparib Alone Followed by Combination with Atezolizumab: Phase Ib COUPLET Clinical Study in Advanced Gynaecological and Triple-Negative Breast Cancers. Br. J. Cancer 2024, 1–12. [Google Scholar] [CrossRef]
- Patsouris, A.; Diop, K.; Tredan, O.; Nenciu, D.; Gonçalves, A.; Arnedos, M.; Sablin, M.-P.; Jézéquel, P.; Jimenez, M.; Droin, N. Rucaparib in Patients Presenting a Metastatic Breast Cancer with Homologous Recombination Deficiency, without Germline BRCA1/2 Mutation. Eur. J. Cancer 2021, 159, 283–295. [Google Scholar] [CrossRef]
- Rodler, E.; Sharma, P.; Barlow, W.E.; Gralow, J.R.; Puhalla, S.L.; Anders, C.K.; Goldstein, L.; Tripathy, D.; Brown-Glaberman, U.A.; Huynh, T.-T. Cisplatin with Veliparib or Placebo in Metastatic Triple-Negative Breast Cancer and BRCA Mutation-Associated Breast Cancer (S1416): A Randomised, Double-Blind, Placebo-Controlled, Phase 2 Trial. Lancet Oncol. 2023, 24, 162–174. [Google Scholar] [CrossRef] [PubMed]
- Pouptsis, A.; Swafe, L.; Patwardhan, M.; Stavraka, C. Surgical and Systemic Treatment of Hereditary Breast Cancer: A Mini-Review with a Focus on BRCA1 and BRCA2 Mutations. Front. Oncol. 2020, 10, 553080. [Google Scholar] [CrossRef] [PubMed]
- Martínez-Sáez, O.; Chic, N.; Pascual, T.; Adamo, B.; Vidal, M.; González-Farré, B.; Sanfeliu, E.; Schettini, F.; Conte, B.; Brasó-Maristany, F. Frequency and Spectrum of PIK3CA Somatic Mutations in Breast Cancer. Breast Cancer Res. 2020, 22, 45. [Google Scholar] [CrossRef]
- André, F.; Ciruelos, E.; Rubovszky, G.; Campone, M.; Loibl, S.; Rugo, H.S.; Iwata, H.; Conte, P.; Mayer, I.A.; Kaufman, B. Alpelisib for PIK3CA-Mutated, Hormone Receptor–Positive Advanced Breast Cancer. N. Engl. J. Med. 2019, 380, 1929–1940. [Google Scholar] [CrossRef]
- Tolaney, S.M.; Toi, M.; Neven, P.; Sohn, J.; Grischke, E.-M.; Llombart-Cussac, A.; Soliman, H.; Wang, H.; Wijayawardana, S.; Jansen, V.M. Clinical Significance of PIK3CA and ESR1 Mutations in Circulating Tumor DNA: Analysis from the MONARCH 2 Study of Abemaciclib plus Fulvestrant. Clin. Cancer Res. 2022, 28, 1500–1506. [Google Scholar] [CrossRef]
- Yi, Z.; Rong, G.; Guan, Y.; Li, J.; Chang, L.; Li, H.; Liu, B.; Wang, W.; Guan, X.; Ouyang, Q. Molecular Landscape and Efficacy of HER2-Targeted Therapy in Patients with HER2-Mutated Metastatic Breast Cancer. NPJ Breast Cancer 2020, 6, 59. [Google Scholar] [CrossRef] [PubMed]
- Cameron, D.; Piccart-Gebhart, M.J.; Gelber, R.D.; Procter, M.; Goldhirsch, A.; de Azambuja, E.; Castro, G.; Untch, M.; Smith, I.; Gianni, L. 11 Years’ Follow-up of Trastuzumab after Adjuvant Chemotherapy in HER2-Positive Early Breast Cancer: Final Analysis of the HERceptin Adjuvant (HERA) Trial. Lancet 2017, 389, 1195–1205. [Google Scholar] [CrossRef]
- Lin, N.U.; Kumthekar, P.; Sahebjam, S.; Ibrahim, N.; Fung, A.; Cheng, A.; Nicholas, A.; Sussell, J.; Pegram, M. Pertuzumab plus High-Dose Trastuzumab for HER2-Positive Breast Cancer with Brain Metastases: PATRICIA Final Efficacy Data. NPJ Breast Cancer 2023, 9, 94. [Google Scholar] [CrossRef]
- Ciruelos, E.; Villagrasa, P.; Pascual, T.; Oliveira, M.; Pernas, S.; Paré, L.; Escrivá-de-Romaní, S.; Manso, L.; Adamo, B.; Martínez, E. Palbociclib and Trastuzumab in HER2-Positive Advanced Breast Cancer: Results from the Phase II SOLTI-1303 PATRICIA Trial. Clin. Cancer Res. 2020, 26, 5820–5829. [Google Scholar] [CrossRef]
- Swain, S.M.; Baselga, J.; Kim, S.-B.; Ro, J.; Semiglazov, V.; Campone, M.; Ciruelos, E.; Ferrero, J.-M.; Schneeweiss, A.; Heeson, S. Pertuzumab, Trastuzumab, and Docetaxel in HER2-Positive Metastatic Breast Cancer. N. Engl. J. Med. 2015, 372, 724–734. [Google Scholar] [CrossRef]
- Swain, S.M.; Miles, D.; Kim, S.-B.; Im, Y.-H.; Im, S.-A.; Semiglazov, V.; Ciruelos, E.; Schneeweiss, A.; Loi, S.; Monturus, E. Pertuzumab, Trastuzumab, and Docetaxel for HER2-Positive Metastatic Breast Cancer (CLEOPATRA): End-of-Study Results from a Double-Blind, Randomised, Placebo-Controlled, Phase 3 Study. Lancet Oncol. 2020, 21, 519–530. [Google Scholar] [CrossRef]
- Rugo, H.S.; Im, S.-A.; Cardoso, F.; Cortés, J.; Curigliano, G.; Musolino, A.; Pegram, M.D.; Wright, G.S.; Saura, C.; Escrivá-de-Romaní, S. Efficacy of Margetuximab vs Trastuzumab in Patients with Pretreated ERBB2-Positive Advanced Breast Cancer: A Phase 3 Randomized Clinical Trial. JAMA Oncol. 2021, 7, 573–584. [Google Scholar] [CrossRef] [PubMed]
- Modi, S.; Saura, C.; Yamashita, T.; Park, Y.H.; Kim, S.-B.; Tamura, K.; Andre, F.; Iwata, H.; Ito, Y.; Tsurutani, J. Trastuzumab Deruxtecan in Previously Treated HER2-Positive Breast Cancer. N. Engl. J. Med. 2020, 382, 610–621. [Google Scholar] [CrossRef] [PubMed]
- Hurvitz, S.A.; Hegg, R.; Chung, W.-P.; Im, S.-A.; Jacot, W.; Ganju, V.; Chiu, J.W.Y.; Xu, B.; Hamilton, E.; Madhusudan, S. Trastuzumab Deruxtecan versus Trastuzumab Emtansine in Patients with HER2-Positive Metastatic Breast Cancer: Updated Results from DESTINY-Breast03, a Randomised, Open-Label, Phase 3 Trial. Lancet 2023, 401, 105–117. [Google Scholar] [CrossRef]
- Modi, S.; Jacot, W.; Yamashita, T.; Sohn, J.; Vidal, M.; Tokunaga, E.; Tsurutani, J.; Ueno, N.T.; Prat, A.; Chae, Y.S. Trastuzumab Deruxtecan in Previously Treated HER2-Low Advanced Breast Cancer. N. Engl. J. Med. 2022, 387, 9–20. [Google Scholar] [CrossRef] [PubMed]
- Curigliano, G.; Hu, X.; Dent, R.A.; Yonemori, K.; Barrios Sr, C.H.; O’Shaughnessy, J.; Wildiers, H.; Zhang, Q.; Im, S.-A.; Saura, C. Trastuzumab Deruxtecan (T-DXd) vs Physician’s Choice of Chemotherapy (TPC) in Patients (Pts) with Hormone Receptor-Positive (HR+), Human Epidermal Growth Factor Receptor 2 (HER2)-Low or HER2-Ultralow Metastatic Breast Cancer (mBC) with Prior Endocrine Therapy (ET): Primary Results from DESTINY-Breast06 (DB-06). J. Clin. Oncol. 2024, 42, LBA1000. [Google Scholar]
- Andre, F.; Hamilton, E.P.; Loi, S.; Anders, C.K.; Schmid, P.; Stroyakovskiy, D.; Villanueva, R.; Pedrini, J.L.; Doval, D.C.; Zurawski, B. DESTINY-Breast07: Dose-Expansion Interim Analysis of T-DXd Monotherapy and T-DXd+ Pertuzumab in Patients with Previously Untreated HER2+ mBC. J. Clin. Oncol. 2024, 42, 1009. [Google Scholar] [CrossRef]
- Saura, C.; Oliveira, M.; Feng, Y.-H.; Dai, M.-S.; Chen, S.-W.; Hurvitz, S.A.; Kim, S.-B.; Moy, B.; Delaloge, S.; Gradishar, W. Neratinib plus Capecitabine versus Lapatinib plus Capecitabine in HER2-Positive Metastatic Breast Cancer Previously Treated With≥ 2 HER2-Directed Regimens: Phase III NALA Trial. J. Clin. Oncol. 2020, 38, 3138–3149. [Google Scholar] [CrossRef]
- Curigliano, G.; Mueller, V.; Borges, V.; Hamilton, E.; Hurvitz, S.; Loi, S.; Murthy, R.; Okines, A.; Paplomata, E.; Cameron, D. Corrigendum to “Tucatinib versus Placebo Added to Trastuzumab and Capecitabine for Patients with Pretreated HER2D Metastatic Breast Cancer with and without Brain Metastases (HER2CLIMB): Final Overall Survival Analysis”: [Annals of Oncology 33 (2022) 321–329, (S0923753421048791), (10.1016/j.Annonc.2021.12.005)]. Ann. Oncol. 2023, 34, 630. [Google Scholar]
- Cameron, D.; Casey, M.; Oliva, C.; Newstat, B.; Imwalle, B.; Geyer, C.E. Lapatinib plus Capecitabine in Women with HER-2–Positive Advanced Breast Cancer: Final Survival Analysis of a Phase III Randomized Trial. Oncologist 2010, 15, 924–934. [Google Scholar] [CrossRef]
- Johnston, S.; Pippen, J., Jr.; Pivot, X.; Lichinitser, M.; Sadeghi, S.; Dieras, V.; Gomez, H.L.; Romieu, G.; Manikhas, A.; Kennedy, M.J. Lapatinib Combined with Letrozole versus Letrozole and Placebo as First-Line Therapy for Postmenopausal Hormone Receptor–Positive Metastatic Breast Cancer. J. Clin. Oncol. 2009, 27, 5538–5546. [Google Scholar] [CrossRef] [PubMed]
- Horimoto, Y.; Thinzar Hlaing, M.; Saeki, H.; Kitano, S.; Nakai, K.; Sasaki, R.; Kurisaki-Arakawa, A.; Arakawa, A.; Otsuji, N.; Matsuoka, S. Microsatellite Instability and Mismatch Repair Protein Expressions in Lymphocyte—Predominant Breast Cancer. Cancer Sci. 2020, 111, 2647–2654. [Google Scholar] [CrossRef]
- Landman, Y.; Ilouze, M.; Wein, S.; Neiman, V.; Yerushalmi, R.; Yakimov, M.; Ku, N.; Schrock, A.B.; Ali, S.; Peled, N. Rapid Response to Larotrectinib (LOXO-101) in an Adult Chemotherapy-Naive Patients with Advanced Triple-Negative Secretory Breast Cancer Expressing ETV6-NTRK3 Fusion. Clin. Breast Cancer 2018, 18, e267–e270. [Google Scholar] [CrossRef]
- Carbognin, L.; Miglietta, F.; Paris, I.; Dieci, M.V. Prognostic and Predictive Implications of PTEN in Breast Cancer: Unfulfilled Promises but Intriguing Perspectives. Cancers 2019, 11, 1401. [Google Scholar] [CrossRef]
- Song, M.S.; Salmena, L.; Pandolfi, P.P. The Functions and Regulation of the PTEN Tumour Suppressor. Nat. Rev. Mol. Cell Biol. 2012, 13, 283–296. [Google Scholar] [CrossRef]
- Dave, B.; Migliaccio, I.; Gutierrez, M.C.; Wu, M.-F.; Chamness, G.C.; Wong, H.; Narasanna, A.; Chakrabarty, A.; Hilsenbeck, S.G.; Huang, J. Loss of Phosphatase and Tensin Homolog or Phosphoinositol-3 Kinase Activation and Response to Trastuzumab or Lapatinib in Human Epidermal Growth Factor Receptor 2–Overexpressing Locally Advanced Breast Cancers. J. Clin. Oncol. 2011, 29, 166. [Google Scholar] [CrossRef] [PubMed]
- Barroso-Sousa, R.; Tyekucheva, S.; Pernas-Simon, S.; Exman, P.; Jain, E.; Garrido-Castro, A.; Hughes, M.; Bychkovsky, B.; Di Lascio, S.; Umeton, R. Abstract P5-12-02: PTEN Alterations and Tumor Mutational Burden (TMB) as Potential Predictors of Resistance or Response to Immune Checkpoint Inhibitors (ICI) in Metastatic Triple-Negative Breast Cancer (mTNBC). Cancer Res. 2019, 79, P5–P12. [Google Scholar] [CrossRef]
- Turner, N.C.; Oliveira, M.; Howell, S.J.; Dalenc, F.; Cortes, J.; Gomez Moreno, H.L.; Hu, X.; Jhaveri, K.; Krivorotko, P.; Loibl, S. Capivasertib in Hormone Receptor–Positive Advanced Breast Cancer. N. Engl. J. Med. 2023, 388, 2058–2070. [Google Scholar] [CrossRef]
- Ali, R.M.; McIntosh, S.A.; Savage, K.I. Homologous Recombination Deficiency in Breast Cancer: Implications for Risk, Cancer Development, and Therapy. Genes Chromosomes Cancer 2021, 60, 358–372. [Google Scholar] [CrossRef]
- Zundelevich, A.; Dadiani, M.; Kahana-Edwin, S.; Itay, A.; Sella, T.; Gadot, M.; Cesarkas, K.; Farage-Barhom, S.; Saar, E.G.; Eyal, E. ESR1 Mutations Are Frequent in Newly Diagnosed Metastatic and Loco-Regional Recurrence of Endocrine-Treated Breast Cancer and Carry Worse Prognosis. Breast Cancer Res. 2020, 22, 16. [Google Scholar] [CrossRef]
- Resources for Information | Approved Drugs. Available online: https://www.fda.gov/drugs/drug-approvals-and-databases/resources-information-approved-drugs/ (accessed on 21 May 2024).
- Fribbens, C.; O’Leary, B.; Kilburn, L.; Hrebien, S.; Garcia-Murillas, I.; Beaney, M.; Cristofanilli, M.; Andre, F.; Loi, S.; Loibl, S. Plasma ESR1 Mutations and the Treatment of Estrogen Receptor-Positive Advanced Breast Cancer. J. Clin. Oncol. 2016, 34, 2961–2968. [Google Scholar] [CrossRef] [PubMed]
- Bidard, F.-C.; Hardy-Bessard, A.-C.; Dalenc, F.; Bachelot, T.; Pierga, J.-Y.; de la Motte Rouge, T.; Sabatier, R.; Dubot, C.; Frenel, J.-S.; Ferrero, J.M. Switch to Fulvestrant and Palbociclib versus No Switch in Advanced Breast Cancer with Rising ESR1 Mutation during Aromatase Inhibitor and Palbociclib Therapy (PADA-1): A Randomised, Open-Label, Multicentre, Phase 3 Trial. Lancet Oncol. 2022, 23, 1367–1377. [Google Scholar] [CrossRef]
- Parisian, A.D.; Barratt, S.A.; Hodges-Gallagher, L.; Ortega, F.E.; Peña, G.; Sapugay, J.; Robello, B.; Sun, R.; Kulp, D.; Palanisamy, G.S. Palazestrant (OP-1250), A Complete Estrogen Receptor Antagonist, Inhibits Wild-Type and Mutant ER-Positive Breast Cancer Models as Monotherapy and in Combination. Mol. Cancer Ther. 2024, 23, 285–300. [Google Scholar] [CrossRef] [PubMed]
- Borges, V.F.; Chan, A.; Lin, N.U.; Tonda, M.E.; Shilkrut, M.; Alemany, C.A. A Phase 1b/2 Dose Escalation and Expansion Study of OP-1250 in Combination with Ribociclib or Alpelisib in Patients with Advanced and/or Metastatic Estrogen Receptor–Positive (ER+)/HER2-Negative (HER2-) Breast Cancer. J. Clin. Oncol. 2023, 41, TPS1127. [Google Scholar] [CrossRef]
- Johnston, S.R.; Pluard, T.J.; Wang, J.S.; Hamilton, E.P.; Song, T.; Rong, Y.; Yamaguchi, K.; Juric, D. H3B-6545+ Palbociclib in Patients (Pts) with Locally Advanced/Metastatic Estrogen Receptor-Positive (ER+), HER2 Negative (–) Breast Cancer (BC). J. Clin. Oncol. 2024, 42, 1051. [Google Scholar] [CrossRef]
- Gough, S.M.; Flanagan, J.J.; Teh, J.; Andreoli, M.; Rousseau, E.; Pannone, M.; Bookbinder, M.; Willard, R.; Davenport, K.; Bortolon, E. Oral Estrogen Receptor PROTAC Vepdegestrant (ARV-471) Is Highly Efficacious as Monotherapy and in Combination with CDK4/6 or PI3K/mTOR Pathway Inhibitors in Preclinical ER+ Breast Cancer Models. Clin. Cancer Res. 2024, 30, OF1–OF15. [Google Scholar] [CrossRef]
- Bertucci, F.; Ng, C.K.; Patsouris, A.; Droin, N.; Piscuoglio, S.; Carbuccia, N.; Soria, J.C.; Dien, A.T.; Adnani, Y.; Kamal, M. Genomic Characterization of Metastatic Breast Cancers. Nature 2019, 569, 560–564. [Google Scholar] [CrossRef]
- Im, S.-A.; Lu, Y.-S.; Bardia, A.; Harbeck, N.; Colleoni, M.; Franke, F.; Chow, L.; Sohn, J.; Lee, K.-S.; Campos-Gomez, S. Overall Survival with Ribociclib plus Endocrine Therapy in Breast Cancer. N. Engl. J. Med. 2019, 381, 307–316. [Google Scholar] [CrossRef]
- Verret, B.; Bottosso, M.; Hervais, S.; Pistilli, B. The Molecular Predictive and Prognostic Biomarkers in Metastatic Breast Cancer: The Contribution of Molecular Profiling. Cancers 2022, 14, 4203. [Google Scholar] [CrossRef]
- Testing the Use of Fulvestrant and Binimetinib Targeted Treatment for NF1 Mutation in Hormone Receptor-Positive Metastatic Breast Cancer (A ComboMATCH Treatment Trial). Available online: https://clinicaltrials.gov/ct2/show/NCT05554354 (accessed on 23 April 2024).
- Dansonka-Mieszkowska, A.; Kluska, A.; Moes, J.; Dabrowska, M.; Nowakowska, D.; Niwinska, A.; Derlatka, P.; Cendrowski, K.; Kupryjanczyk, J. A Novel Germline PALB2 Deletion in Polish Breast and Ovarian Cancer Patients. BMC Med. Genet. 2010, 11, 20. [Google Scholar] [CrossRef]
- Antoniou, A.C.; Casadei, S.; Heikkinen, T.; Barrowdale, D.; Pylkäs, K.; Roberts, J.; Lee, A.; Subramanian, D.; De Leeneer, K.; Fostira, F. Breast-Cancer Risk in Families with Mutations in PALB2. N. Engl. J. Med. 2014, 371, 497–506. [Google Scholar] [CrossRef]
- Gruber, J.J.; Afghahi, A.; Timms, K.; DeWees, A.; Gross, W.; Aushev, V.N.; Wu, H.-T.; Balcioglu, M.; Sethi, H.; Scott, D. A Phase II Study of Talazoparib Monotherapy in Patients with Wild-Type BRCA1 and BRCA2 with a Mutation in Other Homologous Recombination Genes. Nat. Cancer 2022, 3, 1181–1191. [Google Scholar] [CrossRef] [PubMed]
- Yang, L.; Wang, X.; Zhu, L.; Wang, H.; Wang, B.; Zhao, Q.; Wang, X. Significance and Prognosis of Epithelial—Cadherin Expression in Invasive Breast Carcinoma. Oncol. Lett. 2018, 16, 1659–1665. [Google Scholar] [CrossRef]
- Corso, G.; Figueiredo, J.; De Angelis, S.P.; Corso, F.; Girardi, A.; Pereira, J.; Seruca, R.; Bonanni, B.; Carneiro, P.; Pravettoni, G. E-cadherin Deregulation in Breast Cancer. J. Cell. Mol. Med. 2020, 24, 5930–5936. [Google Scholar] [CrossRef] [PubMed]
- Gao, J.; Yao, Y.; Liu, C.; Xie, X.; Li, D.; Liu, P.; Wang, Z.; Zhang, B.; Ren, R. Synergism of FAK and ROS1 Inhibitors in the Treatment of CDH1-Deficient Cancers Mediated by FAK-YAP Signaling. Int. J. Biol. Sci. 2023, 19, 2711. [Google Scholar] [CrossRef] [PubMed]
- Shahbandi, A.; Nguyen, H.D.; Jackson, J.G. TP53 Mutations and Outcomes in Breast Cancer: Reading beyond the Headlines. Trends Cancer 2020, 6, 98–110. [Google Scholar] [CrossRef]
- Li, J.; Zhang, X.; Zhang, Z.; Zheng, L.; Jindal, S.; Liu, Y. Association of P53 Expression with Poor Prognosis in Patients with Triple-Negative Breast Invasive Ductal Carcinoma. Medicine 2019, 98, e15449. [Google Scholar] [CrossRef]
- Huszno, J.; Grzybowska, E. TP53 Mutations and SNPs as Prognostic and Predictive Factors in Patients with Breast Cancer. Oncol. Lett. 2018, 16, 34–40. [Google Scholar] [CrossRef]
- Cybulski, C.; Wokołorczyk, D.; Jakubowska, A.; Huzarski, T.; Byrski, T.; Gronwald, J.; Masojć, B.; Dębniak, T.; Górski, B.; Blecharz, P. Risk of Breast Cancer in Women with a CHEK2 Mutation with and without a Family History of Breast Cancer. J. Clin. Oncol. 2011, 29, 3747–3752. [Google Scholar] [CrossRef]
- Ansari, N.; Shahrabi, S.; Khosravi, A.; Shirzad, R.; Rezaeean, H. Prognostic Significance of CHEK2 Mutation in Progression of Breast Cancer. Lab. Med. 2019, 50, e36–e41. [Google Scholar] [CrossRef]
- Chrisanthar, R.; Knappskog, S.; Løkkevik, E.; Anker, G.; Østenstad, B.; Lundgren, S.; Berge, E.O.; Risberg, T.; Mjaaland, I.; Mæhle, L. CHEK2 Mutations Affecting Kinase Activity Together with Mutations in TP53 Indicate a Functional Pathway Associated with Resistance to Epirubicin in Primary Breast Cancer. PLoS ONE 2008, 3, e3062. [Google Scholar] [CrossRef]
- van Os, N.J.; Roeleveld, N.; Weemaes, C.M.; Jongmans, M.C.; Janssens, G.; Taylor, A.M.R.; Hoogerbrugge, N.; Willemsen, M.A. Health Risks for Ataxia-telangiectasia Mutated Heterozygotes: A Systematic Review, Meta-analysis and Evidence-based Guideline. Clin. Genet. 2016, 90, 105–117. [Google Scholar] [CrossRef] [PubMed]
- Angèle, S.; Hall, J. The ATM Gene and Breast Cancer: Is It Really a Risk Factor? Mutat. Res. Rev. Mutat. Res. 2000, 462, 167–178. [Google Scholar] [CrossRef] [PubMed]
- Bueno, R.; Canevari, R.; Villacis, R.; Domingues, M.A.C.; Caldeira, J.; Rocha, R.M.; Drigo, S.; Rogatto, S.R. ATM Down-Regulation Is Associated with Poor Prognosis in Sporadic Breast Carcinomas. Ann. Oncol. 2014, 25, 69–75. [Google Scholar] [CrossRef]
- Bartkova, J.; Tommiska, J.; Oplustilova, L.; Aaltonen, K.; Tamminen, A.; Heikkinen, T.; Mistrik, M.; Aittomäki, K.; Blomqvist, C.; Heikkilä, P. Aberrations of the MRE11–RAD50–NBS1 DNA Damage Sensor Complex in Human Breast Cancer: MRE11 as a Candidate Familial Cancer-Predisposing Gene. Mol. Oncol. 2008, 2, 296–316. [Google Scholar] [CrossRef]
- Yuan, S.-S.F.; Hou, M.-F.; Hsieh, Y.-C.; Huang, C.-Y.; Lee, Y.-C.; Chen, Y.-J.; Lo, S. Role of MRE11 in Cell Proliferation, Tumor Invasion, and DNA Repair in Breast Cancer. J. Natl. Cancer Inst. 2012, 104, 1485–1502. [Google Scholar] [CrossRef]
- Seal, S.; Thompson, D.; Renwick, A.; Elliott, A.; Kelly, P.; Barfoot, R.; Chagtai, T.; Jayatilake, H.; Ahmed, M.; Spanova, K. Truncating Mutations in the Fanconi Anemia J Gene BRIP1 Are Low-Penetrance Breast Cancer Susceptibility Alleles. Nat. Genet. 2006, 38, 1239–1241. [Google Scholar] [CrossRef]
- Liao, S.; Liu, L.; Wang, Y. Effect of RAD51C Expression on the Chemosensitivity of Eμ-Myc p19Arf-/-cells and Its Clinical Significance in Breast Cancer. Oncol. Lett. 2018, 15, 6107–6114. [Google Scholar] [CrossRef] [PubMed]
- Śniadecki, M.; Brzeziński, M.; Darecka, K.; Klasa-Mazurkiewicz, D.; Poniewierza, P.; Krzeszowiec, M.; Kmieć, N.; Wydra, D. BARD1 and Breast Cancer: The Possibility of Creating Screening Tests and New Preventive and Therapeutic Pathways for Predisposed Women. Genes 2020, 11, 1251. [Google Scholar] [CrossRef]
- Zhu, Y.; Liu, Y.; Zhang, C.; Chu, J.; Wu, Y.; Li, Y.; Liu, J.; Li, Q.; Li, S.; Shi, Q. Tamoxifen-Resistant Breast Cancer Cells Are Resistant to DNA-Damaging Chemotherapy Because of Upregulated BARD1 and BRCA1. Nat. Commun. 2018, 9, 1595. [Google Scholar] [CrossRef]
- Kotalwar, K.S.; Deshmukh, A.V.; Gangane, N.M. Role of Caspase-8 as a Prognostic Biomarker in Breast Cancer—A Pilot Study in Central India. Indian J. Gynecol. Oncol. 2021, 19, 74. [Google Scholar] [CrossRef]
- Pu, X.; Storr, S.J.; Zhang, Y.; Rakha, E.A.; Green, A.R.; Ellis, I.O.; Martin, S.G. Caspase-3 and Caspase-8 Expression in Breast Cancer: Caspase-3 Is Associated with Survival. Apoptosis 2017, 22, 357–368. [Google Scholar] [CrossRef] [PubMed]
- Mao, H.; Zhang, L.; Yang, Y.; Zuo, W.; Bi, Y.; Gao, W.; Deng, B.; Sun, J.; Shao, Q.; Qu, X. New Insights of CTLA-4 into Its Biological Function in Breast Cancer. Curr. Cancer Drug Targets 2010, 10, 728–736. [Google Scholar] [CrossRef]
- Li, W.; Sang, M.; Hao, X.; Wu, Y.; Shan, B. CTLA-4 Blockade Combined with 5-aza-2′-deoxycytidine Enhances the Killing Effect of MAGE-A Family Common Antigen Peptide-specific Cytotoxic T Cells on Breast Cancer. Oncol. Rep. 2020, 44, 1758–1770. [Google Scholar] [CrossRef] [PubMed]
- Kern, R.; Panis, C. CTLA-4 Expression and Its Clinical Significance in Breast Cancer. Arch. Immunol. Et Ther. Exp. 2021, 69, 16. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.; Simpson, E.R.; Brown, K.A. Aromatase Overexpression in Dysfunctional Adipose Tissue Links Obesity to Postmenopausal Breast Cancer. J. Steroid Biochem. Mol. Biol. 2015, 153, 35–44. [Google Scholar] [CrossRef]
- Chang, J.; Liu, X.; Wang, S.; Zhang, Z.; Wu, Z.; Zhang, X.; Li, J. Prognostic Value of FGFR Gene Amplification in Patients with Different Types of Cancer: A Systematic Review and Meta-Analysis. PLoS ONE 2014, 9, e105524. [Google Scholar] [CrossRef]
- Cheng, C.L.; Thike, A.A.; Tan, S.Y.J.; Chua, P.J.; Bay, B.H.; Tan, P.H. Expression of FGFR1 Is an Independent Prognostic Factor in Triple-Negative Breast Cancer. Breast Cancer Res. Treat. 2015, 151, 99–111. [Google Scholar] [CrossRef]
- Turner, N.; Pearson, A.; Sharpe, R.; Lambros, M.; Geyer, F.; Lopez-Garcia, M.A.; Natrajan, R.; Marchio, C.; Iorns, E.; Mackay, A. FGFR1 Amplification Drives Endocrine Therapy Resistance and Is a Therapeutic Target in Breast Cancer. Cancer Res. 2010, 70, 2085–2094. [Google Scholar] [CrossRef]
- Chew, N.J.; Nguyen, E.V.; Su, S.-P.; Novy, K.; Chan, H.C.; Nguyen, L.K.; Luu, J.; Simpson, K.J.; Lee, R.S.; Daly, R.J. FGFR3 Signaling and Function in Triple Negative Breast Cancer. Cell Commun. Signal. 2020, 18, 13. [Google Scholar] [CrossRef]
- Garcia-Recio, S.; Thennavan, A.; East, M.P.; Parker, J.S.; Cejalvo, J.M.; Garay, J.P.; Hollern, D.P.; He, X.; Mott, K.R.; Galván, P. FGFR4 Regulates Tumor Subtype Differentiation in Luminal Breast Cancer and Metastatic Disease. J. Clin. Investig. 2020, 130, 4871–4887. [Google Scholar] [CrossRef] [PubMed]
- Levine, K.M.; Priedigkeit, N.; Basudan, A.; Tasdemir, N.; Sikora, M.J.; Sokol, E.S.; Hartmaier, R.J.; Ding, K.; Ahmad, N.Z.; Watters, R.J. FGFR4 Overexpression and Hotspot Mutations in Metastatic ER+ Breast Cancer Are Enriched in the Lobular Subtype. NPJ Breast Cancer 2019, 5, 19. [Google Scholar] [CrossRef]
- Wang, J.; Sun, J.; Yang, F. The Role of Long Non-coding RNA H19 in Breast Cancer. Oncol. Lett. 2020, 19, 7–16. [Google Scholar] [CrossRef] [PubMed]
- Elias-Rizk, T.; El Hajj, J.; Segal-Bendirdjian, E.; Hilal, G. The Long Non Coding RNA H19 as a Biomarker for Breast Cancer Diagnosis in Lebanese Women. Sci. Rep. 2020, 10, 22228. [Google Scholar] [CrossRef]
- Shay, J.W.; Bacchetti, S. A Survey of Telomerase Activity in Human Cancer. Eur. J. Cancer 1997, 33, 787–791. [Google Scholar] [CrossRef] [PubMed]
- Yoshida, M.; Ogawa, R.; Yoshida, H.; Maeshima, A.; Kanai, Y.; Kinoshita, T.; Hiraoka, N.; Sekine, S. TERT Promoter Mutations Are Frequent and Show Association with MED12 Mutations in Phyllodes Tumors of the Breast. Br. J. Cancer 2015, 113, 1244–1248. [Google Scholar] [CrossRef]
- Pareja, F.; Toss, M.S.; Geyer, F.C.; da Silva, E.M.; Vahdatinia, M.; Sebastiao, A.P.M.; Selenica, P.; Szatrowski, A.; Edelweiss, M.; Wen, H.Y. Immunohistochemical Assessment of HRAS Q61R Mutations in Breast Adenomyoepitheliomas. Histopathology 2020, 76, 865–874. [Google Scholar] [CrossRef]
- Judasz, E.; Lisiak, N.; Kopczyński, P.; Taube, M.; Rubiś, B. The Role of Telomerase in Breast Cancer’s Response to Therapy. Int. J. Mol. Sci. 2022, 23, 12844. [Google Scholar] [CrossRef]
- Nixon, M.J.; Formisano, L.; Mayer, I.A.; Estrada, M.V.; González-Ericsson, P.I.; Isakoff, S.J.; Forero-Torres, A.; Won, H.; Sanders, M.E.; Solit, D.B. PIK3CA and MAP3K1 Alterations Imply Luminal A Status and Are Associated with Clinical Benefit from Pan-PI3K Inhibitor Buparlisib and Letrozole in ER+ Metastatic Breast Cancer. NPJ Breast Cancer 2019, 5, 31. [Google Scholar] [CrossRef]
- Zhang, G.; Zeng, Y.; Liu, Z.; Wei, W. Significant Association between Nijmegen Breakage Syndrome 1 657del5 Polymorphism and Breast Cancer Risk. Tumor Biol. 2013, 34, 2753–2757. [Google Scholar] [CrossRef]
- Lal, S.; Reed, A.E.M.; de Luca, X.M.; Simpson, P.T. Molecular Signatures in Breast Cancer. Methods 2017, 131, 135–146. [Google Scholar] [CrossRef]
- Eigeliene, N.; Saarenheimo, J.; Jekunen, A. Potential of Liquid Biopsies for Breast Cancer Screening, Diagnosis, and Response to Treatment. Oncology 2019, 96, 115–124. [Google Scholar] [CrossRef] [PubMed]
- Bettegowda, C.; Sausen, M.; Leary, R.J.; Kinde, I.; Wang, Y.; Agrawal, N.; Bartlett, B.R.; Wang, H.; Luber, B.; Alani, R.M. Detection of Circulating Tumor DNA in Early-and Late-Stage Human Malignancies. Sci. Transl. Med. 2014, 6, 224ra24. [Google Scholar] [CrossRef] [PubMed]
- Mandel, P.; Metais, P. Nuclear Acids in Human Blood Plasma. C. R. Seances Soc. Biol. Fil. 1948, 142, 241–243. [Google Scholar] [PubMed]
- Sobhani, N.; Generali, D.; Zanconati, F.; Bortul, M.; Scaggiante, B. Cell-Free DNA Integrity for the Monitoring of Breast Cancer: Future Perspectives? World J. Clin. Oncol. 2018, 9, 26. [Google Scholar] [CrossRef]
- Umetani, N.; Giuliano, A.E.; Hiramatsu, S.H.; Amersi, F.; Nakagawa, T.; Martino, S.; Hoon, D.S. Prediction of Breast Tumor Progression by Integrity of Free Circulating DNA in Serum. J. Clin. Oncol. 2006, 24, 4270–4276. [Google Scholar] [CrossRef] [PubMed]
- Shapiro, B.; Chakrabarty, M.; Cohn, E.M.; Leon, S.A. Determination of Circulating DNA Levels in Patients with Benign or Malignant Gastrointestinal Disease. Cancer 1983, 51, 2116–2120. [Google Scholar] [CrossRef] [PubMed]
- Qin, Z.; Ljubimov, V.A.; Zhou, C.; Tong, Y.; Liang, J. Cell-Free Circulating Tumor DNA in Cancer. Chin. J. Cancer 2016, 35, 36. [Google Scholar] [CrossRef]
- Keller, L.; Belloum, Y.; Wikman, H.; Pantel, K. Clinical Relevance of Blood-Based ctDNA Analysis: Mutation Detection and Beyond. Br. J. Cancer 2021, 124, 345–358. [Google Scholar] [CrossRef]
- Markou, A.; Tzanikou, E.; Ladas, I.; Makrigiorgos, G.M.; Lianidou, E. Nuclease-Assisted Minor Allele Enrichment Using Overlapping Probes-Assisted Amplification-Refractory Mutation System: An Approach for the Improvement of Amplification-Refractory Mutation System-Polymerase Chain Reaction Specificity in Liquid Biopsies. Anal. Chem. 2019, 91, 13105–13111. [Google Scholar] [CrossRef]
- Wang, Y.-H.; Song, Z.; Hu, X.-Y.; Wang, H.-S. Circulating Tumor DNA Analysis for Tumor Diagnosis. Talanta 2021, 228, 122220. [Google Scholar] [CrossRef] [PubMed]
- Olsson, E.; Winter, C.; George, A.; Chen, Y.; Howlin, J.; Tang, M.E.; Dahlgren, M.; Schulz, R.; Grabau, D.; van Westen, D. Serial Monitoring of Circulating Tumor DNA in Patients with Primary Breast Cancer for Detection of Occult Metastatic Disease. EMBO Mol. Med. 2015, 7, 1034–1047. [Google Scholar] [CrossRef]
- Li, C.; He, Q.; Liang, H.; Cheng, B.; Li, J.; Xiong, S.; Zhao, Y.; Guo, M.; Liu, Z.; He, J. Diagnostic Accuracy of Droplet Digital PCR and Amplification Refractory Mutation System PCR for Detecting EGFR Mutation in Cell-Free DNA of Lung Cancer: A Meta-Analysis. Front. Oncol. 2020, 10, 290. [Google Scholar] [CrossRef] [PubMed]
- O’Leary, B.; Hrebien, S.; Beaney, M.; Fribbens, C.; Garcia-Murillas, I.; Jiang, J.; Li, Y.; Huang Bartlett, C.; Andre, F.; Loibl, S. Comparison of BEAMing and Droplet Digital PCR for Circulating Tumor DNA Analysis. Clin. Chem. 2019, 65, 1405–1413. [Google Scholar] [CrossRef] [PubMed]
- Hrebien, S.; O’Leary, B.; Beaney, M.; Schiavon, G.; Fribbens, C.; Bhambra, A.; Johnson, R.; Garcia-Murillas, I.; Turner, N. Reproducibility of Digital PCR Assays for Circulating Tumor DNA Analysis in Advanced Breast Cancer. PLoS ONE 2016, 11, e0165023. [Google Scholar] [CrossRef] [PubMed]
- Forbes, S.A.; Beare, D.; Boutselakis, H.; Bamford, S.; Bindal, N.; Tate, J.; Cole, C.G.; Ward, S.; Dawson, E.; Ponting, L. COSMIC: Somatic Cancer Genetics at High-Resolution. Nucleic Acids Res. 2017, 45, D777–D783. [Google Scholar] [CrossRef]
- Hai, L.; Li, L.; Liu, Z.; Tong, Z.; Sun, Y. Whole-genome Circulating Tumor DNA Methylation Landscape Reveals Sensitive Biomarkers of Breast Cancer. MedComm 2022, 3, e134. [Google Scholar] [CrossRef]
- Lin, C.; Liu, X.; Zheng, B.; Ke, R.; Tzeng, C.-M. Liquid Biopsy, ctDNA Diagnosis through NGS. Life 2021, 11, 890. [Google Scholar] [CrossRef]
- Clatot, F. Review ctDNA and Breast Cancer. In Tumor Liquid Biopsies; Springer: Cham, Switzerland, 2020; pp. 231–252. [Google Scholar]
- Zhou, Y.; Xu, Y.; Gong, Y.; Zhang, Y.; Lu, Y.; Wang, C.; Yao, R.; Li, P.; Guan, Y.; Wang, J. Clinical Factors Associated with Circulating Tumor DNA (Ct DNA) in Primary Breast Cancer. Mol. Oncol. 2019, 13, 1033–1046. [Google Scholar] [CrossRef]
- Pascual, J.; Attard, G.; Bidard, F.-C.; Curigliano, G.; de Mattos-Arruda, L.; Diehn, M.; Italiano, A.; Lindberg, J.; Merker, J.D.; Montagut, C. ESMO Recommendations on the Use of Circulating Tumour DNA Assays for Patients with Cancer: A Report from the ESMO Precision Medicine Working Group. Ann. Oncol. 2022, 33, 750–768. [Google Scholar] [CrossRef]
- Rodriguez, B.J.; Córdoba, G.D.; Aranda, A.G.; Álvarez, M.; Vicioso, L.; Pérez, C.L.; Hernando, C.; Bermejo, B.; Parreño, A.J.; Lluch, A. Detection of TP53 and PIK3CA Mutations in Circulating Tumor DNA Using Next-Generation Sequencing in the Screening Process for Early Breast Cancer Diagnosis. J. Clin. Med. 2019, 8, 1183. [Google Scholar] [CrossRef] [PubMed]
- Garcia-Murillas, I.; Schiavon, G.; Weigelt, B.; Ng, C.; Hrebien, S.; Cutts, R.J.; Cheang, M.; Osin, P.; Nerurkar, A.; Kozarewa, I. Mutation Tracking in Circulating Tumor DNA Predicts Relapse in Early Breast Cancer. Sci. Transl. Med. 2015, 7, 302ra133. [Google Scholar] [CrossRef]
- Coombes, R.C.; Page, K.; Salari, R.; Hastings, R.K.; Armstrong, A.; Ahmed, S.; Ali, S.; Cleator, S.; Kenny, L.; Stebbing, J. Personalized Detection of Circulating Tumor DNA Antedates Breast Cancer Metastatic Recurrence. Clin. Cancer Res. 2019, 25, 4255–4263. [Google Scholar] [CrossRef] [PubMed]
- Ranganathan, K.; Sivasankar, V. MicroRNAs-Biology and Clinical Applications. J. Oral Maxillofac. Pathol. 2014, 18, 229–234. [Google Scholar] [CrossRef] [PubMed]
- MacFarlane, L.-A.; R Murphy, P. MicroRNA: Biogenesis, Function and Role in Cancer. Curr. Genom. 2010, 11, 537–561. [Google Scholar] [CrossRef]
- O’Brien, J.; Hayder, H.; Zayed, Y.; Peng, C. Overview of microRNA Biogenesis, Mechanisms of Actions, and Circulation. Front. Endocrinol. 2018, 9, 388354. [Google Scholar] [CrossRef]
- Bofill-De Ros, X.; Vang Ørom, U.A. Recent Progress in miRNA Biogenesis and Decay. RNA Biol. 2024, 21, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Singh, R.; Mo, Y.-Y. Role of microRNAs in Breast Cancer. Cancer Biol. Ther. 2013, 14, 201–212. [Google Scholar] [CrossRef]
- Muñoz, J.P.; Pérez-Moreno, P.; Pérez, Y.; Calaf, G.M. The Role of MicroRNAs in Breast Cancer and the Challenges of Their Clinical Application. Diagnostics 2023, 13, 3072. [Google Scholar] [CrossRef]
- Yan, L.-X.; Huang, X.-F.; Shao, Q.; Huang, M.-Y.; Deng, L.; Wu, Q.-L.; Zeng, Y.-X.; Shao, J.-Y. MicroRNA miR-21 Overexpression in Human Breast Cancer Is Associated with Advanced Clinical Stage, Lymph Node Metastasis and Patient Poor Prognosis. RNA 2008, 14, 2348–2360. [Google Scholar] [CrossRef]
- Grimaldi, A.M.; Nuzzo, S.; Condorelli, G.; Salvatore, M.; Incoronato, M. Prognostic and Clinicopathological Significance of MiR-155 in Breast Cancer: A Systematic Review. Int. J. Mol. Sci. 2020, 21, 5834. [Google Scholar] [CrossRef] [PubMed]
- Khalighfard, S.; Alizadeh, A.M.; Irani, S.; Omranipour, R. Plasma miR-21, miR-155, miR-10b, and Let-7a as the Potential Biomarkers for the Monitoring of Breast Cancer Patients. Sci. Rep. 2018, 8, 17981. [Google Scholar] [CrossRef]
- Mansoori, B.; Silvestris, N.; Mohammadi, A.; Khaze, V.; Baghbani, E.; Mokhtarzadeh, A.; Shanehbandi, D.; Derakhshani, A.; Duijf, P.H.; Baradaran, B. miR-34a and miR-200c Have an Additive Tumor-Suppressive Effect on Breast Cancer Cells and Patient Prognosis. Genes 2021, 12, 267. [Google Scholar] [CrossRef] [PubMed]
- Amiruddin, A.; Massi, M.N.; Islam, A.A.; Patellongi, I.; Pratama, M.Y.; Sutandyo, N.; Natzir, R.; Hatta, M.; Latar, N.H.M.; Wahid, S. microRNA-221 and Tamoxifen Resistance in Luminal-Subtype Breast Cancer Patients: A Case—Control Study. Ann. Med. Surg. 2022, 73, 103092. [Google Scholar] [CrossRef]
- Moody, H.L.; Lind, M.J.; Maher, S.G. MicroRNA-31 Regulates Chemosensitivity in Malignant Pleural Mesothelioma. Mol. Ther. Nucleic Acids 2017, 8, 317–329. [Google Scholar] [CrossRef] [PubMed]
- Kirave, P.; Gondaliya, P.; Kulkarni, B.; Rawal, R.; Garg, R.; Jain, A.; Kalia, K. Exosome Mediated miR-155 Delivery Confers Cisplatin Chemoresistance in Oral Cancer Cells via Epithelial-Mesenchymal Transition. Oncotarget 2020, 11, 1157. [Google Scholar] [CrossRef]
- Holinstat, M. Normal Platelet Function. Cancer Metastasis Rev. 2017, 36, 195–198. [Google Scholar] [CrossRef]
- Haemmerle, M.; Stone, R.L.; Menter, D.G.; Afshar-Kharghan, V.; Sood, A.K. The Platelet Lifeline to Cancer: Challenges and Opportunities. Cancer Cell 2018, 33, 965–983. [Google Scholar] [CrossRef]
- Schlesinger, M. Role of Platelets and Platelet Receptors in Cancer Metastasis. J. Hematol. Oncol. 2018, 11, 125. [Google Scholar] [CrossRef]
- Plantureux, L.; Mège, D.; Crescence, L.; Carminita, E.; Robert, S.; Cointe, S.; Brouilly, N.; Ezzedine, W.; Dignat-George, F.; Dubois, C. The Interaction of Platelets with Colorectal Cancer Cells Inhibits Tumor Growth but Promotes Metastasis. Cancer Res. 2020, 80, 291–303. [Google Scholar] [CrossRef]
- Wurdinger, T.; In ‘t Veld, S.G.; Best, M.G. Platelet RNA as Pan-Tumor Biomarker for Cancer Detection. Cancer Res. 2020, 80, 1371–1373. [Google Scholar] [CrossRef] [PubMed]
- Sol, N.; Wurdinger, T. Platelet RNA Signatures for the Detection of Cancer. Cancer Metastasis Rev. 2017, 36, 263–272. [Google Scholar] [CrossRef] [PubMed]
- GJG, S.; Wurdinger, T. Tumor-Educated Platelets. Blood 2019, 133, 2359–2364. [Google Scholar]
- Best, M.G.; Sol, N.; Kooi, I.; Tannous, J.; Westerman, B.A.; Rustenburg, F.; Schellen, P.; Verschueren, H.; Post, E.; Koster, J. RNA-Seq of Tumor-Educated Platelets Enables Blood-Based Pan-Cancer, Multiclass, and Molecular Pathway Cancer Diagnostics. Cancer Cell 2015, 28, 666–676. [Google Scholar] [CrossRef] [PubMed]
- D’ambrosi, S.; Visser, A.; Antunes-Ferreira, M.; Poutsma, A.; Giannoukakos, S.; Sol, N.; Sabrkhany, S.; Bahce, I.; Kuijpers, M.J.; Oude Egbrink, M.G. The Analysis of Platelet-Derived circRNA Repertoire as Potential Diagnostic Biomarker for Non-Small Cell Lung Cancer. Cancers 2021, 13, 4644. [Google Scholar] [CrossRef]
- Liefaard, M.C.; Moore, K.S.; Mulder, L.; van den Broek, D.; Wesseling, J.; Sonke, G.S.; Wessels, L.F.; Rookus, M.; Lips, E.H. Tumour-Educated Platelets for Breast Cancer Detection: Biological and Technical Insights. Br. J. Cancer 2023, 128, 1572–1581. [Google Scholar] [CrossRef] [PubMed]
| Therapeutic Setup: HER-2 Positive BC | ||
|---|---|---|
| Type | Monoclonal antibodies | Agents: Trastuzumab (Herceptin), Pertuzumab (Perjeta), Ado-trastuzumab emtansine (T-DM1, Kadcyla), Pertuzumab, trastuzumab, Trastuzumab deruxtecan (Enhertu) and hyaluronidase-zzxf (Phesgo) |
| Tyrosine kinase inhibitors | Agents: Neratinib (Nerlynx), Lapatinib (Tykerb), Tucatinib (Tukysa) | |
| Antibody-Drug Conjugates | Agent: Margetuximab-cmkb (Margenza) | |
| Therapeutic setup: Hormone receptor-positive BC | ||
| Type | Selective Estrogen Receptor Modulators (SERMs) | Agents: Tamoxifen citrate (Soltamox), Toremifene (Fareston) |
| Selective Estrogen Receptor Degraders (SERDs) | Agents: Fulvestrant (Faslodex) Elacestrant dihydrochloride (Orserdu) | |
| Aromatase Inhibitors | Agents: Anastrozole (Arimidex), Letrozole (Femara), Exemestane (Aromasin) | |
| CDK4/6 Inhibitors | Agents: Palbociclib (Ibrance), Ribociclib (Kisqali), Abemaciclib (Verzenio) | |
| Therapeutic setup: Triple-Negative Breast Cancer (TNBC) | ||
| Type | Immune Checkpoint Inhibitors | Agents: Atezolizumab (Tecentriq), Pembrolizumab (Keytruda) |
| Antibody-Drug Conjugates | Agent: Sacituzumab govitecan (Trodelvy) | |
| Other indications: | ||
| PARP Inhibitors (for BRCA-Mutated Breast Cancer) | Agents: Olaparib (Lynparza), Talazoparib (Talzenna) | |
| PI3K Inhibitors | Agent: Alpelisib (Piqray) | |
| mTOR Inhibitors | Agent: Everolimus (Afinitor) | |
| AKT inhibitors | Agent: Capivasertib (Truqap) | |
| Antibody-Drug Conjugates | Agent: Trastuzumab deruxtecan (Enhertu) | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ultimescu, F.; Hudita, A.; Popa, D.E.; Olinca, M.; Muresean, H.A.; Ceausu, M.; Stanciu, D.I.; Ginghina, O.; Galateanu, B. Impact of Molecular Profiling on Therapy Management in Breast Cancer. J. Clin. Med. 2024, 13, 4995. https://doi.org/10.3390/jcm13174995
Ultimescu F, Hudita A, Popa DE, Olinca M, Muresean HA, Ceausu M, Stanciu DI, Ginghina O, Galateanu B. Impact of Molecular Profiling on Therapy Management in Breast Cancer. Journal of Clinical Medicine. 2024; 13(17):4995. https://doi.org/10.3390/jcm13174995
Chicago/Turabian StyleUltimescu, Flavia, Ariana Hudita, Daniela Elena Popa, Maria Olinca, Horatiu Alin Muresean, Mihail Ceausu, Diana Iuliana Stanciu, Octav Ginghina, and Bianca Galateanu. 2024. "Impact of Molecular Profiling on Therapy Management in Breast Cancer" Journal of Clinical Medicine 13, no. 17: 4995. https://doi.org/10.3390/jcm13174995





