Comparative Efficacy and Safety of Robot-Assisted vs. Freehand Screw Placement in Femoral Neck Fractures: An Updated Systematic Review and Meta-Analysis
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
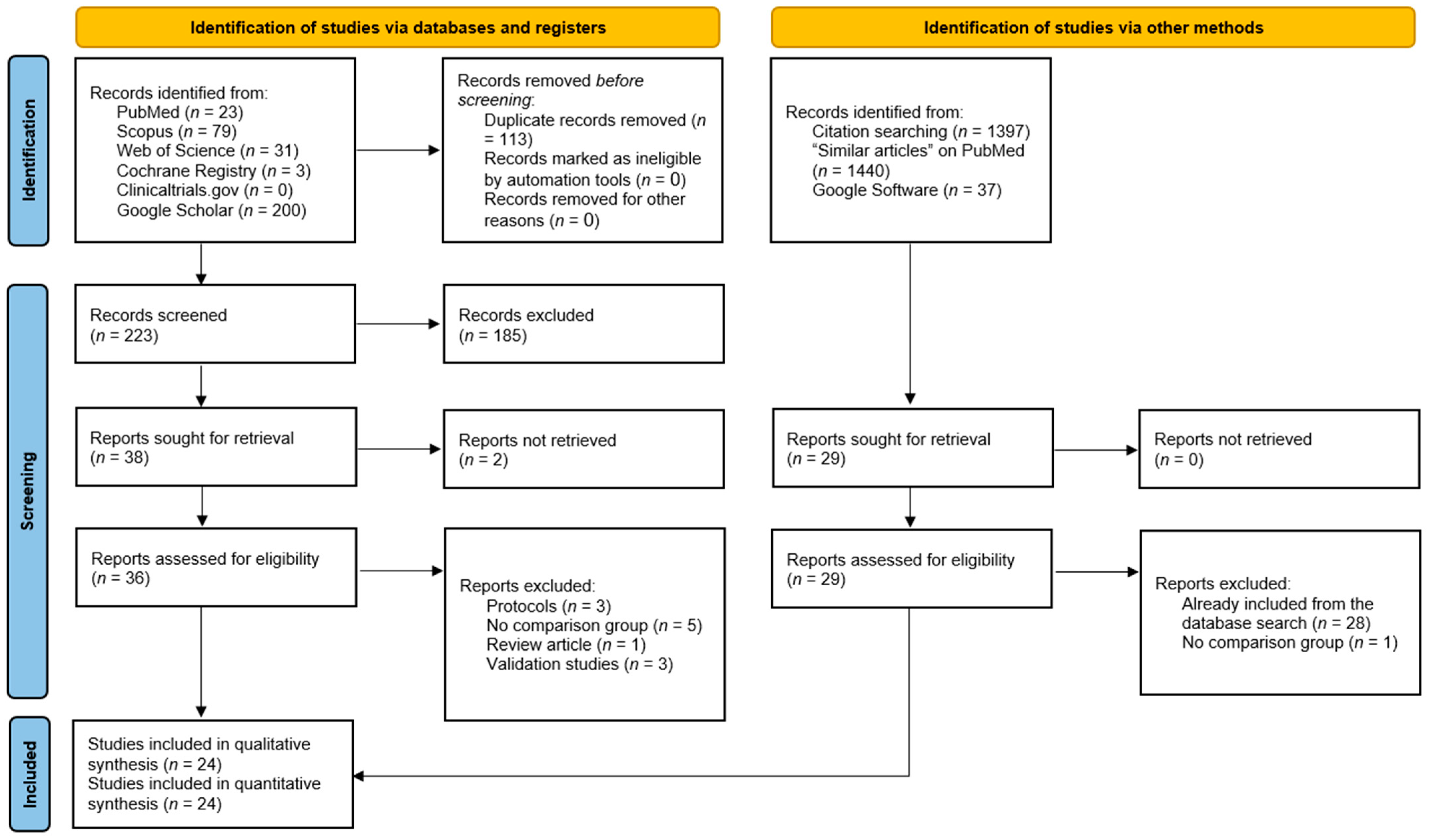
2.2. Literature Search
2.3. Selection Strategy
- Experimental (randomized or non-randomized trial) and observation studies (study design).
- Studies including patients with femoral neck fracture (population).
- Patients receiving robot-assisted screw placement (intervention).
- Studies comparing a robotic approach to a freehand approach (comparison/control group).
- Studies reporting one of our outcomes of interest (listed in the next sub-section).
- Non-original research (i.e., reviews, editorials, perspectives, commentaries, etc.).
- Published protocols without results.
- Studies without a comparison group.
- Validation studies reporting the feasibility of implementing robotics in orthopedic surgery.
- Irrelevant populations (patients without femoral neck fracture or fracture at other sites).
- No clear description of the intervention or comparison groups.
- Duplicates studies.
- Studies with overlapping patients’ data.
2.4. Data Collection and Outcome Measures
2.5. Risk of Bias Assessment
2.6. Statistical Analysis
3. Results
3.1. Literature Search Results
3.2. Baseline Characteristics of Included Studies
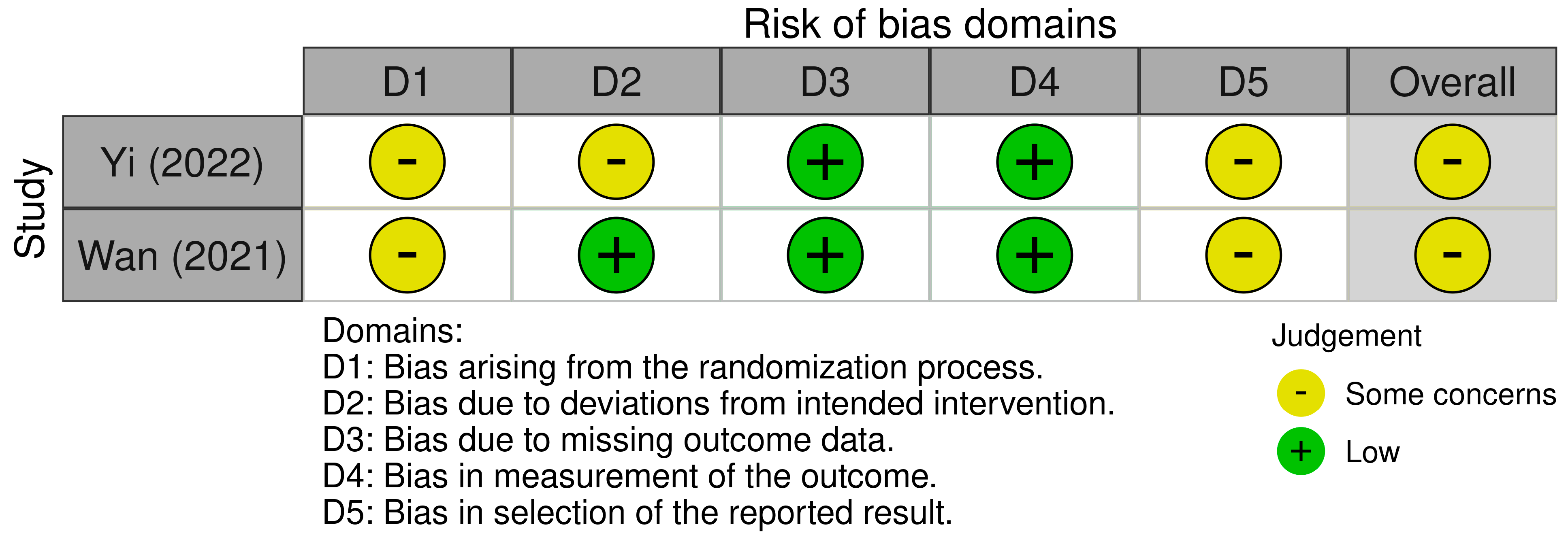
3.3. Risk of Bias of Included Studies
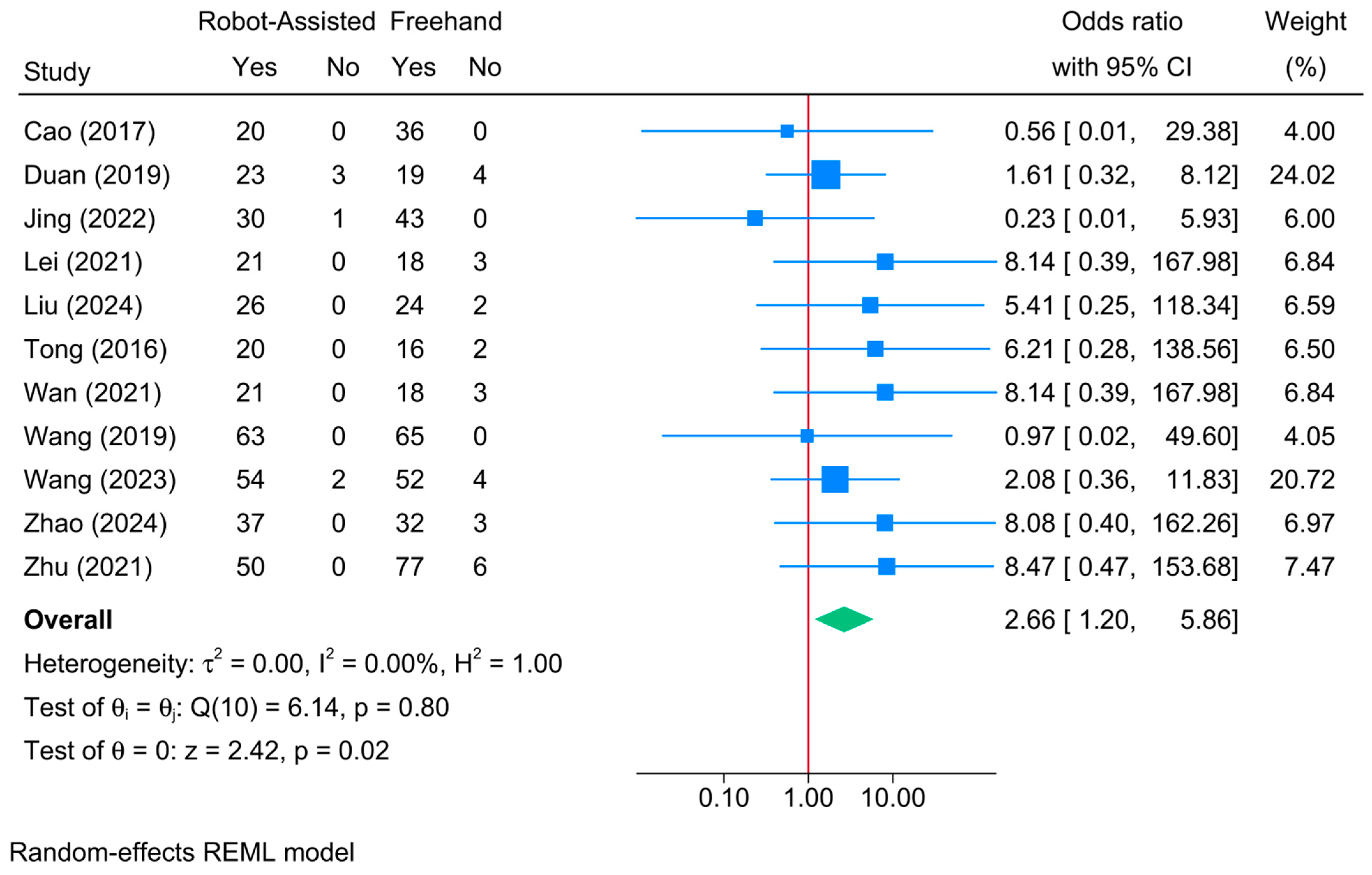
3.4. Union Rate
3.5. Union Time (Days)
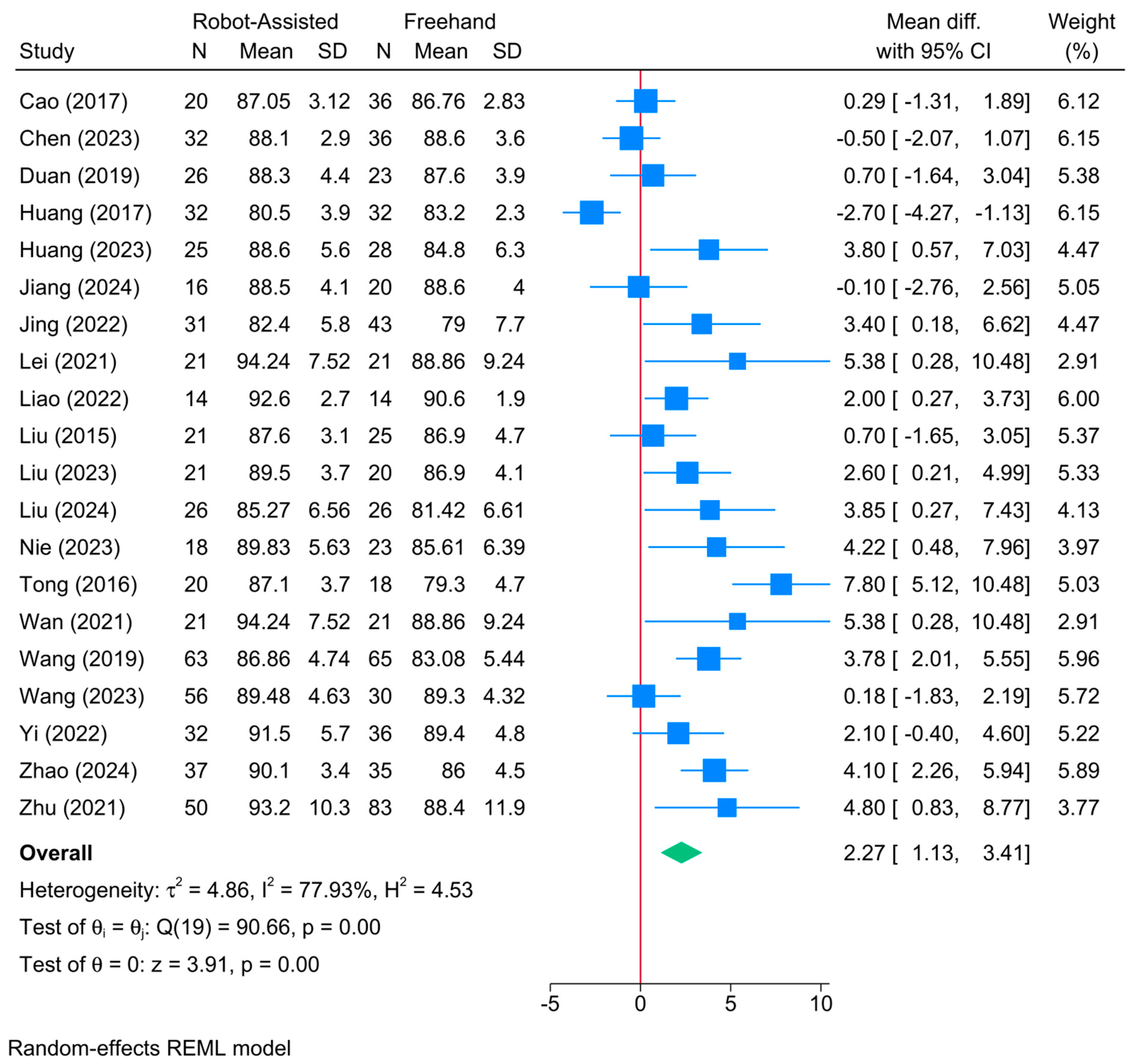
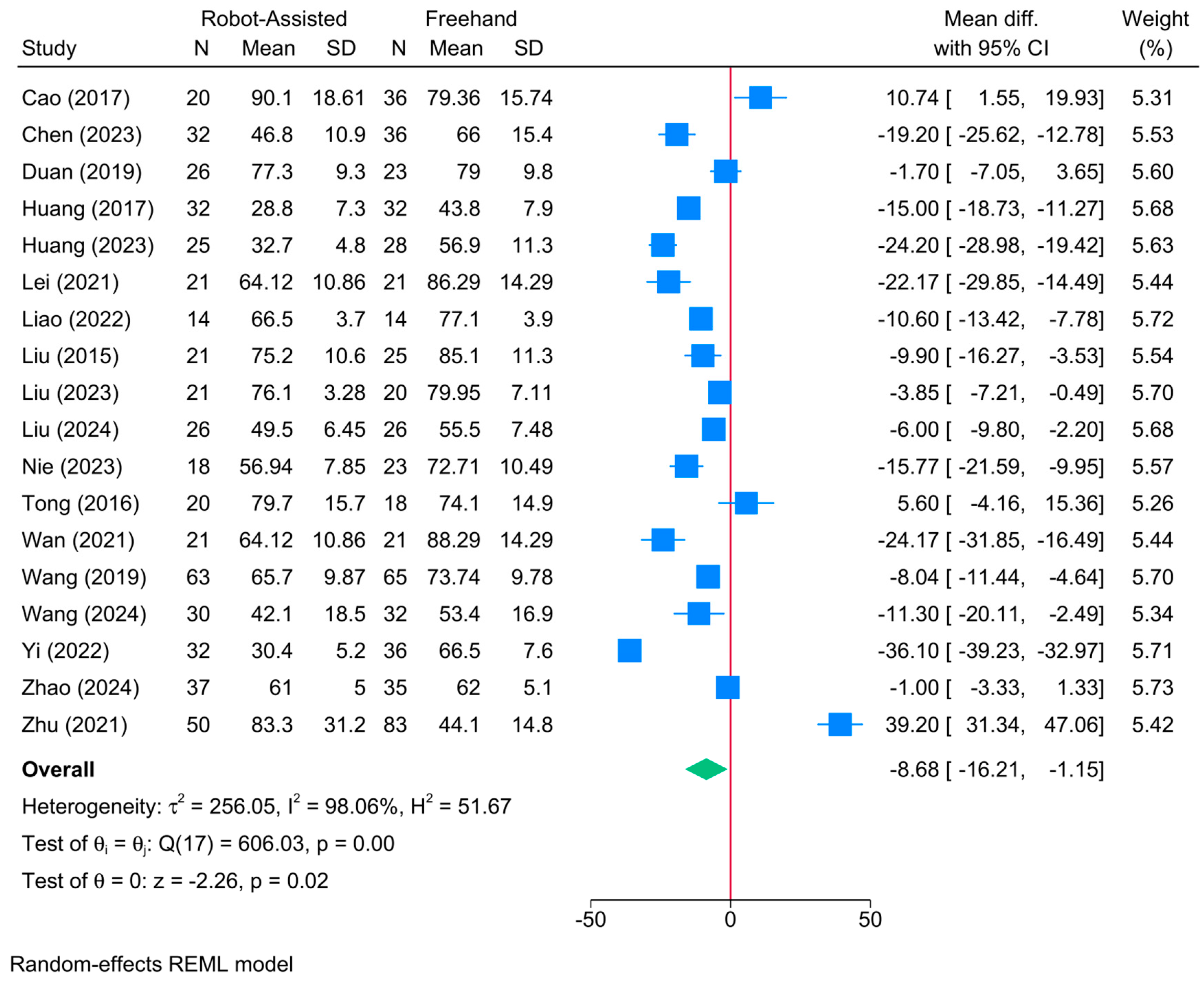
3.6. Harris Score
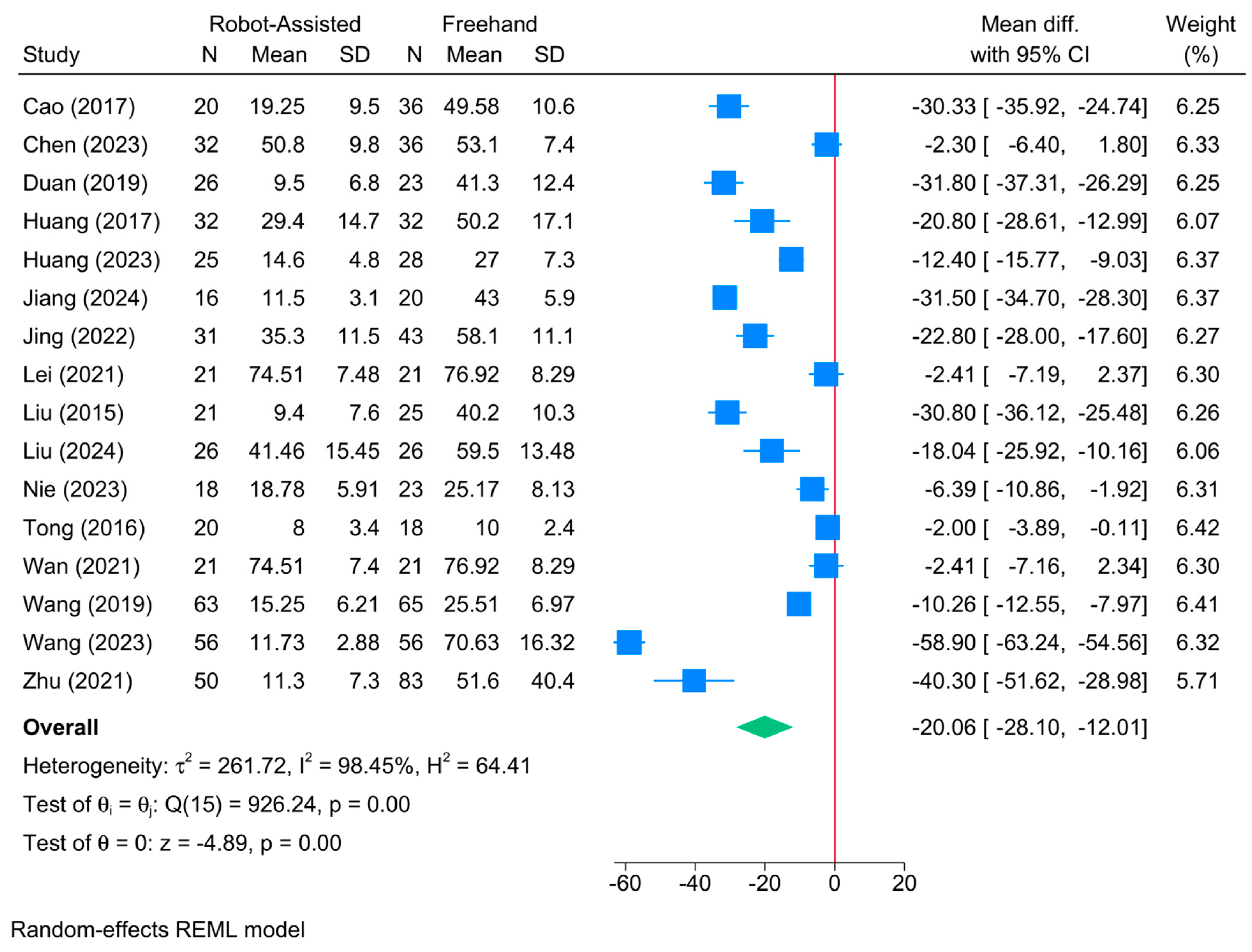
3.7. Operative Time (Mins)
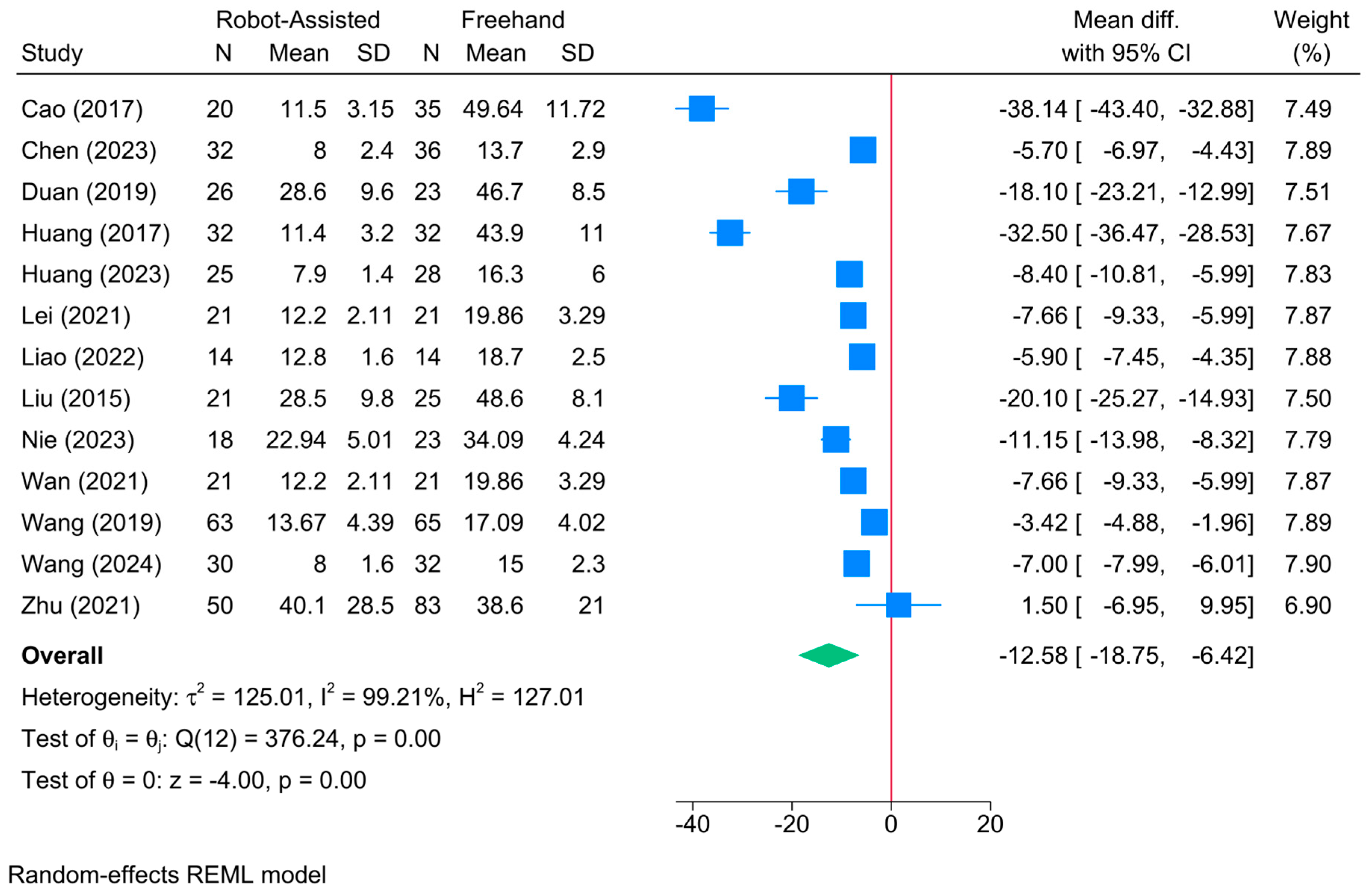
3.8. Frequency of Fluoroscopy
3.9. Intraoperative Fluoroscopy Time (s)
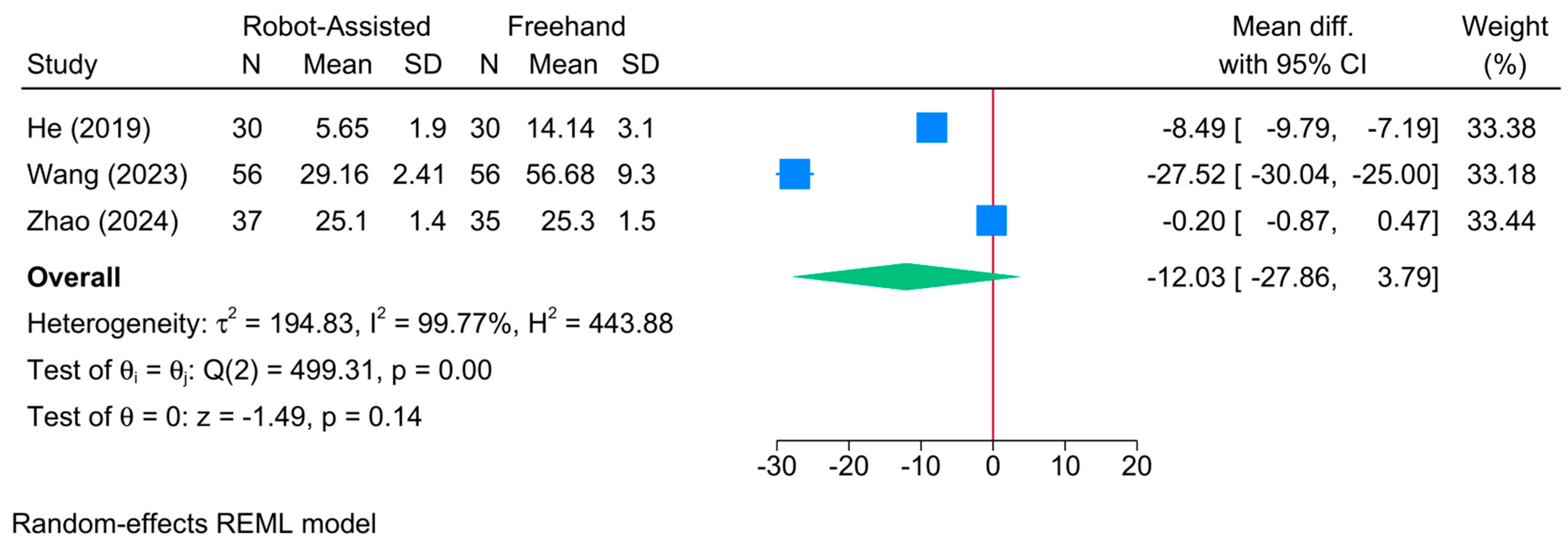
3.10. Frequency of Guide Pin Insertion
3.11. Frequency of Intraoperative Drilling
3.12. Frequency of Guide Pin Adjustment
3.13. Intraoperative Blood Loss (mL)
3.14. Postoperative Hospitalization Time (Day)
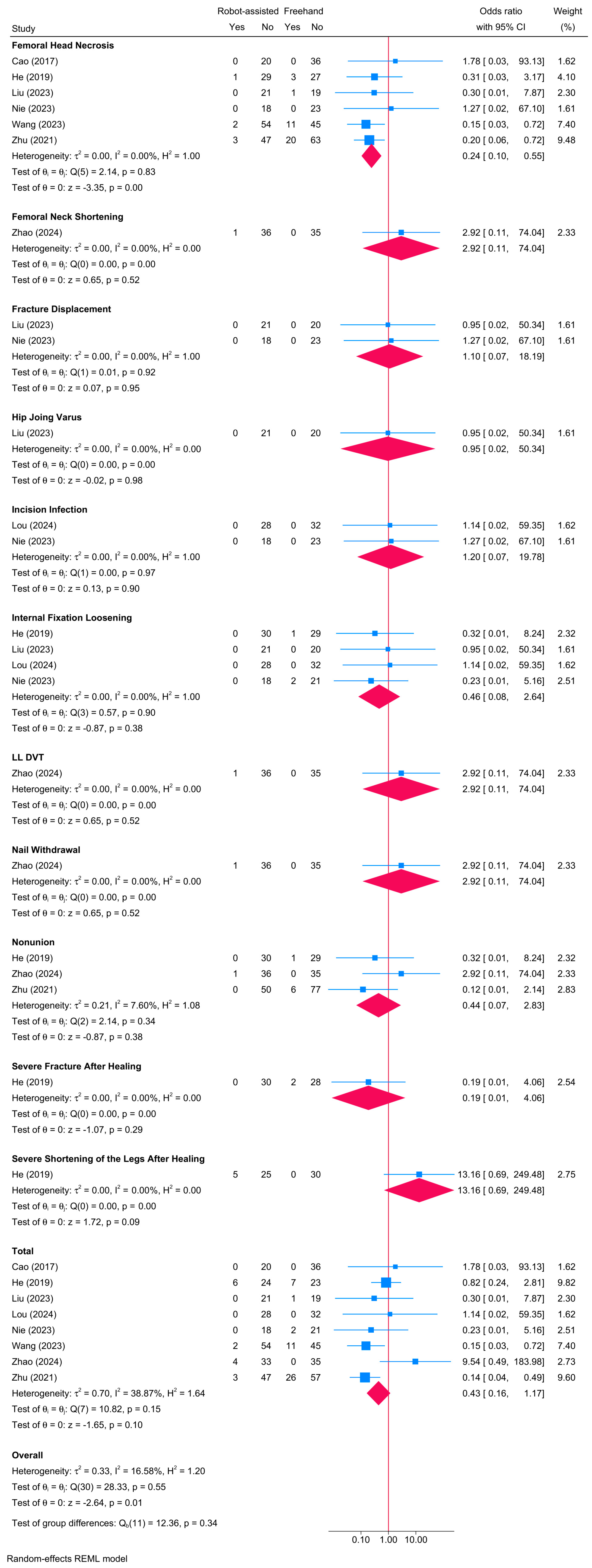
3.15. Postoperative Complications
4. Discussion
4.1. Accuracy of Screw Placement
4.2. Surgical Time and Efficiency
4.3. Postoperative Complications and Recovery
4.4. Patient Outcomes and Satisfaction
4.5. Long-Term Functional Results
4.6. Determinants of Response Based on Meta-Regression
4.7. Surgeon’s Expertise
4.8. Cost Evaluation
4.9. Implications for Clinical Practice
4.10. Study Limitations
4.11. Recommendations for Future Research
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Major, L.J.; North, J.B. Predictors of mortality in patients with femoral neck fracture. J. Orthop. Surg. 2016, 24, 150–152. [Google Scholar] [CrossRef] [PubMed]
- El-Kaissi, S.; Pasco, J.; Henry, M.; Panahi, S.; Nicholson, J.; Nicholson, G.; Kotowicz, M. Femoral neck geometry and hip fracture risk: The Geelong osteoporosis study. Osteoporos. Int. 2005, 16, 1299–1303. [Google Scholar] [CrossRef] [PubMed]
- Karaeminogullari, O.; Demirors, H.; Atabek, M.; Tuncay, C.; Tandogan, R.; Ozalay, M. Avascular necrosis and nonunion after osteosynthesis of femoral neck fractures: Effect of fracture displacement and time to surgery. Adv. Ther. 2004, 21, 335–342. [Google Scholar] [CrossRef]
- Verma, R.; Rigby, A.; Shaw, C.; Mohsen, A. Femoral neck fractures: Does age influence acute hospital stay, delay to surgery, and acute care costs? Orthopedics 2010, 33, 160–165. [Google Scholar] [CrossRef] [PubMed]
- Schmidt-Rohlfing, B.; Heussen, N.; Knobe, M.; Pfeifer, R.; Kaneshige, J.R.; Pape, H.-C. Reoperation rate after internal fixation of intertrochanteric femur fractures with the percutaneous compression plate: What are the risk factors? J. Orthop. Trauma 2013, 27, 312–317. [Google Scholar] [CrossRef]
- Ringel, F.; Stüer, C.; Reinke, A.; Preuss, A.; Behr, M.; Auer, F.; Stoffel, M.; Meyer, B. Accuracy of robot-assisted placement of lumbar and sacral pedicle screws: A prospective randomized comparison to conventional freehand screw implantation. Spine 2012, 37, E496–E501. [Google Scholar] [CrossRef]
- Holmes, C.A.; Edwards, W.T.; Myers, E.R.; Lewallen, D.G.; White, A.A., III; Hayes, W.C. Biomechanics of pin and screw fixation of femoral neck fractures. J. Orthop. Trauma 1993, 7, 242–247. [Google Scholar] [CrossRef]
- Zheng, Y.; Yang, J.; Zhang, F.; Lu, J.; Qian, Y. Robot-assisted vs. freehand cannulated screw placement in femoral neck fractures surgery: A systematic review and meta-analysis. Medicine 2021, 100, e25926. [Google Scholar] [CrossRef]
- Wu, X.B.; Wang, J.Q.; Sun, X.; Han, W. Guidance for the Treatment of Femoral Neck Fracture with Precise Minimally Invasive Internal Fixation Based on the Orthopaedic Surgery Robot Positioning System. Orthop. Surg. 2019, 11, 335–340. [Google Scholar] [CrossRef]
- Li, Y.; Wang, Y.; Dong, B.; Yang, P.; Sun, Y.; Zhou, L.; Shen, J.; Ma, X.; Ma, J. Comparison of rehabilitation outcomes between robot-assisted and freehand screw placement in treatment of femoral neck fractures: A systematic review and meta-analysis. BMC Musculoskelet. Disord. 2024, 25, 208. [Google Scholar] [CrossRef]
- Söylemez, M.S.; Kemah, B.; Poyanli, O. Arthroscopy-Assisted Reduction and Fixation of Femoral Head and Acetabulum Fractures: A Systematic Review of the Literature. Orthop. Surg. 2022, 14, 652–662. [Google Scholar] [CrossRef]
- Duan, S.J.; Liu, H.S.; Wu, W.C.; Yang, K.; Zhang, Z.; Liu, S.D. Robot-assisted percutaneous cannulated screw fixation of femoral neck fractures: Preliminary clinical results. Orthop. Surg. 2019, 11, 34–41. [Google Scholar] [CrossRef] [PubMed]
- Xiao, S.; Fan, L.; Dai, H. Omaha System-based discharge guidance improves knowledge and behavior in Mainland Chinese patients with angina who are not receiving interventional treatment: A randomized controlled trial. Jpn. J. Nurs. Sci. 2019, 16, 355–363. [Google Scholar] [CrossRef] [PubMed]
- Tong, Y.; Luo, X.; Wu, G.; Shi, W. Comparative study on fixation with percutaneous cannulated screws assisted by robot navigation and conventional surgery with manual positioning for femoral neck fractures. Chin. J. Reparative Reconstr. Surg. 2016, 30, 685–689. [Google Scholar]
- Wang, J.-Q.; Zhao, C.-P.; Su, Y.-G.; Li, Z.; Lei, H.; Wang, T.-M.; Wang, M.-Y. Computer-assisted navigation systems for insertion of cannulated screws in femoral neck fractures: A comparison of bi-planar robot navigation with optoelectronic navigation in a Synbone hip model trial. Chin. Med. J. 2011, 124, 3906–3911. [Google Scholar] [PubMed]
- Wang, X.D.; Lan, H.; Li, K.N. Treatment of femoral neck fractures with cannulated screw invasive internal fixation assisted by orthopaedic surgery robot positioning system. Orthop. Surg. 2019, 11, 864–872. [Google Scholar] [CrossRef] [PubMed]
- Chen, J.; Zhou, G.; Chen, X. Robot-assisted percutaneous cannulated screw fixation of femoral neck fracture. Orthop. J. China 2023, 31, 295–299. [Google Scholar] [CrossRef]
- Jiang, S.-H.; Zhang, C.-K.; Jia, F.-T.; Chen, Q.; Xu, M.; Yang, P.-L.; Zhang, Y.-S. Orthopaedic robot assisted closed reduction and cannulated screw internal fixation for the treatment of femoral neck fractures. China J. Orthop. Traumatol. 2024, 37, 119–123. [Google Scholar]
- Liu, G.; Yang, C.; Wang, R.; Tang, J.; Wu, H.; Wei, L.; Hu, J. Application of robot navigation system for insertion of femoral neck system in the treatment of femoral neck fracture. BMC Musculoskelet. Disord. 2024, 25, 47. [Google Scholar] [CrossRef]
- Lou, W.-G.; Chen, J.-M.; Wang, S.-Y.; Li, H.-Y.; Xu, D. Real-time traking and virtual reality technology-assisted trauma orthopaedic surgery robot for femoral neck fractures. China J. Orthop. Traumatol. 2024, 37, 124–128. [Google Scholar]
- Nie, D.-X.; Sun, W.-G.; Wang, X.-Q.; Wang, M.-J.; Sun, J.-B.; Chen, C. Comparison of curative effect between Tianji robot assisted screw placement and traditional cannulated screw internal fixation for femoral neck fracture. China J. Orthop. Traumatol. 2023, 36, 221–225. [Google Scholar]
- Wang, X.; Zhang, Y.; Lou, L.; Xu, L.; Fei, W.; Dai, J.; Wang, J. Robotic-assisted systems for the safe and reliable treatment of femoral neck fractures: Retrospective cohort study. J. Orthop. Surg. Res. 2023, 18, 633. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.-Z.; Chen, Y.-M.; Han, W.; Fei, H.; Zhang, X.; Li, L.; Wang, J.-Q. Orthopaedic robot assisted femoral neck dynamic cross fixation system for the treatment of femoral neck fractures. China J. Orthop. Traumatol. 2024, 37, 114–119. [Google Scholar]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- Muka, T.; Glisic, M.; Milic, J.; Verhoog, S.; Bohlius, J.; Bramer, W.; Chowdhury, R.; Franco, O.H. A 24-step guide on how to design, conduct, and successfully publish a systematic review and meta-analysis in medical research. Eur. J. Epidemiol. 2020, 35, 49–60. [Google Scholar] [CrossRef]
- Abdelaal, A.; Eltaras, M.M.; Katamesh, B.E.; Serhan, H.A.; Farahat, R.A.; Badr, H.; Abdelazeem, B. The prevalence and presentation patterns of microcystic macular oedema: A systematic review and meta-analysis of 2128 glaucomatous eyes. Eye 2023, 37, 3322–3333. [Google Scholar] [CrossRef]
- Amir-Behghadami, M.; Janati, A. Population, Intervention, Comparison, Outcomes and Study (PICOS) design as a framework to formulate eligibility criteria in systematic reviews. Emerg. Med. J. 2020, 37, 387. [Google Scholar] [CrossRef]
- Eldridge, S.; Campbell, M.; Campbell, M.; Dahota, A.; Giraudeau, B.; Higgins, J.; Reeves, B.; Siegfried, N. Revised Cochrane risk of bias tool for randomized trials (RoB 2.0): Additional considerations for cluster-randomized trials. Cochrane Methods Cochrane Database Syst. Rev. 2016, 10, 1–17. [Google Scholar]
- Sedgwick, P. Meta-analyses: Heterogeneity and subgroup analysis. BMJ 2013, 346, f4040. [Google Scholar] [CrossRef]
- Lin, L.; Chu, H. Quantifying publication bias in meta-analysis. Biometrics 2018, 74, 785–794. [Google Scholar] [CrossRef] [PubMed]
- Thompson, S.G.; Higgins, J.P. How should meta-regression analyses be undertaken and interpreted? Stat. Med. 2002, 21, 1559–1573. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.H. Multicollinearity and misleading statistical results. Korean J. Anesthesiol. 2019, 72, 558. [Google Scholar] [CrossRef] [PubMed]
- Cao, Y.; Zhao, Y.; Hu, L.; Li, Z.; Zou, Y.; Lou, S.; Zhang, Y.; Hao, M.; Zhang, H.; Tang, P. Clinical application of computer-assisted cannulated screw internal fixation system based on error correction method for femoral neck fractures. Chin. J. Reparative Reconstr. Surg. 2017, 31, 257–261. [Google Scholar]
- Huang, B.; Rong, S.; LI, J.; Wang, X.; Wei, J.; Zhao, C.; Zhou, L.; Wang, J.; Wang, M. Bi-planar robot navigation for cannulated screw fixation in the treatment of femoral neck fractures. Chin. J. Orthop. 2017, 37, 528–534. [Google Scholar]
- Jing, Y.; Zhang, S.; Han, Z.; Sun, T. Short-term effectiveness of orthopedic robot-assisted femoral neck system fixation for fresh femoral neck fractures. Chin. J. Reparative Reconstr. Surg. 2022, 36, 946–950. [Google Scholar]
- Wan, L.; Zhang, X.; Wu, D.; Li, Z.; Yuan, D.; Li, J.; Zhang, S.; Yue, L. Application of robot positioning for cannulated screw internal fixation in the treatment of femoral neck fracture: Retrospective study. JMIR Med. Inform. 2021, 9, e24164. [Google Scholar] [CrossRef]
- Liao, Y.; Zhang, M.; Xu, J.; Zhang, Y. TiRobot-assisted biplane double-supported screw fixation for femoral neck fractures in middle-aged and young patients. Chin. J. Orthop. Trauma 2022, 12, 1069–1074. [Google Scholar]
- Liu, J.; Liu, L.; Huang, J.; You, W.; Wang, D. Fixation with percutaneous cannulated screws assisted by robot navigation for femoral neck fractures. Zhong Hua Chuang Shang Gu Ke Za Zhi 2015, 17, 692–698. [Google Scholar]
- Liu, Y.; Wang, Z.; Xu, C.; Zhu, Z.; Duan, K.; Guan, J. Early effectiveness of Ti-Robot assisted femoral neck system for minimally invasive treatment of elderly Garden type II and III femoral neck fractures. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi Zhongguo Xiufu Chongjian Waike Zazhi Chin. J. Reparative Reconstr. Surg. 2023, 37, 1471–1476. [Google Scholar]
- Yi, S.; Zhang, D.; Wang, J. Clinical effect evaluation of robot navigation for percutaneous cannulated screw fixation in treatment of femoral neck fractures. Chin. J. Bone Jt. Inj. 2022, 37, 337–341. [Google Scholar] [CrossRef]
- Zhu, Z.D.; Xiao, C.W.; Tan, B.; Tang, X.M.; Wei, D.; Yuan, J.B.; Hu, J.; Feng, L. TiRobot-assisted percutaneous cannulated screw fixation in the treatment of femoral neck fractures: A minimum 2-year follow-up of 50 patients. Orthop. Surg. 2021, 13, 244–252. [Google Scholar] [CrossRef] [PubMed]
- Zhao, X.-L.; Shen, J.-J.; Feng, K.-H.; Chen, Z.-W.; Si, Y.-L.; Zhang, X.; Wang, G.; Hai, X. Comparison of the efficacy of TiRobot orthopaedic robot assisted F screw technique and inverted triangle parallel nail internal fixation in the treatment of unstable femoral neck fractures. Zhongguo Gu Shang China J. Orthop. Traumatol. 2024, 37, 129–134. [Google Scholar]
- Huang, F.; Zhang, X.; Li, W.; Tian, B. Comparison of robot assisted and freehand percutaneous cannulated screwing for femoral neck fractures in the middle aged and young patients. Chin. J. Orthop. Traumatol. 2023, 25, 979–985. [Google Scholar] [CrossRef]
- Bennett, F.S.; Zinar, D.M.; Kilgus, D.J. Ipsilateral hip and femoral shaft fractures. Clin. Orthop. Relat. Res. 1993, 296, 168–177. [Google Scholar] [CrossRef]
- Saeedi-Hosseiny, M.S.; Alruwaili, F.; McMillan, S.; Iordachita, I.; Abedin-Nasab, M.H. A surgical robotic system for long-bone fracture alignment: Prototyping and cadaver study. IEEE Trans. Med. Robot. Bionics 2021, 4, 172–182. [Google Scholar] [CrossRef]
- Karthik, K.; Colegate-Stone, T.; Dasgupta, P.; Tavakkolizadeh, A.; Sinha, J. Robotic surgery in trauma and orthopaedics: A systematic review. Bone Jt. J. 2015, 97, 292–299. [Google Scholar] [CrossRef]
- Ashrafian, H.; Clancy, O.; Grover, V.; Darzi, A. The evolution of robotic surgery: Surgical and anaesthetic aspects. BJA Br. J. Anaesth. 2017, 119, i72–i84. [Google Scholar] [CrossRef]
- Suarez-Ahedo, C.; Lopez-Reyes, A.; Martinez-Armenta, C.; Martinez-Gomez, L.E.; Martinez-Nava, G.A.; Pineda, C.; Vanegas-Contla, D.R.; Domb, B. Revolutionizing orthopedics: A comprehensive review of robot-assisted surgery, clinical outcomes, and the future of patient care. J. Robot. Surg. 2023, 17, 2575–2581. [Google Scholar] [CrossRef]
- Ramkumar, P.N.; Navarro, S.M.; Chughtai, M.; La, T., Jr.; Fisch, E.; Mont, M.A. The patient experience: An analysis of orthopedic surgeon quality on physician-rating sites. J. Arthroplast. 2017, 32, 2905–2910. [Google Scholar] [CrossRef]
- Adili, A. Robot-assisted orthopedic surgery. In Seminars in Laparoscopic Surgery; Sage Publications: Thousand Oaks, CA, USA, 2004; pp. 89–98. [Google Scholar]
- Ali, M.; Phillips, D.; Kamson, A.; Nivar, I.; Dahl, R.; Hallock, R. Learning curve of robotic-assisted total knee arthroplasty for non-fellowship-trained orthopedic surgeons. Arthroplast. Today 2022, 13, 194–198. [Google Scholar] [CrossRef]
- Innocenti, B.; Bori, E. Robotics in orthopaedic surgery: Why, what and how? Arch. Orthop. Trauma Surg. 2021, 141, 2035–2042. [Google Scholar] [CrossRef]
- Schreuder, H.W.; Wolswijk, R.; Zweemer, R.P.; Schijven, M.P.; Verheijen, R.H. Training and learning robotic surgery, time for a more structured approach: A systematic review. BJOG Int. J. Obstet. Gynaecol. 2012, 119, 137–149. [Google Scholar] [CrossRef]






| Author (YOP) | Country | Robot | Design | FU (mo) | Age | Sample | Gender (M/F) | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| RA | FH | RA | FH | Total | RA | FH | |||||
| Cao (2017) [33] | China | Universal Robots | RCS | 14.7 | 44.7 | 47.9 | 20 | 36 | 56 | 10/10 | 19/17 |
| Chen (2023) [17] | China | TiRobot | RCS | 31.4 | 43.6 (13.7) | 45.7 (12.7) | 32 | 36 | 68 | 18/14 | 17/19 |
| Duan (2019) [12] | China | TiRobot | RCS | 13.6 | 61.7 (5.2) | 62.1 (4.1) | 26 | 23 | 49 | 11/15 | 9/14 |
| He (2019) [13] | China | Bi-planar robot | RCS | 24 | 56 (11.1) | 56.2 (9.13) | 30 | 30 | 60 | 11/19 | 12/18 |
| Huang (2017) [34] | China | Bi-planar robot | RCS | 19.6 | 59.4 (5.6) | 59.1 (4.9) | 32 | 32 | 64 | 10/22 | 12/20 |
| Huang (2023) [44] | China | TiRobot Advance | RCS | 22.2 | 48.2 (11.9) | 48.5 (9.8) | 25 | 28 | 53 | 11/14 | 12/16 |
| Jiang (2024) [18] | China | TiRobot | RCS | 15.6 | 53.61 (5.45) | 55.23 (4.64) | 16 | 20 | 36 | 7/9 | 8/12 |
| Jing (2022) [35] | China | TiRobot | RCS | 7 | 55.2 | 55 | 31 | 43 | 74 | 11/20 | 14/29 |
| Lei (2021) [36] | China | TiRobot | RCS | 6 | 51.86 (4.89) | 51.33 (4.3) | 21 | 21 | 42 | 12/9 | 14/7 |
| Liao (2022) [37] | China | TiRobot | RCS | 8 | 44.1 (8.7) | 48.8 (8) | 14 | 14 | 28 | 6/8 | 7/7 |
| Liu (2015) [38] | China | GD-2000 | RCS | 12.5 | 65.2 (4.2) | 60.5 (5.1) | 21 | 25 | 46 | 8/13 | 11/14 |
| Liu (2023) [39] | China | TiRobot | RCS | 24 | 71.3 | 73.2 | 21 | 20 | 41 | 10/11 | 8/12 |
| Liu (2024) [19] | China | TiRobot | RCS | 12 | 51.92 (6.41) | 50.08 (8.41) | 26 | 26 | 52 | 17-Sep | 11/15 |
| Lou (2024) [20] | China | Tianji Robot | RCS | 13 | 46.2 (9.3) | 48.2 (7.8) | 28 | 32 | 60 | 12/16 | 15/17 |
| Nie (2023) [21] | China | TiRobot | RCS | 14.9 | 56 (4.22) | 54.87 (4.81) | 18 | 23 | 41 | 8/10 | 10/13 |
| Tong (2016) [14] | China | TiRobot | RCS | 18 | 47.5 | 51.5 | 20 | 18 | 38 | 12/8 | 11/7 |
| Wan (2021) [40] | China | Tianji Robot | RCT | 6 | 51.86 (4.89) | 51.33 (4.3) | 21 | 21 | 42 | 12/9 | 14/7 |
| Wang (2011) [15] | China | Bi-planar robot | RCS | - | - | - | 6 | 6 | 12 | - | - |
| Wang (2019) [16] | China | TiRobot | RCS | 12 | 49.03 (8.23) | 49.8 (7.68) | 63 | 65 | 128 | 30/33 | 31/34 |
| Wang (2023) [22] | China | TiRobot | RCS | 12 | 59.5 (8.7) | 60.1 (8.2) | 56 | 56 | 112 | 32/34 | 30/36 |
| Wang (2024) [23] | China | TiRobot | RCS | 6 | 41.95 (5.39) | 40.8 (5.08) | 30 | 32 | 62 | - | - |
| Yi (2022) [41] | China | TINAVI | RCT | 18 | 58.5 (6.3) | 57.5 (5.3) | 32 | 36 | 68 | 19/13 | 16/20 |
| Zhao (2024) [43] | China | TiRobot | RCS | 12 | 53.87 (5.28) | 52.36 (5.05) | 37 | 35 | 72 | 16/21 | 13/22 |
| Zhu (2021) [42] | China | TiRobot | RCS | 38.8 | 47.9 (13.5) | 47.7 (12.6) | 50 | 83 | 133 | 26/24 | 47/36 |
| Coefficient | SE | Z | P | Low CI | High CI | |
|---|---|---|---|---|---|---|
| Union rate | ||||||
| Universal Robots | −2.54082 | 2.304537 | −1.1 | 0.27 | −7.05764 | 1.975986 |
| Tianji Robot | 0.93305 | 1.775284 | 0.53 | 0.599 | −2.54644 | 4.412544 |
| Follow-up (month) | 0.043397 | 0.065153 | 0.67 | 0.505 | −0.0843 | 0.171095 |
| Sample size | −0.00764 | 0.014116 | −0.54 | 0.588 | −0.03531 | 0.020026 |
| Mean age (year) | −0.07405 | 0.089556 | −0.83 | 0.408 | −0.24958 | 0.101473 |
| R2 = 0%; I2 = 0% | ||||||
| Union Time (days) | ||||||
| Bi-planar robot | −0.902 | 12.397 | −0.070 | 0.942 | −25.199 | 23.395 |
| Universal Robots | 13.861 | 20.143 | 0.690 | 0.491 | −25.620 | 53.341 |
| GD-2000 Robot | −15.649 | 25.399 | −0.620 | 0.538 | −65.430 | 34.132 |
| Tianji Robot | 0.446 | 5.416 | 0.080 | 0.934 | −10.169 | 11.062 |
| TiRobot Advance | −21.236 | 16.661 | −1.270 | 0.202 | −53.890 | 11.418 |
| Follow-up (month) | 1.113 | 0.709 | 1.570 | 0.116 | −0.277 | 2.503 |
| Sample size | −0.351 | 0.173 | −2.020 | 0.043 | −0.690 | −0.011 |
| Mean age (year) | 0.027 | 0.577 | 0.050 | 0.963 | −1.105 | 1.159 |
| R2 = 100%; I2 = 0% | ||||||
| Harris Score | ||||||
| Bi-planar robot | −2.884 | 2.129 | −1.350 | 0.175 | −7.056 | 1.288 |
| Universal Robots | −3.031 | 2.850 | −1.060 | 0.288 | −8.617 | 2.556 |
| GD-2000 | −1.587 | 3.096 | −0.510 | 0.608 | −7.654 | 4.481 |
| Tianji Robot | 2.153 | 3.778 | 0.570 | 0.569 | −5.252 | 9.558 |
| TiRobot Advance | 0.935 | 3.162 | 0.300 | 0.767 | −5.262 | 7.133 |
| Follow-up (month) | −0.035 | 0.090 | −0.390 | 0.695 | −0.211 | 0.141 |
| Sample size | 0.001 | 0.023 | 0.050 | 0.961 | −0.044 | 0.046 |
| Mean age (year) | −0.054 | 0.103 | −0.520 | 0.601 | −0.255 | 0.148 |
| R2 = 0%; I2 = 78.86% | ||||||
| Operative Time (min) | ||||||
| Bi-planar robot | −24.266 | 10.722 | −2.260 | 0.024 | −45.280 | −3.251 |
| Universal Robots | 18.863 | 14.914 | 1.260 | 0.206 | −10.367 | 48.094 |
| GD-2000 | −1.844 | 15.550 | −0.120 | 0.906 | −32.323 | 28.634 |
| Tianji Robot | −8.777 | 14.779 | −0.590 | 0.553 | −37.743 | 20.188 |
| TiRobot Advance | −21.372 | 14.532 | −1.470 | 0.141 | −49.856 | 7.111 |
| Follow-up (month) | 0.698 | 0.458 | 1.530 | 0.127 | −0.199 | 1.595 |
| Sample size | 0.167 | 0.139 | 1.200 | 0.230 | −0.106 | 0.440 |
| Mean age (year) | 0.160 | 0.508 | 0.310 | 0.753 | −0.836 | 1.156 |
| R2 = 33.43%; I2 = 97.13% | ||||||
| Frequency of Fluroscopy | ||||||
| Bi-planar robot | −20.472 | 3.989 | −5.130 | 0.000 | −28.290 | −12.655 |
| Universal Robots | −32.172 | 3.941 | −8.160 | 0.000 | −39.896 | −24.447 |
| GD-2000 | −4.283 | 4.806 | −0.890 | 0.373 | −13.702 | 5.137 |
| Tianji Robot | 2.493 | 3.095 | 0.810 | 0.421 | −3.574 | 8.559 |
| TiRobot Advance | −0.787 | 3.234 | −0.240 | 0.808 | −7.125 | 5.552 |
| Follow-up (month) | 0.014 | 0.113 | 0.130 | 0.898 | −0.207 | 0.236 |
| Sample size | 0.060 | 0.033 | 1.830 | 0.068 | −0.004 | 0.124 |
| Mean age (year) | −0.450 | 0.175 | −2.570 | 0.010 | −0.792 | −0.107 |
| R2 = 94.67%; I2 = 85.30% | ||||||
| Frequency of Guide Pin Insertion | ||||||
| Bi-planar robot | −3.126 | 3.980 | −0.790 | 0.432 | −10.927 | 4.675 |
| Universal Robots | −7.283 | 3.637 | −2.000 | 0.045 | −14.411 | −0.155 |
| GD-2000 | 4.888 | 4.797 | 1.020 | 0.308 | −4.515 | 14.291 |
| TiRobot Advance | 0.913 | 3.127 | 0.290 | 0.770 | −5.216 | 7.041 |
| Follow-up (month) | −0.202 | 0.180 | −1.120 | 0.262 | −0.556 | 0.151 |
| Sample size | 0.013 | 0.039 | 0.340 | 0.738 | −0.063 | 0.089 |
| Mean age (year) | −0.503 | 0.263 | −1.910 | 0.056 | −1.018 | 0.013 |
| R2 = 44.45%; I2 = 92.81% | ||||||
| Intraoperative Blood Loss (mL) | ||||||
| Bi-planar robot | 21.287 | 14.230 | 1.500 | 0.135 | −6.604 | 49.179 |
| Universal Robots | −37.713 | 14.017 | −2.690 | 0.007 | −65.186 | −10.241 |
| GD-2000 | 18.924 | 15.664 | 1.210 | 0.227 | −11.777 | 49.625 |
| Tianji Robot | 1.532 | 13.189 | 0.120 | 0.908 | −24.318 | 27.381 |
| TiRobot Advance | −4.107 | 12.578 | −0.330 | 0.744 | −28.760 | 20.546 |
| Follow-up (month) | −0.789 | 0.487 | −1.620 | 0.105 | −1.744 | 0.165 |
| Sample size | −0.225 | 0.106 | −2.110 | 0.035 | −0.433 | −0.016 |
| Mean age (year) | −2.980 | 0.826 | −3.610 | 0.000 | −4.598 | −1.362 |
| R2 = 51.16%; I2 = 96.49% | ||||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mert, Ü.; Mahmoud, M.A.; Ghandour, M.; Al Zuabi, A.; Speicher, M.; Kobbe, P.; Horst, K.; Hildebrand, F.; Kabir, K. Comparative Efficacy and Safety of Robot-Assisted vs. Freehand Screw Placement in Femoral Neck Fractures: An Updated Systematic Review and Meta-Analysis. J. Clin. Med. 2024, 13, 5072. https://doi.org/10.3390/jcm13175072
Mert Ü, Mahmoud MA, Ghandour M, Al Zuabi A, Speicher M, Kobbe P, Horst K, Hildebrand F, Kabir K. Comparative Efficacy and Safety of Robot-Assisted vs. Freehand Screw Placement in Femoral Neck Fractures: An Updated Systematic Review and Meta-Analysis. Journal of Clinical Medicine. 2024; 13(17):5072. https://doi.org/10.3390/jcm13175072
Chicago/Turabian StyleMert, Ümit, Mohamad Agha Mahmoud, Maher Ghandour, Ahmad Al Zuabi, Marco Speicher, Philipp Kobbe, Klemens Horst, Frank Hildebrand, and Koroush Kabir. 2024. "Comparative Efficacy and Safety of Robot-Assisted vs. Freehand Screw Placement in Femoral Neck Fractures: An Updated Systematic Review and Meta-Analysis" Journal of Clinical Medicine 13, no. 17: 5072. https://doi.org/10.3390/jcm13175072






