Hand Digit Revascularization: Could Be an “Elective-Urgence” Surgery?
Abstract
:1. Introduction
2. Detailed Case Description
2.1. Patient History and Initial Presentation
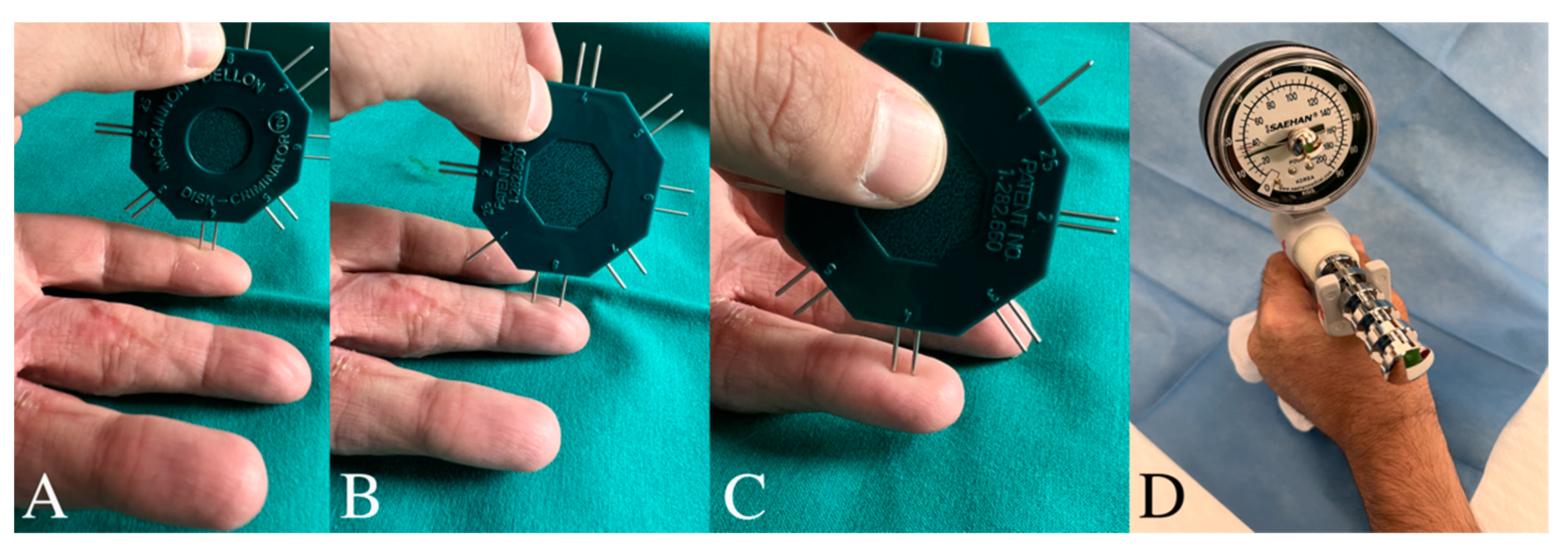
2.2. Clinical Examination
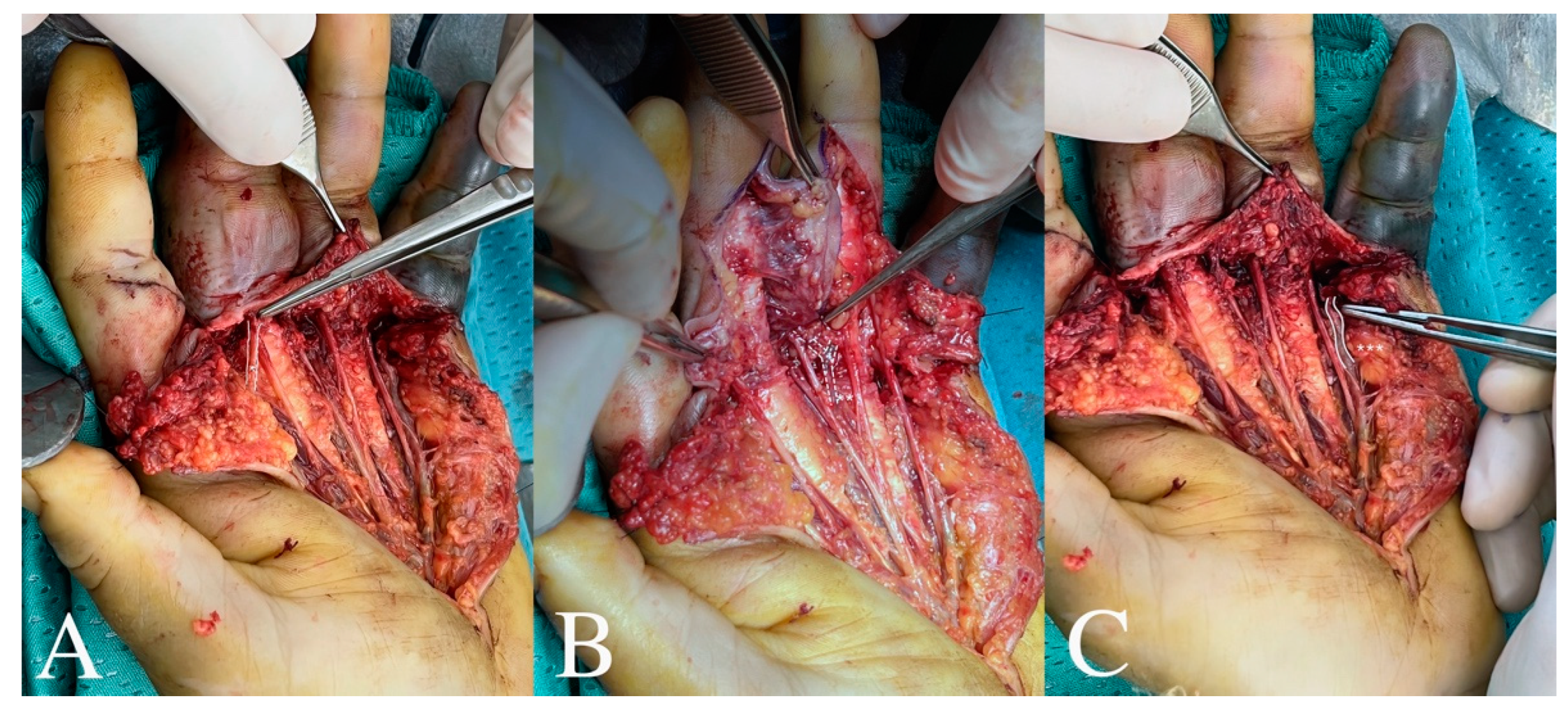
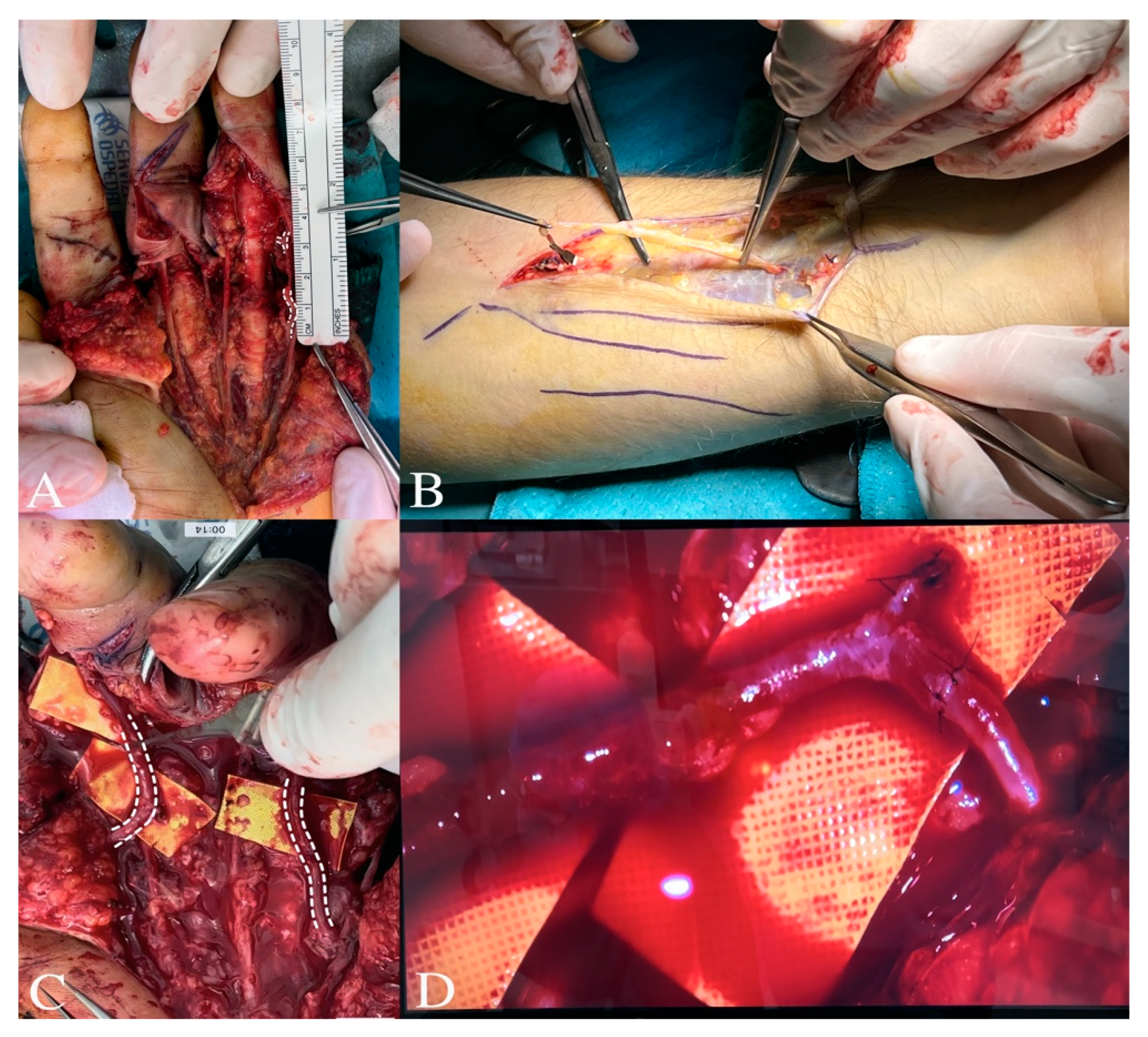
2.3. Surgery
2.4. Follow-Up and Outcome
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Hayhurst, J.W.; O’Brien, B.M.C.; Ishida, H.; Baxter, T.J. Experimental digital replantation after prolonged cooling. Hand 1974, 6, 134–141. [Google Scholar] [CrossRef]
- Wei, F.C.; Chang, Y.L.; Chen, H.C.; Chuang, C.C. Three successful digital replantations in a patient after 84, 86, and 94 hours of cold ischemia time. Plast. Reconstr. Surg. 1988, 82, 346–350. [Google Scholar] [CrossRef] [PubMed]
- Gierej, P.; Radziszewski, M.; Krzesniak, N.E. Microsurgical Revascularization of Two Fingers after Prolonged (52 and 53 Hours) Warm Ischemia Time: Case Report and Literature Review. Clin. Surg. 2021, 6, 3366. [Google Scholar]
- Baek, S.M.; Kim, S.S.; Tsai, T.M.; McCabe, S.; Firrell, J. Successful digital replantation after 42 hours of warm ischemia. J. Reconstr. Microsurg. 1992, 8, 455–459. [Google Scholar] [CrossRef]
- May, J.M., Jr.; Hergrueter, C.A.; Hansen, R.H. Seven-digit replantation: Digit survival after 39 hours of cold ischemia. Plast. Reconstr. Surg. 1986, 78, 522–525. [Google Scholar] [CrossRef]
- Chiu, H.Y.; Chen, M.T. Revascularization of digits after thirty-three hours of warm ischemia time: A case report. J. Hand Surg. Am. 1984, 9, 63–67. [Google Scholar] [CrossRef] [PubMed]
- Inoue, G.; Nakamura, R.; Imamura, T. Revascularization of digits after prolonged warm ischemia. J. Reconstr. Microsurg. 1988, 4, 131–135. [Google Scholar] [CrossRef]
- Seo, T.; Matsuda, M. A case of replantation of a completely amputated digit after 26 hours of warm ischemia. J. Reconstr. Microsurg. 1987, 3, 143–146. [Google Scholar] [CrossRef]
- Chung, K.C.; Pillsbury, M.S.; Walters, M.R.; Hayward, R.A. Reliability and validity testing of the Michigan Hand Outcomes Questionnaire. J. Hand Surg. 1998, 23, 575–587. [Google Scholar] [CrossRef]
- Chung, K.C.; Hamill, J.B.; Walters, M.R.; Hayward, R.A. The Michigan Hand Outcomes Questionnaire (MHQ) after carpal tunnel release: Responsiveness and its relationship to symptoms and functional status. J. Hand Surg. 1999, 24, 73–82. [Google Scholar]
- Fess, E.E. Grip strength. In Clinical Assessment Recommendations, 2nd ed.; Casanova, J., Ed.; American Society of Hand Therapists: Mount Laurel, NJ, USA, 1992; pp. 41–45. [Google Scholar]
- Mathiowetz, V.; Weber, K.; Volland, G.; Kashman, N. Reliability and validity of grip and pinch strength evaluations. J. Hand Surg. 1994, 9, 222–226. [Google Scholar] [CrossRef]
- Huskisson, E.C. Measurement of pain. Lancet 1974, 304, 1127–1131. [Google Scholar] [CrossRef] [PubMed]
- Collins, S.L.; Moore, R.A.; McQuay, H.J. The visual analogue pain intensity scale: What is moderate pain in millimetres? Pain 1997, 72, 95–97. [Google Scholar] [CrossRef] [PubMed]
- Weber, E.H. De Tactu: Anatomia et Physiologia. In Annotationes Anatomicae et Physiologicae; Prostat apud C.F. Koehler: Lipsiae, Germany, 1835. [Google Scholar]
- Dellon, A.L. Evaluation of Sensibility and Re-Education of Sensation in the Hand; Williams & Wilkins: Philadelphia, PA, USA, 1981. [Google Scholar]
- Kleinert, H.E.; Verdan, C. Report of the Committee on Tendon Injuries (International Federation of Societies for Surgery of the Hand). J. Hand Surg. Am. 1983, 8 Pt 2, 794–798. [Google Scholar] [CrossRef] [PubMed]
- Woo, S.H.; Lee, Y.K.; Chong, S.W.; Cheon, H.J.; Kim, Y.W. The fate of delayed revascularization for neglected vascular injury of incompletely amputated digits and hands. J. Hand Surg. 2019, 44, 1026–1030. [Google Scholar] [CrossRef]
- Iglesias, M.; Serrano, A. Replantation of amputated segments after prolonged ischemia. Plast. Reconstr. Surg. 1990, 85, 425–429. [Google Scholar] [CrossRef]
- Yu, H.; Wei, L.; Liang, B.; Hou, S.; Wang, J.; Yang, Y. Nonsurgical factors of digital replantation and survival rate: A metaanalysis. Indian. J. Orthop. 2015, 49, 265–271. [Google Scholar] [CrossRef]
- Li, J.; Guo, Z.; Zhu, Q.; Wei, L.; Han, Y.; Li, M.; Wang, Z. Fingertip replantation: Determinants of survival. Plast. Reconstr. Surg. 2008, 122, 833–839. [Google Scholar] [CrossRef]
- Shaterian, A.; Rajaii, R.; Kanack, M.; Evans, G.; Leis, A. Predictors of Digit Survival following Replantation: Quantitative Review and Meta-Analysis. J. Hand Microsurg. 2018, 10, 66–73. [Google Scholar] [CrossRef]
- Zhu, X.; Zhu, H.; Zhang, C.; Zheng, X. Pre-operative predictive factors for the survival of replanted digits. Int. Orthop. 2017, 41, 1623–1626. [Google Scholar] [CrossRef]
- Dec, W. A meta-analysis of success rates for digit replantation. Tech. Hand Extrem. Surg. 2006, 10, 124–129. [Google Scholar] [CrossRef] [PubMed]
- Tejedor Navarro, A.; Vendrell Jordà, M.; Puente Alonso, C. Digital replantation/revascularization: Predictive factors to microsurgery success—A single-center study. Eur. J. Trauma. Emerg. Surg. 2021, 47, 225–232. [Google Scholar] [CrossRef] [PubMed]
- Woo, S.H.; Cheon, H.J.; Kim, Y.W.; Kang, D.H.; Nam, H.J. Delayed and suspended replantation for complete amputation of digits and hands. J. Hand Surg. Am. 2015, 40, 883–889. [Google Scholar] [CrossRef]
- Cavadas, P.; Rubí, C.; Thione, A.; Perez-Espadero, A. Immediate versus overnight-delayed digital replantation: Comparative retrospective cohort study of survival outcomes. J. Hand Surg. Am. 2018, 43, 625–630. [Google Scholar] [CrossRef] [PubMed]



| MHQ | T1 | T6 | T12 |
|---|---|---|---|
| How well did your hand(s) work during the past week? | |||
| (Function: 1 very good to 5 very poor) | 5 | 3 | 1 |
| How was the sensation (feeling) in your hand(s) during the past week? | |||
| (Function: 1 very good to 5 very poor) | 5 | 3 | 1 |
| How difficult was it for you to hold a frying pain during the last week? | |||
| (Daily activities: 1 not at all difficult to 5 very difficult) | 5 | 3 | 1 |
| How difficult was it for you to button a shirt or blouse during the past week? | |||
| (Daily activities: 1 not at all difficult to 5 very difficult) | 5 | 3 | 1 |
| In the past 4 weeks, how often were you unable to do your work because of problems with your hand(s)/wrist(s) | |||
| (Work activities: 1 always to 5 never) | 3 | 2 | 1 |
| In the past 4 weeks, how often did you take longer to do tasks in your work because of problems with your hand(s)/wrist(s) | |||
| (Work activities: 1 always to 5 never) | 4 | 3 | 1 |
| How often did the pain in your hand(s)/wrist(s) interfere with your daily activities? | |||
| (Pain: 1 very mild to 5 very severe) | 4 | 1 | 1 |
| Describe the pain in your hand(s)/wrist(s) in the past week | |||
| (Pain: 1 very mild to 5 very severe) | 4 | 1 | 1 |
| I am satisfied with the look of my hands | |||
| (Aesthetics: 1 strongly agree to 5 strongly disagree) | 3 | 3 | 3 |
| The appearance of my hands interferes with my normal daily activities | |||
| (Aesthetics: 1 strongly agree to 5 strongly disagree) | 5 | 5 | 5 |
| In the past week, how satisfied were you with the motion of your fingers? | |||
| (Satisfaction: 1 very satisfied to 5 very dissatisfied) | 4 | 3 | 1 |
| In the past week, how satisfied were you with the motion of your wrist? | |||
| (Satisfaction: 1 very satisfied to 5 very dissatisfied) | 2 | 1 | 1 |
| Total | 49 | 31 | 18 |
| Clinical Examination Test | T1 | T6 | T12 |
|---|---|---|---|
| Weber Test | >15 mm | 8 mm | 4 mm |
| Jamar Score | 5 kg | 12 kg | 24 kg |
| Visual Analog Scale (VAS) score | 7 | 2 | 2 |
| TAM | 30° | 190° | 250° |
| %ROM | Poor | good | excellent |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
De Francesco, F.; Mani, O.; Gravina, P.; Riccio, M. Hand Digit Revascularization: Could Be an “Elective-Urgence” Surgery? J. Clin. Med. 2024, 13, 5120. https://doi.org/10.3390/jcm13175120
De Francesco F, Mani O, Gravina P, Riccio M. Hand Digit Revascularization: Could Be an “Elective-Urgence” Surgery? Journal of Clinical Medicine. 2024; 13(17):5120. https://doi.org/10.3390/jcm13175120
Chicago/Turabian StyleDe Francesco, Francesco, Olimpia Mani, Pasquale Gravina, and Michele Riccio. 2024. "Hand Digit Revascularization: Could Be an “Elective-Urgence” Surgery?" Journal of Clinical Medicine 13, no. 17: 5120. https://doi.org/10.3390/jcm13175120







