Investigation of Relationship between Hemodynamic and Morphometric Characteristics of Aortas in Pediatric Patients
Abstract
1. Introduction
2. Materials and Methods
2.1. Patients, MSCT Data Evaluation and Morphometric Features Extraction
2.1.1. Subjects and Data Collection
2.1.2. MSCT Data Evaluation
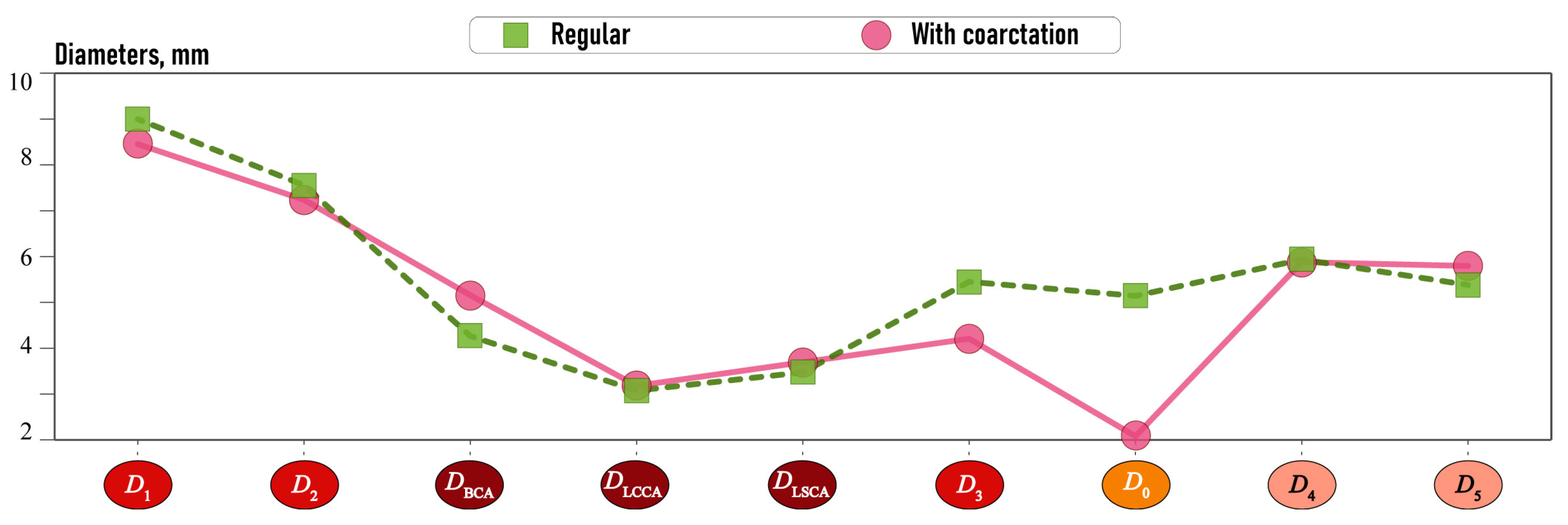
2.1.3. Morphometric Features
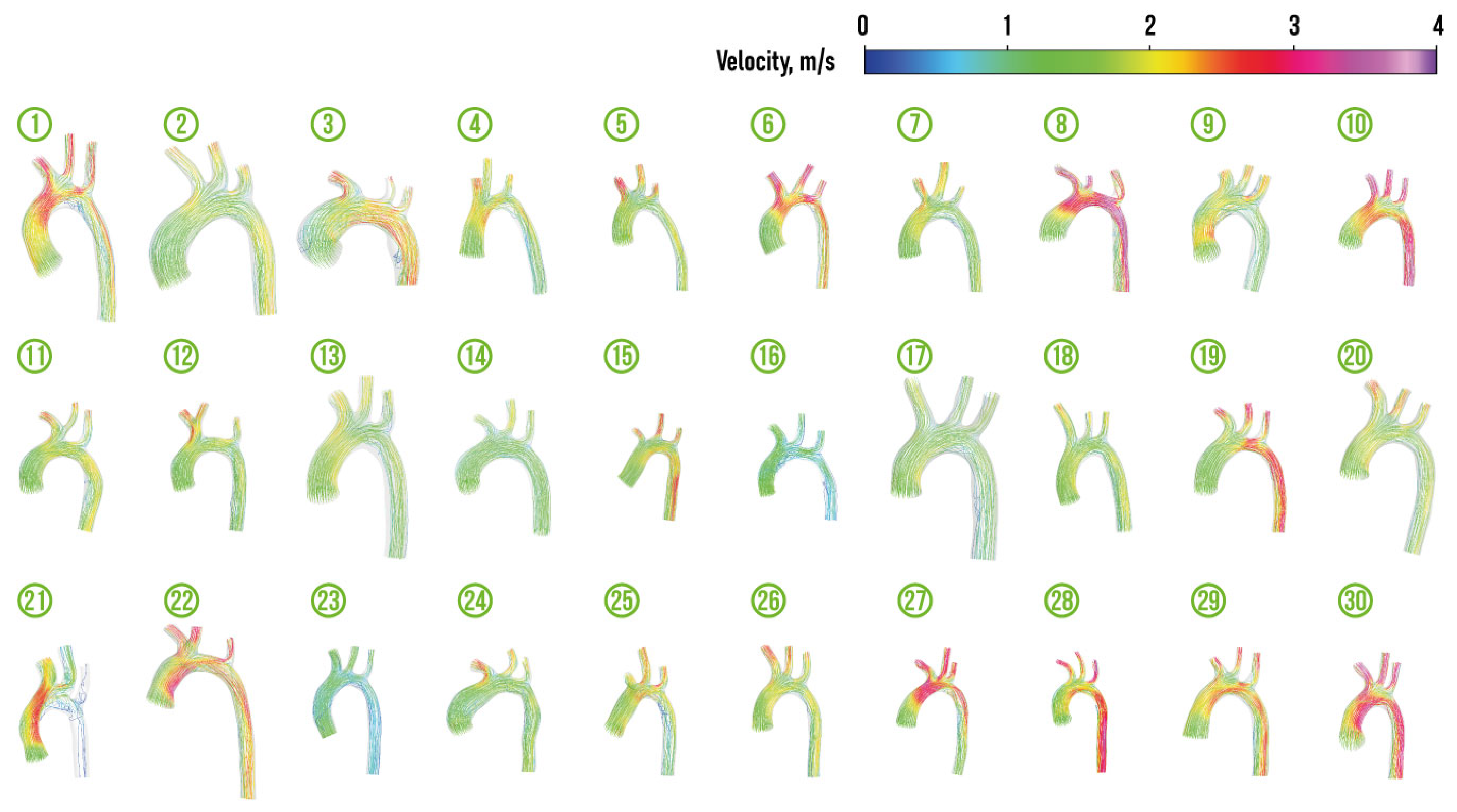
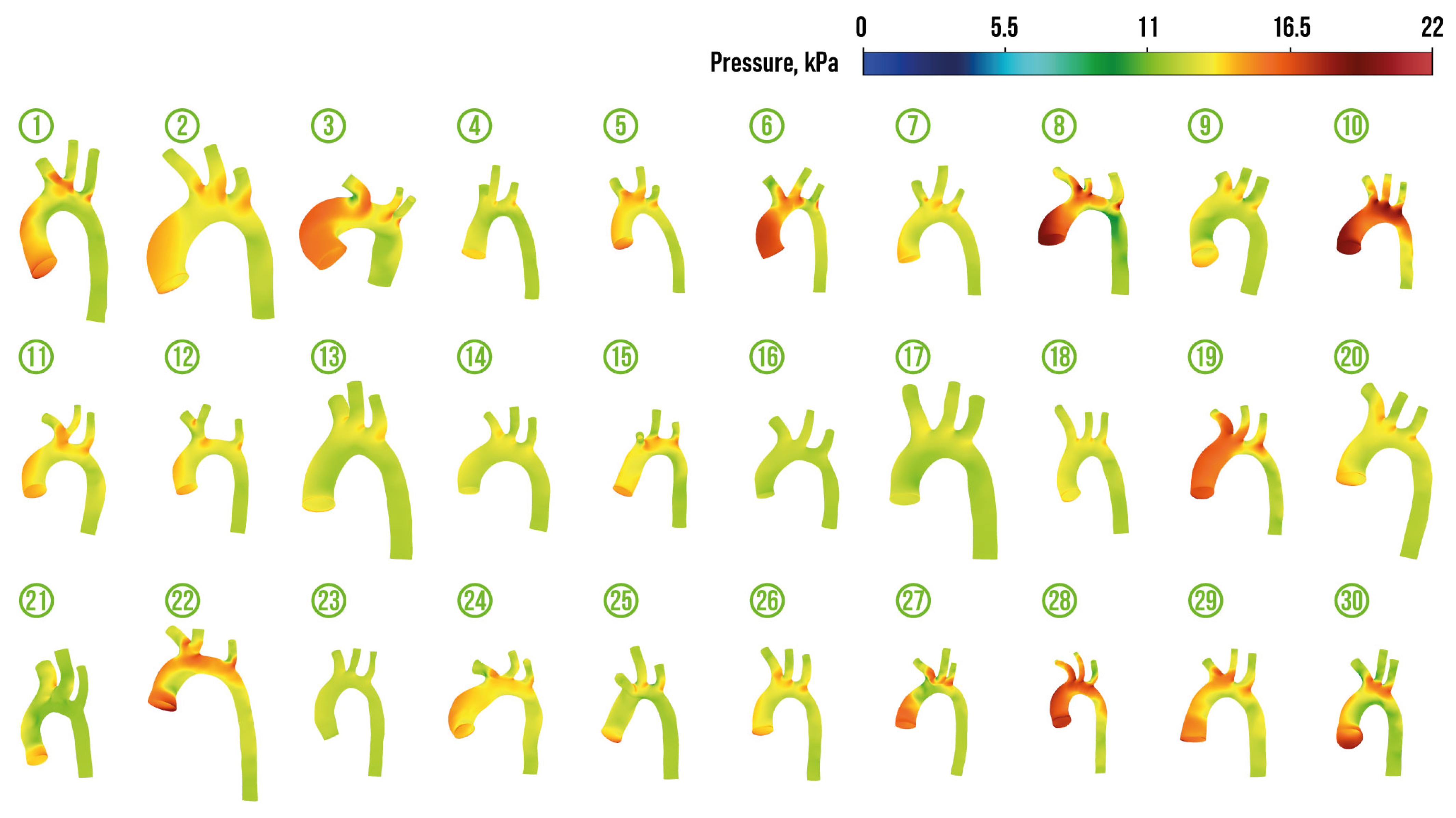
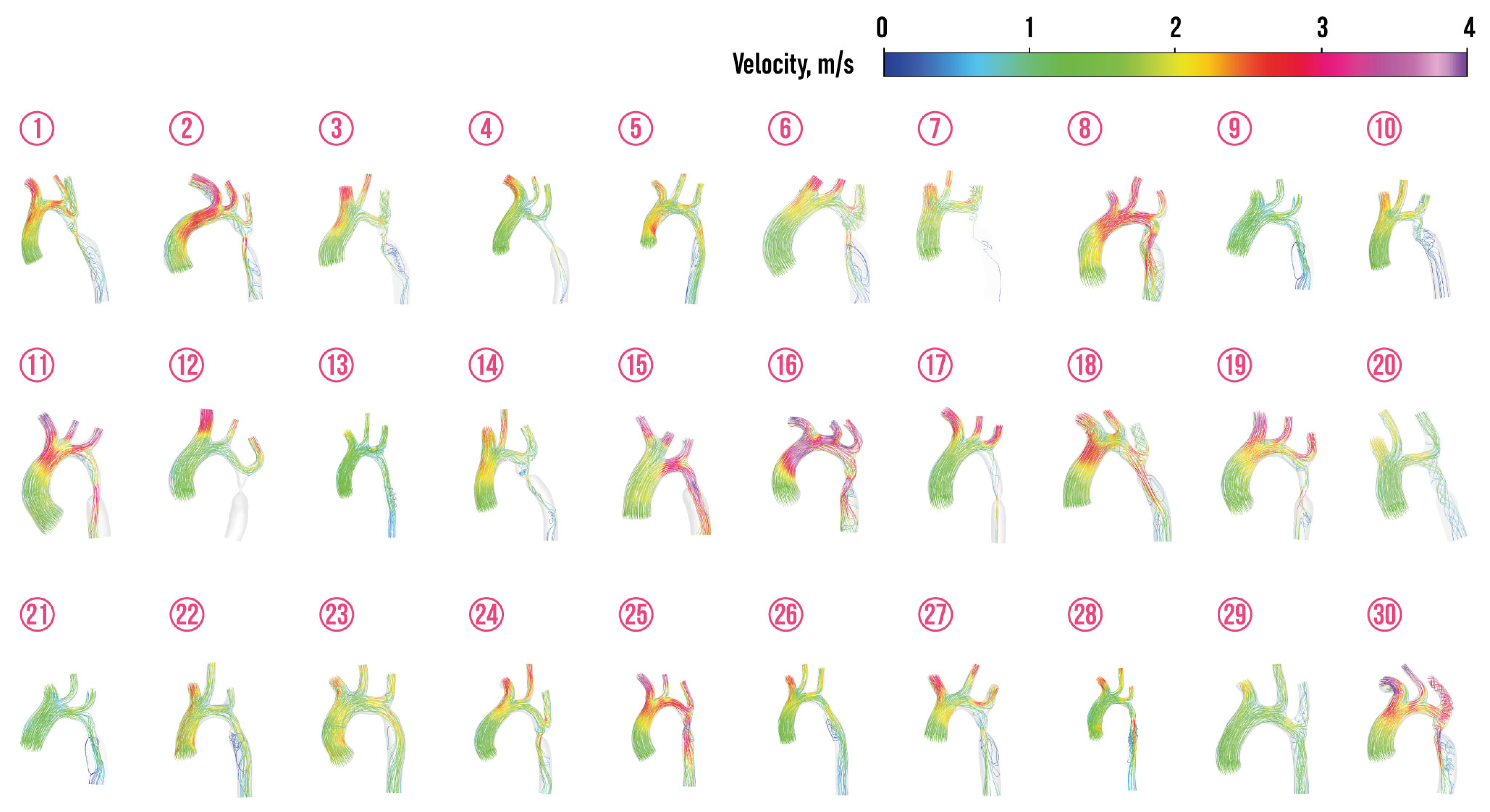
2.2. CFD Model and Hemodynamic Features
2.2.1. CFD Model Application
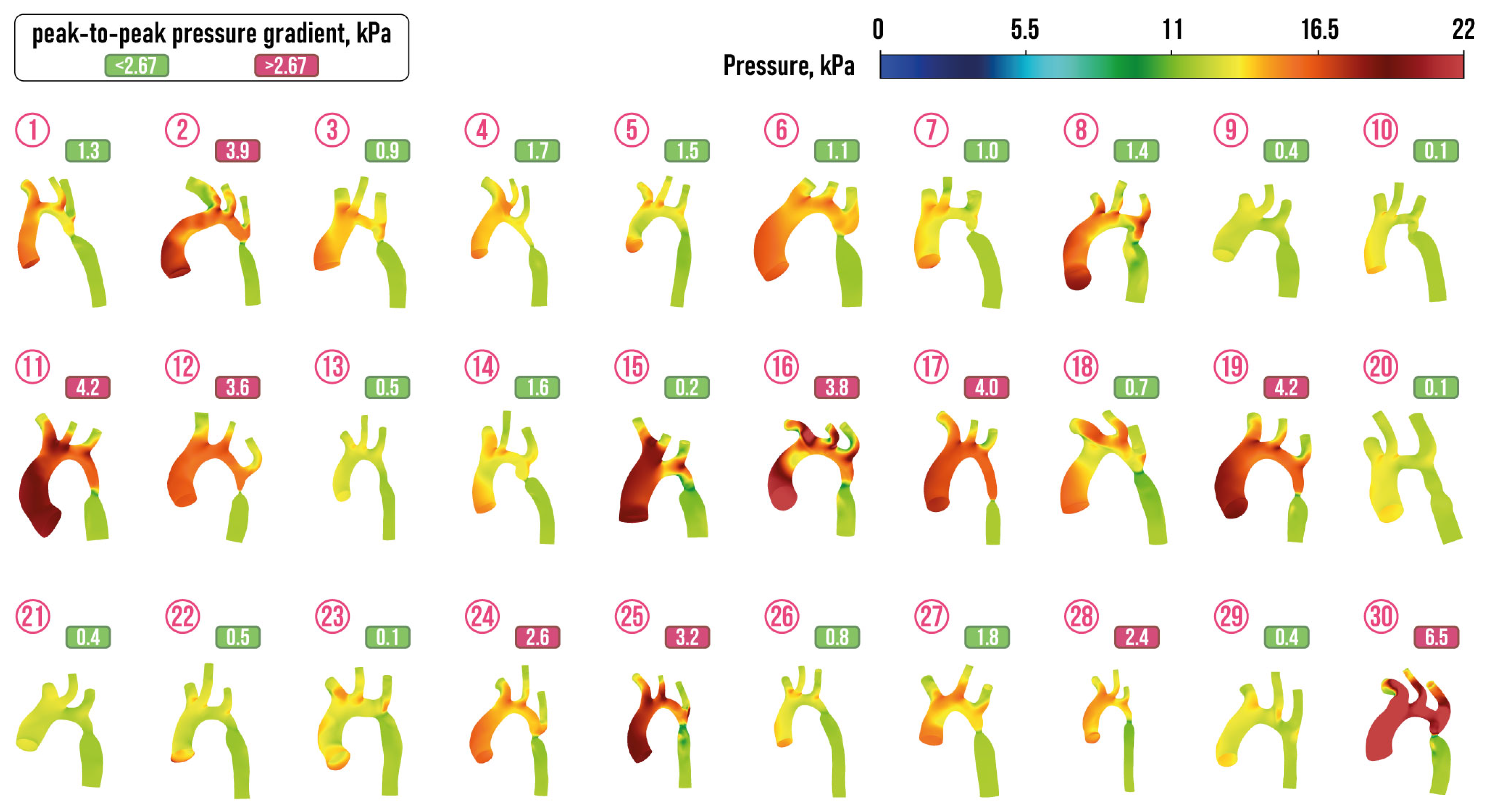
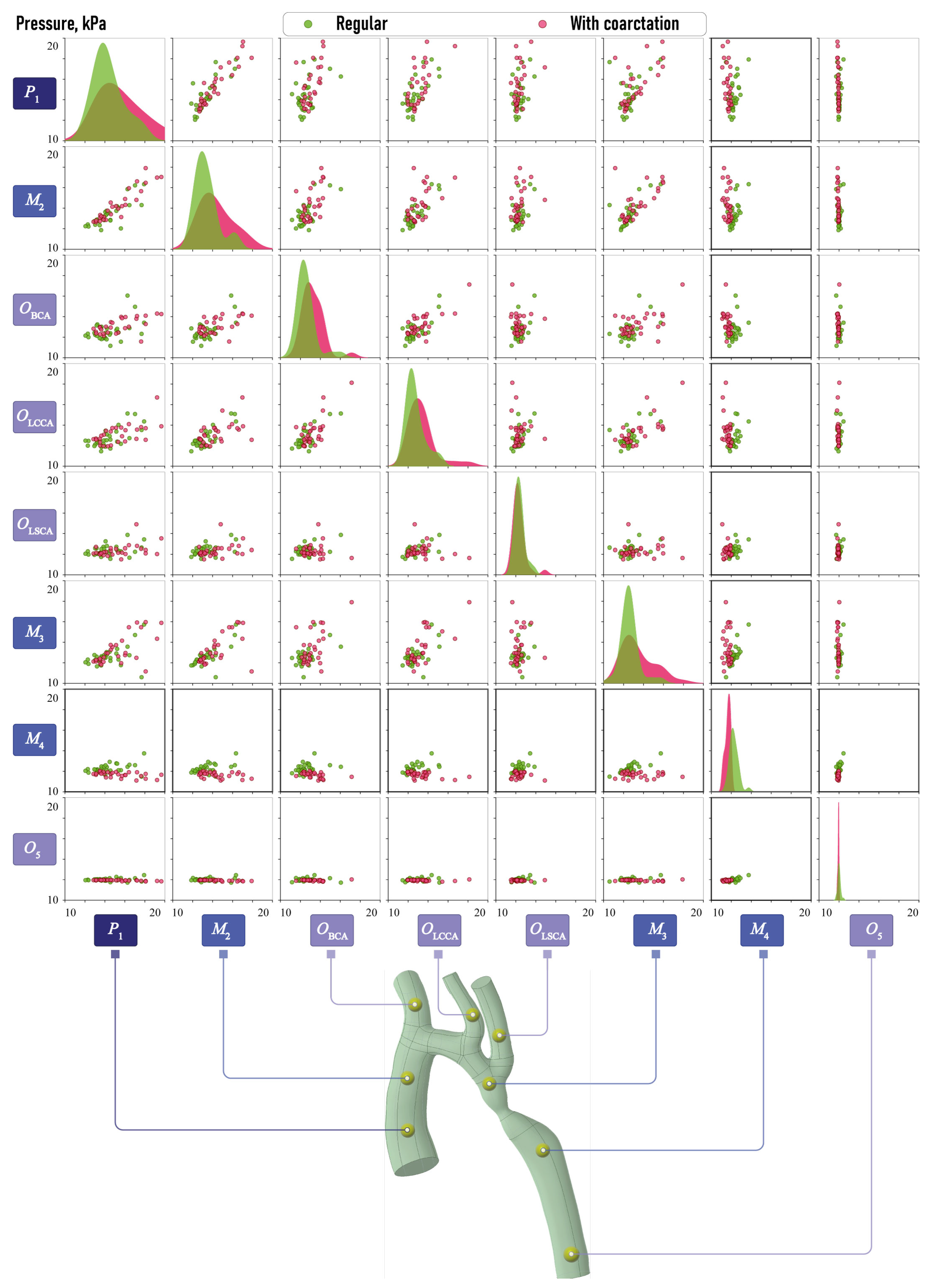
2.2.2. Hemodynamic Features Extraction and Dataset Formation
2.3. Extraction of Key Hemodynamic and Morphometric Characteristics
2.3.1. Morphometric Features
2.3.2. Hemodynamic Features
3. Results
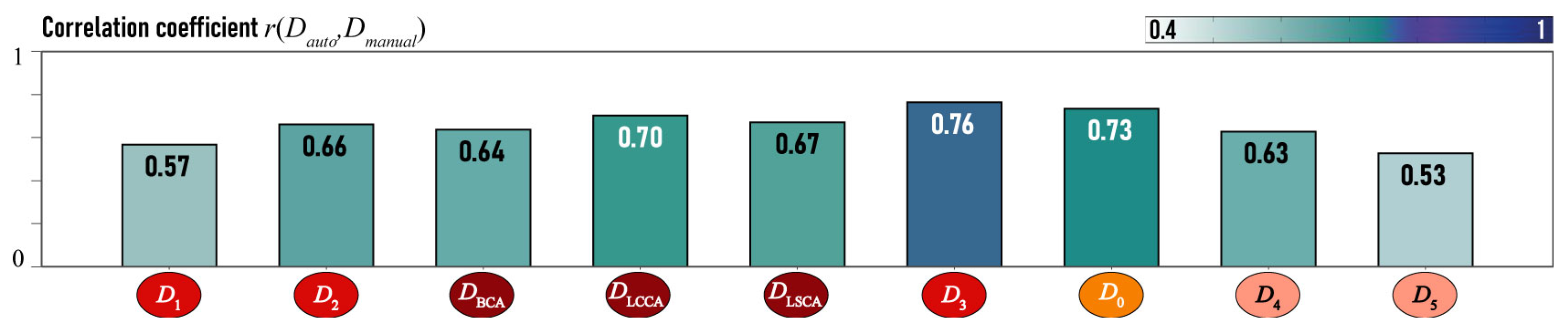
3.1. Metamodel and Relationships between Hemodynamic and Morphometric Characteristics
3.1.1. Hemodynamic Features Prediction by Morphometric Characteristics
3.2. Metamodel
4. Discussion and Concluding Remarks
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| CoA | coarctation of the aorta |
| TTE | transthoracic echocardiography |
| CHD | congenital heart disease |
| MSCT | multi-slice spiral computed tomography |
| ML | machine learning |
| CFD | computational fluid dynamics |
| BCA | brachiocephalic artery |
| LCCA | left common carotid artery |
| LSCA | left subclavian artery |
References
- Godart, F.; Labrot, G.; Devos, P.; Mcfadden, E.; Rey, C.; Beregi, J.P. Coarctation of the aorta: Comparison of aortic dimensions between conventional MR imaging, 3D MR angiography, and conventional angiography. Eur. Radiol. 2002, 12, 2034–2039. [Google Scholar] [CrossRef]
- Bhatt, A.B.; Lantin-Hermoso, M.R.; Daniels, C.J.; Jaquiss, R.; Landis, B.J.; Marino, B.S.; Rathod, R.H.; Vincent, R.N.; Keller, B.B.; Villafane, J. Isolated Coarctation of the Aorta: Current Concepts and Perspectives. Front. Cardiovasc. Med. 2022, 9, 817866. [Google Scholar] [CrossRef]
- Raza, S.; Aggarwal, S.; Jenkins, P.; Kharabish, A.; Anwer, S.; Cullington, D.; Jones, J.; Dua, J.; Papaioannou, V.; Ashrafi, R.; et al. Coarctation of the Aorta: Diagnosis and Management. Diagnostics 2023, 13, 2189. [Google Scholar] [CrossRef] [PubMed]
- Karaosmanoglu, A.D.; Khawaja, R.D.A.; Onur, M.R.; Kalra, M.K. CT and MRI of Aortic Coarctation: Pre- and Postsurgical Findings. Am. J. Roentgenol. 2015, 204, W224–W233. [Google Scholar] [CrossRef] [PubMed]
- Dijkema, E.J.; Leiner, T.; Grotenhuis, H.B. Diagnosis, imaging and clinical management of aortic coarctation. Heart 2017, 103, 1148–1155. [Google Scholar] [CrossRef] [PubMed]
- Baum, U.; Anders, K.; Ropers, D.; Noemayr, A.; Schmid, A.; Seeliger, T.; Singer, H.; Daniel, W.G.; Bautz, W.; Achenbach, S. Multi-slice spiral CT imaging after surgical treatment of aortic coarctation. Eur. Radiol. 2004, 15, 353–355. [Google Scholar] [CrossRef]
- Rius, T.; Goyenechea, M.; Poon, M. Combined cardiac congenital anomalies assessed by multi-slice spiral computed tomography. Eur. Heart J. 2006, 27, 637. [Google Scholar] [CrossRef]
- Li, A.; Peng, Z.; Zhang, C. Comparison of Echocardiography and 64-Multislice Spiral Computed Tomography for the Diagnosis of Pediatric Congenital Heart Disease. Med. Sci. Monit. 2017, 23, 2258–2266. [Google Scholar] [CrossRef][Green Version]
- Gopal, A.; Loewinger, L.; Budoff, M. Aortic coarctation by cardiovascular CT angiography. Catheter. Cardiovasc. Interv. 2010, 76, 551–552. [Google Scholar] [CrossRef]
- Vigneswaran, T.V.; Bellsham-Revell, H.R.; Chubb, H.; Simpson, J.M. Early Postnatal Echocardiography in Neonates with a Prenatal Suspicion of Coarctation of the Aorta. Pediatr. Cardiol. 2020, 41, 772–780. [Google Scholar] [CrossRef]
- Engin, Y.; Kocaoglu, O.P. Aortic Coarctation Diagnosis on Echocardiography Images. J. Artif. Intell. Data Sci. 2024, 4, 39–43. [Google Scholar]
- Yu, Y.; Wang, Y.; Yang, M.; Huang, M.; Li, J.; Jia, Q.; Zhuang, J.; Huang, L. Evaluating the severity of aortic coarctation in infants using anatomic features measured on CTA. Eur. Radiol. 2020, 31, 1216–1226. [Google Scholar] [CrossRef] [PubMed]
- Markl, M.; Frydrychowicz, A.; Kozerke, S.; Hope, M.; Wieben, O. 4D flow MRI. J. Magn. Reson. Imaging 2012, 36, 1015–1036. [Google Scholar] [CrossRef]
- Baybakov, S.; Pavlov, S. Clustering of morphometric parameters of the abdominal aorta and its visceral branches. Med. News North Cauc. 2023, 18, 74–77. [Google Scholar] [CrossRef]
- Leo, I.; Sabatino, J.; Avesani, M.; Moscatelli, S.; Bianco, F.; Borrelli, N.; De Sarro, R.; Leonardi, B.; Calcaterra, G.; Surkova, E.; et al. Non-Invasive Imaging Assessment in Patients with Aortic Coarctation: A Contemporary Review. J. Clin. Med. 2023, 13, 28. [Google Scholar] [CrossRef]
- Fratz, S.; Chung, T.; Greil, G.F.; Samyn, M.M.; Taylor, A.M.; Valsangiacomo Buechel, E.R.; Yoo, S.J.; Powell, A.J. Guidelines and protocols for cardiovascular magnetic resonance in children and adults with congenital heart disease: SCMR expert consensus group on congenital heart disease. J. Cardiovasc. Magn. Reson. 2013, 15, 51. [Google Scholar] [CrossRef]
- Wasserman, M.A.; Shea, E.; Cassidy, C.; Fleishman, C.; France, R.; Parthiban, A.; Landeck, B.F. Recommendations for the Adult Cardiac Sonographer Performing Echocardiography to Screen for Critical Congenital Heart Disease in the Newborn: From the American Society of Echocardiography. J. Am. Soc. Echocardiogr. 2021, 34, 207–222. [Google Scholar] [CrossRef]
- Sun, Z.; Cheng, T.O.; Li, L.; Zhang, L.; Wang, X.; Dong, N.; Lv, Q.; Li, K.; Yuan, L.; Wang, J.; et al. Diagnostic Value of Transthoracic Echocardiography in Patients with Coarctation of Aorta: The Chinese Experience in 53 Patients Studied between 2008 and 2012 in One Major Medical Center. PLoS ONE 2015, 10, e0127399. [Google Scholar] [CrossRef]
- Krishnam, M.S.; Tomasian, A.; Malik, S.; Desphande, V.; Laub, G.; Ruehm, S.G. Image quality and diagnostic accuracy of unenhanced SSFP MR angiography compared with conventional contrast-enhanced MR angiography for the assessment of thoracic aortic diseases. Eur. Radiol. 2009, 20, 1311–1320. [Google Scholar] [CrossRef]
- Benavidez, O.J.; Gauvreau, K.; Geva, T. Diagnostic Errors in Congenital Echocardiography: Importance of Study Conditions. J. Am. Soc. Echocardiogr. 2014, 27, 616–623. [Google Scholar] [CrossRef]
- Suradi, H.; Hijazi, Z.M. Current management of coarctation of the aorta. Glob. Cardiol. Sci. Pract. 2015, 2015, 44. [Google Scholar] [CrossRef] [PubMed]
- Hoffman, J.I.; Kaplan, S. The incidence of congenital heart disease. J. Am. Coll. Cardiol. 2002, 39, 1890–1900. [Google Scholar] [CrossRef]
- Reller, M.D.; Strickland, M.J.; Riehle-Colarusso, T.; Mahle, W.T.; Correa, A. Prevalence of Congenital Heart Defects in Metropolitan Atlanta, 1998–2005. J. Pediatr. 2008, 153, 807–813. [Google Scholar] [CrossRef]
- Hager, A.; Kanz, S.; Kaemmerer, H.; Schreiber, C.; Hess, J. Coarctation Long-term Assessment (COALA): Significance of arterial hypertension in a cohort of 404 patients up to 27 years after surgical repair of isolated coarctation of the aorta, even in the absence of restenosis and prosthetic material. J. Thorac. Cardiovasc. Surg. 2007, 134, 738–745. [Google Scholar] [CrossRef]
- Chen, C.K.; Cifra, B.; Morgan, G.J.; Sarkola, T.; Slorach, C.; Wei, H.; Bradley, T.J.; Manlhiot, C.; McCrindle, B.W.; Redington, A.N.; et al. Left Ventricular Myocardial and Hemodynamic Response to Exercise in Young Patients after Endovascular Stenting for Aortic Coarctation. J. Am. Soc. Echocardiogr. 2016, 29, 237–246. [Google Scholar] [CrossRef]
- Cook, S.C.; Hickey, J.; Maul, T.M.; Zumberge, N.; Krieger, E.V.; Valente, A.M.; Zaidi, A.N.; Daniels, C.J. Assessment of the Cerebral Circulation in Adults with Coarctation of the Aorta. Congenit. Heart Dis. 2013, 8, 289–295. [Google Scholar] [CrossRef] [PubMed]
- Campbell, M.; Baylis, J.H. The course and prognosis of coarctation of the aorta. Heart 1956, 18, 475–495. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Campbell, M. Natural history of coarctation of the aorta. Heart 1970, 32, 633–640. [Google Scholar] [CrossRef] [PubMed]
- Lozano, R.; Naghavi, M.; Foreman, K.; Lim, S.; Shibuya, K.; Aboyans, V.; Abraham, J.; Adair, T.; Aggarwal, R.; Ahn, S.Y.; et al. Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: A systematic analysis for the Global Burden of Disease Study 2010. Lancet 2012, 380, 2095–2128. [Google Scholar] [CrossRef]
- Beckmann, E.; Jassar, A.S. Coarctation Repair—Redo Challenges in the Adults: What to Do? J. Vis. Surg. 2018, 4, 76. [Google Scholar] [CrossRef]
- Asselbergs, F.W.; Fraser, A.G. Artificial intelligence in cardiology: The debate continues. Eur. Heart J.-Digit. Health 2021, 2, 721–726. [Google Scholar] [CrossRef] [PubMed]
- Harrison, C.J.; Sidey-Gibbons, C.J. Machine learning in medicine: A practical introduction to natural language processing. BMC Med. Res. Methodol. 2021, 21, 158. [Google Scholar] [CrossRef] [PubMed]
- Permyakova, A.V.; Porodikov, A.; Kuchumov, A.G.; Biyanov, A.; Arutunyan, V.; Furman, E.G.; Sinelnkov, Y.S. Discriminant Analysis of Main Prognostic Factors Associated with Hemodynamically Significant PDA: Apgar Score, Silverman–Anderson Score, and NT-Pro-BNP Level. J. Clin. Med. 2021, 10, 3729. [Google Scholar] [CrossRef] [PubMed]
- Gao, H.; Li, Y.; Zhang, Z.; Zhao, W. Editorial: Machine Learning Used in Biomedical Computing and Intelligence Healthcare, Volume II. Front. Genet. 2022, 13, 850667. [Google Scholar] [CrossRef]
- Lin, Y.; Hu, J.; Xu, R.; Wu, S.; Ma, F.; Liu, H.; Xie, Y.; Li, X. Application of Logistic Regression and Artificial Intelligence in the Risk Prediction of Acute Aortic Dissection Rupture. J. Clin. Med. 2023, 12, 179. [Google Scholar] [CrossRef]
- Ogaga, D.; Zhao, H. The Rise of Artificial Intelligence and Machine Learning in HealthCare Industry. Int. J. Res. Innov. Appl. Sci. 2023, VIII, 250–253. [Google Scholar] [CrossRef]
- Javaid, M.; Haleem, A.; Pratap Singh, R.; Suman, R.; Rab, S. Significance of machine learning in healthcare: Features, pillars and applications. Int. J. Intell. Netw. 2022, 3, 58–73. [Google Scholar] [CrossRef]
- Krishnan, G.; Singh, S.; Pathania, M.; Gosavi, S.; Abhishek, S.; Parchani, A.; Dhar, M. Artificial intelligence in clinical medicine: Catalyzing a sustainable global healthcare paradigm. Front. Artif. Intell. 2023, 6, 1227091. [Google Scholar] [CrossRef]
- de Vries, E.N.; Ramrattan, M.A.; Smorenburg, S.M.; Gouma, D.J.; Boermeester, M.A. The incidence and nature of in-hospital adverse events: A systematic review. Qual. Saf. Health Care 2008, 17, 216–223. [Google Scholar] [CrossRef]
- Berguer, R.; Heller, P.J. Preventing sharps injuries in the operating room. J. Am. Coll. Surg. 2004, 199, 462–467. [Google Scholar] [CrossRef]
- Emond, R.T.; Evans, B.; Bowen, E.T.; Lloyd, G. A case of Ebola virus infection. BMJ 1977, 2, 541–544. [Google Scholar] [CrossRef]
- Wolfensberger, W. Ethical Issues in Research with Human Subjects: A rationale is formulated for a code of conduct in the recruitment of subjects for research. Science 1967, 155, 47–51. [Google Scholar] [CrossRef]
- Marshall, P. Ethical Challenges in Study Design and Informed Consent for Health Research in Resource-Poor Settings; World Health Organization: Geneva, Switzerland, 2007; p. 79. [Google Scholar]
- Versnjak, J.; Yevtushenko, P.; Kuehne, T.; Bruening, J.; Goubergrits, L. Deep learning based assessment of hemodynamics in the coarctation of the aorta: Comparison of bidirectional recurrent and convolutional neural networks. Front. Physiol. 2024, 15, 1288339. [Google Scholar] [CrossRef] [PubMed]
- Butera, G.; Schievano, S.; Biglino, G.; McElhinney, D.B. Modelling Congenital Heart Disease: Engineering a Patient-Specific Therapy, 1st ed.; Springer International Publishing: Cham, Switzerland, 2022. [Google Scholar] [CrossRef]
- Robertson, A.M.; Sequeira, A.; Owens, R.G. Rheological models for blood. In Cardiovascular Mathematics: Modeling and Simulation of the Circulatory System; Formaggia, L., Quarteroni, A., Veneziani, A., Eds.; Springer: Milan, Italy, 2009; pp. 211–241. [Google Scholar] [CrossRef]
- Kogan, B.J. Introduction to Computational Cardiology: Mathematical Modeling and Computer Simulation; Springer: New York, NY, USA, 2010. [Google Scholar] [CrossRef]
- Guccione, J.M.; Kassab, G.S.; Ratcliffe, M.B. Computational Cardiovascular Mechanics; Springer: New York, NY, USA, 2010. [Google Scholar] [CrossRef]
- Sadeghi, R.; Tomka, B.; Khodaei, S.; Garcia, J.; Ganame, J.; Keshavarz-Motamed, Z. Reducing Morbidity and Mortality in Patients With Coarctation Requires Systematic Differentiation of Impacts of Mixed Valvular Disease on Coarctation Hemodynamics. J. Am. Heart Assoc. 2022, 11, e022664. [Google Scholar] [CrossRef] [PubMed]
- Kuchumov, A.G.; Khairulin, A.; Shmurak, M.; Porodikov, A.; Merzlyakov, A. The Effects of the Mechanical Properties of Vascular Grafts and an Anisotropic Hyperelastic Aortic Model on Local Hemodynamics during Modified Blalock–Taussig Shunt Operation, Assessed Using FSI Simulation. Materials 2022, 15, 2719. [Google Scholar] [CrossRef] [PubMed]
- Hellmeier, F.; Brüning, J.; Sündermann, S.; Jarmatz, L.; Schafstedde, M.; Goubergrits, L.; Kühne, T.; Nordmeyer, S. Hemodynamic Modeling of Biological Aortic Valve Replacement Using Preoperative Data Only. Front. Cardiovasc. Med. 2021, 7, 593709. [Google Scholar] [CrossRef] [PubMed]
- Luraghi, G.; Migliavacca, F.; Chiastra, C.; Rossi, A.; Reimers, B.; Stefanini, G.G.; Rodriguez Matas, J.F. Does clinical data quality affect fluid-structure interaction simulations of patient-specific stenotic aortic valve models? J. Biomech. 2019, 94, 202–210. [Google Scholar] [CrossRef]
- Jack, J.T.; Jensen, M.; Collins, R.T.; Chan, F.P.; Millett, P.C. Numerical study of hemodynamic flow in the aortic vessel of Williams syndrome patient with congenital heart disease. J. Biomech. 2024, 168, 112124. [Google Scholar] [CrossRef] [PubMed]
- Van der Palen, R.L.; Barker, A.J.; Bollache, E.; Garcia, J.; Rose, M.J.; van Ooij, P.; Young, L.T.; Roest, A.A.; Markl, M.; Robinson, J.D.; et al. Altered aortic 3D hemodynamics and geometry in pediatric Marfan syndrome patients. J. Cardiovasc. Magn. Reson. 2016, 19, 30. [Google Scholar] [CrossRef]
- Kuchumov, A.G.; Doroshenko, O.V.; Golub, M.V.; Saychenko, N.D.; Rakisheva, I.O.; Shekhmametyev, R.M. Numerical Method for Geometrical Feature Extraction and Identification of Patient-Specific Aorta Models in Pediatric Congenital Heart Disease. Mathematics 2023, 11, 2871. [Google Scholar] [CrossRef]
- Antonuccio, M.N.; Mariotti, A.; Fanni, B.M.; Capellini, K.; Capelli, C.; Sauvage, E.; Celi, S. Effects of Uncertainty of Outlet Boundary Conditions in a Patient-Specific Case of Aortic Coarctation. Ann. Biomed. Eng. 2021, 49, 3494–3507. [Google Scholar] [CrossRef]
- Chen, Z.; Zhou, Y.; Wang, J.; Liu, X.; Ge, S.; He, Y. Modeling of coarctation of aorta in human fetuses using 3D/4D fetal echocardiography and computational fluid dynamics. Echocardiography 2017, 34, 1858–1866. [Google Scholar] [CrossRef]
- Swanson, L.; Owen, B.; Keshmiri, A.; Deyranlou, A.; Aldersley, T.; Lawrenson, J.; Human, P.; De Decker, R.; Fourie, B.; Comitis, G.; et al. A Patient-Specific CFD Pipeline Using Doppler Echocardiography for Application in Coarctation of the Aorta in a Limited Resource Clinical Context. Front. Bioeng. Biotechnol. 2020, 8, 409. [Google Scholar] [CrossRef] [PubMed]
- Morris, P.D.; Narracott, A.; von Tengg-Kobligk, H.; Silva Soto, D.A.; Hsiao, S.; Lungu, A.; Evans, P.; Bressloff, N.W.; Lawford, P.V.; Hose, D.R.; et al. Computational fluid dynamics modelling in cardiovascular medicine. Heart 2015, 102, 18–28. [Google Scholar] [CrossRef]
- Perinajová, R.; Juffermans, J.F.; Mercado, J.L.; Aben, J.P.; Ledoux, L.; Westenberg, J.J.M.; Lamb, H.J.; Kenjereš, S. Assessment of turbulent blood flow and wall shear stress in aortic coarctation using image-based simulations. BioMed. Eng. Online 2021, 20, 84. [Google Scholar] [CrossRef] [PubMed]
- Schubert, C.; Brüning, J.; Goubergrits, L.; Hennemuth, A.; Berger, F.; Kühne, T.; Kelm, M. Assessment of hemodynamic responses to exercise in aortic coarctation using MRI-ergometry in combination with computational fluid dynamics. Sci. Rep. 2020, 10, 18894. [Google Scholar] [CrossRef] [PubMed]
- Kamaltdinov, M.; Kuchumov, A. Application of a mathematical model of systemic circulation for determination of blood flow parameters after modified Blalock-Taussig shunt operation in newborns. Russ. J. Biomech. 2021, 25, 268–284. [Google Scholar] [CrossRef]
- Sinelnikov, Y.; Arutunyan, V.; Porodikov, A.; Biyanov, A.; Tuktamyshev, V.; Shmurak, M.; Khairulin, A.; Kuchumov, A. Application of mathematical modelling for the evaluation of the results of systemic-pulmonary shunts formation. Patol. Krovoobrashcheniya Kardiokhirurgiya 2020, 24, 45–61. [Google Scholar] [CrossRef]
- Kuchumov, A.G.; Selyaninov, A. Application of Computational Fluid Dynamics in Biofluids Simulation to Solve Actual Surgery Tasks. In Human Interaction and Emerging Technologies; Springer International Publishing: Cham, Switzerland, 2019; pp. 576–580. [Google Scholar] [CrossRef]
- Khairulin, A.R.; Rakisheva, I.O.; Kuchumov, A.G.; Golub, M.V.; Shekhmametiev, R.M.; Lazarkov, P.V. Investigation of the influence of intersystem shunt characteristics on hemodynamic parameters and oxygen distribution. Izv. Saratov Univ. Math. Mech. Inform. 2024, 24, 254–274. [Google Scholar] [CrossRef]
- Kuchumov, A.; Khairulin, A.; Biyanov, A.; Porodikov, A.; Aratyunyan, V.; Sinelnikov, Y. Effectiveness of Blalock–Taussig shunt performance in the congenital heart disease children. Russ. J. Biomech. 2020, 24, 65–83. [Google Scholar] [CrossRef]
- Black, S.M.; Maclean, C.; Hall Barrientos, P.; Ritos, K.; McQueen, A.; Kazakidi, A. Calibration of patient-specific boundary conditions for coupled CFD models of the aorta derived from 4D Flow-MRI. Front. Bioeng. Biotechnol. 2023, 11, 1178483. [Google Scholar] [CrossRef] [PubMed]
- Kuchumov, A.G.; Kamaltdinov, M.R.; Khairulin, A.R.; Kochergin, M.V.; Shmurak, M.I. Patient-Specific 0D–3D Modeling of Blood Flow in Newborns To Predict Risks of Complications After Surgery. Health Risk Anal. 2022, 4, 159–167. [Google Scholar] [CrossRef]
- Nita, C.I.; Puiu, A.; Bunescu, D.; Mihai Itu, L.; Mihalef, V.; Chintalapani, G.; Armstrong, A.; Zampi, J.; Benson, L.; Sharma, P.; et al. Personalized Pre- and Post-Operative Hemodynamic Assessment of Aortic Coarctation from 3D Rotational Angiography. Cardiovasc. Eng. Technol. 2021, 13, 14–40. [Google Scholar] [CrossRef] [PubMed]
- Liu, X.; Aslan, S.; Hess, R.; Mass, P.; Olivieri, L.; Loke, Y.H.; Hibino, N.; Fuge, M.; Krieger, A. Automatic Shape Optimization of Patient-Specific Tissue Engineered Vascular Grafts for Aortic Coarctation. In Proceedings of the 2020 42nd Annual International Conference of the IEEE Engineering in Medicine & Biology Society (EMBC), Montreal, QC, Canada, 20–24 July 2020. [Google Scholar] [CrossRef]
- Li, G.; Wang, H.; Zhang, M.; Tupin, S.; Qiao, A.; Liu, Y.; Ohta, M.; Anzai, H. Prediction of 3D Cardiovascular hemodynamics before and after coronary artery bypass surgery via deep learning. Commun. Biol. 2021, 4, 99. [Google Scholar] [CrossRef] [PubMed]
- Yevtushenko, P.; Goubergrits, L.; Gundelwein, L.; Setio, A.; Ramm, H.; Lamecker, H.; Heimann, T.; Meyer, A.; Kuehne, T.; Schafstedde, M. Deep Learning Based Centerline-Aggregated Aortic Hemodynamics: An Efficient Alternative to Numerical Modeling of Hemodynamics. IEEE J. Biomed. Health Inform. 2022, 26, 1815–1825. [Google Scholar] [CrossRef]
- Lu, Q.; Lin, W.; Zhang, R.; Chen, R.; Wei, X.; Li, T.; Du, Z.; Xie, Z.; Yu, Z.; Xie, X.; et al. Validation and Diagnostic Performance of a CFD-Based Non-invasive Method for the Diagnosis of Aortic Coarctation. Front. Neuroinform. 2020, 14, 613666. [Google Scholar] [CrossRef]
- Singh, H.; Meyer, A.N.D.; Thomas, E.J. The frequency of diagnostic errors in outpatient care: Estimations from three large observational studies involving US adult populations. BMJ Qual. Saf. 2014, 23, 727–731. [Google Scholar] [CrossRef]
- Lassetter, J.H.; Warnick, M.L. Medical Errors, Drug-Related Problems, and Medication Errors: A Literature Review on Quality of Care and Cost Issues. J. Nurs. Care Qual. 2003, 18, 175–183. [Google Scholar] [CrossRef]
- Shaikhina, T.; Lowe, D.; Daga, S.; Briggs, D.; Higgins, R.; Khovanova, N. Machine Learning for Predictive Modelling based on Small Data in Biomedical Engineering. IFAC-PapersOnLine 2015, 48, 469–474. [Google Scholar] [CrossRef]
- Tanwani, A.K.; Afridi, J.; Shafiq, M.Z.; Farooq, M. Guidelines to Select Machine Learning Scheme for Classification of Biomedical Datasets. In Lecture Notes in Computer Science; Springer: Berlin/Heidelberg, Germany, 2009; pp. 128–139. [Google Scholar] [CrossRef]
- Xiao, N.; Humphrey, J.D.; Figueroa, C.A. Multi-scale computational model of three-dimensional hemodynamics within a deformable full-body arterial network. J. Comput. Phys. 2013, 244, 22–40. [Google Scholar] [CrossRef]
- Randles, A.; Draeger, E.W.; Oppelstrup, T.; Krauss, L.; Gunnels, J.A. Massively parallel models of the human circulatory system. In Proceedings of the International Conference for High Performance Computing, Networking, Storage and Analysis, SC15, Austin, TX, USA, 15–20 November 2015; ACM: New York, NY, USA, 2015. [Google Scholar] [CrossRef]
- Baumgartner, H.; Bonhoeffer, P.; De Groot, N.M.S.; de Haan, F.; Deanfield, J.E.; Galie, N.; Gatzoulis, M.A.; Gohlke-Baerwolf, C.; Kaemmerer, H.; Kilner, P.; et al. ESC Guidelines for the management of grown-up congenital heart disease (new version 2010): The Task Force on the Management of Grown-up Congenital Heart Disease of the European Society of Cardiology (ESC). Eur. Heart J. 2010, 31, 2915–2957. [Google Scholar] [CrossRef] [PubMed]
- Boussel, L.; Rayz, V.; McCulloch, C.; Martin, A.; Acevedo-Bolton, G.; Lawton, M.; Higashida, R.; Smith, W.S.; Young, W.L.; Saloner, D. Aneurysm Growth Occurs at Region of Low Wall Shear Stress: Patient-Specific Correlation of Hemodynamics and Growth in a Longitudinal Study. Stroke 2008, 39, 2997–3002. [Google Scholar] [CrossRef] [PubMed]
- Cheng, C.; Tempel, D.; van Haperen, R.; van der Baan, A.; Grosveld, F.; Daemen, M.J.; Krams, R.; de Crom, R. Atherosclerotic Lesion Size and Vulnerability Are Determined by Patterns of Fluid Shear Stress. Circulation 2006, 113, 2744–2753. [Google Scholar] [CrossRef] [PubMed]
- Kim, G.B.; Park, K.H.; Kim, S.J. Hemodynamics and Wall Shear Stress of Blood Vessels in Aortic Coarctation with Computational Fluid Dynamics Simulation. Molecules 2022, 27, 1403. [Google Scholar] [CrossRef]
- Rafiei, D.; Abazari, M.A.; Soltani, M.; Alimohammadi, M. The effect of coarctation degrees on wall shear stress indices. Sci. Rep. 2021, 11, 12757. [Google Scholar] [CrossRef]
- Snider, A.; Enderlein, M.; Teitel, D.; Juster, R. Two-dimensional echocardiographic determination of aortic and pulmonary artery sizes from infancy to adulthood in normal subjects. Am. J. Cardiol. 1984, 53, 218–224. [Google Scholar] [CrossRef]
- Truong, D.; Tani, L.; Minich, L.; Burch, P.; Bardsley, T.; Menon, S. Factors Associated with Recoarctation After Surgical Repair of Coarctation of the Aorta by way of Thoracotomy in Young Infants. Pediatr. Cardiol. 2013, 7, 164–170. [Google Scholar] [CrossRef]
- Rose-Felker, K.; Robinson, J.; Backer, C.; Rigsby, C.; Eltayeb, O.; Monge, M.; Rychlik, K.; Sammet, C.; Gossett, J. Preoperative Use of CT Angiography in Infants With Coarctation of the Aorta. World J. Pediatr. Congenit. Heart Surg. 2017, 8, 196–202. [Google Scholar] [CrossRef]
- Kieffer, E.; Sabatier, J.; Koskas, F.; Bahnini, A. Atherosclerotic innominate artery occlusive disease: Early and long-term results of surgical reconstruction. J. Vasc. Surg. 1995, 21, 326–337. [Google Scholar] [CrossRef]
- Azakie, A.; Mcelhinney, D.; Messina, L.; Stoney, R. Common brachiocephalic trunk: Strategies for revascularization. Ann. Thorac. Surg. 1999, 67, 657–660. [Google Scholar] [CrossRef]
- Apithanung, L.; Sethasathien, S.; Silvilairat, S.; Sittiwangkul, R.; Makonkawkeyoon, K.; Saengsin, K.; Woragidpoonpol, S. Correlation between pressure gradient from echocardiography and peak-to-peak pressure gradient from cardiac catheterization or surgery in patients with coarctation of aorta. J. Cardiovasc. Imaging 2024, 40, 1193–1200. [Google Scholar] [CrossRef] [PubMed]
- Warnes, C.; Williams, R.; Bashore, T.; Child, J.; Connolly, H.; Dearani, J.; Del Nido, P.; Fasules, J.; Graham, T.; Hijazi, Z.; et al. ACC/AHA 2008 Guidelines for the Management of Adults with Congenital Heart Disease. Circulation 2008, 118, e714–e833. [Google Scholar] [CrossRef]
- Gholamy, A.; Kreinovich, V.; Kosheleva, O. Why 70/30 or 80/20 Relation between Training and Testing Sets: A Pedagogical Explanation; Techreport; University of Texas at El Paso: El Paso, TX, USA, 2018. [Google Scholar]
- Tonyan, A.G.; Khan, V.V.; Khalafyan, A.A.; Bunyakin, A.V.; Avakyan, S.N.; Lymar, M.S. Pathogenetic development factors of position-dependent changes in oxygen saturation. Vestn. Vosstanov. Med. 2021, 20, 77–90. [Google Scholar] [CrossRef]
- Azahari, A.; Naim, W.; Sari, N.; Lim, E.; Mokhtarudin, M. Advancement in computational simulation and validation of congenital heart disease: A review. Comput. Methods Biomech. Biomed. Eng. 2024, 27, 1–14. [Google Scholar] [CrossRef] [PubMed]





| −0.399 | 0.999 | 0.11 | −1.726 | 1.134 |
| Characteristic | |||||
|---|---|---|---|---|---|
| Coefficients | 1.377 | −1.472 | −1.914 | 0.482 | 0.414 |
| Characteristic | |||||
|---|---|---|---|---|---|
| Coefficients | −1.05 | −1.05 | −1.05 | 1.138 | 0.799 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Doroshenko, O.V.; Kuchumov, A.G.; Golub, M.V.; Rakisheva, I.O.; Skripka, N.A.; Pavlov, S.P.; Strazhec, Y.A.; Lazarkov, P.V.; Saychenko, N.D.; Shekhmametyev, R.M. Investigation of Relationship between Hemodynamic and Morphometric Characteristics of Aortas in Pediatric Patients. J. Clin. Med. 2024, 13, 5141. https://doi.org/10.3390/jcm13175141
Doroshenko OV, Kuchumov AG, Golub MV, Rakisheva IO, Skripka NA, Pavlov SP, Strazhec YA, Lazarkov PV, Saychenko ND, Shekhmametyev RM. Investigation of Relationship between Hemodynamic and Morphometric Characteristics of Aortas in Pediatric Patients. Journal of Clinical Medicine. 2024; 13(17):5141. https://doi.org/10.3390/jcm13175141
Chicago/Turabian StyleDoroshenko, Olga V., Alex G. Kuchumov, Mikhail V. Golub, Irina O. Rakisheva, Nikita A. Skripka, Sergey P. Pavlov, Yulija A. Strazhec, Petr V. Lazarkov, Nikita D. Saychenko, and Roman M. Shekhmametyev. 2024. "Investigation of Relationship between Hemodynamic and Morphometric Characteristics of Aortas in Pediatric Patients" Journal of Clinical Medicine 13, no. 17: 5141. https://doi.org/10.3390/jcm13175141
APA StyleDoroshenko, O. V., Kuchumov, A. G., Golub, M. V., Rakisheva, I. O., Skripka, N. A., Pavlov, S. P., Strazhec, Y. A., Lazarkov, P. V., Saychenko, N. D., & Shekhmametyev, R. M. (2024). Investigation of Relationship between Hemodynamic and Morphometric Characteristics of Aortas in Pediatric Patients. Journal of Clinical Medicine, 13(17), 5141. https://doi.org/10.3390/jcm13175141








