Respiratory Drive, Effort, and Lung-Distending Pressure during Transitioning from Controlled to Spontaneous Assisted Ventilation in Patients with ARDS: A Multicenter Prospective Cohort Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Population and Setting
2.2. Measurements and Study Protocol
2.3. Statistical Methods
3. Results
3.1. Patients Baseline Characteristics
3.2. Ventilator Settings, Respiratory Drive, and Effort during Spontaneous Assisted Breathing
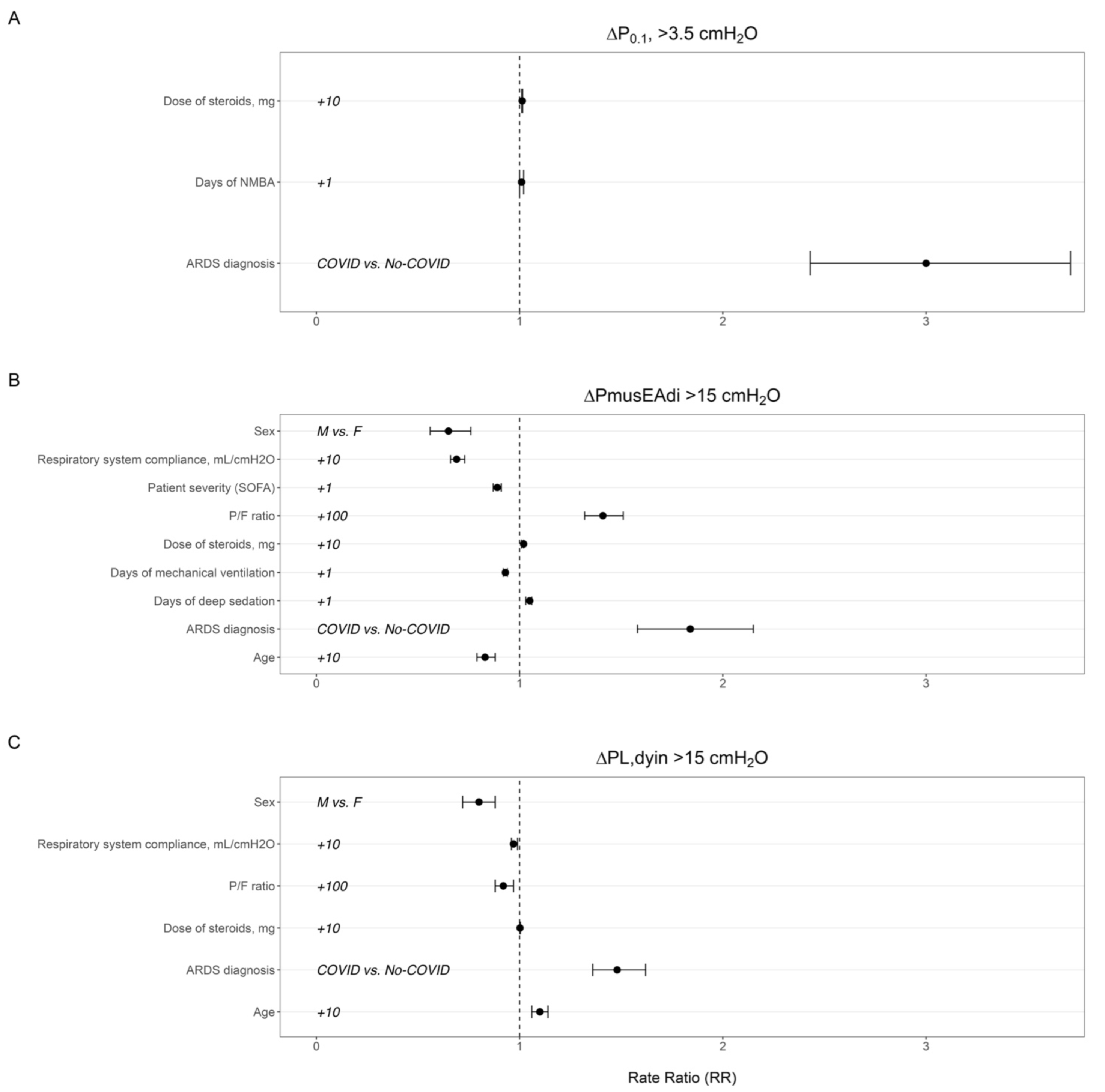
3.3. Effects of Patients’ Baseline Characteristics and Treatment Factors before Transition to Assisted Ventilation on Respiratory Drive, Inspiratory Effort, and Lung-Distending Pressure
3.4. Effects of Patients’ Baseline Characteristics and Treatment Factors on Need for Sedation and Resuming Control Ventilation
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Yoshida, T.; Nakahashi, S.; Nakamura, M.A.M.; Koyama, Y.; Roldan, R.; Torsani, V.; De Santis, R.R.; Gomes, S.; Uchiyama, A.; Amato, M.B.P.; et al. Volume-controlled Ventilation Does Not Prevent Injurious Inflation during Spontaneous Effort. Am. J. Respir. Crit. Care Med. 2017, 196, 590–601. [Google Scholar] [CrossRef] [PubMed]
- Yoshida, T.; Torsani, V.; Gomes, S.; De Santis, R.R.; Beraldo, M.A.; Costa, E.L.; Tucci, M.R.; Zin, W.A.; Kavanagh, B.P.; Amato, M.B. Spontaneous effort causes occult pendelluft during mechanical ventilation. Am. J. Respir. Crit. Care Med. 2013, 188, 1420–1427. [Google Scholar] [CrossRef] [PubMed]
- Yoshida, T.; Amato, M.B.P.; Grieco, D.L.; Chen, L.; Lima, C.A.S.; Roldan, R.; Morais, C.C.A.; Gomes, S.; Costa, E.L.V.; Cardoso, P.F.G.; et al. Esophageal Manometry and Regional Transpulmonary Pressure in Lung Injury. Am. J. Respir. Crit. Care Med. 2018, 197, 1018–1026. [Google Scholar] [CrossRef] [PubMed]
- Grasselli, G.; Tonetti, T.; Protti, A.; Langer, T.; Girardis, M.; Bellani, G.; Laffey, J.; Carrafiello, G.; Carsana, L.; Rizzuto, C.; et al. Pathophysiology of COVID-19-associated acute respiratory distress syndrome: A multicentre prospective observational study. Lancet Respir. Med. 2020, 8, 1201–1208. [Google Scholar] [CrossRef]
- Ferrando, C.; Suarez-Sipmann, F.; Mellado-Artigas, R.; Hernandez, M.; Gea, A.; Arruti, E.; Aldecoa, C.; Martinez-Palli, G.; Martinez-Gonzalez, M.A.; Slutsky, A.S.; et al. Clinical features, ventilatory management, and outcome of ARDS caused by COVID-19 are similar to other causes of ARDS. Intensive Care Med. 2020, 46, 2200–2211. [Google Scholar] [CrossRef]
- Torregiani, C.; Baratella, E.; Segalotti, A.; Ruaro, B.; Salton, F.; Confalonieri, P.; Tavano, S.; Lapadula, G.; Bozzi, C.; Confalonieri, M.; et al. Oscillometry Longitudinal Data on COVID-19 Acute Respiratory Syndrome Treated with Non-Invasive Respiratory Support. J. Clin. Med. 2024, 13, 1868. [Google Scholar] [CrossRef]
- Tonelli, R.; Fantini, R.; Tabbi, L.; Castaniere, I.; Pisani, L.; Pellegrino, M.R.; Della Casa, G.; D’Amico, R.; Girardis, M.; Nava, S.; et al. Early Inspiratory Effort Assessment by Esophageal Manometry Predicts Noninvasive Ventilation Outcome in De Novo Respiratory Failure. A Pilot Study. Am. J. Respir. Crit. Care Med. 2020, 202, 558–567. [Google Scholar] [CrossRef]
- Goligher, E.C.; Brochard, L.J.; Reid, W.D.; Fan, E.; Saarela, O.; Slutsky, A.S.; Kavanagh, B.P.; Rubenfeld, G.D.; Ferguson, N.D. Diaphragmatic myotrauma: A mediator of prolonged ventilation and poor patient outcomes in acute respiratory failure. Lancet. Respir. Med. 2019, 7, 90–98. [Google Scholar] [CrossRef]
- Goligher, E.C.; Dres, M.; Fan, E.; Rubenfeld, G.D.; Scales, D.C.; Herridge, M.S.; Vorona, S.; Sklar, M.C.; Rittayamai, N.; Lanys, A.; et al. Mechanical Ventilation-induced Diaphragm Atrophy Strongly Impacts Clinical Outcomes. Am. J. Respir. Crit. Care Med. 2017, 197, 204–213. [Google Scholar] [CrossRef]
- Spinelli, E.; Mauri, T.; Beitler, J.R.; Pesenti, A.; Brodie, D. Respiratory drive in the acute respiratory distress syndrome: Pathophysiology, monitoring, and therapeutic interventions. Intensive Care Med. 2020, 46, 606–618. [Google Scholar] [CrossRef]
- Brochard, L.; Slutsky, A.; Pesenti, A. Mechanical Ventilation to Minimize Progression of Lung Injury in Acute Respiratory Failure. Am. J. Respir. Crit. Care Med. 2017, 195, 438–442. [Google Scholar] [CrossRef]
- Goligher, E.C.; Dres, M.; Patel, B.K.; Sahetya, S.K.; Beitler, J.R.; Telias, I.; Yoshida, T.; Vaporidi, K.; Grieco, D.L.; Schepens, T.; et al. Lung- and Diaphragm-Protective Ventilation. Am. J. Respir. Crit. Care Med. 2020, 202, 950–961. [Google Scholar] [CrossRef]
- Vaporidi, K.; Akoumianaki, E.; Telias, I.; Goligher, E.C.; Brochard, L.; Georgopoulos, D. Respiratory Drive in Critically Ill Patients. Pathophysiology and Clinical Implications. Am. J. Respir. Crit. Care Med. 2020, 201, 20–32. [Google Scholar] [CrossRef] [PubMed]
- Alberti, A.; Gallo, F.; Fongaro, A.; Valenti, S.; Rossi, A. P0.1 is a useful parameter in setting the level of pressure support ventilation. Intensive Care Med. 1995, 21, 547–553. [Google Scholar] [CrossRef] [PubMed]
- Bellani, G.; Mauri, T.; Coppadoro, A.; Grasselli, G.; Patroniti, N.; Spadaro, S.; Sala, V.; Foti, G.; Pesenti, A. Estimation of patient’s inspiratory effort from the electrical activity of the diaphragm. Crit. Care Med. 2013, 41, 1483–1491. [Google Scholar] [CrossRef] [PubMed]
- Bertoni, M.; Telias, I.; Urner, M.; Long, M.; Del Sorbo, L.; Fan, E.; Sinderby, C.; Beck, J.; Liu, L.; Qiu, H.; et al. A novel non-invasive method to detect excessively high respiratory effort and dynamic transpulmonary driving pressure during mechanical ventilation. Crit. Care 2019, 23, 346. [Google Scholar] [CrossRef] [PubMed]
- Goligher, E.C.; Fan, E.; Herridge, M.S.; Murray, A.; Vorona, S.; Brace, D.; Rittayamai, N.; Lanys, A.; Tomlinson, G.; Singh, J.M.; et al. Evolution of Diaphragm Thickness during Mechanical Ventilation. Impact of Inspiratory Effort. Am. J. Respir. Crit. Care Med. 2015, 192, 1080–1088. [Google Scholar] [CrossRef]
- Vaschetto, R.; Cammarota, G.; Colombo, D.; Longhini, F.; Grossi, F.; Giovanniello, A.; Della Corte, F.; Navalesi, P. Effects of propofol on patient-ventilator synchrony and interaction during pressure support ventilation and neurally adjusted ventilatory assist. Crit. Care Med. 2014, 42, 74–82. [Google Scholar] [CrossRef]
- Esnault, P.; Cardinale, M.; Hraiech, S.; Goutorbe, P.; Baumstrack, K.; Prud’homme, E.; Bordes, J.; Forel, J.M.; Meaudre, E.; Papazian, L.; et al. High Respiratory Drive and Excessive Respiratory Efforts Predict Relapse of Respiratory Failure in Critically Ill Patients with COVID-19. Am. J. Respir. Crit. Care Med. 2020, 202, 1173–1178. [Google Scholar] [CrossRef]
- Lassola, S.; Miori, S.; Sanna, A.; Menegoni, I.; De Rosa, S.; Bellani, G.; Umbrello, M. Assessment of Inspiratory Effort in Spontaneously Breathing COVID-19 ARDS Patients Undergoing Helmet CPAP: A Comparison between Esophageal, Transdiaphragmatic and Central Venous Pressure Swing. Diagnostics 2023, 13, 1965. [Google Scholar] [CrossRef]
- de Vries, H.J.; Jonkman, A.H.; de Grooth, H.J.; Duitman, J.W.; Girbes, A.R.J.; Ottenheijm, C.A.C.; Schultz, M.J.; van de Ven, P.M.; Zhang, Y.; de Man, A.M.E.; et al. Lung- and Diaphragm-Protective Ventilation by Titrating Inspiratory Support to Diaphragm Effort: A Randomized Clinical Trial. Crit. Care Med. 2022, 50, 192–203. [Google Scholar] [CrossRef] [PubMed]
- Pham, T.; Montanya, J.; Telias, I.; Piraino, T.; Magrans, R.; Coudroy, R.; Damiani, L.F.; Mellado Artigas, R.; Madorno, M.; Blanch, L.; et al. Automated detection and quantification of reverse triggering effort under mechanical ventilation. Crit. Care 2021, 25, 60. [Google Scholar] [CrossRef]
- Di Mussi, R.; Spadaro, S.; Volta, C.A.; Bartolomeo, N.; Trerotoli, P.; Staffieri, F.; Pisani, L.; Iannuzziello, R.; Dalfino, L.; Murgolo, F.; et al. Continuous assessment of neuro-ventilatory drive during 12 h of pressure support ventilation in critically ill patients. Crit. Care 2020, 24, 652. [Google Scholar] [CrossRef] [PubMed]
- Di Mussi, R.; Spadaro, S.; Mirabella, L.; Volta, C.A.; Serio, G.; Staffieri, F.; Dambrosio, M.; Cinnella, G.; Bruno, F.; Grasso, S. Impact of prolonged assisted ventilation on diaphragmatic efficiency: NAVA versus PSV. Crit. Care 2016, 20, 1. [Google Scholar] [CrossRef] [PubMed]
- Telias, I.; Junhasavasdikul, D.; Rittayamai, N.; Piquilloud, L.; Chen, L.; Ferguson, N.D.; Goligher, E.C.; Brochard, L. Airway Occlusion Pressure As an Estimate of Respiratory Drive and Inspiratory Effort during Assisted Ventilation. Am. J. Respir. Crit. Care Med. 2020, 201, 1086–1098. [Google Scholar] [CrossRef]
- Telias, I.; Damiani, F.; Brochard, L. The airway occlusion pressure (P(0.1)) to monitor respiratory drive during mechanical ventilation: Increasing awareness of a not-so-new problem. Intensive Care Med. 2018, 44, 1532–1535. [Google Scholar] [CrossRef]
- Meinhardt, J.; Radke, J.; Dittmayer, C.; Franz, J.; Thomas, C.; Mothes, R.; Laue, M.; Schneider, J.; Brunink, S.; Greuel, S.; et al. Olfactory transmucosal SARS-CoV-2 invasion as a port of central nervous system entry in individuals with COVID-19. Nat. Neurosci. 2021, 24, 168–175. [Google Scholar] [CrossRef]
- Liu, L.; Liu, H.; Yang, Y.; Huang, Y.; Liu, S.; Beck, J.; Slutsky, A.S.; Sinderby, C.; Qiu, H. Neuroventilatory efficiency and extubation readiness in critically ill patients. Crit. Care 2012, 16, R143. [Google Scholar] [CrossRef]
- Roze, H.; Repusseau, B.; Perrier, V.; Germain, A.; Seramondi, R.; Dewitte, A.; Fleureau, C.; Ouattara, A. Neuro-ventilatory efficiency during weaning from mechanical ventilation using neurally adjusted ventilatory assist. Br. J. Anaesth. 2013, 111, 955–960. [Google Scholar] [CrossRef]
- Boscolo, A.; Sella, N.; Pettenuzzo, T.; Pistollato, E.; Calabrese, F.; Gregori, D.; Cammarota, G.; Dres, M.; Rea, F.; Navalesi, P.; et al. Diaphragm dysfunction predicts weaning outcome after bilateral lung transplant. Anesthesiology 2023, 140, 126–136. [Google Scholar] [CrossRef]
- Dres, M.; Schmidt, M.; Ferre, A.; Mayaux, J.; Similowski, T.; Demoule, A. Diaphragm electromyographic activity as a predictor of weaning failure. Intensive Care Med. 2012, 38, 2017–2025. [Google Scholar] [CrossRef]
- Meduri, G.U.; Bridges, L.; Shih, M.C.; Marik, P.E.; Siemieniuk, R.A.C.; Kocak, M. Prolonged glucocorticoid treatment is associated with improved ARDS outcomes: Analysis of individual patients’ data from four randomized trials and trial-level meta-analysis of the updated literature. Intensive Care Med. 2016, 42, 829–840. [Google Scholar] [CrossRef] [PubMed]
- Pham, T.; Heunks, L.; Bellani, G.; Madotto, F.; Aragao, I.; Beduneau, G.; Goligher, E.C.; Grasselli, G.; Laake, J.H.; Mancebo, J.; et al. Weaning from mechanical ventilation in intensive care units across 50 countries (WEAN SAFE): A multicentre, prospective, observational cohort study. Lancet. Respir. Med. 2023, 11, 465–476. [Google Scholar] [CrossRef] [PubMed]
- Kress, J.P.; Pohlman, A.S.; O’Connor, M.F.; Hall, J.B. Daily interruption of sedative infusions in critically ill patients undergoing mechanical ventilation. N. Engl. J. Med. 2000, 342, 1471–1477. [Google Scholar] [CrossRef] [PubMed]
- Sklar, M.C.; Madotto, F.; Jonkman, A.; Rauseo, M.; Soliman, I.; Damiani, L.F.; Telias, I.; Dubo, S.; Chen, L.; Rittayamai, N.; et al. Duration of diaphragmatic inactivity after endotracheal intubation of critically ill patients. Crit. Care 2021, 25, 26. [Google Scholar] [CrossRef]
- Ely, E.W.; Truman, B.; Shintani, A.; Thomason, J.W.; Wheeler, A.P.; Gordon, S.; Francis, J.; Speroff, T.; Gautam, S.; Margolin, R.; et al. Monitoring sedation status over time in ICU patients: Reliability and validity of the Richmond Agitation-Sedation Scale (RASS). JAMA 2003, 289, 2983–2991. [Google Scholar] [CrossRef]
- Bellani, G.; Laffey, J.G.; Pham, T.; Fan, E.; Brochard, L.; Esteban, A.; Gattinoni, L.; van Haren, F.; Larsson, A.; McAuley, D.F.; et al. Epidemiology, Patterns of Care, and Mortality for Patients with Acute Respiratory Distress Syndrome in Intensive Care Units in 50 Countries. JAMA 2016, 315, 788–800. [Google Scholar] [CrossRef]
- Colebatch, H.J.; Greaves, I.A.; Ng, C.K. Exponential analysis of elastic recoil and aging in healthy males and females. J. Appl. Physiol. Respir. Env. Exerc. Physiol. 1979, 47, 683–691. [Google Scholar] [CrossRef]
- Akoumianaki, E.; Maggiore, S.M.; Valenza, F.; Bellani, G.; Jubran, A.; Loring, S.H.; Pelosi, P.; Talmor, D.; Grasso, S.; Chiumello, D.; et al. The Application of Esophageal Pressure Measurement in Patients with Respiratory Failure. Am. J. Respir. Crit. Care Med. 2014, 189, 520–531. [Google Scholar] [CrossRef]

| Variables | n = 48 |
|---|---|
| Age, yrs | 58.2 (11.9) |
| Gender—male, n (%) | 34 (70.8) |
| BMI, kg/m2 | 28.1 (5.6) |
| Underlying comorbidities | |
| Obesity, n (%) | 14 (29.2) |
| Arterial hypertension, n (%) | 25 (52.1) |
| Diabetes, n (%) | 13 (27.1) |
| COPD, n (%) | 9 (18.8) |
| Malignancy, n (%) | 6 (12.5) |
| Chronic heart failure, n (%) | 1 (2.1) |
| Chronic renal failure, n (%) | 4 (8.3) |
| SOFA score | 7.4 (3.3) |
| SAPS II score | 37.5 (11.8) |
| Etiology | |
| COVID-19 pneumonia, n (%) | 16 (33) |
| Outcomes | |
| Patients who went from PSV to ACV within 48 h, n (%) | 3 (6.3) |
| Patients who went to RASS < −2 within 48 h, n (%) | 9 (18.8) |
| Composite outcome †, n (%) | 9 (18.8) |
| ICU mortality, n (%) | 4 (8.3) |
| Mortality at 60 days after ICU admission, n (%) | 3 (6.3) |
| Variables | |
|---|---|
| Ventilator Setting | |
| Peak airway pressure (cmH2O) | 17.5 [16.2–19.9] |
| PEEP (cmH2O) | 8 [7.4–9.7] |
| VT/PBW (mL/kg) | 7.4 [6–9.3] |
| Minute Ventilation (L/min) | 9.9 [7.8–11.8] |
| Respiratory Rate (b/min) | 20.5 [15.3–25.3] |
| Flow peak (L/s) | 0.7 [0.7–0.9] |
| ERS (cmH2O/mL) | 19.9 [14.1–24.8] |
| RRS (cmH2O/L/s) | 12.4 [10.4–15.4] |
| ΔPL,dyn (cmH2O) | 16.2 [12.2–20.5] |
| Respiratory Drive | |
| P0.1 (cmH2O) | 0.8 [0.4–1.9] |
| EAdi peak (µV) | 9.6 [4.7–16.6] |
| Ti,MECH (s) | 1 [0.8–1.2] |
| Ti,NEUR (s) | 0.8 [0.6–1] |
| Inspiratory duty cycle (Ti/Ttot) | 33.3 [27.7–38.4] |
| Neural inspiratory duty cycle (Tineu/Ttot) | 0.3 [0.2–0.3] |
| PEIdyn (cmH2O/µV) | 0.6 [0.4–1.8] |
| Neuroventilatory efficiency (mL/µV) | 50.8 [29–99.9] |
| Respiratory Effort | |
| ∆PmusEAdi (cmH2O) | −10.5 [−16.4–−5.1] |
| ΔPocc (cmH2O) | 7.9 [3.8–11.1] |
| ∆PmusΔPocc (cmH2O) | 7.9 [3.3–16] |
| PTP EAdi/min (cmH2O/s/min) | 95.6 [38.9–175.3] |
| PTPEAdi/b (cmH2O/s) | 4.9 [2.2–9] |
| Blood gas Exchange | |
| pH | 7.4 [7.4–7.5] |
| PaCO2, mmHg | 42 [39–48] |
| PaO2, mmHg | 95 [86–116] |
| HCO3−, mEq/L | 29 [27–32.8] |
| Parameter | Unadjusted Hazard Ratio | Adjusted Hazard Ratio | ||
|---|---|---|---|---|
| p | HR (95% CI) | p | HR (95% CI) | |
| COVID-19 (Ref = No-COVID) | 0.0064 | 8.9 (1.85–43.2) | 0.0502 | 6.96 (1–48.5) |
| Age | 0.4785 | 0.98 (0.93–1.04) | - | - |
| Patient severity (SOFA) | 0.0363 | 0.76 (0.6–0.98) | - | - |
| P/F ratio | 0.0264 | 0.98 (0.97–1.00) | 0.0884 | 0.99 (0.97–1.00) |
| Respiratory system compliance | 0.1738 | 0.97 (0.93–1.01) | - | - |
| Days of deep sedation | <0.0001 | 1.12 (1.07–1.17) | 0.0002 | 1.15 (1.07–1.24) |
| Days of NMBA | 0.1104 | 1.04 (0.99–1.08) | - | - |
| Dose of steroids | 0.0050 | 1.005 (1.002–1.009) | - | - |
| Days of mechanical ventilation | 0.0762 | 1.02 (1.00–1.05) | - | - |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Balzani, E.; Murgolo, F.; Pozzi, M.; Di Mussi, R.; Bartolomeo, N.; Simonetti, U.; Brazzi, L.; Spadaro, S.; Bellani, G.; Grasso, S.; et al. Respiratory Drive, Effort, and Lung-Distending Pressure during Transitioning from Controlled to Spontaneous Assisted Ventilation in Patients with ARDS: A Multicenter Prospective Cohort Study. J. Clin. Med. 2024, 13, 5227. https://doi.org/10.3390/jcm13175227
Balzani E, Murgolo F, Pozzi M, Di Mussi R, Bartolomeo N, Simonetti U, Brazzi L, Spadaro S, Bellani G, Grasso S, et al. Respiratory Drive, Effort, and Lung-Distending Pressure during Transitioning from Controlled to Spontaneous Assisted Ventilation in Patients with ARDS: A Multicenter Prospective Cohort Study. Journal of Clinical Medicine. 2024; 13(17):5227. https://doi.org/10.3390/jcm13175227
Chicago/Turabian StyleBalzani, Eleonora, Francesco Murgolo, Matteo Pozzi, Rossella Di Mussi, Nicola Bartolomeo, Umberto Simonetti, Luca Brazzi, Savino Spadaro, Giacomo Bellani, Salvatore Grasso, and et al. 2024. "Respiratory Drive, Effort, and Lung-Distending Pressure during Transitioning from Controlled to Spontaneous Assisted Ventilation in Patients with ARDS: A Multicenter Prospective Cohort Study" Journal of Clinical Medicine 13, no. 17: 5227. https://doi.org/10.3390/jcm13175227
APA StyleBalzani, E., Murgolo, F., Pozzi, M., Di Mussi, R., Bartolomeo, N., Simonetti, U., Brazzi, L., Spadaro, S., Bellani, G., Grasso, S., & Fanelli, V. (2024). Respiratory Drive, Effort, and Lung-Distending Pressure during Transitioning from Controlled to Spontaneous Assisted Ventilation in Patients with ARDS: A Multicenter Prospective Cohort Study. Journal of Clinical Medicine, 13(17), 5227. https://doi.org/10.3390/jcm13175227








