Unsupervised Pattern Analysis to Differentiate Multiple Sclerosis Phenotypes Using Principal Component Analysis on Various MRI Sequences
Abstract
1. Introduction
2. Methods
2.1. Participants
2.2. MRI Acquisition
2.3. MRI Post-Processing
2.4. Statistical Analysis
3. Results
3.1. Group Characteristics
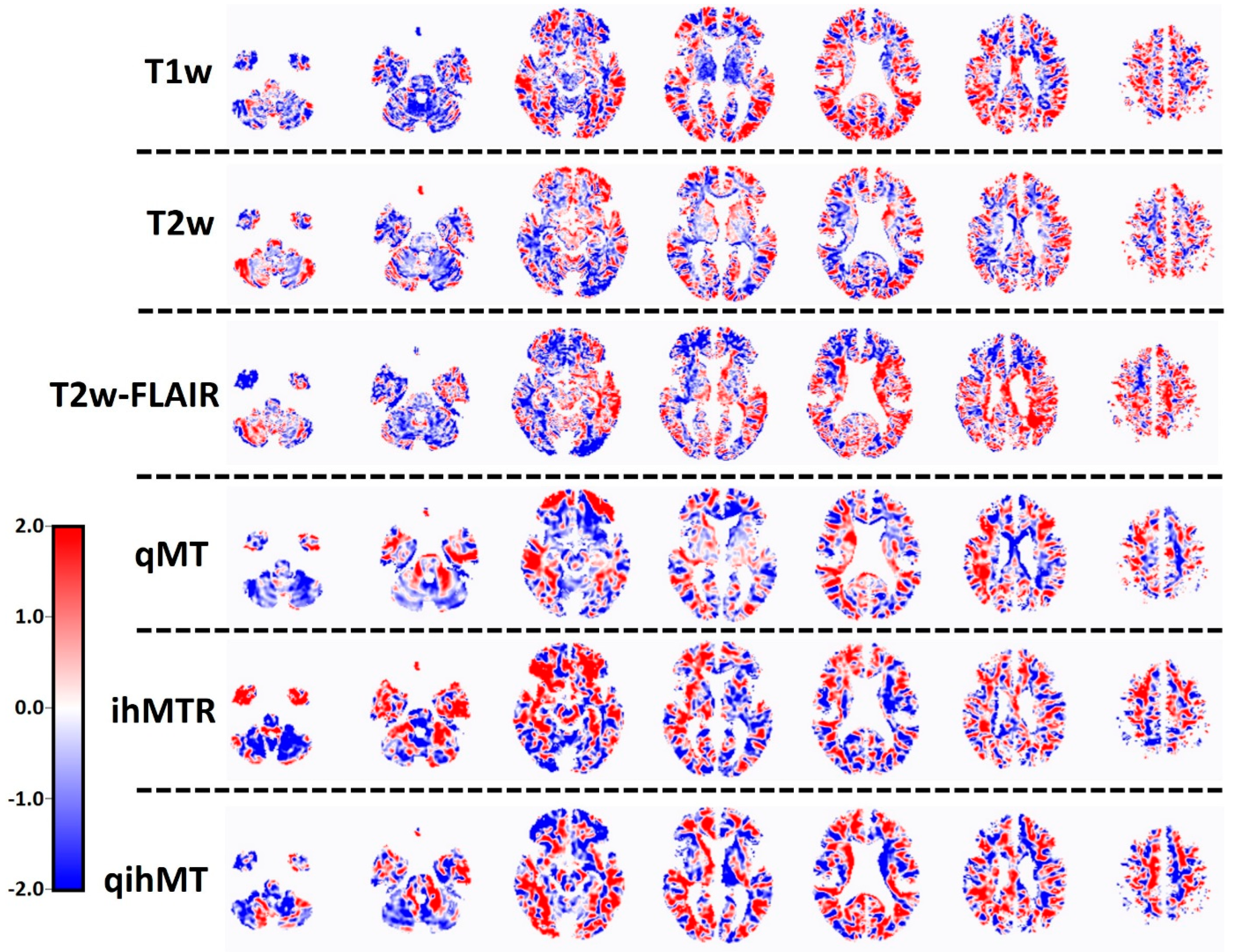
3.2. Discriminative Analysis of MRI Patterns for MS Phenotypes
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ramagopalan, S.V.; Dobson, R.; Meier, U.C.; Giovannoni, G. Multiple Sclerosis: Risk Factors, Prodromes, and Potential Causal Pathways. Lancet Neurol. 2010, 9, 727–739. [Google Scholar] [CrossRef]
- Traugott, U.; Reinherz, E.L.; Raine, C.S. Multiple Sclerosis: Distribution of T Cells, T Cell Subsets and Ia-Positive Macrophages in Lesions of Different Ages. J. Neuroimmunol. 1983, 4, 201–221. [Google Scholar] [CrossRef] [PubMed]
- Walton, C.; King, R.; Rechtman, L.; Kaye, W.; Leray, E.; Marrie, R.A.; Robertson, N.; La Rocca, N.; Uitdehaag, B.; van der Mei, I. Rising Prevalence of Multiple Sclerosis Worldwide: Insights from the Atlas of MS. Mult. Scler. J. 2020, 26, 1816–1821. [Google Scholar] [CrossRef]
- Poser, S.; Raun, N.E.; Poser, W. Age at Onset, Initial Symptomatology and the Course of Multiple Sclerosis. Acta Neurol. Scand. 1982, 66, 355–362. [Google Scholar] [CrossRef]
- Thompson, A.J.; Banwell, B.L.; Barkhof, F.; Carroll, W.M.; Coetzee, T.; Comi, G.; Correale, J.; Fazekas, F.; Filippi, M.; Freedman, M.S. Diagnosis of Multiple Sclerosis: 2017 Revisions of the McDonald Criteria. Lancet Neurol. 2018, 17, 162–173. [Google Scholar] [CrossRef] [PubMed]
- Lublin, F.D. New Multiple Sclerosis Phenotypic Classification. Eur. Neurol. 2014, 72, 1–5. [Google Scholar] [CrossRef]
- Lublin, F.D.; Reingold, S.C.; Cohen, J.A.; Cutter, G.R.; Sørensen, P.S.; Thompson, A.J.; Wolinsky, J.S.; Balcer, L.J.; Banwell, B.; Barkhof, F. Defining the Clinical Course of Multiple Sclerosis: The 2013 Revisions. Neurology 2014, 83, 278–286. [Google Scholar] [CrossRef] [PubMed]
- Baecher-Allan, C.; Kaskow, B.J.; Weiner, H.L. Multiple Sclerosis: Mechanisms and Immunotherapy. Neuron 2018, 97, 742–768. [Google Scholar] [CrossRef]
- Absinta, M.; Lassmann, H.; Trapp, B. Mechanisms Underlying Progression in Multiple Sclerosis. Curr. Opin. Neurol. 2020, 33, 277. [Google Scholar] [CrossRef]
- Montalban, X.; Hauser, S.L.; Kappos, L.; Arnold, D.L.; Bar-Or, A.; Comi, G.; De Seze, J.; Giovannoni, G.; Hartung, H.-P.; Hemmer, B. Ocrelizumab versus Placebo in Primary Progressive Multiple Sclerosis. N. Engl. J. Med. 2017, 376, 209–220. [Google Scholar] [CrossRef]
- Kappos, L.; Bar-Or, A.; Cree, B.A.C.; Fox, R.J.; Giovannoni, G.; Gold, R.; Vermersch, P.; Arnold, D.L.; Arnould, S.; Scherz, T. Siponimod versus Placebo in Secondary Progressive Multiple Sclerosis (EXPAND): A Double-Blind, Randomised, Phase 3 Study. Lancet 2018, 391, 1263–1273. [Google Scholar] [CrossRef]
- Matthews, P.M. Chronic Inflammation in Multiple Sclerosis—Seeing What Was Always There. Nat. Rev. Neurol. 2019, 15, 582–593. [Google Scholar] [CrossRef] [PubMed]
- Bagnato, F.; Gauthier, S.A.; Laule, C.; Moore, G.R.W.; Bove, R.; Cai, Z.; Cohen-Adad, J.; Harrison, D.M.; Klawiter, E.C.; Morrow, S.A. Imaging Mechanisms of Disease Progression in Multiple Sclerosis: Beyond Brain Atrophy. J. Neuroimaging 2020, 30, 251–266. [Google Scholar] [CrossRef] [PubMed]
- Polman, C.H.; Reingold, S.C.; Banwell, B.; Clanet, M.; Cohen, J.A.; Filippi, M.; Fujihara, K.; Havrdova, E.; Hutchinson, M.; Kappos, L. Diagnostic Criteria for Multiple Sclerosis: 2010 Revisions to the McDonald Criteria. Ann. Neurol. 2011, 69, 292–302. [Google Scholar] [CrossRef] [PubMed]
- Mallik, S.; Samson, R.S.; Wheeler-Kingshott, C.A.M.; Miller, D.H. Imaging Outcomes for Trials of Remyelination in Multiple Sclerosis. J. Neurol. Neurosurg. Psychiatry 2014, 85, 1396–1404. [Google Scholar] [CrossRef]
- van der Weijden, C.W.J.; Biondetti, E.; Gutmann, I.W.; Dijkstra, H.; McKerchar, R.; de Paula Faria, D.; de Vries, E.F.J.; Meilof, J.F.; Dierckx, R.A.J.O.; Prevost, V.H. Quantitative Myelin Imaging with MRI and PET: An Overview of Techniques and Their Validation Status. Brain 2022, 146, 1243–1266. [Google Scholar] [CrossRef]
- Moeller, J.R.; Strother, S.C.; Sidtis, J.J.; Rottenberg, D.A. Scaled Subprofile Model: A Statistical Approach to the Analysis of Functional Patterns in Positron Emission Tomographic Data. J. Cereb. Blood Flow Metab. 1987, 7, 649–658. [Google Scholar] [CrossRef]
- Teune, L.K.; Renken, R.J.; Mudali, D.; De Jong, B.M.; Dierckx, R.A.; Roerdink, J.B.T.M.; Leenders, K.L. Validation of Parkinsonian Disease-Related Metabolic Brain Patterns. Mov. Disord. 2013, 28, 547–551. [Google Scholar] [CrossRef]
- Peretti, D.E.; Renken, R.J.; Reesink, F.E.; de Jong, B.M.; De Deyn, P.P.; Dierckx, R.A.J.O.; Doorduin, J.; Boellaard, R.; García, D.V. Feasibility of Pharmacokinetic Parametric PET Images in Scaled Subprofile Modelling Using Principal Component Analysis. NeuroImage Clin. 2021, 30, 102625. [Google Scholar] [CrossRef]
- van der Weijden, C.W.J.; García, D.V.; Borra, R.J.H.; Thurner, P.; Meilof, J.F.; van Laar, P.-J.; Dierckx, R.A.J.O.; Gutmann, I.W.; de Vries, E.F.J. Myelin Quantification with MRI: A Systematic Review of Accuracy and Reproducibility. Neuroimage 2021, 226, 117561. [Google Scholar] [CrossRef]
- Kurtzke, J.F. Rating Neurologic Impairment in Multiple Sclerosis: An Expanded Disability Status Scale (EDSS). Neurology 1983, 33, 1444. [Google Scholar] [CrossRef]
- Ashburner, J.; Friston, K.J. Unified Segmentation. Neuroimage 2005, 26, 839–851. [Google Scholar] [CrossRef]
- Spetsieris, P.G.; Ma, Y.; Dhawan, V.; Eidelberg, D. Differential Diagnosis of Parkinsonian Syndromes Using PCA-Based Functional Imaging Features. Neuroimage 2009, 45, 1241–1252. [Google Scholar] [CrossRef] [PubMed]
- Spetsieris, P.G.; Eidelberg, D. Scaled Subprofile Modeling of Resting State Imaging Data in Parkinson’s Disease: Methodological Issues. Neuroimage 2011, 54, 2899–2914. [Google Scholar] [CrossRef]
- Meles, S.K.; Renken, R.J.; Pagani, M.; Teune, L.K.; Arnaldi, D.; Morbelli, S.; Nobili, F.; Van Laar, T.; Obeso, J.A.; Rodríguez-Oroz, M.C. Abnormal Pattern of Brain Glucose Metabolism in Parkinson’s Disease: Replication in Three European Cohorts. Eur. J. Nucl. Med. Mol. Imaging 2020, 47, 437–450. [Google Scholar] [CrossRef] [PubMed]
- Santangelo, G.; Altieri, M.; Gallo, A.; Trojano, L. Does Cognitive Reserve Play Any Role in Multiple Sclerosis? A Meta-Analytic Study. Mult. Scler. Relat. Disord. 2019, 30, 265–276. [Google Scholar] [CrossRef] [PubMed]
- Thornton, A.E.; Raz, N. Memory Impairment in Multiple Sclerosis: A Quantitative Review. Neuropsychology 1997, 11, 357. [Google Scholar] [CrossRef]
- Højsgaard Chow, H.; Schreiber, K.; Magyari, M.; Ammitzbøll, C.; Börnsen, L.; Romme Christensen, J.; Ratzer, R.; Soelberg Sørensen, P.; Sellebjerg, F. Progressive Multiple Sclerosis, Cognitive Function, and Quality of Life. Brain Behav. 2018, 8, e00875. [Google Scholar] [CrossRef]
- Zackowski, K.M.; Freeman, J.; Brichetto, G.; Centonze, D.; Dalgas, U.; DeLuca, J.; Ehde, D.; Elgott, S.; Fanning, V.; Feys, P. Prioritizing Progressive MS Rehabilitation Research: A Call from the International Progressive MS Alliance. Mult. Scler. J. 2021, 27, 989–1001. [Google Scholar] [CrossRef]
- Meles, S.K.; Pagani, M.; Arnaldi, D.; De Carli, F.; Dessi, B.; Morbelli, S.; Sambuceti, G.; Jonsson, C.; Leenders, K.L.; Nobili, F. The Alzheimer’s Disease Metabolic Brain Pattern in Mild Cognitive Impairment. J. Cereb. Blood Flow Metab. 2017, 37, 3643–3648. [Google Scholar] [CrossRef]
- Teune, L.K.; Renken, R.J.; de Jong, B.M.; Willemsen, A.T.; van Osch, M.J.; Roerdink, J.B.T.M.; Dierckx, R.A.; Leenders, K.L. Parkinson’s Disease-Related Perfusion and Glucose Metabolic Brain Patterns Identified with PCASL-MRI and FDG-PET Imaging. NeuroImage Clin. 2014, 5, 240–244. [Google Scholar] [CrossRef] [PubMed]
- Mato-Abad, V.; Labiano-Fontcuberta, A.; Rodríguez-Yáñez, S.; García-Vázquez, R.; Munteanu, C.R.; Andrade-Garda, J.; Domingo-Santos, A.; Galán Sánchez-Seco, V.; Aladro, Y.; Martínez-Ginés, M.L.; et al. Classification of Radiologically Isolated Syndrome and Clinically Isolated Syndrome with Machine-Learning Techniques. Eur. J. Neurol. 2019, 26, 1000–1005. [Google Scholar] [CrossRef] [PubMed]
- Yoo, Y.; Tang, L.Y.W.; Brosch, T.; Li, D.K.B.; Kolind, S.; Vavasour, I.; Rauscher, A.; MacKay, A.L.; Traboulsee, A.; Tam, R.C. Deep Learning of Joint Myelin and T1w MRI Features in Normal-Appearing Brain Tissue to Distinguish between Multiple Sclerosis Patients and Healthy Controls. NeuroImage Clin. 2018, 17, 169–178. [Google Scholar] [CrossRef] [PubMed]
- Lassmann, H.; Brück, W.; Lucchinetti, C.F. The Immunopathology of Multiple Sclerosis: An Overview. Brain Pathol. 2007, 17, 210–218. [Google Scholar] [CrossRef]
- Sombekke, M.H.; Vellinga, M.M.; Uitdehaag, B.M.J.; Barkhof, F.; Polman, C.H.; Arteta, D.; Tejedor, D.; Martinez, A.; Crusius, J.B.A.; Peña, A.S. Genetic Correlations of Brain Lesion Distribution in Multiple Sclerosis: An Exploratory Study. Am. J. Neuroradiol. 2011, 32, 695–703. [Google Scholar] [CrossRef]
| RRMS | PMS | |
|---|---|---|
| Number of participants | 30 | 20 |
| Gender (%male) | 30 | 45 |
| Age (y) | 37 (19–49) | 51 (33–62) |
| Education (y) | 13 (6–20) | 11 (5–20) |
| EDSS | 2.5 (1–6) | 6.5 (3.5–7.5) |
| Number of lesions | 15 (1–37) | 17 (2–32) |
| Lesion volume (mL) | 10.3 (0.4–77.6) | 10.6 (0.1–91.7) |
| Image | Success% | LOOCV |
|---|---|---|
| T1w | 85% | Yes |
| T2w | 96% | Yes |
| T2w-FLAIR | 93% | Yes |
| MTR | 96% | No |
| qMT | 94% | Yes |
| ihMTR | 74% | Yes |
| qihMT | 77% | Yes |
| AUC | Specificity | Sensitivity | NPV | PPV | |
|---|---|---|---|---|---|
| T1w | 0.68 | 60% 53% | 87% 93% | 82% 89% | 68% 67% |
| T2w | 0.58 | 60% | 67% | 75% | 71% |
| T2w-FLAIR | 0.46 | 87% | 27% | 58% | 88% |
| MTR | - | - | - | - | - |
| qMT | 0.61 | 80% | 47% | 83% | 65% |
| 60% | 67% | 75% | 71% | ||
| 47% | 80% | 65% | 83% | ||
| ihMTR | 0.58 | 53% | 87% | 88% | 68% |
| qihMT | 0.70 | 87% | 67% | 72% | 83% |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
van der Weijden, C.W.J.; Pitombeira, M.S.; Peretti, D.E.; Campanholo, K.R.; Kolinger, G.D.; Rimkus, C.M.; Buchpiguel, C.A.; Dierckx, R.A.J.O.; Renken, R.J.; Meilof, J.F.; et al. Unsupervised Pattern Analysis to Differentiate Multiple Sclerosis Phenotypes Using Principal Component Analysis on Various MRI Sequences. J. Clin. Med. 2024, 13, 5234. https://doi.org/10.3390/jcm13175234
van der Weijden CWJ, Pitombeira MS, Peretti DE, Campanholo KR, Kolinger GD, Rimkus CM, Buchpiguel CA, Dierckx RAJO, Renken RJ, Meilof JF, et al. Unsupervised Pattern Analysis to Differentiate Multiple Sclerosis Phenotypes Using Principal Component Analysis on Various MRI Sequences. Journal of Clinical Medicine. 2024; 13(17):5234. https://doi.org/10.3390/jcm13175234
Chicago/Turabian Stylevan der Weijden, Chris W. J., Milena S. Pitombeira, Débora E. Peretti, Kenia R. Campanholo, Guilherme D. Kolinger, Carolina M. Rimkus, Carlos Alberto Buchpiguel, Rudi A. J. O. Dierckx, Remco J. Renken, Jan F. Meilof, and et al. 2024. "Unsupervised Pattern Analysis to Differentiate Multiple Sclerosis Phenotypes Using Principal Component Analysis on Various MRI Sequences" Journal of Clinical Medicine 13, no. 17: 5234. https://doi.org/10.3390/jcm13175234
APA Stylevan der Weijden, C. W. J., Pitombeira, M. S., Peretti, D. E., Campanholo, K. R., Kolinger, G. D., Rimkus, C. M., Buchpiguel, C. A., Dierckx, R. A. J. O., Renken, R. J., Meilof, J. F., de Vries, E. F. J., & de Paula Faria, D. (2024). Unsupervised Pattern Analysis to Differentiate Multiple Sclerosis Phenotypes Using Principal Component Analysis on Various MRI Sequences. Journal of Clinical Medicine, 13(17), 5234. https://doi.org/10.3390/jcm13175234







