Interrater Variability of ML-Based CT-FFR in Patients without Obstructive CAD before TAVR: Influence of Image Quality, Coronary Artery Calcifications, and Location of Measurement
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Patient Population
2.2. CT Acquisition
2.3. Image Analysis
2.4. Statistics
3. Results
3.1. Study Population
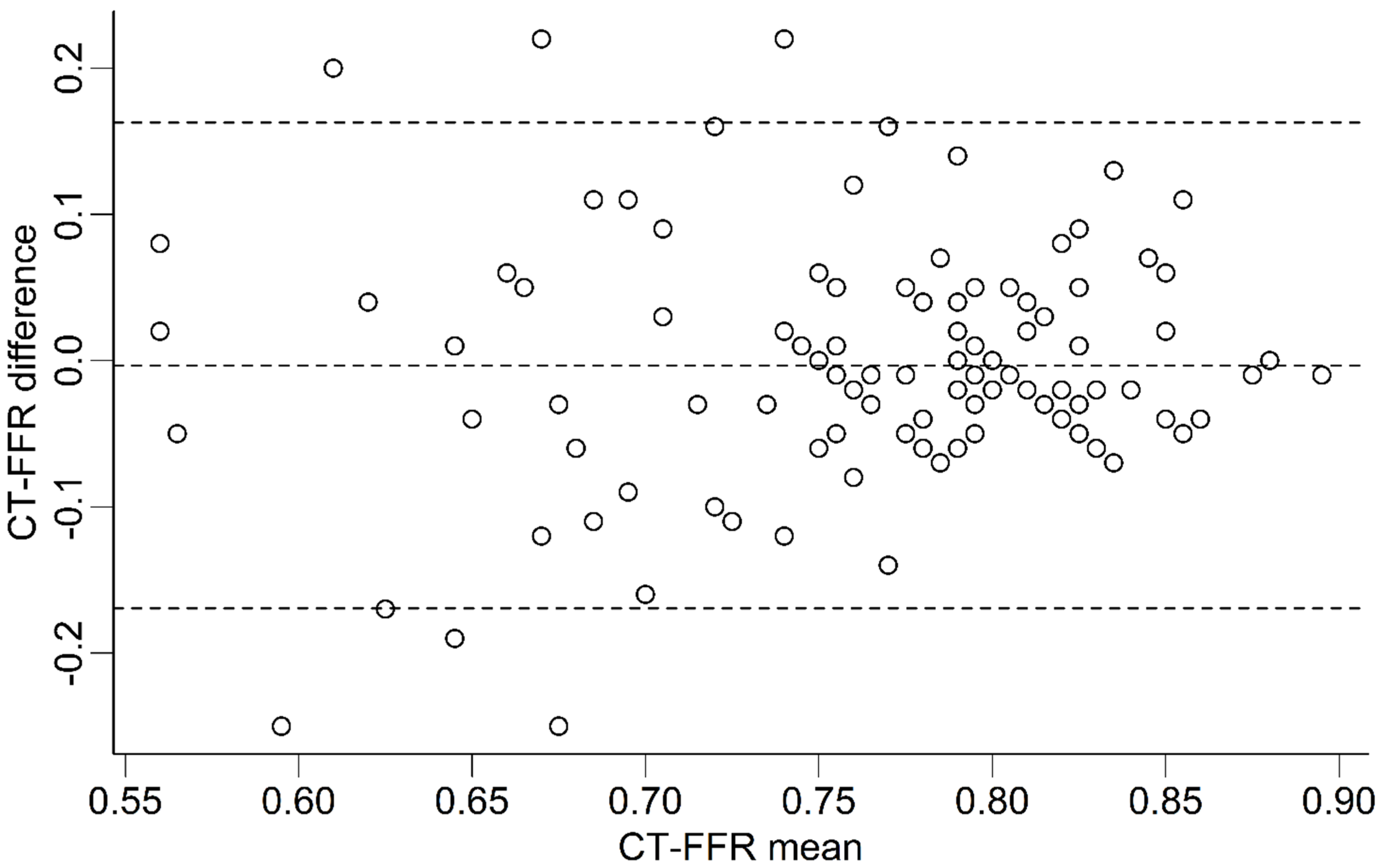
3.2. Absolute Differences
3.3. Interobserver Variability
3.4. Diagnostic Performance
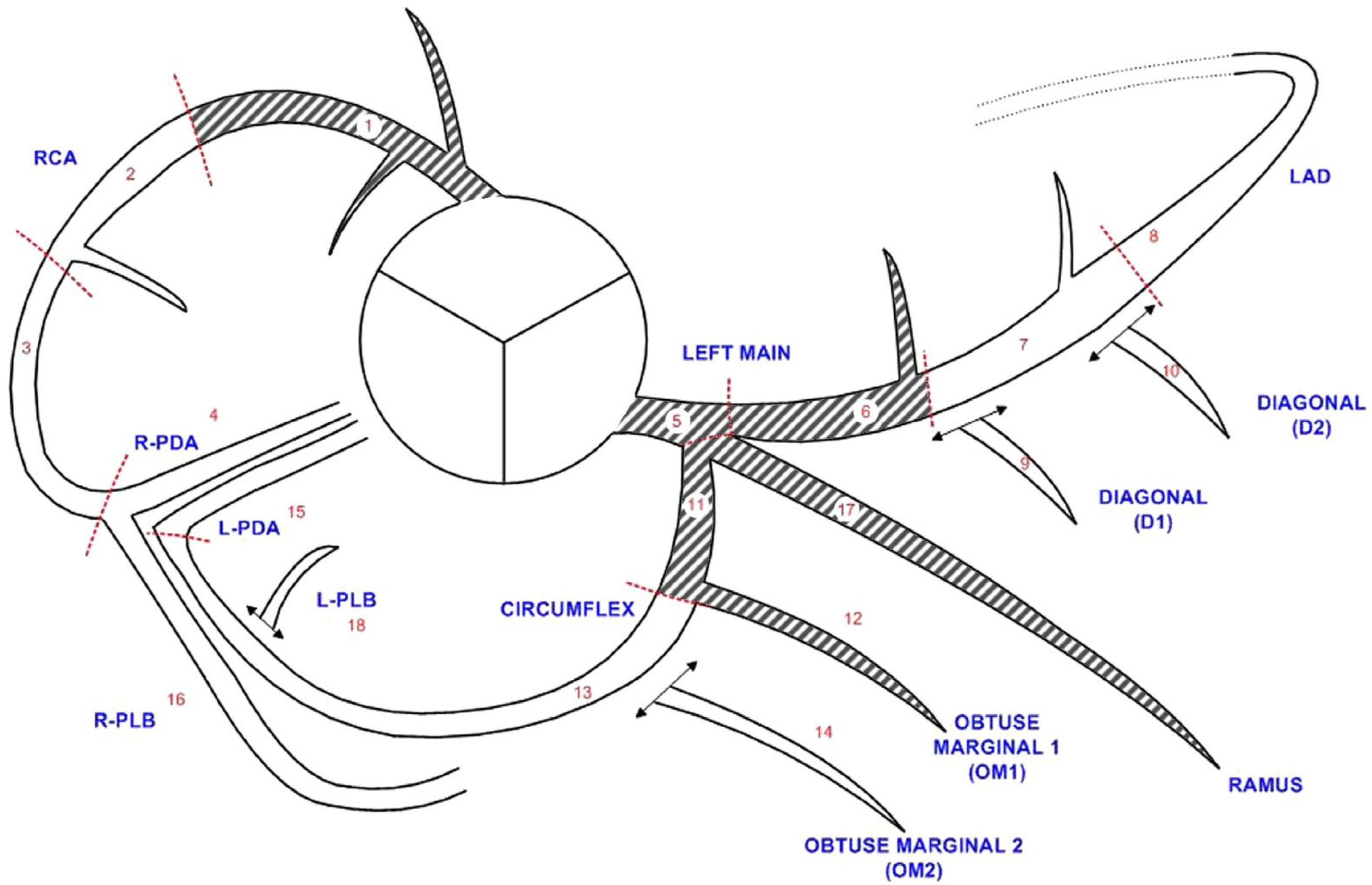
3.5. Localization of Measurement
3.6. Influence of Image Quality and Coronary Artery Calcifications
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| AS | aortic stenosis |
| CAC | coronary artery calcium score |
| CAD | coronary artery disease |
| CAD+ | positive for coronary artery disease |
| CAD− | negative for coronary artery disease |
| cCTA | coronary CT-angiography |
| CFD | computational fluid dynamics |
| CT-FFR | CT-derived fractional flow reserve |
| ICA | invasive coronary angiography |
| ICC | intra-class correlation coefficient |
| ML | machine learning |
| LM | left main coronary artery |
| LAD | left anterior descending coronary artery |
| LCX | circumflex coronary artery |
| QCA | quantitative coronary angiography |
| RCA | right coronary artery |
| TAVR | transcatheter aortic valve replacement |
References
- Maurovich-Horvat, P.; Bosserdt, M.; Kofoed, K.F.; Rieckmann, N.; Benedek, T.; Donnelly, P.; Rodriguez-Palomares, J.; Erglis, A.; Štěchovský, C.; Šakalyte, G.; et al. CT or Invasive Coronary Angiography in Stable Chest Pain. N. Engl. J. Med. 2022, 386, 1591–1602. [Google Scholar] [CrossRef] [PubMed]
- van den Boogert, T.P.W.; Vendrik, J.; Claessen, B.E.P.M.; Baan, J.; Beijk, M.A.; Limpens, J.; Boekholdt, S.A.M.; Hoek, R.; Planken, R.N.; Henriques, J.P. CTCA for Detection of Significant Coronary Artery Disease in Routine TAVI Work-up: A Systematic Review and Meta-Analysis. Neth. Heart J. 2018, 26, 591–599. [Google Scholar] [CrossRef] [PubMed]
- Gohmann, R.F.; Lauten, P.; Seitz, P.; Krieghoff, C.; Lücke, C.; Gottschling, S.; Mende, M.; Weiß, S.; Wilde, J.; Kiefer, P.; et al. Combined Coronary CT-Angiography and TAVI-Planning: A Contrast-Neutral Routine Approach for Ruling-Out Significant Coronary Artery Disease. J. Clin. Med. 2020, 9, 1623. [Google Scholar] [CrossRef] [PubMed]
- Coenen, A.; Kim, Y.-H.; Kruk, M.; Tesche, C.; De Geer, J.; Kurata, A.; Lubbers, M.L.; Daemen, J.; Itu, L.; Rapaka, S.; et al. Diagnostic Accuracy of a Machine-Learning Approach to Coronary Computed Tomographic Angiography–Based Fractional Flow Reserve. Circ. Cardiovasc. Imaging 2018, 11, e007217. [Google Scholar] [CrossRef]
- Gohmann, R.F.; Pawelka, K.; Seitz, P.; Majunke, N.; Heiser, L.; Renatus, K.; Desch, S.; Lauten, P.; Holzhey, D.; Noack, T.; et al. Combined CCTA and TAVR Planning for Ruling Out Significant CAD: Added Value of ML-Based CT-FFR. JACC Cardiovasc. Imaging 2022, 15, 476–486. [Google Scholar] [CrossRef]
- Taylor, C.A.; Fonte, T.A.; Min, J.K. Computational Fluid Dynamics Applied to Cardiac Computed Tomography for Noninvasive Quantification of Fractional Flow Reserve: Scientific Basis. J. Am. Coll. Cardiol. 2013, 61, 2233–2241. [Google Scholar] [CrossRef]
- Itu, L.; Rapaka, S.; Passerini, T.; Georgescu, B.; Schwemmer, C.; Schoebinger, M.; Flohr, T.; Sharma, P.; Comaniciu, D. A Machine-Learning Approach for Computation of Fractional Flow Reserve from Coronary Computed Tomography. J. Appl. Physiol. 2016, 121, 42–52. [Google Scholar] [CrossRef]
- Langenbach, M.C.; Langenbach, I.L.; Foldyna, B.; Mauri, V.; Klein, K.; Macherey-Meyer, S.; Heyne, S.; Meertens, M.; Lee, S.; Baldus, S.; et al. Advanced CT Measures of Coronary Artery Disease with Intermediate Stenosis in Patients with Severe Aortic Valve Stenosis. Eur. Radiol. 2024, 34, 4897–4908. [Google Scholar] [CrossRef]
- Brandt, V.; Schoepf, U.J.; Aquino, G.J.; Bekeredjian, R.; Varga-Szemes, A.; Emrich, T.; Bayer, R.R.; Schwarz, F.; Kroencke, T.J.; Tesche, C.; et al. Impact of Machine-Learning-Based Coronary Computed Tomography Angiography-Derived Fractional Flow Reserve on Decision-Making in Patients with Severe Aortic Stenosis Undergoing Transcatheter Aortic Valve Replacement. Eur. Radiol. 2022, 32, 6008–6016. [Google Scholar] [CrossRef]
- Michail, M.; Ihdayhid, A.R.; Comella, A.; Thakur, U.; Cameron, J.D.; McCormick, L.M.; Gooley, R.P.; Nicholls, S.J.; Mathur, A.; Hughes, A.D.; et al. Feasibility and Validity of Computed Tomography-Derived Fractional Flow Reserve in Patients With Severe Aortic Stenosis: The CAST-FFR Study. Circ. Cardiovasc. Interv. 2021, 14, E009586. [Google Scholar] [CrossRef]
- Peper, J.; Becker, L.M.; van den Berg, H.; Bor, W.L.; Brouwer, J.; Nijenhuis, V.J.; van Ginkel, D.J.; Rensing, B.J.M.W.; ten Berg, J.M.; Timmers, L.; et al. Diagnostic Performance of CCTA and CT-FFR for the Detection of CAD in TAVR Work-Up. JACC Cardiovasc. Interv. 2022, 15, 1140–1149. [Google Scholar] [CrossRef] [PubMed]
- Wienemann, H.; Langenbach, M.C.; Mauri, V.; Banazadeh, M.; Klein, K.; Hohmann, C.; Lee, S.; Breidert, I.; Hof, A.; Eghbalzadeh, K.; et al. Feasibility and Comparison of Resting Full-Cycle Ratio and Computed Tomography Fractional Flow Reserve in Patients with Severe Aortic Valve Stenosis. J. Cardiovasc. Dev. Dis. 2022, 9, 116. [Google Scholar] [CrossRef] [PubMed]
- Nørgaard, B.L.; Fairbairn, T.A.; Safian, R.D.; Rabbat, M.G.; Ko, B.; Jensen, J.M.; Nieman, K.; Chinnaiyan, K.M.; Sand, N.P.; Matsuo, H.; et al. Coronary CT Angiography-Derived Fractional Flow Reserve Testing in Patients with Stable Coronary Artery Disease: Recommendations on Interpretation and Reporting. Radiol. Cardiothorac. Imaging 2019, 1, e190050. [Google Scholar] [CrossRef] [PubMed]
- Gohmann, R.F.; Seitz, P.; Pawelka, K.; Majunke, N.; Schug, A.; Heiser, L.; Renatus, K.; Desch, S.; Lauten, P.; Holzhey, D.; et al. Clinical Medicine Combined Coronary CT-Angiography and TAVI Planning: Utility of CT-FFR in Patients with Morphologically Ruled-Out Obstructive Coronary Artery Disease. J. Clin. Med. 2022, 11, 1331. [Google Scholar] [CrossRef]
- De Bruyne, B.; Hersbach, F.; Pijls, N.H.J.; Bartunek, J.; Bech, J.W.; Heyndrickx, G.R.; Gould, K.L.; Wijns, W. Abnormal Epicardial Coronary Resistance in Patients With Diffuse Atherosclerosis but “Normal” Coronary Angiography. Circulation 2001, 104, 2401–2406. [Google Scholar] [CrossRef]
- Leipsic, J.; Abbara, S.; Achenbach, S.; Cury, R.; Earls, J.P.; Mancini, G.J.; Nieman, K.; Pontone, G.; Raff, G.L. SCCT Guidelines for the Interpretation and Reporting of Coronary CT Angiography: A Report of the Society of Cardiovascular Computed Tomography Guidelines Committee. J. Cardiovasc. Comput. Tomogr. 2014, 8, 342–358. [Google Scholar] [CrossRef] [PubMed]
- Gohmann, R.F.; Schug, A.; Pawelka, K.; Seitz, P.; Majunke, N.; El Hadi, H.; Heiser, L.; Renatus, K.; Desch, S.; Leontyev, S.; et al. Interrater Variability of ML-Based CT-FFR during TAVR-Planning: Influence of Image Quality and Coronary Artery Calcifications. Front. Cardiovasc. Med. 2023, 10, 1301619. [Google Scholar] [CrossRef]
- Chinnaiyan, K.M.; Akasaka, T.; Amano, T.; Bax, J.J.; Blanke, P.; De Bruyne, B.; Kawasaki, T.; Leipsic, J.; Matsuo, H.; Morino, Y.; et al. Rationale, Design and Goals of the HeartFlow Assessing Diagnostic Value of Non-Invasive FFRCT in Coronary Care (ADVANCE) Registry. J. Cardiovasc. Comput. Tomogr. 2017, 11, 62–67. [Google Scholar] [CrossRef]
- Kottner, J.; Audigé, L.; Brorson, S.; Donner, A.; Gajewski, B.J.; Hróbjartsson, A.; Roberts, C.; Shoukri, M.; Streiner, D.L. Guidelines for Reporting Reliability and Agreement Studies (GRRAS) Were Proposed. J. Clin. Epidemiol. 2011, 64, 96–106. [Google Scholar] [CrossRef]
- Shrout, P.E.; Fleiss, J.L. Intraclass Correlations: Uses in Assessing Rater Reliability. Psychol. Bull. 1979, 86, 420–428. [Google Scholar] [CrossRef]
- Cicchetti, D.V. Guidelines, Criteria, and Rules of Thumb for Evaluating Normed and Standardized Assessment Instruments in Psychology. Psychol. Assess. 1994, 6, 284–290. [Google Scholar] [CrossRef]
- Gaur, S.; Bezerra, H.G.; Lassen, J.F.; Christiansen, E.H.; Tanaka, K.; Jensen, J.M.; Oldroyd, K.G.; Leipsic, J.; Achenbach, S.; Kaltoft, A.K.; et al. Fractional Flow Reserve Derived from Coronary CT Angiography: Variation of Repeated Analyses. J. Cardiovasc. Comput. Tomogr. 2014, 8, 307–314. [Google Scholar] [CrossRef]
- Yang, D.H.; Kim, Y.H.; Roh, J.H.; Kang, J.W.; Ahn, J.M.; Kweon, J.; Lee, J.B.; Choi, S.H.; Shin, E.S.; Park, D.W.; et al. Diagnostic Performance of On-Site CT-Derived Fractional Flow Reserve versus CT Perfusion. Eur. Heart J. Cardiovasc. Imaging 2017, 18, 432–440. [Google Scholar] [CrossRef]
- Donnelly, P.M.; Kolossváry, M.; Karády, J.; Ball, P.A.; Kelly, S.; Fitzsimons, D.; Spence, M.S.; Celeng, C.; Horváth, T.; Szilveszter, B.; et al. Experience With an On-Site Coronary Computed Tomography-Derived Fractional Flow Reserve Algorithm for the Assessment of Intermediate Coronary Stenoses. Am. J. Cardiol. 2018, 121, 9–13. [Google Scholar] [CrossRef]
- Giannopoulos, A.A.; Keller, L.; Sepulcri, D.; Boehm, R.; Garefa, C.; Venugopal, P.; Mitra, J.; Ghose, S.; Deak, P.; Pack, J.D.; et al. High-Speed On-Site Deep Learning-Based FFR-CT Algorithm: Evaluation Using Invasive Angiography as the Reference Standard. AJR Am. J. Roentgenol. 2023, 221, 460–470. [Google Scholar] [CrossRef] [PubMed]
- Ihdayhid, A.R.; Sakaguchi, T.; Kerrisk, B.; Hislop-Jambrich, J.; Fujisawa, Y.; Nerlekar, N.; Cameron, J.D.; Seneviratne, S.K.; Ko, B.S. Influence of Operator Expertise and Coronary Luminal Segmentation Technique on Diagnostic Performance, Precision and Reproducibility of Reduced-Order CT-Derived Fractional Flow Reserve Technique. J. Cardiovasc. Comput. Tomogr. 2020, 14, 356–362. [Google Scholar] [CrossRef] [PubMed]
- Kumamaru, K.K.; Angel, E.; Sommer, K.N.; Iyer, V.; Wilson, M.F.; Agrawal, N.; Bhardwaj, A.; Kattel, S.B.; Kondziela, S.; Malhotra, S.; et al. Inter- and Intraoperator Variability in Measurement of On-Site CT-Derived Fractional Flow Reserve Based on Structural and Fluid Analysis: A Comprehensive Analysis. Radiol. Cardiothorac. Imaging 2019, 1, e180012. [Google Scholar] [CrossRef]
- Nicol, E.D.; Stirrup, J.; Roughton, M.; Padley, S.P.G.; Rubens, M.B. 64-Channel Cardiac Computed Tomography: Intraobserver and Interobserver Variability (Part 1): Coronary Angiography. J. Comput. Assist. Tomogr. 2009, 33, 161–168. [Google Scholar] [CrossRef]
- Kerl, J.M.; Schoepf, U.J.; Bauer, R.W.; Tekin, T.; Costello, P.; Vogl, T.J.; Herzog, C. 64-Slice Multidetector-Row Computed Tomography in the Diagnosis of Coronary Artery Disease: Interobserver Agreement among Radiologists with Varied Levels of Experience on a per-Patient and per-Segment Basis. J. Thorac. Imaging 2012, 27, 29–35. [Google Scholar] [CrossRef]
- Murphy, M.L.; Galbraith, J.E.; de Soyza, N. The Reliability of Coronary Angiogram Interpretation: An Angiographic-Pathologic Correlation with a Comparison of Radiographic Views. Am. Heart J. 1979, 97, 578–584. [Google Scholar] [CrossRef]
- Cook, C.M.; Petraco, R.; Shun-Shin, M.J.; Ahmad, Y.; Nijjer, S.; Al-Lamee, R.; Kikuta, Y.; Shiono, Y.; Mayet, J.; Francis, D.P.; et al. Diagnostic Accuracy of Computed Tomography-Derived Fractional Flow Reserve: A Systematic Review. JAMA Cardiol. 2017, 2, 803–810. [Google Scholar] [CrossRef] [PubMed]
- Tanigaki, T.; Emori, H.; Kawase, Y.; Kubo, T.; Omori, H.; Shiono, Y.; Sobue, Y.; Shimamura, K.; Hirata, T.; Matsuo, Y.; et al. QFR Versus FFR Derived From Computed Tomography for Functional Assessment of Coronary Artery Stenosis. JACC Cardiovasc. Interv. 2019, 12, 2050–2059. [Google Scholar] [CrossRef]
- Rajiah, P.; Cummings, K.W.; Williamson, E.; Young, P.M. CT Fractional Flow Reserve: A Practical Guide to Application, Interpretation, and Problem Solving. Radiographics 2022, 42, 340–358. [Google Scholar] [CrossRef] [PubMed]
- Tsugu, T.; Tanaka, K.; Belsack, D.; Nagatomo, Y.; Tsugu, M.; Argacha, J.F.; Cosyns, B.; Buls, N.; De Maeseneer, M.; De Mey, J. Impact of Vessel Morphology on CT-Derived Fractional-Flow-Reserve in Non-Obstructive Coronary Artery Disease in Right Coronary Artery. Eur. Radiol. 2024, 34, 1836–1845. [Google Scholar] [CrossRef]
- Van Hamersvelt, R.W.; Voskuil, M.; De Jong, P.A.; Willemink, M.J.; Išgum, I.; Leiner, T. Diagnostic Performance of On-Site Coronary CT Angiography–Derived Fractional Flow Reserve Based on Patient-Specific Lumped Parameter Models. Radiol. Cardiothorac. Imaging 2019, 1, e190036. [Google Scholar] [CrossRef] [PubMed]
- Yan, H.; Gao, Y.; Zhao, N.; Geng, W.; Hou, Z.; An, Y.; Zhang, J.; Lu, B. Change in Computed Tomography-Derived Fractional Flow Reserve Across the Lesion Improve the Diagnostic Performance of Functional Coronary Stenosis. Front. Cardiovasc. Med. 2022, 8, 788703. [Google Scholar] [CrossRef]
- Cami, E.; Tagami, T.; Raff, G.; Fonte, T.A.; Renard, B.; Gallagher, M.J.; Chinnaiyan, K.; Bilolikar, A.; Fan, A.; Hafeez, A.; et al. Assessment of Lesion-Specific Ischemia Using Fractional Flow Reserve (FFR) Profiles Derived from Coronary Computed Tomography Angiography (FFRCT) and Invasive Pressure Measurements (FFRINV): Importance of the Site of Measurement and Implications for Patient Referral for Invasive Coronary Angiography and Percutaneous Coronary Intervention. J. Cardiovasc. Comput. Tomogr. 2018, 12, 480–492. [Google Scholar] [CrossRef]
- Chen, M.; Almeida, S.O.; Sayre, J.W.; Karlsberg, R.P.; Packard, R.R.S. Distal-Vessel Fractional Flow Reserve by Computed Tomography to Monitor Epicardial Coronary Artery Disease. Eur. Heart J. Cardiovasc. Imaging 2024, 25, 163–172. [Google Scholar] [CrossRef]
- Renker, M.; Baumann, S.; Hamm, C.W.; Tesche, C.; Kim, W.K.; Savage, R.H.; Coenen, A.; Nieman, K.; De Geer, J.; Persson, A.; et al. Influence of Coronary Stenosis Location on Diagnostic Performance of Machine Learning-Based Fractional Flow Reserve from CT Angiography. J. Cardiovasc. Comput. Tomogr. 2021, 15, 492–498. [Google Scholar] [CrossRef]
- Knuuti, J.; Wijns, W.; Saraste, A.; Capodanno, D.; Barbato, E.; Funck-Brentano, C.; Prescott, E.; Storey, R.F.; Deaton, C.; Cuisset, T.; et al. 2019 ESC Guidelines for the Diagnosis and Management of Chronic Coronary Syndromes: The Task Force for the Diagnosis and Management of Chronic Coronary Syndromes of the European Society of Cardiology (ESC). Eur. Heart J. 2020, 41, 407–477. [Google Scholar] [CrossRef]
- Tesche, C.; Otani, K.; De Cecco, C.N.; Coenen, A.; De Geer, J.; Kruk, M.; Kim, Y.H.; Albrecht, M.H.; Baumann, S.; Renker, M.; et al. Influence of Coronary Calcium on Diagnostic Performance of Machine Learning CT-FFR: Results From MACHINE Registry. JACC Cardiovasc. Imaging 2020, 13, 760–770. [Google Scholar] [CrossRef] [PubMed]
| Level of Observation | n | Difference | 95% CI | p | ICC | 95% CI | p | RoR % | 95% CI | |
|---|---|---|---|---|---|---|---|---|---|---|
| Patient | 109 | −0.005 (−0.09 to 0.04) | −0.02, 0.01 | 0.47 | 0.421 | 0.25, 0.56 | <0.001 | 29.4 | 21.6, 38.5 | |
| Vessel | RCA | 109 | 0.0 (−0.03 to 0.05) | −0.01, 0.02 | 0.62 | 0.701 | 0.59, 0.79 | <0.001 | 26.6 | 19.2, 35.6 |
| LM | 109 | 0.0 (0.00 to 0.01) | 0.00, 0.01 | 0.14 | 0.507 | 0.35, 0.63 | <0.001 | 0.0 | 0.0, 3.4 | |
| LAD | 109 | −0.015 (−0.08 to 0.04) | −0.03, 0.01 | 0.12 | 0.334 | 0.16, 0.49 | <0.001 | 31.2 | 23.3, 40.4 | |
| LCX | 109 | 0.00 (−0.05 to 0.05) | −0.02, 0.01 | 0.76 | 0.588 | 0.45, 0.70 | <0.001 | 20.2 | 13.7, 28.7 | |
| Segments | S1 | 109 | 0.01 (−0.01 to 0.01) | 0.01, 0.02 | <0.001 | 0.498 | 0.34, 0.63 | <0.001 | 0.0 | 0.0, 3.4 |
| S2 | 108 | 0.015 (−0.01 to 0.03) | 0.01, 0.02 | <0.001 | 0.725 | 0.62, 0.80 | <0.001 | 1.9 | 0.5, 6.5 | |
| S3 | 101 | 0.015 (−0.02 to 0.04) | 0.01, 0.03 | 0.003 | 0.724 | 0.62, 0.81 | <0.001 | 13.9 | 8.4, 21.9 | |
| S4 | 76 | −0.005 (−0.04 to 0.03) | −0.02, 0.01 | 0.46 | 0.73 | 0.61, 0.82 | <0.001 | 28.9 | 20.0, 40.0 | |
| S16 | 80 | 0.00 (−0.04 to 0.04) | −0.01, 0.02 | 0.83 | 0.676 | 0.54, 0.78 | <0.001 | 21.2 | 13.7, 31.4 | |
| S5 | 109 | 0.00 (0.00 to 0.01) | 0.00, 0.01 | 0.14 | 0.507 | 0.35, 0.63 | <0.001 | 0.0 | 0.0, 3.4 | |
| S6 | 109 | 0.015 (−0.01 to 0.02) | 0.01, 0.02 | <0.001 | 0.432 | 0.27, 0.57 | <0.001 | 0.9 | 0.2, 5.0 | |
| S7 | 109 | 0.00 (−0.05 to 0.03) | −0.02, 0.01 | 0.81 | 0.349 | 0.17, 0.50 | <0.001 | 9.2 | 5.1, 16.1 | |
| S8 | 108 | −0.01 (−0.08 to 0.03) | −0.03, 0.01 | 0.17 | 0.362 | 0.19, 0.52 | <0.001 | 29.6 | 21.8, 38.8 | |
| S9 | 88 | 0.00 (−0.05 to 0.04) | −0.02, 0.02 | 0.77 | 0.343 | 0.15, 0.52 | <0.001 | 14.8 | 8.8, 23.7 | |
| S10 | 56 | −0.01 (−0.06 to 0.03) | −0.04, 0.01 | 0.42 | 0.475 | 0.24, 0.65 | <0.001 | 17.9 | 10.0, 29.8 | |
| S17 | 34 | 0.01 (−0.03 to 0.03) | −0.02, 0.04 | 0.35 | 0.304 | −0.03, 0.58 | 0.04 | 14.7 | 6.4, 30.1 | |
| S11 | 109 | 0.01 (−0.01 to 0.03) | 0.01, 0.02 | <0.001 | 0.485 | 0.33, 0.62 | <0.001 | 2.8 | 0.9, 7.8 | |
| S12 | 88 | 0.005 (−0.03 to 0.04) | −0.01, 0.02 | 0.38 | 0.297 | 0.10, 0.48 | 0.002 | 10.2 | 5.5, 18.3 | |
| S13 | 90 | 0.015 (−0.02 to 0.05) | 0.01, 0.03 | 0.009 | 0.554 | 0.39, 0.68 | <0.001 | 11.1 | 6.1, 19.3 | |
| S14 | 58 | 0.00 (−0.06 to 0.04) | −0.02, 0.02 | 1.00 | 0.621 | 0.43, 0.76 | <0.001 | 19.0 | 10.9, 30.9 | |
| S15 | 11 | 0.005 (−0.03 to 0.06) | −0.06, 0.07 | 0.89 | 0.619 | 0.07, 0.88 | 0.02 | 9.1 | 1.6, 37.7 | |
| S18 | 13 | −0.024 (−0.06 to 0.06) | −0.09, 0.03 | 0.33 | 0.430 | −0.13, 0.78 | 0.06 | 30.8 | 12.7, 57.6 | |
| Level of Observation | Observer | n | TP | TN | FP | FN | Sen. % | Spe. % | PPV % | NPV % | Acc. % |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Patient | Observer A | 109 | 2 | 31 | 76 | 0 | 100.0% | 29.0 | 2.6 | 100.0 | 30.3 |
| Observer B | 2 | 31 | 76 | 0 | 100.0% | 29.0 | 2.6 | 100.0 | 30.3 | ||
| Difference Δ | 0 | 0 | 0 | 0 | 0.0% | 0.0 | 0.0 | 0.00 | 0.0 | ||
| Vessel | Observer A | 436 | 0 | 306 | 128 | 2 | 0.0% | 70.5 | 0.0 | 99.4 | 70.2 |
| Observer B | 1 | 314 | 120 | 1 | 50.0% | 72.4 | 0.8 | 99.7 | 72.3 | ||
| Difference Δ | 1 | 8 | −8 | −1 | 50.0% | +1.8 | +0.8 | +0.3 | +2.1 | ||
| Segment | Observer A | 1456 | 0 | 1265 | 189 | 2 | 0.0% | 87.0 | 0.0 | 99.8 | 86.9 |
| Observer B | 0 | 1271 | 183 | 2 | 0.0% | 87.4 | 0.0 | 99.8 | 87.3 | ||
| Difference Δ | 0 | 6 | −6 | 0 | 0.0% | +0.4 | 0.0 | 0.0 | +0.4 |
| Segment Location | Observer | n | TP | TN | FP | FN | Sen. % | Spe. % | PPV % | NPV % | Acc. % |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Proximal | Observer A | 470 | 0 | 465 | 5 | 0 | / | 98.9% | 0.0% | 100.0% | 98.9% |
| Observer B | 0 | 466 | 4 | 0 | / | 99.1% | 0.0% | 100.0% | 99.1% | ||
| Difference Δ | 0 | −1 | 1 | 0 | / | −0.2% | 0.0% | 0.0% | −0.2% | ||
| Distal | Observer A | 986 | 0 | 800 | 184 | 2 | 0.0% | 81.3% | 0.0% | 99.8% | 81.1% |
| Observer B | 0 | 805 | 179 | 2 | 0.0% | 81.8% | 0.0% | 99.8% | 81.6% | ||
| Difference Δ | 0 | −5 | 5 | 0 | 0.0% | −0.5% | 0.0% | 0.0% | −0.5% |
| CT-FFR Values | Level of Observation | n | Image Quality | Calcium Burden | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| r CNR | 95% CI | p | r HU | 95% CI | p | r QIQ | 95% CI | p | r CAC | 95% CI | p | ||||
| Absolute | Patient | 109 | −0.059 | −0.241, 0.127 | 0.55 | −0.073 | −0.261, 0.120 | 0.45 | −0.064 | −0.208, 0.080 | 0.40 | 0.394 | 0.221, 0.542 | <0.001 | |
| Vessel | RCA | 109 | −0.032 | −0.223, 0.157 | 0.74 | −0.081 | −0.276, 0.121 | 0.41 | −0.127 | −0.283, 0.033 | 0.10 | 0.078 | −0.115, 0.264 | 0.42 | |
| LM | 109 | 0.173 | −0.038, 0.363 | 0.07 | 0.204 | −0.010, 0.396 | 0.03 | 0.004 | −0.178, 0.184 | 0.97 | 0.001 | −0.184, 0.192 | 1.00 | ||
| LAD | 109 | −0.122 | −0.311, 0.075 | 0.21 | −0.146 | −0.340, 0.059 | 0.13 | −0.094 | −0.246, 0.066 | 0.22 | 0.393 | 0.200, 0.553 | <0.001 | ||
| LCX | 109 | 0.090 | −0.102, 0.276 | 0.35 | 0.066 | −0.135, 0.260 | 0.50 | −0.026 | −0.175, 0.128 | 0.73 | 0.129 | −0.069, 0.311 | 0.18 | ||
| Categorized | Patient | 109 | 0.011 | −0.177, 0.199 | 0.91 | −0.040 | −0.226, 0.149 | 0.68 | 0.009 | −0.227, 0.243 | 0.94 | 0.133 | −0.057, 0.313 | 0.17 | |
| Vessel | RCA | 109 | 0.114 | −0.076, 0.296 | 0.24 | 0.218 | 0.031, 0.390 | 0.02 | −0.226 | −0.444, 0.016 | 0.05 | 0.013 | −0.176, 0.200 | 0.90 | |
| LAD | 109 | 0.118 | −0.071, 0.300 | 0.22 | 0.091 | −0.098, 0.275 | 0.35 | −0.019 | −0.249, 0.213 | 0.86 | 0.099 | −0.091, 0.282 | 0.31 | ||
| LCX | 109 | −0.020 | −0.207, 0.169 | 0.84 | -0.061 | −0.246, 0.129 | 0.53 | 0.139 | −0.131, 0.389 | 0.28 | 0.207 | 0.019, 0.380 | 0.03 | ||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gohmann, R.F.; Schug, A.; Krieghoff, C.; Seitz, P.; Majunke, N.; Buske, M.; Kaiser, F.; Schaudt, S.; Renatus, K.; Desch, S.; et al. Interrater Variability of ML-Based CT-FFR in Patients without Obstructive CAD before TAVR: Influence of Image Quality, Coronary Artery Calcifications, and Location of Measurement. J. Clin. Med. 2024, 13, 5247. https://doi.org/10.3390/jcm13175247
Gohmann RF, Schug A, Krieghoff C, Seitz P, Majunke N, Buske M, Kaiser F, Schaudt S, Renatus K, Desch S, et al. Interrater Variability of ML-Based CT-FFR in Patients without Obstructive CAD before TAVR: Influence of Image Quality, Coronary Artery Calcifications, and Location of Measurement. Journal of Clinical Medicine. 2024; 13(17):5247. https://doi.org/10.3390/jcm13175247
Chicago/Turabian StyleGohmann, Robin F., Adrian Schug, Christian Krieghoff, Patrick Seitz, Nicolas Majunke, Maria Buske, Fyn Kaiser, Sebastian Schaudt, Katharina Renatus, Steffen Desch, and et al. 2024. "Interrater Variability of ML-Based CT-FFR in Patients without Obstructive CAD before TAVR: Influence of Image Quality, Coronary Artery Calcifications, and Location of Measurement" Journal of Clinical Medicine 13, no. 17: 5247. https://doi.org/10.3390/jcm13175247






