Abstract
Background: Dysmenorrhea is a common condition that may have negative effects on social life, couples’ relationships and professional activities. The objectives of this study were to evaluate the prevalence, risk factors and characteristics of dysmenorrhea and its impact on patients’ quality of life using a specific self-questionnaire named “DysmenQoL questionnaire”. We also checked the validity and reliability of this questionnaire in our population. Methods: We conducted a cross-sectional study that included 504 participants of reproductive age between 18 and 45 years of age. The data were collected with an original form divided into three sections. The last section (DysmenQoL questionnaire) included 20 statements scored from 1 (“never”) to 5 (“every time”) that evaluates the effects of menstrual pain on health and feelings, daily activities, relationships and professional activity. We calculated the sum of the scores for each statement and we called it the “DysmenQoL score”. Results: The prevalence of dysmenorrhea was 83.7%. The presence of dysmenorrhea was statistically significant associated with the degree of menstrual bleeding (p = 0.017), the presence of infertility (p = 0.034) and dyspareunia (p = 0.002), but also with the presence of premenstrual syndrome and a family history of dysmenorrhea (p < 0.001). Among the participants with dysmenorrhea, 73.9% considered that this symptom affected their quality of life, and this was correlated with pain intensity and the DysmenQoL score (p < 0.001). A significant difference regarding the DysmenQoL score depending on the pain intensity, frequency and duration of dysmenorrhea and the methods used to reduce the pain was observed. Conclusions: Dysmenorrhea had a high prevalence among the participants included in the study, and its presence was associated with a series of risk factors. Most women considered that dysmenorrhea affected their quality of life. The DysmenQoL questionnaire proved to be a reliable and valid method for evaluating the impact of dysmenorrhea on quality of life.
1. Introduction
Dysmenorrhea was defined as the presence of painful menstruation and its prevalence was reported to vary between 16 and 91%, with severe pain occurring in 2% to 29% of cases [,]. A higher rate of dysmenorrhea was observed among adolescents between 12 and 19 years old [,]. Two types of dysmenorrhea have been described: primary and secondary dysmenorrhea. Most of the time, primary dysmenorrhea appears at 6 months after menarche, and it has no identifiable cause. Usually, the pain is more intense in the first two days of menstruation, lasts between 8 and 72 h, and can be associated with numerous other symptoms such as fatigue, dizziness or insomnia []. The occurrence mechanism involves the cyclooxygenase pathway and the production of prostaglandins that can cause the contraction of the uterine muscles with the reduction of blood flow and the stimulation of pain receptors by anaerobic metabolites []. Secondary dysmenorrhea usually occurs more than two years after menarche and it is associated with pelvic diseases such as endometriosis, uterine fibroids, ovarian cysts, uterine polyps or adenomyosis [].
Several risk factors for dysmenorrhea have been identified, including heavy menstrual flow, family history of dysmenorrhea [], the presence of premenstrual syndrome [] (affective, cognitive or somatic symptoms that occur before menstruation, such as increased appetite, constipation, nausea, weight gain, headache, breast tenderness, fatigue, restlessness, anxiety or mood changes) [], young age of menarche, nulliparity, low intake of omega 3 fatty acids [] and smoking or regular coffee consumption []. It has been observed that maintaining a normal body mass index and reduction of stress can be beneficial in preventing dysmenorrhea []. It was found that the onset and frequency of dysmenorrhea in adolescence are predictive factors for the presence of endometriosis in adulthood [].
It was observed that dysmenorrhea influenced women’s daily activities and negatively affected their quality of life []. Among female students, the presence of dysmenorrhea had negative effects on academic performance due to the appearance of difficulties in studying, the impossibility to concentrate in classes [] and absenteeism, but also sleep disturbances or problems in personal relationships [].
Most of the time, dysmenorrhea is not properly managed so menstrual pain persists and can have negative effects on women’s quality of life. Sometimes dysmenorrhea is not considered important; in addition, women can believe that it represents a normality. Women with dysmenorrhea have a low quality of life for several days each month and they have a poorer mood []. The most effective drugs prescribed to reduce pain are non-steroidal anti-inflammatory drugs (NSAIDs) []. Apart from pharmacological agents, complementary and alternative medicine is used to relieve menstrual pain []. Among the non-pharmacological methods, warming techniques such as hot packs, hot water or clothes have been identified as the most used to reduce menstrual pain []. It was found that practicing yoga for 30 min twice a week for 12 weeks can relieve menstrual pain [].
The purpose of this study was to evaluate the characteristics of dysmenorrhea such as prevalence, duration and intensity of pain, risk factors, and methods used to reduce pain. Another objective was to evaluate the impact of dysmenorrhea on the quality of life by using our own specific questionnaire (the DysmenQoL questionnaire) that estimated the negative effects of dysmenorrhea on health and feelings, daily activities, relationships with others and professional activity. We also checked the validity and reliability of this specific questionnaire in our population.
We evaluated dysmenorrhea and its impact on the quality of life in participants of reproductive age and we did not limit the study to adolescents. We did not find in the literature a score or a specific questionnaire to observe the relationship between this condition and quality of life.
2. Materials and Methods
We conducted a cross-sectional study between January and April 2024 in Bucharest, Romania. In this study were included women of reproductive age between 18 and 45 years of age who agreed to participate in the study and who answered all of the questions. Women who did not meet the age criterion or who did not complete the entire form were not included in this study. The exclusion criteria were represented by women without menstruation, menopausal women, patients with diagnosed gynecological pathology (such as endometriosis, uterine fibromatosis, ovarian cysts or pelvic inflammatory disease), patient with previous gynecological surgeries, patients with medical or mental disorders or patients in their menstrual period at the time of distribution of the questionnaire.
This study received the ethical approval of our institution Saint John Hospital Bucharest (protocol code 9083/12 April 2023). The patients’ informed consent for participation in the study was obtained through online methods.
We collected data from the participants with our original form consisting of 71 questions: 36 questions with two or more answer options, 6 multiple choice questions, 9 questions with open answers and 20 statements scored from 1 to 5. This form was divided into three sections. It was structured with the online tool Google Forms and it was distributed through social media to specific groups of women.
The first section (27 questions) aimed to collect data about general characteristics: professional activity, medical history, diet, physical activities, lifestyle and menstrual period. Quantitative limits were defined for the frequent consumption of coffee (250 mL at least 3 times a week) and chocolate (30 g at least 3 times a week). All participants in the study answered the first section. The rest of the questions were addressed exclusively to the participants who stated that they have dysmenorrhea.
The second section (24 questions) aimed to collect data about the characteristics of dysmenorrhea: frequency, duration, location, intensity of menstrual pain and symptoms associated with it and methods used to reduce pain and evaluate their effectiveness. The intensity of the menstrual pain was evaluated by giving a number from 1 to 10 (1—no pain; 10—unbearable pain). Menstrual cycles were considered regular if they occurred at an interval between 21 and 35 days, and irregular if they did not respect this interval [].
These two sections were useful in achieving the objective of evaluating the characteristics of dysmenorrhea (prevalence, risk factors, pain assessment).
The third section was useful for evaluating the impact of dysmenorrhea on the quality of life of the participants.
The last section was named “DysmenQoL questionnaire” (dysmenorrhea and quality of life) and it was represented by 20 statements about the negative effects of dysmenorrhea on quality of life (effects on health and feelings, relationships with family members or friends, couple relationships and professional activity). Only the study participants who stated that they have dysmenorrhea responded to this section. The twenty statements were developed after extensive consultation with clinicians, discussions with patients and literature review [,,]. The participants gave a score from 1 to 5 for each statement: 1—“Never”; 2—“Few cases”; 3—“Sometimes”; 4—“Most of the time”; 5—“Every time”. We calculated the sum of the scores for each statement and we called it “DysmenQoL score”, whose value could vary between 20 and 100.
In addition, we checked the validity and reliability of our own DysmenQoL questionnaire in our population.
The database was created and analyzed using SPSS Statistics, version 23. We used descriptive statistics methods to calculate frequencies, means and standard deviations. We performed the statistical analysis by using tests corresponding to the types of variables and the proposed objectives: Pearson correlation, independent samples t-test, one-way ANOVA and Chi-squared. The results of these tests were statistically significant if the p value was below 0.05. We tested the validity and reliability of DysmenQoL questionnaire. Reliability was evaluated by calculating Cronbach’s alpha, which had to be above 0.7 for the score to be reliable. Validity was tested for each individual statement using Pearson correlation.
3. Results
In this study were included 504 participants aged between 18 and 45 years. The mean age was 30.95 ± 6.37 years. There were no participants who did not meet the inclusion criteria. The general characteristics of the participants were summarized in Table 1. The prevalence of dysmenorrhea among the participants included in the study was 83.7% (422 participants). The age of menarche varied between 8 and 18 years, with an average of 12.64 ± 1.42 years. Using the independent samples t-test, we found out that the average age of menarche was statistically significantly higher in the case of participants who do not have dysmenorrhea (p = 0.035).

Table 1.
General characteristics of the participants.
Possible risk factors for the presence of dysmenorrhea were evaluated (Table 2). It was observed that dysmenorrhea was statistically significantly associated with the degree of menstrual bleeding (p = 0.017), the presence of dyspareunia (p = 0.002), infertility (p = 0.034), a family history of dysmenorrhea (p < 0.001), premenstrual syndrome (p < 0.001) and a history of gastritis (p = 0.040). The presence of dysmenorrhea did not have a statistically significant correlation with smoking status, the number of hours of sleep, the type of food eaten, coffee or chocolate consumption and the type of physical activity practiced.

Table 2.
Risk factors for the presence of dysmenorrhea.
A total of 312 participants (73.9%) considered that dysmenorrhea affected their quality of life. From the total of 422 participants with dysmenorrhea, 54.7% of the participants stated that dysmenorrhea appeared from the first menstruation and in 61.8% of the cases, it started from the first day of menstruation. A percentage of 64.9% of the participants stated that dysmenorrhea occurred with every menstruation, and 26.5% of the participants stated that the pain occurred during more than half of the periods. In 95% of the cases, the pain was located at the level of the pelvis and lower abdomen and in 40% of the cases, it radiated most frequently at the lumbar region. In 82.2% of the cases, menstrual pain lasted at least one day.
It was found that 65.4% of the participants considered that the intensity of the pain was greater if they had a stressful period, and 80.8% of the participants stated that the intensity of the pain did not decrease after the start of sexual life. Out of the 162 participants who gave birth at least once, 65 participants stated that after giving birth the characteristics of the menstrual pain changed.
The participants used both pharmacological and non-pharmacological methods to reduce pain in 69.9% of the cases. The most used pharmacological methods were NSAIDs (54.7%). Regarding the moment of starting the medication, 54.5% of the participants said that they start the medication when the pain becomes unbearable, 38.6% of the participants said that they start the medication when the pain appears and 13.3% of the participants said that they start the medication before pain occurs when they have scheduled events. Regarding the usefulness of the drugs, 65.9% of the participants stated that the drugs were useful most of the time in reducing menstrual pain, and 18.5% of the participants believed that if they take drugs before the onset of the pain, it will have a low intensity regardless of the number of days of medication. Drugs were considered useful in performing daily activities in normal conditions by 79.1% of the participants. The most used non-pharmacological methods were applying liquids or warm objects on the abdomen (53.6%), sleeping (42.4%), massaging painful areas (22.5%) and eating sweets (14.2%).
Menstrual pain was not the only disturbing symptom present during menstruation; it was also accompanied by agitation or irritability (54.0%), fatigue (63.5%), headaches (47.9%), diarrhea (38.2%), nausea (35.3%) and dizziness (32.0%).
The intensity of menstrual pain was considered by 313 participants (74.2%) the most important characteristic of pain for the negative effects on the quality of life. Most of the participants (72.3%) stated that work from home was useful during the menstrual period.
Each participant with dysmenorrhea evaluated the intensity of the pain giving a number from 1 to 10 (1—no pain; 10—unbearable pain). The mean pain intensity was 7.13 ± 1.78. In addition, they completed a section (the DysmenQoL questionnaire) with 20 affirmations with a score from 1 to 5 about the negative effects of dysmenorrhea on the quality of life. The DysmenQoL score was calculated by adding these twenty answers. The values of the DysmenQoL score varied between 22 and 100, and the mean score was 61.39 ± 16.61. Information about the relationship between these scores and pain intensity is presented in Table 3.

Table 3.
Pain intensity.
Using the independent samples t-test, the patients with dysmenorrhea were divided into two groups: those who considered that dysmenorrhea affected their quality of life and those who claimed the opposite. It was observed that there was a statistically significant difference between these two groups regarding the mean pain intensity (p < 0.001) and the mean DysmenQoL score (p < 0.001). A statistically significant correlation was found between the pain intensity score and the DysmenQoL score (p < 0.001). The relationship between them was illustrated in Figure 1. No statistically significant correlation was observed between the DysmenQoL score and the age of the study participants (p = 0.344).
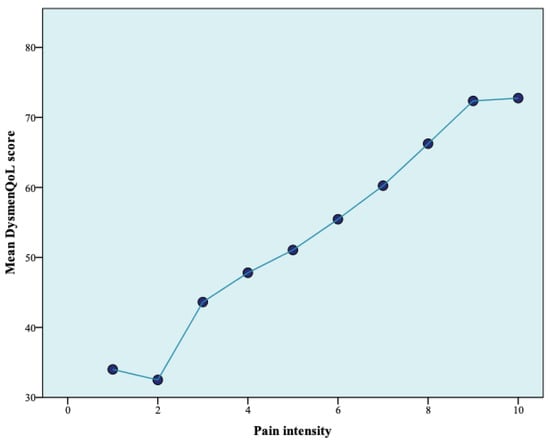
Figure 1.
The relationship between pain intensity and DysmenQoL score.
We used the one-way ANOVA test to analyze the DysmenQoL score. The results showed that there were statistically significant differences regarding the DysmenQoL score depending on the frequency (p < 0.001) and duration (p < 0.001) of dysmenorrhea, the intensity of pain (mild, moderate, severe) (p < 0.001), the methods used to reduce pain (p < 0.001) and the characteristic of pain that the participants considered the most important in affecting their quality of life (p < 0.001). No significant differences were observed regarding pain location (p = 0.116).
We used the independent samples t-test and found statistically significant differences regarding the DysmenQoL score and the presence of symptoms associated with menstrual pain: agitation or irritability (p = 0.009), nausea, vomiting, fatigue, diarrhea, headaches, dizziness, sweating, insomnia, loss of appetite for food (p < 0.001) and polyuria (p = 0.022).
The analysis of the scores for each statement is summarized in Table 4. It was observed that the average scores were increased for the following statements: “You feel more stressed” (3.75 ± 1.09), “You feel more agitated or nervous” (3.92 ± 0.99), “You feel more tired” (3.99 ± 0.99) and “You have less energy for daily activities” (4.04 ± 1.11). The lowest average was for the statement “Family members do not understand your discomfort and are not there for you” (2.01 ± 1.29).

Table 4.
DysmenQoL questionnaire.
We tested the reliability of this questionnaire (consisting of 20 statements) by calculating Cronbach’s alpha, which had a value of 0.928, which indicated an excellent internal consistency. We used the Pearson correlation to test the validity of this questionnaire and confirmed that each statement that contributed to the calculation of the DysmenQoL questionnaire was valid (p < 0.001). The DysmenQoL questionnaire proved to be a reliable and valid method for evaluating the impact of dysmenorrhea on the quality of life.
4. Discussion
We conducted a cross-sectional study that included 504 participants who fully answered our own questionnaire about dysmenorrhea. We evaluated the prevalence, risk factors and characteristics of menstrual pain. The questionnaire included a section dedicated to the impact of dysmenorrhea on the patients’ quality of life and based on the answers we calculated a score that we called the “DysmenQoL score”.
We found a high prevalence of dysmenorrhea (83.7%) among the participants included in the study. We identified a number of factors associated with the presence of dysmenorrhea, such as a familial history of dysmenorrhea and the presence of premenstrual syndrome, infertility or dyspareunia, as well as the degree of menstrual bleeding. Most of the participants believed that dysmenorrhea negatively affects their quality of life through the negative impact on health, affectivity, daily activities or relationships with others. The DysmenQoL score was useful in quantifying these negative effects. We hope that future studies will prove its effectiveness. Menstrual pain is a condition that requires more attention from those who provide health care because many women face this condition every month, for several days.
Dysmenorrhea is one of the most common gynecological complaints worldwide and can be found in over 90% of women of reproductive age [,]. In our study, the prevalence of dysmenorrhea was 83.7%.
A number of risk factors for the occurrence of dysmenorrhea were reported in the literature, such as a young age of menarche and a family history of dysmenorrhea and heavy menstrual flow []. Our data analysis indicated the same results. It has been reported that there is a positive relationship between the presence of dysmenorrhea and smoking, emotional problems, regular coffee consumption, physical activity [], frequency of menstrual cycles [], nulliparity [], underweight, excessive sugar intake [] and skipping breakfast []. In addition, we found that dyspareunia and infertility were associated with the presence of dysmenorrhea. Protective factors for the occurrence of dysmenorrhea were identified as older age, high fruit and vegetable consumption [], young age at the time of first childbirth and the use of combined oral contraceptives [].
In our study, 73.9% of the participants stated that dysmenorrhea affected their quality of life. In 54% of the cases, the participants stated that they presented agitation or irritability, and in 63.5% of these cases, they felt fatigue in the presence of dysmenorrhea. A total of 165 participants (39.1%) considered that the menstrual pain had a severe intensity. The mean pain intensity in this case was 8.69 ± 1.00, and the mean DysmenQoL score was 69.53 ± 15.90. Moderate pain was experienced by 230 participants (54.5%), with a pain intensity of 6.36 ± 1.22 and a DysmenQoL score of 57.34 ± 14.45. In a study conducted by Helwa et al., the average pain intensity among all participants was 6.79 ± 2.64 and most of the participants presented moderate or severe pain (80.34%) []. In another study by Ullah et al., it was observed that moderate meat or protein consumption and high levels of stress were associated with moderate or severe menstrual pain. The average intensity of dysmenorrhea among all study participants was 5.62 ± 2.28 and 65.8% of them had moderate or severe menstrual pain [].
Dysmenorrhea is a public health problem worldwide. It was estimated that in the United States, approximately 600 million hours were lost from work annually due to dysmenorrhea []. In a study by Armor et al. which included 4202 teenage girls and young women, it was observed that absenteeism and concentration problems were more frequent during the menstrual period; almost half of the participants stated that they had missed a class in the last three menstrual periods and severe menstrual pain was associated with a decrease in academic performance []. A study by Schoep et al. included 42,879 women and assessed the impact of menstrual symptoms on quality of life. It has been observed that during the menstrual period 1 in 3 women cancel their daily activities due to the symptoms associated with menstruation []. It was found that the presence of dysmenorrhea could affect social life and relationships with family members and friends []. Intense menstrual pains negatively affect socializing, practicing physical exercises and personal study []. Hashim et al. used SF-36 (36-item Short-Form Health Survey) scales to quantify the impact of dysmenorrhea on quality of life and observed that domains related to emotional and physical health, including health changes and pain, were significantly negatively influenced by the presence of dysmenorrhea []. The results of another study that used the SF-36 indicated lower scores for the domains of general health, bodily pain and social function in the presence of dysmenorrhea []. Mizuta et al. used the World Health Organization Quality of Life scale and showed that the lowest quality of life scores were associated with severe dysmenorrhea []. It has been observed that dysmenorrhea can negatively affect the quality of sleep []. However, the polysomnogram performed during the menstrual periods did not highlight important changes in the sleep patterns of women who had menstrual pain [].
The participants in our study stated that in 69.9% of cases, they use both pharmacological and non-pharmacological methods to reduce menstrual pain. NSAIDs were the most used drugs. The application of liquids or warm objects on the abdomen, sleeping or massaging painful areas represented frequently used non-pharmacological methods. Most of the participants considered that the administration of drugs was useful for reducing menstrual pain and for carrying out daily activities in normal conditions.
The persistence of menstrual pains and the negative effects that they have on patients can cause an exaggerated increase in drug consumption. Thus, it is very important to evaluate the intensity of dysmenorrhea and its impact on patients’ quality of life. It is necessary for women to learn to properly manage menstrual pain in safe conditions.
There are numerous dedicated questionnaires that evaluate the impact of gynecological symptoms or pathologies on quality of life, such as the ICIQ-VS for vaginal symptoms [,,,], P-QOL for genital prolapse [,,], SQOL-F for quality of sexual life [,,], FertiQoL for fertility problems [,], FACIT-CD for cervical dysplasia [,], PISQ-IR for the assessment of sexual function in patients with pelvic floor disorders [,,], UFS-QOL for uterine fibromatosis [,] and MENQOL for the impact of symptoms associated with menopause [,]. We did not find a specific questionnaire for evaluating the impact of dysmenorrhea on quality of life. Future studies are required to reproduce the validity of the DymenQoL questionnaire.
The DysmenQoL questionnaire proved to be a specific, reliable, valid and useful tool in evaluating the impact of dysmenorrhea on quality of life. Its validity was supported by its statistically significant correlation with a series of dysmenorrhea characteristics such as duration, frequency and intensity (evaluated both quantitatively with a score from 1 to 10 and qualitatively—mild, moderate, severe). We believe that future studies will be necessary to confirm its use in other populations. We believe that this tool will prove useful in the evaluation of the therapeutic management of dysmenorrhea.
The limitations of our study were represented by the questions with predefined answers included in our questionnaire as well as by the accuracy of the answers of the participants in the study. Other limitations of the study were the possibility of misinterpretation of questions and the lack of interest and involvement of the participants during the response to the form, as well as the large number of questions.
5. Conclusions
The presence of dysmenorrhea was directly associated with the degree of menstrual bleeding, the presence of dyspareunia and infertility and the presence of premenstrual syndrome and a family history of dysmenorrhea. Most women considered that dysmenorrhea affected their quality of life, and this was correlated with the pain intensity and the DysmenQoL score. A significant difference regarding the DysmenQoL score depending on the pain intensity, frequency and duration of dysmenorrhea and the methods used to reduce the pain was observed. The DysmenQoL questionnaire proved to be a reliable and valid method for evaluating the impact of dysmenorrhea on the quality of life. Future studies are required to reproduce its validity.
Author Contributions
Conceptualization, M.A. and S.F.; methodology, B.H.H.; software, M.-O.P.; validation, M.P. and S.F.; formal analysis, B.H.H.; investigation, M.-O.P.; resources, M.P.; data curation, R.-M.S.; writing—original draft preparation, M.A.; writing—review and editing, R.-M.S.; visualization, L.P.; supervision, L.P. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
This study was conducted according to the guidelines of the Declaration of Helsinki and approved by the Ethics Committee of “Sf. Ioan” Emergency Hospital, Bucharest, Romania (protocol code 9083 and date 12 April 2023).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The data used in this study are available from the corresponding author, and the authors can share the information if there is a reasonable request.
Acknowledgments
Publication of this paper was supported by the University of Medicine Pharmacy Carol Davila, through the institutional program Publish not Perish.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Ju, H.; Jones, M.; Mishra, G. The Prevalence and Risk Factors of Dysmenorrhea. Epidemiologic Rev. 2014, 36, 104–113. [Google Scholar] [CrossRef] [PubMed]
- Ghandour, R.; Hammoudeh, W.; Stigum, H.; Giacaman, R.; Fjeld, H.; Holmboe-Ottesen, G. The hidden burden of dysmenorrhea among adolescent girls in Palestine refugee camps: A focus on well-being and academic performance. BMC Public Health 2024, 24, 726. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Baidhya, N.; Paneru, D.P. Prevalence of Dysmenorrhea and its Associated Factors among Adolescent Girls Studying in Technical Schools of Dang, Nepal. J. Health Allied Sci. 2020, 10, 24–29. [Google Scholar] [CrossRef]
- Acheampong, K.; Baffour-Awuah, D.; Ganu, D.; Appiah, S.; Pan, X.; Kaminga, A.; Liu, A. Prevalence and Predictors of Dysmenorrhea, Its Effect, and Coping Mechanisms among Adolescents in Shai Osudoku District, Ghana. Obstet. Gynecol. Int. 2019, 2019, 5834159. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Guimarães, I.; Póvoa, A.M. Primary Dysmenorrhea: Assessment and Treatment. Rev Bras Ginecol Obstet. 2020, 42, 501–507. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Ferries-Rowe, E.; Corey, E.; Archer, J.S. Primary Dysmenorrhea: Diagnosis and Therapy. Obstet. Gynecol. 2020, 136, 1047–1058. [Google Scholar] [CrossRef] [PubMed]
- Dong, Y.; Li, M.-J.; Hong, Y.-Z.; Li, W.-J. Insight into Dysmenorrhea Research from 1992 to 2022: A Bibliometric Analysis. J. Pain Res. 2023, 16, 3591–3611. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Karout, S.; Soubra, L.; Rahme, D.; Karout, L.; Khojah, H.M.J.; Itani, R. Prevalence, risk factors, and management practices of primary dysmenorrhea among young females. BMC Women’s Health 2021, 21, 392. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Sima, R.-M.; Sulea, M.; Radosa, J.C.; Findeklee, S.; Hamoud, B.H.; Popescu, M.; Gorecki, G.P.; Bobircă, A.; Bobirca, F.; Cirstoveanu, C.; et al. The Prevalence, Management and Impact of Dysmenorrhea on Medical Students’ Lives—A Multicenter Study. Healthcare 2022, 10, 157. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Oboza, P.; Ogarek, N.; Wójtowicz, M.; Rhaiem, T.B.; Olszanecka-Glinianowicz, M.; Kocełak, P. Relationships between Premenstrual Syndrome (PMS) and Diet Composition, Dietary Patterns and Eating Behaviors. Nutrients 2024, 16, 1911. [Google Scholar] [CrossRef]
- Jiang, W.; Hua, X.-G.; Hu, C.-Y.; Li, F.-L.; Huang, K.; Zhang, X.-J.; Jiang, W.; Hua, X.-G.; Hu, C.-Y.; Li, F.-L.; et al. The prevalence and risk factors of menstrual pain of married women in Anhui Province, China. Eur. J. Obstet. Gynecol. Reprod. Biol. 2018, 229, 190–194. [Google Scholar] [CrossRef] [PubMed]
- Dai, Y.; Luo, H.; Zhu, L.; Yang, W.; Xiang, H.; Shi, Q.; Jin, P. Dysmenorrhea pattern in adolescences informing adult endometriosis. BMC Public Health 2024, 24, 373. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Iacovides, S.; Avidon, I.; Bentley, A.; Baker, F.C. Reduced quality of life when experiencing menstrual pain in women with primary dysmenorrhea. Acta Obstet. Gynecol. Scand. 2014, 93, 213–217. [Google Scholar] [CrossRef] [PubMed]
- Mesele, T.T.; Ayalew, H.G.; Syoum, A.T.; Antehneh, T.A. Impact of Dysmenorrhea on Academic Performance Among Haramaya University Undergraduate Regular Students, Eastern Ethiopia. Front. Reprod. Health 2022, 4, 939035. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Belayneh, W.; Kassaye, Z.; Arusi, T.; Abera, N.; Hantalo, A.; Melkamu, B.; Gutulo, M. Prevalence of dysmenorrhea and associated factors and its effect on daily academic activities among female undergraduate students of Hawassa University College of Medicine and Health Sciences, Hawassa, Ethiopia. Front. Reprod. Health 2023, 5, 1244540. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Martire, F.G.; Piccione, E.; Exacoustos, C.; Zupi, E. Endometriosis and Adolescence: The Impact of Dysmenorrhea. J. Clin. Med. 2023, 12, 5624. [Google Scholar] [CrossRef]
- Iacovides, S.; Avidon, I.; Baker, F.C. What we know about primary dysmenorrhea today: A critical review. Hum. Reprod. Update 2015, 21, 762–778. [Google Scholar] [CrossRef] [PubMed]
- Lee, H.W.; Ang, L.; Lee, M.S.; Alimoradi, Z.; Kim, E. Fennel for Reducing Pain in Primary Dysmenorrhea: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Nutrients 2020, 12, 3438. [Google Scholar] [CrossRef]
- Matsuura, Y.; Tran, N.H.; Nguyen, B.T.; Phan, Q.N.; Nguyen, K.T.; Yasui, T. Menstruation-Related Symptoms and Associated Factors among Female University Students in Vietnam. Youth 2024, 4, 344–356. [Google Scholar] [CrossRef]
- Yonglitthipagon, P.; Muansiangsai, S.; Wongkhumngern, W.; Donpunha, W.; Chanavirut, R.; Siritaratiwat, W.; Mato, L.; Eungpinichpong, W.; Janyacharoen, T. Effect of yoga on the menstrual pain, physical fitness, and quality of life of young women with primary dysmenorrhea. J. Bodyw. Mov. Ther. 2017, 21, 840–846. [Google Scholar] [CrossRef] [PubMed]
- Attia, G.M.; Alharbi, O.A.; Aljohani, R.M. The Impact of Irregular Menstruation on Health: A Review of the Literature. Cureus 2023, 15, e49146. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Vlachou, E.; Owens, D.A.; Lavdaniti, M.; Kalemikerakis, J.; Evagelou, E.; Margari, N.; Fasoi, G.; Evangelidou, E.; Govina, O.; Tsartsalis, A.N. Prevalence, Wellbeing, and Symptoms of Dysmenorrhea among University Nursing Students in Greece. Diseases 2019, 7, 5. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Joshi, T.; Kural, M.; Agrawal, D.; Noor, N.N.; Patil, A.B. Primary dysmenorrhea and its effect on quality of life in young girls. Int. J. Med. Sci. Public Health 2015, 4, 381–385. [Google Scholar] [CrossRef]
- Abu Helwa, H.A.; Mitaeb, A.A.; Al-Hamshri, S.; Sweileh, W.M. Prevalence of dysmenorrhea and predictors of its pain intensity among Palestinian female university students. BMC Women’s Health 2018, 18, 18. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Molla, A.; Duko, B.; Girma, B.; Madoro, D.; Nigussie, J.; Belayneh, Z.; Mengistu, N.; Mekuriaw, B. Prevalence of dysmenorrhea and associated factors among students in Ethiopia: A systematic review and meta-analysis. Women’s Health 2022, 18, 17455057221079443. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Gebeyehu, M.B.; Mekuria, A.B.; Tefera, Y.G.; Andarge, D.A.; Debay, Y.B.; Bejiga, G.S.; Gebresillassie, B.M. Prevalence, Impact, and Management Practice of Dysmenorrhea among University of Gondar Students, Northwestern Ethiopia: A Cross-Sectional Study. Int. J. Reprod. Med. 2017, 2017, 3208276. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- De Sanctis, V.; Soliman, A.; Bernasconi, S.; Bianchin, L.; Bona, G.; Bozzola, M.; Buzi, F.; De Sanctis, C.; Tonini, G.; Rigon, F.; et al. Primary Dysmenorrhea in Adolescents: Prevalence, Impact and Recent Knowledge. Pediatr. Endocrinol. Rev. 2015, 13, 512–520. [Google Scholar] [PubMed]
- Duman, N.B.; Yıldırım, F.; Vural, G. Risk factors for primary dysmenorrhea and the effect of complementary and alternative treat-ment methods: Sample from Corum, Turkey. Int. J. Health Sci. 2022, 16, 35–43. [Google Scholar] [PubMed] [PubMed Central]
- Aktaş, D. Prevalence and Factors Affecting Dysmenorrhea in Female University Students: Effect on General Comfort Level. Pain Manag. Nurs. 2015, 16, 534–543. [Google Scholar] [CrossRef] [PubMed]
- Nyirenda, T.; Nyagumbo, E.; Murewanhema, G.; Mukonowenzou, N.; Kagodora, S.B.; Mapfumo, C.; Bhebhe, M.; Mufunda, J. Prevalence of dysmenorrhea and associated risk factors among university students in Zimbabwe. Women’s Health 2023, 19, 17455057231189549. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Ozerdogan, N.; Sayiner, D.; Ayranci, U.; Unsal, A.; Giray, S. Prevalence and predictors of dysmenorrhea among students at a university in Turkey. Int. J. Gynecol. Obstet. 2009, 107, 39–43. [Google Scholar] [CrossRef] [PubMed]
- Hu, Z.; Tang, L.; Chen, L.; Kaminga, A.C.; Xu, H. Prevalence and Risk Factors Associated with Primary Dysmenorrhea among Chinese Female University Students: A Cross-sectional Study. J. Pediatr. Adolesc. Gynecol. 2020, 33, 15–22. [Google Scholar] [CrossRef] [PubMed]
- Tavallaee, M.; Joffres, M.R.; Corber, S.J.; Bayanzadeh, M.; Rad, M.M. The prevalence of menstrual pain and associated risk factors among Iranian women. J. Obstet. Gynaecol. Res. 2011, 37, 442–451. [Google Scholar] [CrossRef] [PubMed]
- Latthe, P.; Mignini, L.; Gray, R.; Hills, R.; Khan, K. Factors predisposing women to chronic pelvic pain: Systematic review. BMJ 2006, 332, 749–755. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Ullah, A.; Fayyaz, K.; Javed, U.; Usman, M.; Malik, R.; Arif, N.; Kaleem, A. Prevalence of Dysmenorrhea and Determinants of Pain Intensity Among University-Age Women. Pain Med. 2021, 22, 2851–2862. [Google Scholar] [CrossRef] [PubMed]
- Hailemeskel, S.; Demissie, A.; Assefa, N. Primary dysmenorrhea magnitude, associated risk factors, and its effect on academic performance: Evidence from female university students in Ethiopia. Int. J. Women’s Health 2016, 8, 489–496. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Armour, M.; Ferfolja, T.; Curry, C.; Hyman, M.S.; Parry, K.; Chalmers, K.J.; Smith, C.A.; MacMillan, F.; Holmes, K. The Prevalence and Educational Impact of Pelvic and Menstrual Pain in Australia: A National Online Survey of 4202 Young Women Aged 13–25 Years. J. Pediatr. Adolesc. Gynecol. 2020, 33, 511–518. [Google Scholar] [CrossRef] [PubMed]
- Schoep, M.E.; Nieboer, T.E.; van der Zanden, M.; Braat, D.D.; Nap, A.W. The impact of menstrual symptoms on everyday life: A survey among 42,879 women. Am. J. Obstet. Gynecol. 2019, 220, 569.e1–569.e7. [Google Scholar] [CrossRef]
- Mohamed, H.E.; Mansour, S.E. The Effect of Dysmenorrhea on Quality of Life of Technical Secondary Schools Girls. Med. J. Cairo Univ. 2013, 81, 83–90. [Google Scholar]
- Hashim, R.T.; Alkhalifah, S.S.; Alsalman, A.A.; Alfaris, D.M.; Alhussaini, M.A.; Qasim, R.S.; Shaik, S.A. Prevalence of primary dysmenorrhea and its effect on the quality of life amongst female medical students at King Saud University, Riyadh, Saudi Arabia. A cross-sectional study. Saudi Med. J. 2020, 41, 283–289. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Wong, C.L. Health-related quality of life among Chinese adolescent girls with Dysmenorrhoea. Reprod. Health 2018, 15, 80. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Mizuta, R.; Maeda, N.; Tashiro, T.; Suzuki, Y.; Oda, S.; Komiya, M.; Urabe, Y. Quality of life by dysmenorrhea severity in young and adult Japanese females: A web-based cross-sectional study. PLoS ONE 2023, 18, e0283130. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Sahin, S.; Ozdemir, K.; Unsal, A.; Arslan, R. Review of Frequency of Dysmenorrhea and Some Associated Factors and Evaluation of the Relationship between Dysmenorrhea and Sleep Quality in University Students. Gynecol. Obstet. Investig. 2014, 78, 179–185. [Google Scholar] [CrossRef] [PubMed]
- Araujo, P.; Hachul, H.; Santos-Silva, R.; Bittencourt, L.R.; Tufik, S.; Andersen, M.L. Sleep pattern in women with menstrual pain. Sleep Med. 2011, 12, 1028–1030. [Google Scholar] [CrossRef] [PubMed]
- Price, N.; Jackson, S.R.; Avery, K.; Brookes, S.T.; Abrams, P. Development and psychometric evaluation of the ICIQ Vaginal Symptoms Questionnaire: The ICIQ-VS. BJOG 2006, 113, 700–712. [Google Scholar] [CrossRef] [PubMed]
- Arenholt, L.T.S.; Glavind-Kristensen, M.; Bøggild, H.; Glavind, K. Translation and validation of the International Consultation on Incontinence Questionnaire Vaginal Symptoms (ICIQ-VS): The Danish version. Int. Urogynecol. J. 2019, 30, 17–22. [Google Scholar] [CrossRef] [PubMed]
- Köleli, I.; Astepe, B.S. Validation of the Turkish version of the International Consultation on Incontinence Questionnaire-vaginal symptoms (ICIQ-VS). Int. Urogynecol. J. 2019, 30, 1203–1209. [Google Scholar] [CrossRef] [PubMed]
- Ekanayake, C.D.; Pathmeswaran, A.; Herath, R.P.; Perera, H.S.S.; Patabendige, M.; Wijesinghe, P.S. Validation of the International Consultation on Incontinence Questionnaire–Vaginal Symptoms (ICIQ-VS) in two south- Asian languages. Int. Urogynecol. J. 2017, 28, 1849–1855. [Google Scholar] [CrossRef] [PubMed]
- Digesu, G.A.; Khullar, V.; Cardozo, L.; Robinson, D.; Salvatore, S. P-QOL: A validated questionnaire to assess the symptoms and quality of life of women with urogenital prolapse. Int. Urogynecol. J. Pelvic Floor Dysfunct. 2005, 16, 176–181; discussion 181. [Google Scholar] [CrossRef] [PubMed]
- Sánchez-Sánchez, B.; Yuste-Sánchez, M.J.; Arranz-Martín, B.; Navarro-Brazález, B.; Romay-Barrero, H.; Torres-Lacomba, M. Quality of Life in POP: Validity, Reliability and Responsiveness of the Prolapse Quality of Life Questionnaire (P-QoL) in Spanish Women. Int. J. Environ. Res. Public Health 2020, 17, 1690. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Belayneh, T.; Gebeyehu, A.; Adefris, M.; Rortveit, G.; Genet, T. Translation, transcultural adaptation, reliability and validation of the pelvic organ prolapse quality of life (P-QoL) in Amharic. Health Qual. Life Outcomes 2019, 17, 12. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Maasoumi, R.; Lamyian, M.; Montazeri, A.; Azin, S.A.; Aguilar-Vafaie, M.E.; Hajizadeh, E. The sexual quality of life-female (SQOL-F) questionnaire: Translation and psychometric properties of the Iranian version. Reprod. Health 2013, 10, 25. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Sim-Sim, M.; Aaberg, V.; Gómez-Cantarino, S.; Dias, H.; Caldeira, E.; Soto-Fernandez, I.; Gradellini, C. Sexual Quality of Life-Female (SQoL-F): Cultural Adaptation and Validation of European Portuguese Version. Healthcare 2022, 10, 255. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Symonds, T.; Boolell, M.; Quirk, F. Development of a Questionnaire on Sexual Quality of Life in Women. J. Sex Marital. Ther. 2005, 31, 385–397. [Google Scholar] [CrossRef]
- Boivin, J.; Takefman, J.; Braverman, A. The fertility quality of life (FertiQoL) tool: Development and general psychometric properties. Hum. Reprod. 2011, 26, 2084–2091. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Woods, B.M.; Bray, L.A.; Campbell, S.; Holland, A.; Mrug, S.; Ladores, S. A review of the psychometric properties and implications for the use of the fertility quality of life tool. Health Qual. Life Outcomes 2023, 21, 45. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Fregnani, C.M.S.; Fregnani, J.H.T.G.; Paiva, C.E.; Barroso, E.M.; Camargos, M.G.; Tsunoda, A.T.; Longatto-Filho, A.; Paiva, B.S.R. Translation and cultural adaptation of the Functional Assessment of Chronic Illness Therapy—Cervical Dysplasia (FACIT-CD) to evaluate quality of life in women with cervical intraepithelial neoplasia. Einstein 2017, 15, 155–161, Erratum in: Einstein 2017, 15, 389. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Fregnani, C.M.S.; Fregnani, J.H.T.G.; Longatto-Filho, A. Methodological study to evaluate the psychometric properties of FACIT-CD in a sample of Brazilian women with cervical intraepithelial neoplasia. BMC Cancer 2017, 17, 686. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Rockwood, T.H.; Constantine, M.L.; Adegoke, O.; Rogers, R.G.; McDermott, E.; Davila, G.W.; Domoney, C.; Jha, S.; Kammerer-Doak, D.; Lukacz, E.S.; et al. The PISQ-IR: Considerations in scale scoring and development. Int. Urogynecol. J. 2013, 24, 1105–1122. [Google Scholar] [CrossRef] [PubMed]
- Constantine, M.L.; Pauls, R.N.; Rogers, R.R.; Rockwood, T.H. Validation of a single summary score for the Prolapse/Incontinence Sexual Questionnaire–IUGA revised (PISQ-IR). Int. Urogynecol. J. 2017, 28, 1901–1907. [Google Scholar] [CrossRef] [PubMed]
- Rusavy, Z.; Kovarova, V.; Tvarozek, S.; Smazinka, M.; Havir, M.; Kalis, V. A Comprehensive Evaluation of Sexual Life in Women After Laparoscopic Sacrocolpopexy using PISQ-IR. Int. Urogynecol. J. 2024, 35, 873–880. [Google Scholar] [CrossRef] [PubMed]
- Keizer, A.L.; van Kesteren, P.J.M.; Terwee, C.; de Lange, M.E.; Hehenkamp, W.J.K.; Kok, H.S. Uterine Fibroid Symptom and Quality of Life questionnaire (UFS-QOL NL) in the Dutch population: A validation study. BMJ Open 2021, 11, e052664. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Coyne, K.S.; Soliman, A.M.; Margolis, M.K.; Thompson, C.L.; Chwalisz, K. Validation of the 4 week recall version of the Uterine Fibroid Symptom and Health-related Quality of Life (UFS-QOL) Questionnaire. Curr. Med. Res. Opin. 2017, 33, 193–200. [Google Scholar] [CrossRef] [PubMed]
- Radtke, J.V.; Terhorst, L.; Cohen, S.M. The Menopause-Specific Quality of Life Questionnaire: Psychometric evaluation among breast cancer survivors. Menopause 2011, 18, 289–295. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Nie, G.; Yang, H.; Liu, J.; Zhao, C.; Wang, X. Psychometric properties of the Chinese version of the Menopause-Specific Quality-of-Life questionnaire. Menopause 2017, 24, 546–554. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).