Prospective Study of Preoperative Negative Affect and Postoperative Pain in Patients Undergoing Thoracic Surgery: The Moderating Role of Sex
Abstract
1. Introduction
2. Materials and Methods
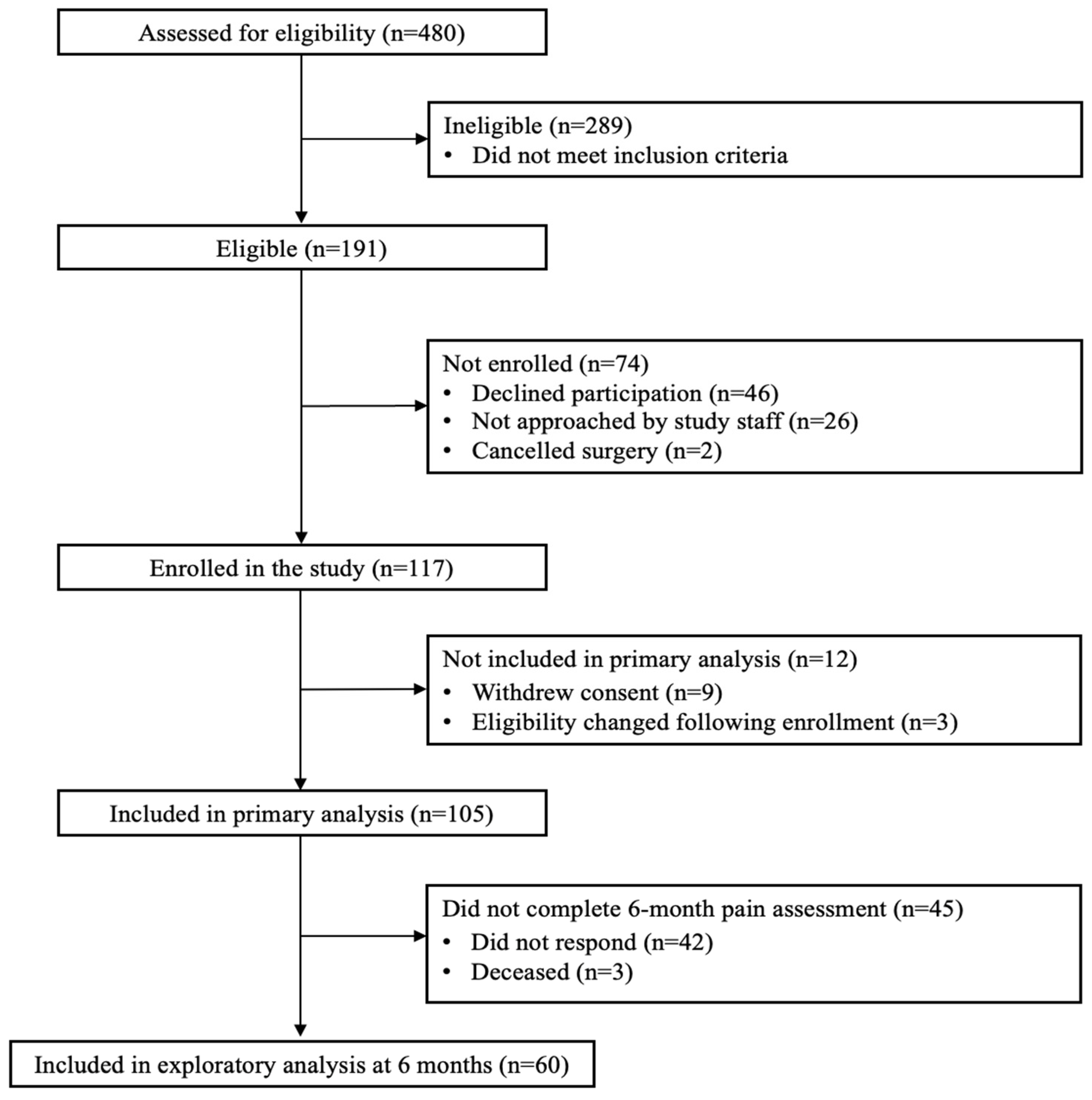
2.1. Participants and Procedure
2.2. Measures
2.2.1. Preoperative Assessments
2.2.2. Acute Postoperative Assessments
2.2.3. Chronic Postsurgical Pain
2.3. Data Analysis
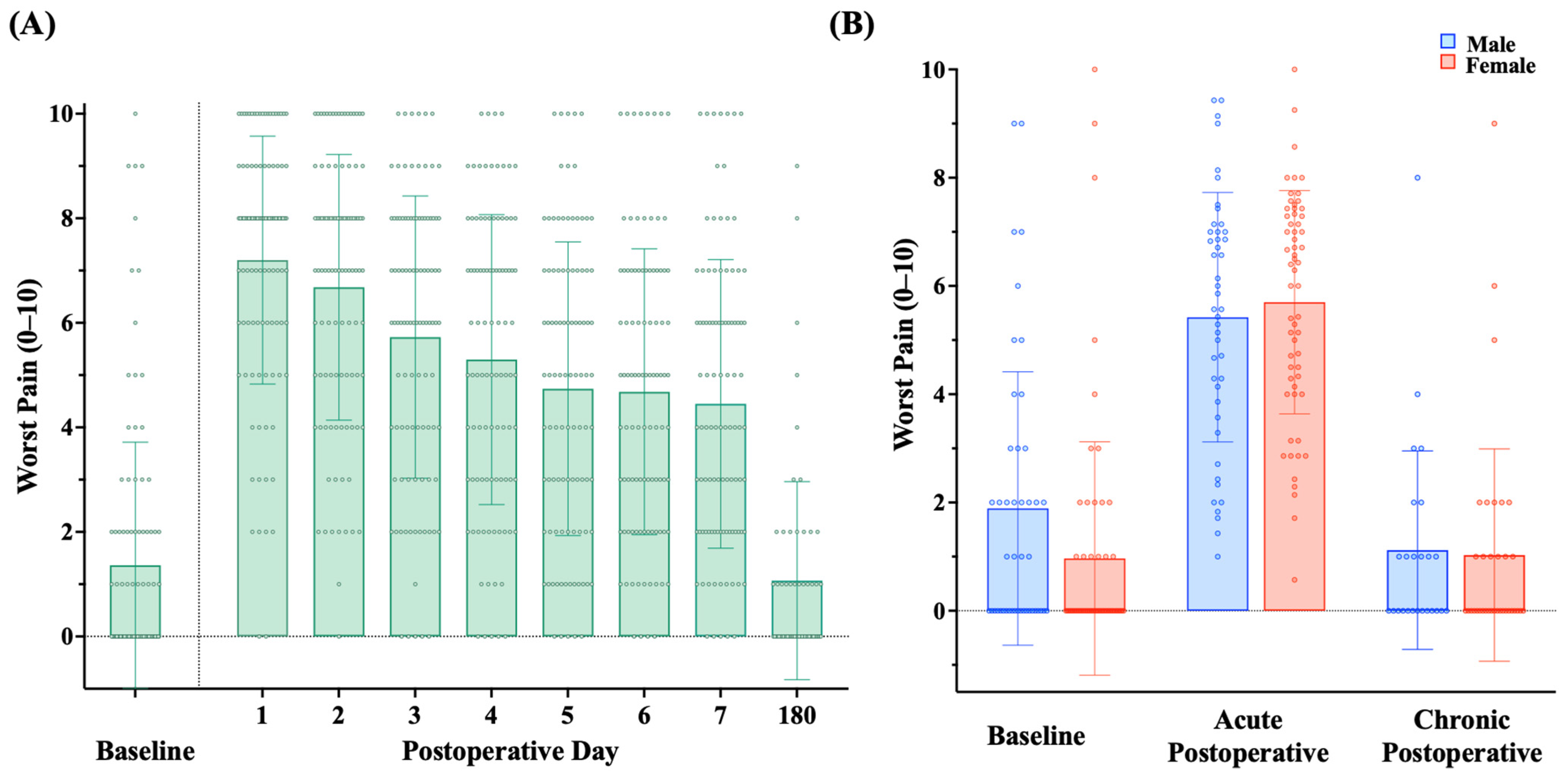
3. Results
3.1. Preoperative Patient Characteristics
3.2. Surgical Characteristics
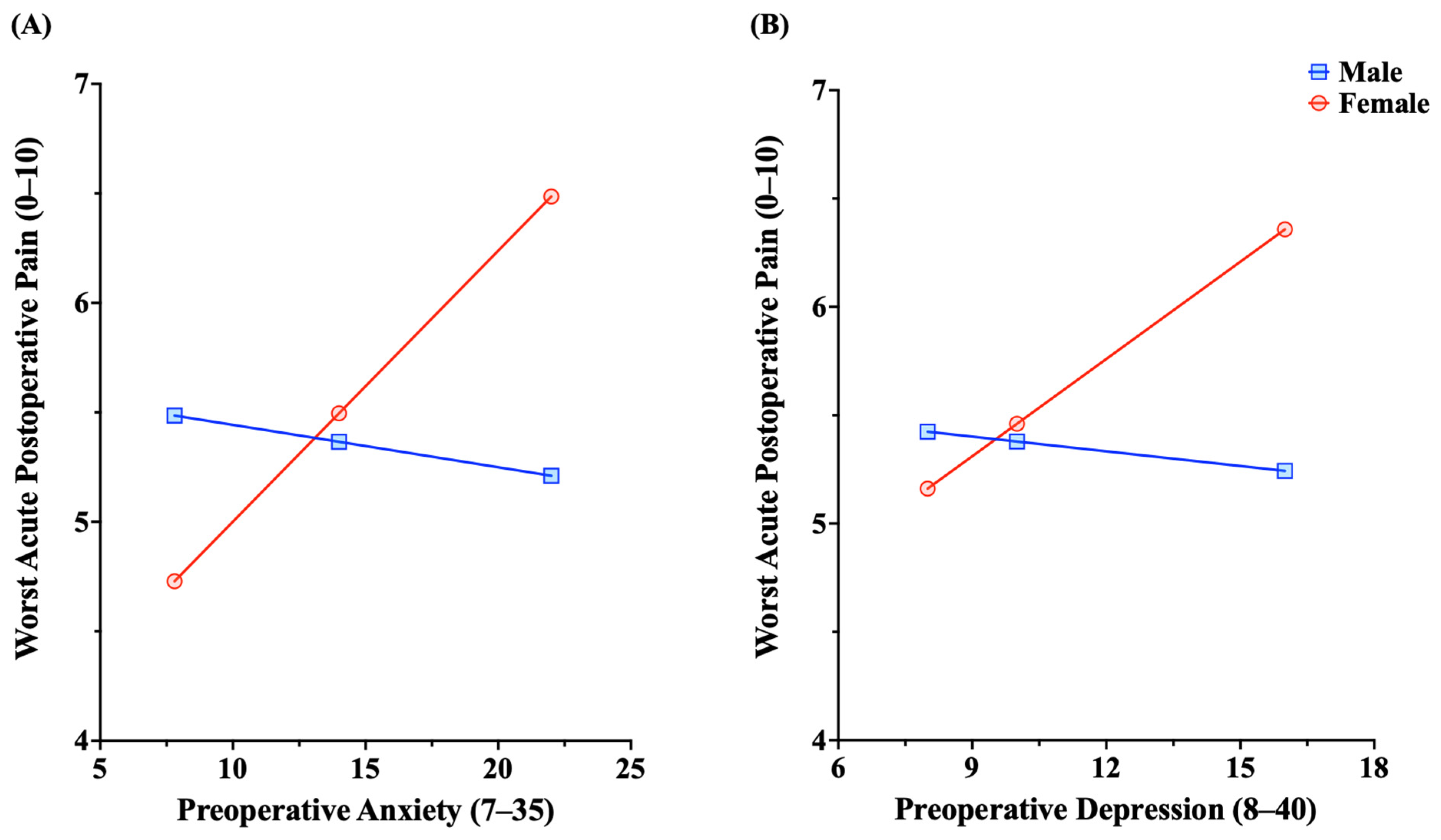
3.3. Association of Preoperative Negative Affect with Acute Postoperative Pain: The Role of Sex
3.4. Exploratory Analysis: Preoperative Negative Affect, Chronic Postsurgical Pain, and Sex
4. Discussion
5. Conclusions
6. Clinical Implications
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Byrd, C.T.; Williams, K.M.; Backhus, L.M. A Brief Overview of Thoracic Surgery in the United States. J. Thorac. Dis. 2022, 14, 218–226. [Google Scholar] [CrossRef] [PubMed]
- Servais, E.L.; Blasberg, J.D.; Brown, L.M.; Towe, C.W.; Seder, C.W.; Onaitis, M.W.; Block, M.I.; David, E.A. The Society of Thoracic Surgeons General Thoracic Surgery Database: 2022 Update on Outcomes and Research. Ann. Thorac. Surg. 2023, 115, 43–49. [Google Scholar] [CrossRef] [PubMed]
- Sun, K.; Liu, D.; Chen, J.; Yu, S.; Bai, Y.; Chen, C.; Yao, Y.; Yu, L.; Yan, M. Moderate-Severe Postoperative Pain in Patients Undergoing Video-Assisted Thoracoscopic Surgery: A Retrospective Study. Sci. Rep. 2020, 10, 795. [Google Scholar] [CrossRef] [PubMed]
- Niraj, G.; Kelkar, A.; Kaushik, V.; Tang, Y.; Fleet, D.; Tait, F.; Mcmillan, T.; Rathinam, S. Audit of Postoperative Pain Management after Open Thoracotomy and the Incidence of Chronic Postthoracotomy Pain in More than 500 Patients at a Tertiary Center. J. Clin. Anesth. 2017, 36, 174–177. [Google Scholar] [CrossRef] [PubMed]
- Bayman, E.O.; Oleson, J.J.; Rabbitts, J.A. AAAPT: Assessment of the Acute Pain Trajectory. Pain Med. 2021, 22, 533–547. [Google Scholar] [CrossRef]
- Gatchel, R.J.; Peng, Y.B.; Peters, M.L.; Fuchs, P.N.; Turk, D.C. The Biopsychosocial Approach to Chronic Pain: Scientific Advances and Future Directions. Psychol. Bull. 2007, 133, 581–624. [Google Scholar] [CrossRef]
- Anagnostopoulou, M.; Stroumpoulis, K.; Baltayiannis, N.; Voyagis, G.; Haniotis, D.; Iacovidou, N.; Papadimitriou, L.; Xanthos, T. Quality of Life and Pre-Operative Anxiety Level in Patients Scheduled to Undergo Thoracic Surgery. J. BUON 2011, 16, 522–527. [Google Scholar]
- Takamiya, S.; Honma, M.; Masaoka, Y.; Okada, M.; Ohashi, S.; Tanaka, Y.; Suzuki, K.; Uematsu, S.; Kitami, A.; Izumizaki, M. Preoperative State Anxiety Predicts Postoperative Health-Related Quality of Life: A Prospective Observational Study on Patients Undergoing Lung Cancer Surgery. Front. Psychol. 2023, 14, 1161333. [Google Scholar] [CrossRef]
- Takenaka, S.; Hirose, M. Preoperative Anxiety and Intraoperative Nociception in Patients Undergoing Thoracic Surgery. J. Surg. Res. 2020, 249, 13–17. [Google Scholar] [CrossRef]
- Kitagawa, R.; Yasui-Furukori, N.; Tsushima, T.; Kaneko, S.; Fukuda, I. Depression Increases the Length of Hospitalization for Patients Undergoing Thoracic Surgery: A Preliminary Study. Psychosomatics 2011, 52, 428–432. [Google Scholar] [CrossRef]
- Vasilopoulos, T.; Wardhan, R.; Rashidi, P.; Fillingim, R.B.; Wallace, M.R.; Crispen, P.L.; Parvataneni, H.K.; Prieto, H.A.; Machuca, T.N.; Hughes, S.J.; et al. Patient and Procedural Determinants of Postoperative Pain Trajectories. Anesthesiology 2021, 134, 421–434. [Google Scholar] [CrossRef] [PubMed]
- Yang, Y.; Sun, H.; Luo, X.; Li, W.; Yang, F.; Xu, W.; Ding, K.; Zhou, J.; Liu, W.; Garg, S.; et al. Network Connectivity between Fear of Cancer Recurrence, Anxiety, and Depression in Breast Cancer Patients. J. Affect. Disord. 2022, 309, 358–367. [Google Scholar] [CrossRef]
- Schreiber, K.L.; Zinboonyahgoon, N.; Xu, X.; Spivey, T.; King, T.; Dominici, L.; Partridge, A.; Golshan, M.; Strichartz, G.; Edwards, R.R. Preoperative Psychosocial and Psychophysical Phenotypes as Predictors of Acute Pain Outcomes after Breast Surgery. J. Pain 2019, 20, 540–556. [Google Scholar] [CrossRef] [PubMed]
- Nandi, M.; Schreiber, K.L.; Martel, M.O.; Cornelius, M.; Campbell, C.M.; Haythornthwaite, J.A.; Smith, M.T.; Wright, J.; Aglio, L.S.; Strichartz, G.; et al. Sex Differences in Negative Affect and Postoperative Pain in Patients Undergoing Total Knee Arthroplasty. Biol. Sex. Differ. 2019, 10, 23. [Google Scholar] [CrossRef] [PubMed]
- Montes, A.; Roca, G.; Sabate, S.; Lao, J.I.; Navarro, A.; Cantillo, J.; Canet, J. Genetic and Clinical Factors Associated with Chronic Postsurgical Pain after Hernia Repair, Hysterectomy, and Thoracotomy. Anesthesiology 2015, 122, 1123–1141. [Google Scholar] [CrossRef] [PubMed]
- Schreiber, K.L.; Martel, M.O.; Shnol, H.; Shaffer, J.R.; Greco, C.; Viray, N.; Taylor, L.N.; McLaughlin, M.; Brufsky, A.; Ahrendt, G.; et al. Persistent Pain in Postmastectomy Patients: Comparison of Psychophysical, Medical, Surgical, and Psychosocial Characteristics between Patients with and without Pain. Pain 2013, 154, 660–668. [Google Scholar] [CrossRef]
- Edwards, R.R.; Campbell, C.; Schreiber, K.L.; Meints, S.; Lazaridou, A.; Martel, M.O.; Cornelius, M.; Xu, X.; Jamison, R.N.; Katz, J.N.; et al. Multimodal Prediction of Pain and Functional Outcomes 6 Months Following Total Knee Replacement: A Prospective Cohort Study. BMC Musculoskelet. Disord. 2022, 23, 302. [Google Scholar] [CrossRef]
- Bayman, E.O.; Parekh, K.R.; Keech, J.; Larson, N.; Vander Weg, M.; Brennan, T.J. Preoperative Patient Expectations of Postoperative Pain Are Associated with Moderate to Severe Acute Pain after VATS. Pain Med. 2019, 20, 543–554. [Google Scholar] [CrossRef]
- Paller, C.J.; Campbell, C.M.; Edwards, R.R.; Dobs, A.S. Sex-Based Differences in Pain Perception and Treatment. Pain Med. 2009, 10, 289–299. [Google Scholar] [CrossRef]
- Kwon, S.T.; Zhao, L.; Reddy, R.M.; Chang, A.C.; Orringer, M.B.; Brummett, C.M.; Lin, J. Evaluation of Acute and Chronic Pain Outcomes after Robotic, Video-Assisted Thoracoscopic Surgery, or Open Anatomic Pulmonary Resection. J. Thorac. Cardiovasc. Surg. 2017, 154, 652–659.e1. [Google Scholar] [CrossRef]
- Kampe, S.; Wendland, M.; Welter, S.; Aigner, C.; Hachenberg, T.; Ebmeyer, U.; Weinreich, G. Independent Predictors for Higher Postoperative Pain Intensity during Recovery after Open Thoracic Surgery: A Retrospective Analysis in 621 Patients. Pain Med. 2018, 19, 1667–1673. [Google Scholar] [CrossRef] [PubMed]
- Gerbershagen, H.J.; Pogatzki-Zahn, E.; Aduckathil, S.; Peelen, L.M.; Kappen, T.H.; Van Wijck, A.J.M.; Kalkman, C.J.; Meissner, W. Procedure-Specific Risk Factor Analysis for the Development of Severe Postoperative Pain. Anesthesiology 2014, 120, 1237–1245. [Google Scholar] [CrossRef] [PubMed]
- Kalkman, J.C.; Visser, K.; Moen, J.; Bonsel, J.G.; Grobbee, E.D.; Moons, M.K.G. Preoperative Prediction of Severe Postoperative Pain. Pain 2003, 105, 415–423. [Google Scholar] [CrossRef] [PubMed]
- Schnabel, A.; Yahiaoui-Doktor, M.; Meissner, W.; Zahn, P.K.; Pogatzki-Zahn, E.M. Predicting Poor Postoperative Acute Pain Outcome in Adults: An International, Multicentre Database Analysis of Risk Factors in 50,005 Patients. Pain Rep. 2020, 5, e831. [Google Scholar] [CrossRef]
- Harris, P.A.; Taylor, R.; Thielke, R.; Payne, J.; Gonzalez, N.; Conde, J.G. Research Electronic Data Capture (REDCap)—A Metadata-Driven Methodology and Workflow Process for Providing Translational Research Informatics Support. J. Biomed. Inf. 2009, 42, 377–381. [Google Scholar] [CrossRef]
- Harris, P.A.; Taylor, R.; Minor, B.L.; Elliott, V.; Fernandez, M.; O’Neal, L.; McLeod, L.; Delacqua, G.; Delacqua, F.; Kirby, J.; et al. The REDCap Consortium: Building an International Community of Software Platform Partners. J. Biomed. Inform. 2019, 95, 103208. [Google Scholar] [CrossRef]
- Cella, D.; Riley, W.; Stone, A.; Rothrock, N.; Reeve, B.; Yount, S.; Amtmann, D.; Bode, R.; Buysse, D.; Choi, S.; et al. The Patient-Reported Outcomes Measurement Information System (PROMIS) Developed and Tested Its First Wave of Adult Self-Reported Health Outcome Item Banks: 2005-2008. J. Clin. Epidemiol. 2010, 63, 1179–1194. [Google Scholar] [CrossRef]
- Cleeland, C.S.; Ryan, K.M. Pain Assessment: Global Use of the Brief Pain Inventory. Ann. Acad. Med. Singap. 1994, 23, 129–138. [Google Scholar] [PubMed]
- Hayes, A.F. Introduction to Mediation, Moderation, and Conditional Process Analysis: A Regression-Based Approach, 3rd ed.; Methodology in the Social Sciences; The Guilford Press: New York, NY, USA; London, UK, 2022; ISBN 978-1-4625-4903-0. [Google Scholar]
- Chan, J.J.I.; Tan, C.W.; Yeam, C.T.; Sultana, R.; Sia, A.T.H.; Habib, A.S.; Sng, B.L. Risk Factors Associated with Development of Acute and Sub-Acute Post-Cesarean Pain: A Prospective Cohort Study. J. Pain Res. 2020, 13, 2317–2328. [Google Scholar] [CrossRef]
- Katz, J.; Jackson, M.; Kavanagh, B.P.; Sandler, A.N. Acute Pain after Thoracic Surgery Predicts Long-Term Post-Thoracotomy Pain. Clin. J. Pain 1996, 12, 50–55. [Google Scholar] [CrossRef]
- Bayman, E.O.; Parekh, K.R.; Keech, J.; Selte, A.; Brennan, T.J. A Prospective Study of Chronic Pain after Thoracic Surgery. Anesthesiology 2017, 126, 938–951. [Google Scholar] [CrossRef] [PubMed]
- Blichfeldt-Eckhardt, M.R.; Andersen, C.; Ørding, H.; Licht, P.; Toft, P. From Acute to Chronic Pain after Thoracic Surgery: The Significance of Different Components of the Acute Pain Response. J. Pain Res. 2018, 11, 1541–1548. [Google Scholar] [CrossRef]
- Horn-Hofmann, C.; Scheel, J.; Dimova, V.; Parthum, A.; Carbon, R.; Griessinger, N.; Sittl, R.; Lautenbacher, S. Prediction of Persistent Post-operative Pain: Pain-specific Psychological Variables Compared with Acute Post-operative Pain and General Psychological Variables. Eur. J. Pain 2018, 22, 191–202. [Google Scholar] [CrossRef] [PubMed]
- Wildgaard, K.; Ringsted, T.K.; Hansen, H.J.; Petersen, R.H.; Kehlet, H. Persistent Postsurgical Pain after Video-assisted Thoracic Surgery—An Observational Study. Acta Anaesthesiol. Scand. 2016, 60, 650–658. [Google Scholar] [CrossRef]
- Khan, J.S.; Dana, E.; Xiao, M.Z.X.; Rao, V.; Djaiani, G.; Seltzer, Z.; Ladha, K.; Huang, A.; McRae, K.; Cypel, M.; et al. Prevalence and Risk Factors for Chronic Postsurgical Pain after Thoracic Surgery: A Prospective Cohort Study. J. Cardiothorac. Vasc. Anesth. 2024, 38, 490–498. [Google Scholar] [CrossRef] [PubMed]
- Auinger, D.; Sandner-Kiesling, A.; Strießnig, A.; Lindenmann, J.; Smolle, J.; Friedl, H.; Smolle-Jüttner, F.-M. Is There an Impact of Sex on Acute Postthoracotomy Pain? A Retrospective Analysis. Ann. Thorac. Surg. 2020, 109, 1104–1111. [Google Scholar] [CrossRef]
- Ochroch, E.A.; Gottschalk, A.; Troxel, A.B.; Farrar, J.T. Women Suffer More Short and Long-Term Pain than Men after Major Thoracotomy. Clin. J. Pain 2006, 22, 491–498. [Google Scholar] [CrossRef]
- Lim, J.; Chen, D.; McNicol, E.; Sharma, L.; Varaday, G.; Sharma, A.; Wilson, E.; Wright-Yatsko, T.; Yaeger, L.; Gilron, I.; et al. Risk Factors for Persistent Pain after Breast and Thoracic Surgeries: A Systematic Literature Review and Meta-Analysis. Pain 2022, 163, 3–20. [Google Scholar] [CrossRef]
- Carstensen, L.L.; Pasupathi, M.; Mayr, U.; Nesselroade, J.R. Emotional Experience in Everyday Life across the Adult Life Span. J. Personal. Soc. Psychol. 2000, 79, 644–655. [Google Scholar] [CrossRef]
- Mroczek, D.K.; Kolarz, C.M. The Effect of Age on Positive and Negative Affect: A Developmental Perspective on Happiness. J. Personal. Soc. Psychol. 1998, 75, 1333–1349. [Google Scholar] [CrossRef]
- Peng, Z.; Li, H.; Zhang, C.; Qian, X.; Feng, Z.; Zhu, S. A Retrospective Study of Chronic Post-Surgical Pain Following Thoracic Surgery: Prevalence, Risk Factors, Incidence of Neuropathic Component, and Impact on Qualify of Life. PLoS ONE 2014, 9, e90014. [Google Scholar] [CrossRef] [PubMed]
- Doering, L.V.; McGuire, A.; Eastwood, J.-A.; Chen, B.; Bodán, R.C.; Czer, L.S.; Irwin, M.R. Cognitive Behavioral Therapy for Depression Improves Pain and Perceived Control in Cardiac Surgery Patients. Eur. J. Cardiovasc. Nurs. 2016, 15, 417–424. [Google Scholar] [CrossRef]
- Hanley, A.W.; Gililland, J.; Erickson, J.; Pelt, C.; Peters, C.; Rojas, J.; Garland, E.L. Brief Preoperative Mind–Body Therapies for Total Joint Arthroplasty Patients: A Randomized Controlled Trial. Pain 2021, 162, 1749–1757. [Google Scholar] [CrossRef] [PubMed]
- Nicholls, J.L.; Azam, M.A.; Burns, L.C.; Englesakis, M.; Sutherland, A.M.; Weinrib, A.Z.; Katz, J.; Clarke, H. Psychological Treatments for the Management of Postsurgical Pain: A Systematic Review of Randomized Controlled Trials. Patient Relat. Outcome Meas. 2018, 9, 49–64. [Google Scholar] [CrossRef] [PubMed]
- Racine, M.; Solé, E.; Sánchez-Rodríguez, E.; Tomé-Pires, C.; Roy, R.; Jensen, M.P.; Miró, J.; Moulin, D.E.; Cane, D. An Evaluation of Sex Differences in Patients with Chronic Pain Undergoing an Interdisciplinary Pain Treatment Program. Pain Pract. 2020, 20, 62–74. [Google Scholar] [CrossRef]
- Bartley, E.J.; Fillingim, R.B. Sex Differences in Pain: A Brief Review of Clinical and Experimental Findings. Br. J. Anaesth. 2013, 111, 52–58. [Google Scholar] [CrossRef]
- Dubert, M.; Pourbaix, A.; Alkhoder, S.; Mabileau, G.; Lescure, F.-X.; Ghodhbane, W.; Belorgey, S.; Rioux, C.; Armand-Lefèvre, L.; Wolff, M.; et al. Sternal Wound Infection after Cardiac Surgery: Management and Outcome. PLoS ONE 2015, 10, e0139122. [Google Scholar] [CrossRef][Green Version]
- Meszaros, K.; Fuehrer, U.; Grogg, S.; Sodeck, G.; Czerny, M.; Marschall, J.; Carrel, T. Risk Factors for Sternal Wound Infection after Open Heart Operations Vary According to Type of Operation. Ann. Thorac. Surg. 2016, 101, 1418–1425. [Google Scholar] [CrossRef]
- Guru, V.; Fremes, S.E.; Austin, P.C.; Blackstone, E.H.; Tu, J.V. Gender Differences in Outcomes after Hospital Discharge from Coronary Artery Bypass Grafting. Circulation 2006, 113, 507–516. [Google Scholar] [CrossRef]
- Hirji, S.A.; Guetter, C.R.; Trager, L.; Yazdchi, F.; Landino, S.; Lee, J.; Anastasopulos, A.; Percy, E.; McGurk, S.; Pelletier, M.P.; et al. Sex-Based Differences in Mitral Valve Re-Operation after Mitral Valve Repair: Truth or Myth? Am. J. Surg. 2020, 220, 1344–1350. [Google Scholar] [CrossRef]
- Bradley, S.; White, R.S.; Jiang, S.Y.; Ma, X.; Hoyler, M.M.; Muehlschlegel, J.D.; Karamnov, S.; Tangel, V.E.; Lanahan, J.; Rong, L.Q. Sex Differences in In-Hospital Mortality after Open Cardiac Valve Surgery. Anesth. Analg. 2022, 135, 944–953. [Google Scholar] [CrossRef] [PubMed]
- Guazzi, M.; Arena, R. Endothelial Dysfunction and Pathophysiological Correlates in Atrial Fibrillation. Heart 2009, 95, 102–106. [Google Scholar] [CrossRef] [PubMed]
- Al-Khalili, F.; Eriksson, M.; Landgren, B.-M.; Schenck-Gustafsson, K. Effect of Conjugated Estrogen on Peripheral Flow-Mediated Vasodilation in Postmenopausal Women. Am. J. Cardiol. 1998, 82, 215–218. [Google Scholar] [CrossRef] [PubMed]
- Harding, A.T.; Heaton, N.S. The Impact of Estrogens and Their Receptors on Immunity and Inflammation during Infection. Cancers 2022, 14, 909. [Google Scholar] [CrossRef] [PubMed]
- Desborough, J.P. The Stress Response to Trauma and Surgery. Br. J. Anaesth. 2000, 85, 109–117. [Google Scholar] [CrossRef]
- Hernandez-Leon, A.; De La Luz-Cuellar, Y.E.; Granados-Soto, V.; González-Trujano, M.E.; Fernández-Guasti, A. Sex Differences and Estradiol Involvement in Hyperalgesia and Allodynia in an Experimental Model of Fibromyalgia. Horm. Behav. 2018, 97, 39–46. [Google Scholar] [CrossRef]
- Kundakovic, M.; Rocks, D. Sex Hormone Fluctuation and Increased Female Risk for Depression and Anxiety Disorders: From Clinical Evidence to Molecular Mechanisms. Front. Neuroendocrinol. 2022, 66, 101010. [Google Scholar] [CrossRef]
- Lavernia, C.J.; Alcerro, J.C.; Contreras, J.S.; Rossi, M.D. Ethnic and Racial Factors Influencing Well-Being, Perceived Pain, and Physical Function after Primary Total Joint Arthroplasty. Clin. Orthop. Relat. Res. 2011, 469, 1838–1845. [Google Scholar] [CrossRef]
- Badreldin, N.; Grobman, W.A.; Yee, L.M. Racial Disparities in Postpartum Pain Management. Obstet. Gynecol. 2019, 134, 1147–1153. [Google Scholar] [CrossRef]
- Faucett, J.; Gordon, N.; Levine, J. Differences in Postoperative Pain Severity among Four Ethnic Groups. J. Pain Symptom Manag. 1994, 9, 383–389. [Google Scholar] [CrossRef]
- Fecho, K.; Miller, N.R.; Merritt, S.A.; Klauber-DeMore, N.; Hultman, C.S.; Blau, W.S. Acute and Persistent Postoperative Pain after Breast Surgery. Pain Med. 2009, 10, 708–715. [Google Scholar] [CrossRef] [PubMed]
| Males (n = 45) | Females (n = 60) | ||
|---|---|---|---|
| Mean ± SD or n (%) | Mean ± SD or n (%) | p-Value | |
| Age (n = 105) | 67.0 ± 9.2 | 63.3 ± 11.7 | 0.15 |
| BMI (n = 105) | 28.3 ± 4.9 | 27.6 ± 5.5 | 0.37 |
| White race (n = 105) | 43 (96%) | 57 (95%) | 0.90 |
| Currently smoking/tobacco use (n = 105) | 2 (4%) | 4 (7%) | 0.63 |
| Preoperative cancer diagnosis (n = 105) | 0.93 | ||
| No | 2 (4.4%) | 2 (3%) | |
| Yes | 11 (24.4%) | 16 (27%) | |
| Unknown | 32 (71.1%) | 42 (70%) | |
| Had prior chest surgery on same side (n = 99) | 6 (14%) | 14 (25%) | 0.18 |
| Type of surgery (n = 105) | 0.34 | ||
| Minor VATS surgery (e.g., biopsy, wedge resection) | 26 (58%) | 40 (67%) | |
| Major VATS surgery (e.g., VATS segmentectomy) | 10 (22%) | 14 (23%) | |
| Thoracotomy | 9 (20%) | 6 (10%) | |
| More than 1 chest tube (n = 104) | 9 (20%) | 6 (10%) | 0.16 |
| Size of chest tube (n = 97) | 0.57 | ||
| 14 | 1 (2%) | ||
| 19 | 6 (14%) | 11 (20%) | |
| 24 | 21 (49%) | 27 (50%) | |
| 28 | 16 (37%) | 15 (28%) | |
| Had postoperative complications (n = 105) | 16 (36%) | 14 (23%) | 0.17 |
| Length of stay (n = 105) | 3.9 ± 3.1 | 3.3 ± 2.8 | 0.21 |
| Acute Pain Severity | p-Value | |
|---|---|---|
| Age (n = 105) | −0.05 | 0.63 |
| BMI (n = 105) | −0.09 | 0.39 |
| Race (n = 105) | 0.54 | |
| White | 5.61 ± 2.18 | |
| Non-White | 4.10 ± 1.73 | |
| Current smoking/tobacco use (n = 105) | 0.12 | |
| No | 5.50 ± 2.17 | |
| Yes | 6.93 ± 1.59 | |
| Preoperative cancer diagnosis (n = 105) | 0.17 | |
| No | 6.86 ± 1.91 | |
| Yes | 6.05 ± 1.79 | |
| Unknown | 5.34 ± 2.27 | |
| Prior chest surgery, same side (n = 99) | 0.93 | |
| No | 5.62 ± 2.16 | |
| Yes | 5.67 ± 2.20 | |
| Type of surgery (n = 105) | 0.35 | |
| Minor VATS surgery (e.g., biopsy, wedge resection) | 5.67 ± 2.23 | |
| Major VATS surgery (e.g., VATS segmentectomy) | 5.06 ± 2.13 | |
| Thoracotomy | 6.03 ± 1.88 | |
| Number of chest tubes (n = 104) | 0.39 | |
| 1 | 5.50 ± 2.24 | |
| 2 | 6.02 ± 1.66 | |
| Size of chest tube (n = 97) | 0.16 | |
| 14 | 4.2 ± 3.3 | |
| 19 | 5.8 ± 2.0 | |
| 24 | 5.2 ± 2.3 | |
| 28 | 5.4 ± 2.3 | |
| Postoperative complications (n = 105) | 0.41 | |
| No | 5.58 ± 2.13 | |
| Yes | 6.39 ± 2.49 | |
| Length of stay (n = 105) | 0.14 | 0.17 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Franqueiro, A.R.; Wilson, J.M.; He, J.; Azizoddin, D.R.; Karamnov, S.; Rathmell, J.P.; Soens, M.; Schreiber, K.L. Prospective Study of Preoperative Negative Affect and Postoperative Pain in Patients Undergoing Thoracic Surgery: The Moderating Role of Sex. J. Clin. Med. 2024, 13, 5722. https://doi.org/10.3390/jcm13195722
Franqueiro AR, Wilson JM, He J, Azizoddin DR, Karamnov S, Rathmell JP, Soens M, Schreiber KL. Prospective Study of Preoperative Negative Affect and Postoperative Pain in Patients Undergoing Thoracic Surgery: The Moderating Role of Sex. Journal of Clinical Medicine. 2024; 13(19):5722. https://doi.org/10.3390/jcm13195722
Chicago/Turabian StyleFranqueiro, Angelina R., Jenna M. Wilson, Jingui He, Desiree R. Azizoddin, Sergey Karamnov, James P. Rathmell, Mieke Soens, and Kristin L. Schreiber. 2024. "Prospective Study of Preoperative Negative Affect and Postoperative Pain in Patients Undergoing Thoracic Surgery: The Moderating Role of Sex" Journal of Clinical Medicine 13, no. 19: 5722. https://doi.org/10.3390/jcm13195722
APA StyleFranqueiro, A. R., Wilson, J. M., He, J., Azizoddin, D. R., Karamnov, S., Rathmell, J. P., Soens, M., & Schreiber, K. L. (2024). Prospective Study of Preoperative Negative Affect and Postoperative Pain in Patients Undergoing Thoracic Surgery: The Moderating Role of Sex. Journal of Clinical Medicine, 13(19), 5722. https://doi.org/10.3390/jcm13195722





