Asymmetry in Atypical Parkinsonian Syndromes—A Review
Abstract
:1. Introduction
2. Materials and Methods
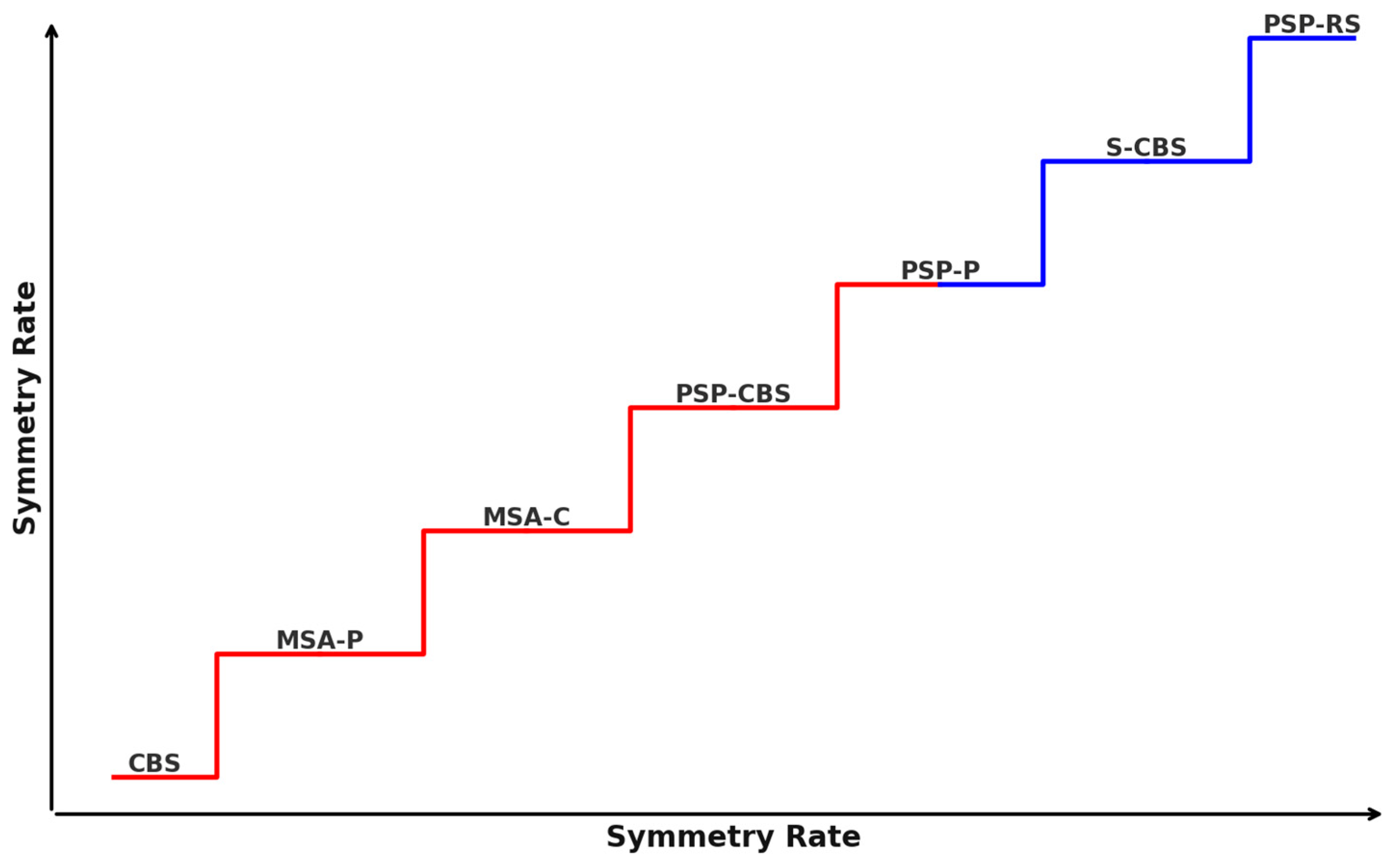
3. Atypical Parkinsonism’s Clinical Symptom Asymmetry
4. Brain Lateralization
5. Imaging Tests
6. MRI
7. Single-Photon Emission Computed Tomography (SPECT)
8. PET
9. Transcranial Sonography
10. Discussion
11. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| APSs | atypical parkinsonian syndromes |
| IPD | idiopathic Parkinson’s disease |
| MSA | multiple system atrophy |
| PSP | progressive supranuclear palsy |
| CBS | corticobasal syndrome |
| DLB | dementia with Lewy bodies |
| SPECT | single-photon emission computed tomography |
| PD | Parkinson’s disease |
| PSP-RS | progressive supranuclear palsy-Richardson syndrome |
| NNIPPS | Neuroprotection and natural history in Parkinson plus syndromes |
| PSP-P | progressive supranuclear palsy-parkinsonism |
| PSP-CBS | progressive supranuclear palsy-corticobasal syndrome |
| MDS | Movement Disorder Society |
| PSP-PAGF | progressive supranuclear palsy-pure akinesia with gait freezing |
| PSP-FTD | progressive supranuclear palsy-frontotemporal dementia |
| PSP-AOS | progressive supranuclear palsy-apraxia of speech syndrome |
| PSP-PNFA | progressive supranuclear palsy-progressive non-fluent aphasia |
| Hemi-PSP | progressive supranuclear palsy with a lateralized disease manifestation |
| SymPSP | progressive supranuclear palsy with symmetric clinical presentation, a symmetric disease manifestation |
| CBD | corticobasal degeneration |
| S-CBD | symmetric corticobasal degeneration |
| CBD-CBS | corticobasal degeneration-corticobasal syndrome |
| CBD-RS | corticobasal degeneration-Richardson syndrome |
| MSA-P | multiple system atrophy-parkinsonism |
| MSA-C | multiple system atrophy-cerebellum |
| MRI | magnetic resonance imaging |
| PET | positron emission tomography |
| DTI | diffusion tensor imaging |
| MD | mean diffusivity |
| FA | fractional anisotropy |
| FLAIR | fluid-attenuated inversion recovery |
| HCB | “hot cross bun” sign |
| DaTscan | dopamine transporter scan |
| DaT-SPECT | dopamine transporter single-photon emission computed tomography |
| AI | asymmetry index |
| SUVRs | standardized uptake value ratios |
| FDG PET | fludeoxyglucose-18 positron emission tomography |
| 18F-DOPA | 18F-dihydroxyphenylalanine |
| TCS | transcranial sonography |
| SN | substantia nigra |
| LN | lenticular nucleus |
| LID | levodopa-induced dyskinesia |
References
- Levin, J.; Kurz, A.; Arzberger, T.; Giese, A.; Höglinger, G.U. The Differential Diagnosis and Treatment of Atypical Parkinsonism. Dtsch. Aerztebl. Int. 2016, 113, 61–69. [Google Scholar] [CrossRef] [PubMed]
- Lo, R.Y. Epidemiology of atypical parkinsonian syndromes. Tzu Chi Med. J. 2022, 34, 169–181. [Google Scholar] [CrossRef] [PubMed]
- Vertes, A.C.; Beato, M.R.; Sonne, J.; Khan Suheb, M.Z. Parkinson-Plus Syndrome; StatPearls Publishing: Treasure Island, FL, USA, 2024. [Google Scholar]
- Oba, H.; Yagishita, A.; Terada, H.; Barkovich, A.J.; Kutomi, K.; Yamauchi, T.; Furui, S.; Shimizu, T.; Uchigata, M.; Matsumura, K.; et al. New Reliab. MRI Diagn. Progress. Supranuclear Palsy. Neurology 2005, 64, 2050–2055. [Google Scholar] [CrossRef] [PubMed]
- Daniel, S.E.; Lees, A.J. Parkinson’s Disease Society Brain Bank, London: Overview and Research. J. Neural Transm. Suppl. 1993, 39, 165–172. [Google Scholar]
- Murphy, K.T.; Lynch, G.S. Impaired skeletal muscle health in Parkinsonian syndromes: Clinical implications, mechanisms and potential treatments. J. Cachex Sarcopenia Muscle 2023, 14, 1987–2002. [Google Scholar] [CrossRef]
- Wenning, G.K.; Stankovic, I.; Vignatelli, L.; Fanciulli, A.; Calandra-Buonaura, G.; Seppi, K.; Palma, J.; Meissner, W.G.; Krismer, F.; Berg, D.; et al. The Movement Disorder Society Criteria for the Diagnosis of Multiple System Atrophy. Mov. Disord. 2022, 37, 1131–1148. [Google Scholar] [CrossRef] [PubMed]
- Armstrong, M.J.; Litvan, I.; Lang, A.E.; Bak, T.H.; Bhatia, K.P.; Borroni, B.; Boxer, A.L.; Dickson, D.W.; Grossman, M.; Hallett, M.; et al. Criteria for the diagnosis of corticobasal degeneration. Neurology 2013, 80, 496–503. [Google Scholar] [CrossRef]
- Höglinger, G.U.; Respondek, G.; Stamelou, M.; Kurz, C.; Josephs, K.A.; Lang, A.E.; Mollenhauer, B.; Müller, U.; Nilsson, C.; Whitwell, J.L.; et al. Clinical diagnosis of progressive supranuclear palsy: The movement disorder society criteria. Mov. Disord. 2017, 32, 853–864. [Google Scholar] [CrossRef]
- Jankovic, J. Parkinson’s disease: Clinical features and diagnosis. J. Neurol. Neurosurg. Psychiatry 2008, 79, 368–376. [Google Scholar] [CrossRef]
- Martin, W.W.; Miles, M.; Zhong, Q.; Hartlein, J.; Racette, B.A.; Norris, S.A.; Ushe, M.; Maiti, B.; Criswell, S.; Davis, A.A.; et al. Is Levodopa Response a Valid Indicator of Parkinson’s Disease? Mov. Disord. 2021, 36, 948–954. [Google Scholar] [CrossRef]
- Bologna, M.; Suppa, A.; Di Stasio, F.; Conte, A.; Fabbrini, G.; Berardelli, A. Neurophysiological studies on atypical parkinsonian syndromes. Park. Relat. Disord. 2017, 42, 12–21. [Google Scholar] [CrossRef] [PubMed]
- Meijer, F.J.; Bloem, B.R.; Mahlknecht, P.; Seppi, K.; Goraj, B. Update on diffusion MRI in Parkinson’s disease and atypical parkinsonism. J. Neurol. Sci. 2013, 332, 21–29. [Google Scholar] [CrossRef] [PubMed]
- Talai, A.S.; Sedlacik, J.; Boelmans, K.; Forkert, N.D. Utility of Multi-Modal MRI for Differentiating of Parkinson’s Disease and Progressive Supranuclear Palsy Using Machine Learning. Front. Neurol. 2021, 12, 648548. [Google Scholar] [CrossRef]
- Miki, Y.; Foti, S.C.; Asi, Y.T.; Tsushima, E.; Quinn, N.; Ling, H.; Holton, J.L. Improving diagnostic accuracy of multiple system atrophy: A clinicopathological study. Brain 2019, 142, 2813–2827. [Google Scholar] [CrossRef]
- Malarte, M.-L.; Gillberg, P.-G.; Kumar, A.; Bogdanovic, N.; Lemoine, L.; Nordberg, A. Discriminative binding of tau PET tracers PI2620, MK6240 and RO948 in Alzheimer’s disease, corticobasal degeneration and progressive supranuclear palsy brains. Mol. Psychiatry 2023, 28, 1272–1283. [Google Scholar] [CrossRef]
- Liu, Z.; Cheung, H.-H. Stem Cell-Based Therapies for Parkinson Disease. Int. J. Mol. Sci. 2020, 21, 8060. [Google Scholar] [CrossRef] [PubMed]
- Kowalska-Taczanowska, R.; Friedman, A.; Koziorowski, D. Parkinson’s disease or atypical parkinsonism? The importance of acoustic voice analysis in differential diagnosis of speech disorders. Brain Behav. 2020, 10, e01700. [Google Scholar] [CrossRef]
- Litvan, I.; Agid, Y.; Calne, D.; Campbell, G.; Dubois, B.; Duvoisin, R.C.; Goetz, C.G.; Golbe, L.I.; Grafman, J.; Growdon, J.H.; et al. Clinical research criteria for the diagnosis of progressive supranuclear palsy (Steele-Richardson-Olszewski syndrome): Report of the NINDS-SPSP international workshop. Neurology 1996, 47, 1–9. [Google Scholar] [CrossRef]
- Gultekin, M. Phenotypic Variants of Patients with Progressive Supranuclear Palsy. Noro Psikiyatr. Ars. 2020, 57, 61–64. [Google Scholar] [CrossRef]
- Picillo, M.; Tepedino, M.F.; Abate, F.; Ponticorvo, S.; Erro, R.; Cuoco, S.; Oksuz, N.; Di Salle, G.; Di Salle, F.; Esposito, F.; et al. Uncovering clinical and radiological asymmetry in progressive supranuclear palsy—Richardson’s syndrome. Neurol. Sci. 2022, 43, 3677–3682. [Google Scholar] [CrossRef]
- Kishore, A.; Mahale, R.; Krishnan, S.; Divya, K.; Jisha, V. Subtypes of PSP and prognosis: A retrospective analysis. Ann. Indian Acad. Neurol. 2021, 24, 56–62. [Google Scholar] [CrossRef]
- Hassan, A.; Whitwell, J.L.; Boeve, B.F.; Jack, C.R.; Parisi, J.E.; Dickson, D.W.; Josephs, K.A. Symmetric corticobasal degeneration (S-CBD). Park. Relat. Disord. 2010, 16, 208–214. [Google Scholar] [CrossRef] [PubMed]
- Wunderlich, J.; Behler, A.; Dreyhaupt, J.; Ludolph, A.C.; Pinkhardt, E.H.; Kassubek, J. Diagnostic value of video-oculography in progressive supranuclear palsy: A controlled study in 100 patients. J. Neurol. 2021, 268, 3467–3475. [Google Scholar] [CrossRef] [PubMed]
- Stezin, A.; Holla, V.V.; Chaithra, S.; Kamble, N.; Saini, J.; Yadav, R.; Pal, P.K. Asymmetric Limb Dystonia in Progressive Supranuclear Palsy: Conundrum in Nosology. Mov. Disord. Clin. Pr. 2019, 6, 415–416. [Google Scholar] [CrossRef]
- Amtage, F.; Hellwig, S.; Kreft, A.; Spehl, T.; Glauche, V.; Winkler, C.; Rijntjes, M.; Hellwig, B.; Weiller, C.; Weber, W.A.; et al. Neuronal Correlates of Clinical Asymmetry in Progressive Supranuclear Palsy. Clin. Nucl. Med. 2014, 39, 319–325. [Google Scholar] [CrossRef]
- Chung, E.J.; Cho, H.J.; Jang, W.; Hur, D.Y.; Kim, Y.S.; Lee, K.-H.; Kim, S.J. A Case of Pathologically Confirmed Corticobasal Degeneration Initially Presenting as Progressive Supranuclear Palsy Syndrome. J. Korean Med. Sci. 2022, 37, e183. [Google Scholar] [CrossRef]
- Liscic, R.M.; Srulijes, K.; Gröger, A.; Maetzler, W.; Berg, D. Differentiation of Progressive Supranuclear Palsy: Clinical, imaging and laboratory tools. Acta Neurol. Scand. 2013, 127, 362–370. [Google Scholar] [CrossRef]
- Kouri, N.; Murray, M.E.; Hassan, A.; Rademakers, R.; Uitti, R.J.; Boeve, B.F.; Graff-Radford, N.R.; Wszolek, Z.K.; Litvan, I.; Josephs, K.A.; et al. Neuropathological features of corticobasal degeneration presenting as corticobasal syndrome or Richardson syndrome. Brain 2011, 134 Pt 11, 3264–3275. [Google Scholar] [CrossRef]
- Niethammer, M.; Tang, C.C.; Feigin, A.; Allen, P.J.; Heinen, L.; Hellwig, S.; Amtage, F.; Hanspal, E.; Vonsattel, J.P.; Poston, K.L.; et al. A disease-specific metabolic brain network associated with corticobasal degeneration. Brain 2014, 137 Pt 11, 3036–3046. [Google Scholar] [CrossRef]
- Kwon, K.; Choi, C.G.; Kim, J.S.; Lee, M.C.; Chung, S.J. Comparison of brain MRI and 18F-FDG PET in the differential diagnosis of multiple system atrophy from Parkinson’s disease. Mov. Disord. 2007, 22, 2352–2358. [Google Scholar] [CrossRef]
- Van Laere, K.; Casteels, C.; De Ceuninck, L.; Vanbilloen, B.; Maes, A.; Mortelmans, L.; Vandenberghe, W.; Verbruggen, A. Dom, RDual-tracer dopamine transporter and perfusion SPECT in differential diagnosis of parkinsonism using template-based discriminant analysis. J. Nucl. Med. 2006, 47, 384–392. [Google Scholar]
- Kathuria, H.; Mehta, S.; Ahuja, C.K.; Chakravarty, K.; Ray, S.; Mittal, B.R.; Singh, P.; Lal, V. Utility of Imaging of Nigrosome-1 on 3T MRI and Its Comparison with 18F-DOPA PET in the Diagnosis of Idiopathic Parkinson Disease and Atypical Parkinsonism. Mov. Disord. Clin. Pr. 2020, 8, 224–230. [Google Scholar] [CrossRef] [PubMed]
- Faurie, C.; Raymond, M. Handedness frequency over more than ten thousand years. Proc. R. Soc. B Biol. Sci. 2004, 271, S43–S45. [Google Scholar] [CrossRef] [PubMed]
- Tejavibulya, L.; Peterson, H.; Greene, A.; Gao, S.; Rolison, M.; Noble, S.; Scheinost, D. Large-scale differences in functional organization of left- and right-handed individuals using whole-brain, data-driven analysis of connectivity. Neuroimage 2022, 252, 119040. [Google Scholar] [CrossRef] [PubMed]
- Vingerhoets, G.; Acke, F.; Alderweireldt, A.S.; Nys, J.; Vandemaele, P.; Achten, E. Cerebral lateralization of praxis in right- and left-handedness: Same pattern, different strength. Hum. Brain Mapp. 2012, 33, 763–777. [Google Scholar] [CrossRef] [PubMed]
- Kato, N.; Arai, K.; Hattori, T. Study of the rostral midbrain atrophy in progressive supranuclear palsy. J. Neurol. Sci. 2003, 210, 57–60. [Google Scholar] [CrossRef]
- Adachi, M.; Kawanami, T.; Ohshima, H.; Sugai, Y.; Hosoya, T. Morning Glory Sign: A Particular MR Finding in Progressive Supranuclear Palsy. Magn. Reson. Med Sci. 2004, 3, 125–132. [Google Scholar] [CrossRef]
- Smith, R.; Schain, M.; Nilsson, C.; Strandberg, O.; Olsson, T.; Hägerström, D.; Jögi, J.; Borroni, E.; Schöll, M.; Honer, M.; et al. Increased basal ganglia binding of 18F-AV-1451 in patients with progressive supranuclear palsy. Mov. Disord. 2017, 32, 108–114. [Google Scholar] [CrossRef]
- Whitwell, J.L.; Xu, J.; Mandrekar, J.N.; Gunter, J.L.; Jack, C.R.; Josephs, K.A. Rates of brain atrophy and clinical decline over 6 and 12-month intervals in PSP: Determining sample size for treatment trials. Park. Relat. Disord. 2011, 18, 252–256. [Google Scholar] [CrossRef]
- Bopp, M.H.A.; Emde, J.; Carl, B.; Nimsky, C.; Saß, B. Diffusion Kurtosis Imaging Fiber Tractography of Major White Matter Tracts in Neurosurgery. Brain Sci. 2021, 11, 381. [Google Scholar] [CrossRef]
- Moretti, R.; Caberlotto, R.; Signori, R. Apathy in corticobasal degeneration: Possible parietal involvement. Funct. Neurol. 2017, 22, 201–210. [Google Scholar] [CrossRef] [PubMed]
- Caso, F.; Canu, E.; Lukic, M.J.; Petrovic, I.N.; Fontana, A.; Nikolic, I.; Kostic, V.S.; Filippi, M.; Agosta, F. Cognitive impairment and structural brain damage in multiple system atrophy-parkinsonian variant. J. Neurol. 2019, 267, 87–94. [Google Scholar] [CrossRef]
- Whitwell, J.L.; Schwarz, C.G.; Reid, R.I.; Kantarci, K.; Jack, C.R.; Josephs, K.A. Diffusion tensor imaging comparison of progressive supranuclear palsy and corticobasal syndromes. Park. Relat. Disord. 2014, 20, 493–498. [Google Scholar] [CrossRef] [PubMed]
- Stamelou, M.; Respondek, G.; Giagkou, N.; Whitwell, J.L.; Kovacs, G.G.; Höglinger, G.U. Evolving concepts in progressive supranuclear palsy and other 4-repeat tauopathies. Nat. Rev. Neurol. 2021, 17, 601–620. [Google Scholar] [CrossRef]
- Koga, S.A.; Josephs, K.; Aiba, I.; Yoshida, M.; Dickson, D.W. Neuropathology and emerging biomarkers in corticobasal syndrome. J. Neurol. Neurosurg. Psychiatry 2022, 93, 919–929. [Google Scholar] [CrossRef]
- Risacher, S.L.; Saykin, A.J. Neuroimaging in aging and neurologic diseases. Handb Clin Neurol. 2019, 167, 191–227. [Google Scholar] [CrossRef] [PubMed]
- Heim, B.; Krismer, F.; Seppi, K. Structural Imaging in Atypical Parkinsonism. Int. Rev. Neurobiol. 2018, 142, 67–148. [Google Scholar] [CrossRef]
- Michalowski, B.; Buchwald, M.; Klichowski, M.; Ras, M.; Kroliczak, G. Action goals and the praxis network: An fMRI study. Brain Struct. Funct. 2022, 227, 2261–2284. [Google Scholar] [CrossRef]
- Ando, T.; Yokoi, F.; Riku, Y.; Akagi, A.; Miyahara, H.; Hasegawa, M.; Katsuno, M.; Yoshida, M.; Iwasaki, Y. The hot cross bun sign in corticobasal degeneration. Neuropathology 2021, 41, 376–380. [Google Scholar] [CrossRef]
- Liu, M.; Ren, H.; Lin, N.; Tan, Y.; Fan, S.; Guan, H. The “hot cross bun sign” in patients with autoimmune cerebellar ataxia: A case report and literature review. Front. Neurol. 2022, 13, 979203. [Google Scholar] [CrossRef]
- Mestre, T.A.; Gupta, A.; Lang, A.E. MRI signs of multiple system atrophy preceding the clinical diagnosis: The case for an imaging-supported probable MSA diagnostic category. J. Neurol. Neurosurg. Psychiatry 2016, 87, 443–444. [Google Scholar] [CrossRef] [PubMed]
- Ghandili, M.; Munakomi, S. Neuroanatomy, Putamen; StatPearls Publishing: Treasure Island, FL, USA, 2024. [Google Scholar]
- Viñas-Guasch, N.; Wu, Y.J. The role of the putamen in language: A meta-analytic connectivity modeling study. Brain Struct. Funct. 2017, 222, 3991–4004. [Google Scholar] [CrossRef]
- Mori, K.; Yagishita, A.; Shimizu, T. Asymmetrical putaminal atrophy in parkinsonism-predominant multiple system atrophy (MSA-P): A case report. Radiol. Case Rep. 2023, 18, 2975–2977. [Google Scholar] [CrossRef]
- Constantinides, V.C.; Souvatzoglou, M.; Paraskevas, G.P.; Chalioti, M.; Stefanis, L.; Kapaki, E. Dopamine transporter SPECT imaging in Parkinson’s disease and atypical Parkinsonism: A study of 137 patients. Neurol. Sci. 2023, 44, 1613–1623. [Google Scholar] [CrossRef]
- Niccolini, F.; Politis, M. A systematic review of lessons learned from PET molecular imaging research in atypical parkinsonism. Eur. J. Nucl. Med. 2016, 43, 2244–2254. [Google Scholar] [CrossRef] [PubMed]
- Shigekiyo, T.; Arawaka, S. Laterality of specific binding ratios on DAT-SPECT for differential diagnosis of degenerative parkinsonian syndromes. Sci. Rep. 2020, 10, 15761. [Google Scholar] [CrossRef] [PubMed]
- Goolla, M.; Cheshire, W.P.; Ross, O.A.; Kondru, N. Diagnosing multiple system atrophy: Current clinical guidance and emerging molecular biomarkers. Front Neurol. 2023, 14, 1210220. [Google Scholar] [CrossRef]
- Pirker, W.; Asenbaum, S.; Bencsits, G.; Prayer, D.; Gerschlager, W.; Deecke, L.; Brücke, T. [123I]β-CIT spect in multiple system atrophy, progressive supranuclear palsy, and corticobasal degeneration. Mov. Disord. 2000, 15, 1158–1167. [Google Scholar] [CrossRef] [PubMed]
- Basso, D.; Saracini, C. Differential involvement of left and right frontoparietal areas in visuospatial planning: An rTMS study. Neuropsychologia 2020, 136, 107260. [Google Scholar] [CrossRef]
- Koyama, M.; Yagishita, A.; Nakata, Y.; Hayashi, M.; Bandoh, M.; Mizutani, T. Imaging of corticobasal degeneration syndrome. Neuroradiology 2007, 49, 905–912. [Google Scholar] [CrossRef]
- Di Stasio, F.; Suppa, A.; Marsili, L.; Upadhyay, N.; Asci, F.; Bologna, M.; Colosimo, C.; Fabbrini, G.; Pantano, P.; Berardelli, A. Corticobasal syndrome: Neuroimaging and neurophysiological advances. Eur. J. Neurol. 2019, 26, 701-e52. [Google Scholar] [CrossRef] [PubMed]
- Crosson, B.; Benefield, H.; Cato, M.A.; Sadek, J.R.; Moore, A.B.; Wierenga, C.E.; Gopinath, K.; Soltysik, D.; Bauer, R.M.; Auerbach, E.J.; et al. Left and right basal ganglia and frontal activity during language generation: Contributions to lexical, semantic, and phonological processes. J. Int. Neuropsychol. Soc. 2003, 9, 1061–1077. [Google Scholar] [CrossRef]
- Uddin, L.Q.; Nomi, J.S.; Hébert-Seropian, B.; Ghaziri, J.; Boucher, O. Structure and Function of the Human Insula. J. Clin. Neurophysiol. 2017, 34, 300–306. [Google Scholar] [CrossRef] [PubMed]
- Seiffert, A.P.; Gómez-Grande, A.; Alonso-Gómez, L.; Méndez-Guerrero, A.; Villarejo-Galende, A.; Gómez, E.J.; Sánchez-González, P. Differences in Striatal Metabolism in [18F]FDG PET in Parkinson’s Disease and Atypical Parkinsonism. Diagnostics 2023, 13, 6. [Google Scholar] [CrossRef]
- Arnone, A.; Allocca, M.; Di Dato, R.; Puccini, G.; Laghai, I.; Rubino, F.; Nerattini, M.; Ramat, S.; Lombardi, G.; Ferrari, C.; et al. FDG PET in the differential diagnosis of degenerative parkinsonian disorders: Usefulness of voxel-based analysis in clinical practice. Neurol. Sci. 2022, 43, 5333–5341. [Google Scholar] [CrossRef] [PubMed]
- Li, J.; Kumar, A.; Långström, B.; Nordberg, A.; Ågren, H. Insight into the Binding of First- and Second-Generation PET Tracers to 4R and 3R/4R Tau Protofibrils. ACS Chem. Neurosci. 2023, 14, 3528–3539. [Google Scholar] [CrossRef]
- Beyer, L.; Meyer-Wilmes, J.; Schönecker, S.; Schnabel, J.; Brendel, E.; Prix, C.; Nübling, G.; Unterrainer, M.; Albert, N.L.; Pogarell, O.; et al. Clinical Routine FDG-PET Imaging of Suspected Progressive Supranuclear Palsy and Corticobasal Degeneration: A Gatekeeper for Subsequent Tau-PET Imaging? Front. Neurol. 2018, 9, 483. [Google Scholar] [CrossRef]
- Alster, P.; Madetko, N.K.; Koziorowski, D.M.; Królicki, L.; Budrewicz, S.; Friedman, A. Accumulation of Tau Protein, Metabolism and Perfusion-Application and Efficacy of Positron Emission Tomography (PET) and Single Photon Emission Computed Tomography (SPECT) Imaging in the Examination of Progressive Supranuclear Palsy (PSP) and Corticobasal Syndrome (CBS). Front. Neurol. 2019, 14, 101. [Google Scholar]
- Szurowska, E.; Teodorczyk, J.; Dziadziuszko, K.; Pieńkowska, J.; Romanowicz, G.; Lass, P. Positron emission tomography in oncology with use of radiotracers alternative to 18F-fluorodeoxyglucose. Oncol. Clin. Pract. 2013, 9, 197–199. [Google Scholar]
- Akdemir, Ü.Ö.; Tokçaer, A.B.; Atay, L.Ö. Dopamine transporter SPECT imaging in Parkinson’s disease and parkinsonian disorders. Turk. J. Med Sci. 2021, 51, 400–410. [Google Scholar] [CrossRef]
- Tai, Y.F.; Ahsan, R.L.; de Yébenes, J.G.; Pavese, N.; Brooks, D.J.; Piccini, P. Characterization of dopaminergic dysfunction in familial progressive supranuclear palsy: An 18F-dopa PET study. J. Neural Transm. 2006, 114, 337–340. [Google Scholar] [CrossRef] [PubMed]
- Nagasawa, H.; Tanji, H.; Nomura, H.; Saito, H.; Itoyama, Y.; Kimura, I.; Tuji, S.; Fujiwara, T.; Iwata, R.; Itoh, M.; et al. PET study of cerebral glucose metabolism and fluorodopa uptake in patients with corticobasal degeneration. J. Neurol. Sci. 1996, 139, 210–217. [Google Scholar] [CrossRef] [PubMed]
- El Ouartassi, A.; Giordana, C.; Schiazza, A.; Chardin, D.; Darcourt, J. [18F]-FDopa positron emission tomography imaging in corticobasal syndrome. Brain Imaging Behav. 2023, 17, 619–627. [Google Scholar] [CrossRef] [PubMed]
- Xian, W.B.; Shi, X.C.; Luo, G.H.; Yi, C.; Zhang, X.S.; Pei, Z. Co-registration Analysis of Fluorodopa and Fluorodeoxyglucose Positron Emission Tomography for Differentiating Multiple System Atrophy Parkinsonism Type from Parkinson’s Disease. Front. Aging Neurosci. 2021, 13, 648531. [Google Scholar] [CrossRef]
- Jellinger, K. Evaluation of Multiple System Atrophy Subtypes with FDG-PET. Ann. Indian Acad. Neurol. 2021, 24, 468. [Google Scholar] [CrossRef] [PubMed]
- Habibi, S.A.H.; Aghavali, S.; Azad, Z.; Amini, E.; Falah, M.; Gholibeigian, Z.; Yazdi, N.; Emamikhah, M.; Rohani, M. Transcranial sonography in neurodegeneration with brain iron accumulation disorders. Clin. Neurol. Neurosurg. 2024, 236, 108074. [Google Scholar] [CrossRef]
- Nowakowska-Kotas, M. Ultrasonografia przezczaszkowa w diagnostyce parkinsonizmu. Pol. Przegląd Neurol. 2015, 11, 51–57. [Google Scholar]
- Alonso-Canovas, A.; Ferrairó, J.I.T.; Martínez-Torres, I.; Moreno, J.L.L.S.; Parees-Moreno, I.; Monreal-Laguillo, E.; Pérez-Torre, P.; Delgado, R.T.; Ribas, G.G.; Bataller, I.S.; et al. Transcranial sonography in atypical parkinsonism: How reliable is it in real clinical practice? A multicentre comprehensive study. Park. Relat. Disord. 2019, 68, 40–45. [Google Scholar] [CrossRef]
- Wen, Y.; Zhou, H.; Xia, M.; Liu, Q.; Quan, H.; Fang, L. Differentiating progressive supranuclear palsy from other movement disorders using transcranial sonography: A systematic review and meta-analysis. Neurol. Sci. 2023, 45, 455–465. [Google Scholar] [CrossRef]
- Ebentheuer, J.; Canelo, M.; Trautmann, E.; Trenkwalder, C. Substantia nigra echogenicity in progressive supranuclear palsy. Mov. Disord. 2010, 25, 773–777. [Google Scholar] [CrossRef]
- Yan, J.H.; Li, K.; Ge, Y.L.; Li, W.; Wang, P.Z.; Jin, H.; Zhang, J.R.; Chen, J.; Wang, F.; Yang, Y.P.; et al. Quantitative Transcranial Sonography Evaluation of Substantia Nigra Hyperechogenicity Is Useful for Predicting Levodopa-Induced Dyskinesia in Parkinson Disease. Ultrasound Med. Biol. 2023, 49, 607–615. [Google Scholar] [CrossRef] [PubMed]
- Koziorowski, D.; Figura, M.; Milanowski, Ł.M.; Szlufik, S.; Alster, P.; Madetko, N.; Friedman, A. Mechanisms of Neurodegeneration in Various Forms of Parkinsonism—Similarities and Differences. Cells 2021, 10, 656. [Google Scholar] [CrossRef] [PubMed]
- Dunalska, A.; Pikul, J.; Schok, K.; Wiejak, K.A.; Alster, P. The Significance of Vascular Pathogenesis in the Examination of Corticobasal Syndrome. Front. Aging Neurosci. 2021, 4, 668614. [Google Scholar] [CrossRef] [PubMed]
- Whitwell, J.L.; Master, A.V.; Avula, R.; Kantarci, K.; Eggers, S.D.; Edmonson, H.A.; Jack, C.R.; Josephs, K.A. Clinical correlates of white matter tract degeneration in progressive supranuclear palsy. Arch. Neurol. 2011, 68, 753–760. [Google Scholar] [CrossRef]
- Saito, Y.; Kamagata, K.; Wijeratne, P.A.; Andica, C.; Uchida, W.; Takabayashi, K.; Fujita, S.; Akashi, T.; Wada, A.; Shimoji, K.; et al. Temporal Progression Patterns of Brain Atrophy in Corticobasal Syndrome and Progressive Supranuclear Palsy Revealed by Subtype and Stage Inference (SuStaIn). Front. Neurol. 2022, 13, 814768. [Google Scholar] [CrossRef]
- Monzio Compagnoni, G.; Di Fonzo, A. Understanding the pathogenesis of multiple system atrophy: State of the art and future perspectives. Acta Neuropathol. Commun. 2019, 7, 113. [Google Scholar] [CrossRef] [PubMed]
- Goh, Y.Y.; Saunders, E.; Pavey, S.; Rushton, E.; Quinn, N.; Houlden, H.; Chelban, V. Multiple system atrophy. Pract Neurol. 2023, 23, 208–221. [Google Scholar] [CrossRef]
- Aslam, S.; Manfredsson, F.; Stokes, A.; Shill, H. "Advanced" Parkinson’s disease: A review. Park. Relat. Disord. 2024, 123, 106065. [Google Scholar] [CrossRef]

| Imaging | Often Occuring Disease | Finding | Morphology | Symmetry | Specificity | Sensivity |
|---|---|---|---|---|---|---|
| MRI | PSP-RS | Hummingbird sign/penguin sign | A midbrain tegmental atrophy without pontine atrophy | Unpaired structure | 99.5% | 57% |
| PSP-RS | Morning glory sign | An increased lateral concavity of the midbrain tegmentum | Unpaired structure | 97% | 37% | |
| PSP | Basal ganglia, brain stem and frontal cortex atrophy | Symmetric | ||||
| MSA | Hot cross bun sign | A linear T2-hyperintensity extending across the rostral pons | Symmetric | 98.5% | 50% | |
| MSA | Putamina rim sign | A near-total loss of neurons in the putamen | Asymmetric | 90% | 72% | |
| CBS | Basal ganglia, brain stem and frontal cortex atrophy | Asymmetric | ||||
| SPECT | PSP, MSA-P, CBS | Basal ganglia, brain stem and frontal cortex | Hypoperfusion | Asymmetric (less than in PD) | ||
| PET | PSP | Pimple sign | A reduced metabolism in the midbrain | Unpaired structure | ||
| PSP | Frontal cortices, the anterior cingulate gyrus, and the midbrain | A reduced glucose metabolism | Symmetric or asymmetric | |||
| CBS | Disseminated: Parieto-frontal thalamus, basal ganglia, middle cingulate, parietal lobe | A reduced glucose metabolism | Asymmetric | |||
| MSA-P | Striatum | A reduced glucose metabolism | Symmetric or asymmetric | 95% | ||
| MSA-C | Cerebellum and brainstem | A reduced glucose metabolism | Asymmetric | 95% | ||
| Undifferentiated (mixed) MSA | Cerebellum, brainstem, stratium, fronto-parietal regions | A reduced glucose metabolism | Asymmetric | 95% | ||
| TCS | PSP and MSA | SN | Hyperechogenicity | Symmetric | PSP (86%) PSP-RS (3.8%) | |
| PSP and MSA | LN | Hyperechogenicity | Asymmetric | PSP—70% | ||
| CBD | SN | Hyperechogenicity | Symmetric | |||
| CBD | LN | Hyperechogenicity | Symmetric or asymmetric |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chunowski, P.; Madetko-Alster, N.; Alster, P. Asymmetry in Atypical Parkinsonian Syndromes—A Review. J. Clin. Med. 2024, 13, 5798. https://doi.org/10.3390/jcm13195798
Chunowski P, Madetko-Alster N, Alster P. Asymmetry in Atypical Parkinsonian Syndromes—A Review. Journal of Clinical Medicine. 2024; 13(19):5798. https://doi.org/10.3390/jcm13195798
Chicago/Turabian StyleChunowski, Patryk, Natalia Madetko-Alster, and Piotr Alster. 2024. "Asymmetry in Atypical Parkinsonian Syndromes—A Review" Journal of Clinical Medicine 13, no. 19: 5798. https://doi.org/10.3390/jcm13195798






