Monoclonal Antibodies for the Treatment of Ocular Diseases
Abstract
1. Introduction
2. Ocular Diseases
2.1. Age-Related Macular Degeneration
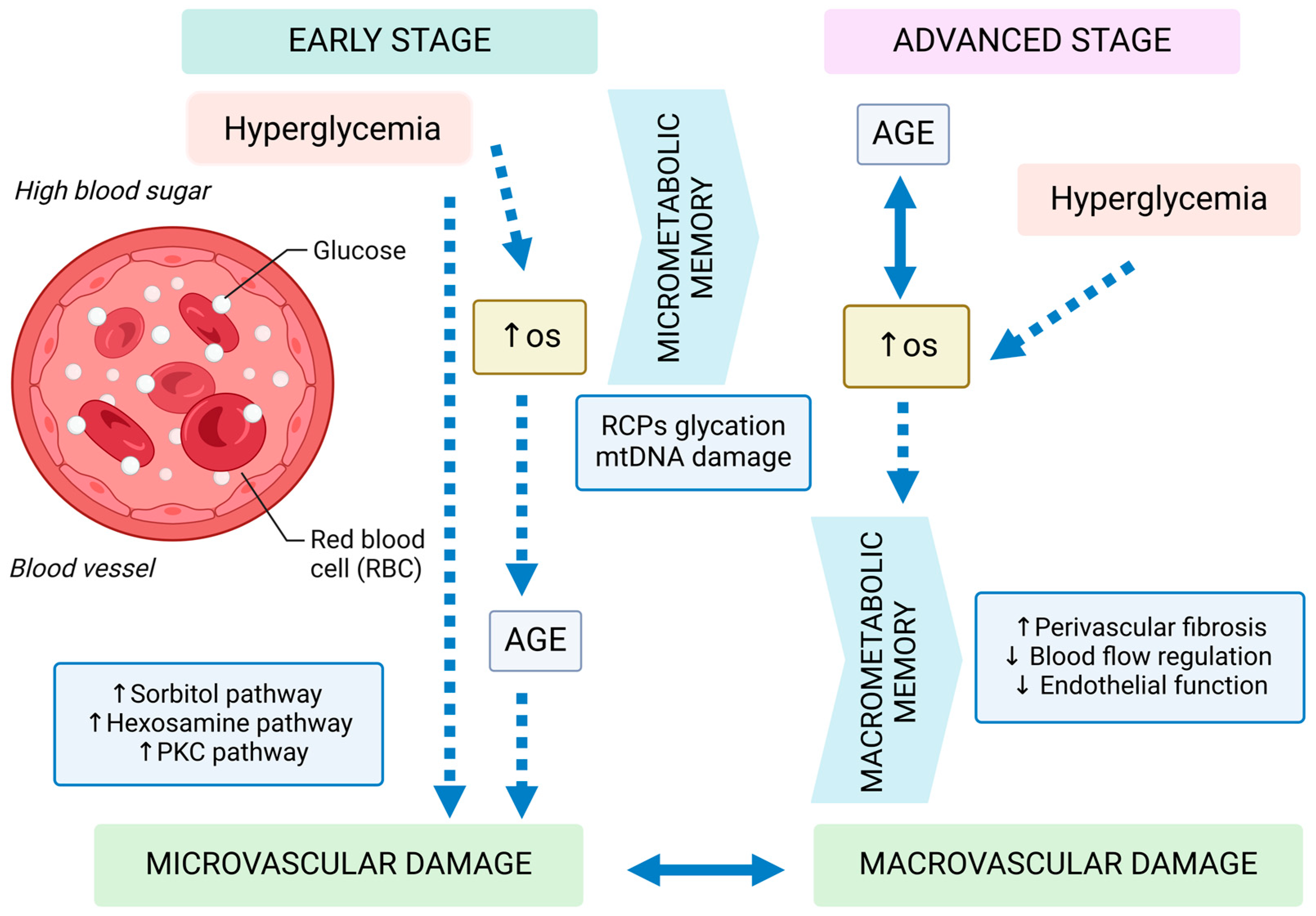
2.2. Diabetic Retinopathy
2.3. Uveitis
2.4. COVID-19
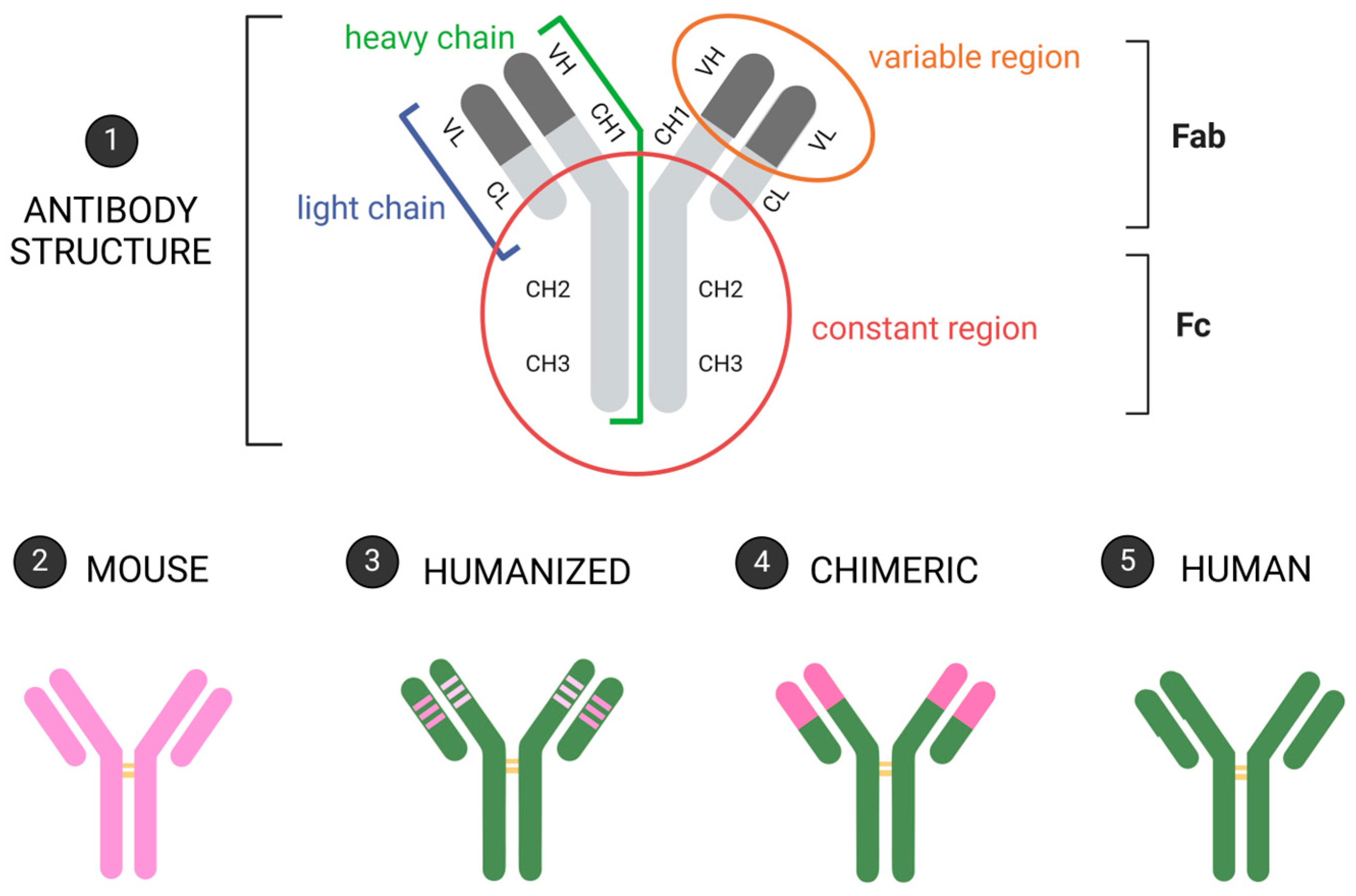
3. Monoclonal Antibodies and Their Application in Ocular Diseases
3.1. Bevacizumab
3.2. Ranibizumab
3.3. Adalimumab
3.4. Infliximab
3.5. Certolizumab
3.6. Bamlanivimab
3.7. Casirivimab
3.8. Imdevimab
3.9. Brolucizumab
3.10. Faricimab
3.11. Aflibercept
3.12. Etanercept
4. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Breedveld, F. Therapeutic monoclonal antibodies. Lancet 2000, 355, 735–740. [Google Scholar] [CrossRef] [PubMed]
- Bayer, V. An overview of monoclonal antibodies. Semin. Oncol. Nurs. 2019, 35, 150927. [Google Scholar] [CrossRef]
- Ecker, D.M.; Jones, S.D.; Levine, H.L. The therapeutic monoclonal antibody market. mAbs 2015, 7, 9–14. [Google Scholar] [CrossRef] [PubMed]
- Rodríguez-Nava, C.; Ortuño-Pineda, C.; Illades-Aguiar, B.; Flores-Alfaro, E.; Leyva-Vázquez, M.A.; Parra-Rojas, I.; del Moral-Hernández, O.; Vences-Velázquez, A.; Cortés-Sarabia, K.; Alarcón-Romero, L.d.C. Mechanisms of action and limitations of monoclonal antibodies and single chain fragment variable (scFv) in the treatment of cancer. Biomedicines 2023, 11, 1610. [Google Scholar] [CrossRef] [PubMed]
- McMaster, P.D.; Hudack, S.S. The formation of agglutinins with lymph nodes. J. Exp. Med. 1935, 61, 783–805. [Google Scholar] [CrossRef] [PubMed]
- Singh, S.; Tank, N.K.; Dwiwedi, P.; Charan, J.; Kaur, R.; Sidhu, P.; Chugh, V.K. Monoclonal antibodies: A review. Curr. Clin. Pharmacol. 2018, 13, 85–99. [Google Scholar] [CrossRef]
- Rodrigues, E.B.; Farah, M.E.; Maia, M.; Penha, F.M.; Regatieri, C.; Melo, G.B.; Pinheiro, M.M.; Zanetti, C.R. Therapeutic monoclonal antibodies in ophthalmology. Prog. Retin. Eye Res. 2009, 28, 117–144. [Google Scholar] [CrossRef]
- Shibuya, M. Vascular Endothelial Growth Factor (VEGF) and Its Receptor (VEGFR) Signaling in Angiogenesis: A Crucial Target for Anti- and Pro-Angiogenic Therapies. Genes Cancer 2011, 2, 1097–1105. [Google Scholar] [CrossRef]
- Penn, J.S.; Madan, A.; Caldwell, R.B.; Bartoli, M.; Caldwell, R.W.; Hartnett, M.E. Vascular endothelial growth factor in eye disease. Prog. Retin. Eye Res. 2008, 27, 331–371. [Google Scholar] [CrossRef]
- Lad, E.M.; Finger, R.P.; Guymer, R. Biomarkers for the Progression of Intermediate Age-Related Macular Degeneration. Ophthalmol. Ther. 2023, 12, 2917–2941. [Google Scholar] [CrossRef]
- Thomas, C.J.; Mirza, R.G.; Gill, M.K. Age-Related Macular Degeneration. Med. Clin. N. Am. 2021, 105, 473–491. [Google Scholar] [CrossRef] [PubMed]
- Stahl, A. The Diagnosis and Treatment of Age-Related Macular Degeneration. Dtsch. Arztebl. Int. 2020, 117, 513–520. [Google Scholar] [CrossRef] [PubMed]
- Stone, E.M. Macular degeneration. Annu. Rev. Med. 2007, 58, 477–490. [Google Scholar] [CrossRef] [PubMed]
- Kikushima, W.; Sakurada, Y.; Fukuda, Y.; Matsubara, M.; Kotoda, Y.; Sugiyama, A.; Kashiwagi, K. A Treat-and-Extend Regimen of Intravitreal Brolucizumab for Exudative Age-Related Macular Degeneration Refractory to Aflibercept: A 12-Month Result. Pharmaceuticals 2023, 16, 562. [Google Scholar] [CrossRef]
- Coleman, H.R.; Chan, C.-C.; Ferris, F.L.; Chew, E.Y. Age-related macular degeneration. Lancet 2008, 372, 1835–1845. [Google Scholar] [CrossRef]
- Lim, L.S.; Mitchell, P.; Seddon, J.M.; Holz, F.G.; Wong, T.Y. Age-related macular degeneration. Lancet 2012, 379, 1728–1738. [Google Scholar] [CrossRef]
- Domalpally, A.; Xing, B.; Pak, J.W.; Agrón, E.; Ferris, F.L., 3rd; Clemons, T.E.; Chew, E.Y. Extramacular Drusen and Progression of Age-Related Macular Degeneration: Age Related Eye Disease Study 2 Report 30. Ophthalmol. Retin. 2023, 7, 111–117. [Google Scholar] [CrossRef]
- Flores, R.; Carneiro, Â.; Vieira, M.; Tenreiro, S.; Seabra, M.C. Age-Related Macular Degeneration: Pathophysiology, Management, and Future Perspectives. Ophthalmologica 2021, 244, 495–511. [Google Scholar] [CrossRef]
- Leitch, I.M.; Gerometta, M.; Eichenbaum, D.; Finger, R.P.; Steinle, N.C.; Baldwin, M.E. Vascular Endothelial Growth Factor C and D Signaling Pathways as Potential Targets for the Treatment of Neovascular Age-Related Macular Degeneration: A Narrative Review. Ophthalmol. Ther. 2024, 13, 1857–1875. [Google Scholar] [CrossRef]
- Rosenfeld, P.J.; Rich, R.M.; Lalwani, G.A. Ranibizumab: Phase III clinical trial results. Ophthalmol. Clin. N. Am. 2006, 19, 361–372. [Google Scholar] [CrossRef]
- Wang, W.; Lo, A.C. Diabetic retinopathy: Pathophysiology and treatments. Int. J. Mol. Sci. 2018, 19, 1816. [Google Scholar] [CrossRef] [PubMed]
- Fong, D.S.; Aiello, L.P.; Ferris, F.L., III; Klein, R. Diabetic retinopathy. Diabetes Care 2004, 27, 2540–2553. [Google Scholar] [CrossRef] [PubMed]
- Porta, M.; Bandello, F. Diabetic retinopathy: A clinical update. Diabetologia 2002, 45, 1617–1634. [Google Scholar] [CrossRef] [PubMed]
- Ferris, F.L.; Davis, M.D.; Aiello, L.M. Treatment of diabetic retinopathy. N. Engl. J. Med. 1999, 341, 667–678. [Google Scholar] [CrossRef]
- Akinsoji, E.; Goldhardt, R.; Galor, A. A Glimpse into Uveitis in the Aging Eye: Pathophysiology, Clinical Presentation and Treatment Considerations. Drugs Aging 2018, 35, 399–408. [Google Scholar] [CrossRef]
- Cuartero-Martínez, A.; García-Otero, X.; Codesido, J.; Gómez-Lado, N.; Mateos, J.; Bravo, S.B.; Rodríguez-Fernández, C.A.; González-Barcia, M.; Aguiar, P.; Ortega-Hortas, M.; et al. Preclinical characterization of endotoxin-induced uveitis models using OCT, PET/CT and proteomics. Int. J. Pharm. 2024, 662, 124516. [Google Scholar] [CrossRef]
- Muñoz-Fernández, S.; Martín-Mola, E. Uveitis. Best Pract. Res. Clin. Rheumatol. 2006, 20, 487–505. [Google Scholar] [CrossRef]
- Chang, J.H.-M.; Wakefield, D. Uveitis: A global perspective. Ocul. Immunol. Inflamm. 2002, 10, 263–279. [Google Scholar] [CrossRef]
- de Vos, A.F.; van Haren, M.A.; Verhagen, C.; Hoekzema, R.; Kijlstra, A. Kinetics of intraocular tumor necrosis factor and interleukin-6 in endotoxin-induced uveitis in the rat. Investig. Ophthalmol. Vis. Sci. 1994, 35, 1100–1106. Available online: https://pubmed.ncbi.nlm.nih.gov/8125720/ (accessed on 8 July 2024).
- Santos Lacomba, M.; Marcos Martín, C.; Gallardo Galera, J.M.; Gómez Vidal, M.A.; Collantes Estévez, E.; Ramírez Chamond, R.; Omar, M. Aqueous humor and serum tumor necrosis factor-alpha in clinical uveitis. Ophthalmic Res. 2001, 33, 251–255. [Google Scholar] [CrossRef]
- Santos, M.F.C.; Mirada, G.S.; do Couto, J.O.; de Oliveira Costa, G.; Rangel Rosa, A.C.; Gambeta Borges, C.H.; Crevelin, E.J.; de Araujo, L.S.; Bastos, J.K.; Veneziani, R.C.S.; et al. A validated ultra-performance liquid chromatography with tandem mass spectrometry method for the quantification of Brazilian green propolis main compounds. Nat. Prod. Res. 2024, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Leung, E.H.; Fan, J.; Flynn, H.W., Jr.; Albini, T.A. Ocular and Systemic Complications of COVID-19: Impact on Patients and Healthcare. Clin. Ophthalmol. 2022, 16, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Siemieniuk, R.A.; Bartoszko, J.J.; Díaz Martinez, J.P.; Kum, E.; Qasim, A.; Zeraatkar, D.; Izcovich, A.; Mangala, S.; Ge, L.; Han, M.A.; et al. Antibody and cellular therapies for treatment of COVID-19: A living systematic review and network meta-analysis. BMJ 2021, 374, n2231. [Google Scholar] [CrossRef] [PubMed]
- Braghiroli, M.I.; Sabbaga, J.; Hoff, P.M. Bevacizumab: Overview of the literature. Expert Rev. Anticancer Ther. 2012, 12, 567–580. [Google Scholar] [CrossRef] [PubMed]
- Kazazi-Hyseni, F.; Beijnen, J.H.; Schellens, J.H. Bevacizumab. Oncologist 2010, 15, 819–825. [Google Scholar] [CrossRef]
- Singh, R.P.; Avery, R.L.; Barakat, M.R.; Kim, J.E.; Kiss, S. Evidence-Based Use of Bevacizumab in the Management of Neovascular Age-Related Macular Degeneration. Ophthalmic Surg. Lasers Imaging Retin. 2024, 55, 156–162. [Google Scholar] [CrossRef]
- Estarreja, J.; Mendes, P.; Silva, C.; Camacho, P.; Mateus, V. Off-Label Use of Bevacizumab in Patients Diagnosed with Age-Related Macular Degeneration: A Systematic Review and Meta-Analysis. Pharmaceuticals 2024, 17, 1000. [Google Scholar] [CrossRef]
- Gomez-Lumbreras, A.; Ghule, P.; Panchal, R.; Giannouchos, T.; Lockhart, C.M.; Brixner, D. Real-world evidence in the use of Bevacizumab in age-related macular degeneration (ArMD): A scoping review. Int. Ophthalmol. 2023, 43, 4527–4539. [Google Scholar] [CrossRef]
- Gumus, G.; Berhuni, M.; Ozturkmen, C. The short-term effects of intravitreal bevacizumab injection on intraocular pressure, cornea, iridocorneal angle, and anterior chamber. Ther. Adv. Ophthalmol. 2022, 14, 25158414221133772. [Google Scholar] [CrossRef]
- Blick, S.K.; Keating, G.M.; Wagstaff, A.J. Ranibizumab. Drugs 2007, 67, 1199–1206. [Google Scholar] [CrossRef]
- Triantafylla, M.; Massa, H.F.; Dardabounis, D.; Gatzioufas, Z.; Kozobolis, V.; Ioannakis, K.; Perente, I.; Panos, G.D. Ranibizumab for the treatment of degenerative ocular conditions. Clin. Ophthalmol. 2014, 8, 1187–1198. [Google Scholar] [CrossRef] [PubMed]
- Pershing, S.; Talwar, N.; Armenti, S.T.; Grubbs, J., Jr.; Rosenthal, J.M.; Dedania, V.S.; Stein, J.D. Use of Bevacizumab and Ranibizumab for Wet Age-Related Macular Degeneration: Influence of CATT Results and Introduction of Aflibercept. Am. J. Ophthalmol. 2019, 207, 385–394. [Google Scholar] [CrossRef] [PubMed]
- Parravano, M.; Costanzo, E.; Scondotto, G.; Trifirò, G.; Virgili, G. Anti-VEGF and Other Novel Therapies for Neovascular Age-Related Macular Degeneration: An Update. BioDrugs 2021, 35, 673–692. [Google Scholar] [CrossRef] [PubMed]
- Scheinfeld, N. Adalimumab: A review of side effects. Expert Opin. Drug Saf. 2005, 4, 637–641. [Google Scholar] [CrossRef]
- Rudwaleit, M.; Rødevand, E.; Holck, P.; Vanhoof, J.; Kron, M.; Kary, S.; Kupper, H. Adalimumab effectively reduces the rate of anterior uveitis flares in patients with active ankylosing spondylitis: Results of a prospective open-label study. Ann. Rheum. Dis. 2009, 68, 696–701. [Google Scholar] [CrossRef]
- Takase, K.; Ohno, S.; Ideguchi, H.; Uchio, E.; Takeno, M.; Ishigatsubo, Y. Successful switching to adalimumab in an infliximab-allergic patient with severe Behçet disease-related uveitis. Rheumatol. Int. 2011, 31, 243–245. [Google Scholar] [CrossRef]
- Diaz-Llopis, M.; García-Delpech, S.; Salom, D.; Udaondo, P.; Hernández-Garfella, M.; Bosch-Morell, F.; Quijada, A.; Romero, F.J. Adalimumab therapy for refractory uveitis: A pilot study. J. Ocul. Pharmacol. Ther. 2008, 24, 351–361. [Google Scholar] [CrossRef]
- Winterfield, L.S.; Menter, A. Infliximab. Dermatol. Ther. 2004, 17, 409–426. [Google Scholar] [CrossRef]
- Miraldi Utz, V.; Bulas, S.; Lopper, S.; Fenchel, M.; Sa, T.; Mehta, M.; Ash, D.; Lovell, D.J.; Kaufman, A.H. Effectiveness of long-term infliximab use and impact of treatment adherence on disease control in refractory, non-infectious pediatric uveitis. Pediatr. Rheumatol. 2019, 17, 79. [Google Scholar] [CrossRef]
- Cordero-Coma, M.; Sobrin, L. Anti-tumor necrosis factor-α therapy in uveitis. Surv. Ophthalmol. 2015, 60, 575–589. [Google Scholar] [CrossRef]
- Deitch, I.; Amer, R.; Tomkins-Netzer, O.; Habot-Wilner, Z.; Friling, R.; Neumann, R.; Kramer, M. The effect of anti-tumor necrosis factor alpha agents on the outcome in pediatric uveitis of diverse etiologies. Graefe’s Arch. Clin. Exp. Ophthalmol. 2018, 256, 801–808. [Google Scholar] [CrossRef] [PubMed]
- Maleki, A.; Sahawneh, H.F.; Ma, L.; Meese, H.; He, Y.; Foster, C.S. Infliximab therapy with noninfectious intermediate uveitis resistant to conventional immunomodulatory therapy. Retina 2017, 37, 836–843. [Google Scholar] [CrossRef] [PubMed]
- Cunningham, E.T., Jr. Exogenous factors influencing endogenous inflammation: What can patients do to improve control of their own uveitis? Br. J. Ophthalmol. 2010, 94, 813–814. [Google Scholar] [CrossRef] [PubMed]
- Dolz-Marco, R.; Gallego-Pinazo, R.; Díaz-Llopis, M.; Cunningham, E.T., Jr.; Arévalo, J.F. Noninfectious uveitis: Strategies to optimize treatment compliance and adherence. Clin. Ophthalmol. 2015, 9, 1477–1481. [Google Scholar] [CrossRef]
- Mushtaq, B.; Saeed, T.; Situnayake, R.D.; Murray, P.I. Adalimumab for sight-threatening uveitis in Behçet’s disease. Eye 2007, 21, 824–825. [Google Scholar] [CrossRef]
- Llorenç, V.; Mesquida, M.; Sainz de la Maza, M.; Blanco, R.; Calvo, V.; Maíz, O.; Blanco, A.; de Dios-Jiménez de Aberásturi, J.R.; Adán, A. Certolizumab Pegol, a New Anti-TNF-α in the Armamentarium against Ocular Inflammation. Ocul. Immunol. Inflamm. 2016, 24, 167–172. [Google Scholar] [CrossRef]
- Lee, J.U.; Shin, W.; Son, J.Y.; Yoo, K.Y.; Heo, Y.S. Molecular Basis for the Neutralization of Tumor Necrosis Factor α by Certolizumab Pegol in the Treatment of Inflammatory Autoimmune Diseases. Int. J. Mol. Sci. 2017, 18, 228. [Google Scholar] [CrossRef]
- Frías, E.D.; González, J.F.D. Certolizumab pegol. Reumatol. Clin. 2011, 6 (Suppl. 3), 7–11. [Google Scholar] [CrossRef]
- Moisseiev, E.; Shulman, S. Certolizumab-induced uveitis: A case report and review of the literature. Case Rep. Ophthalmol. 2014, 5, 54–59. [Google Scholar] [CrossRef]
- Sharon, Y.; Chu, D.S. Certolizumab pegol—Tumor necrosis factor inhibitor for refractory uveitis. Am. J. Ophthalmol. Case Rep. 2020, 18, 100633. [Google Scholar] [CrossRef]
- Benschop, R.J.; Tuttle, J.L.; Zhang, L.; Poorbaugh, J.; Kallewaard, N.L.; Vaillancourt, P.; Crisp, M.; Trinh, T.N.V.; Freitas, J.J.; Beasley, S.; et al. The anti-SARS-CoV-2 monoclonal antibody bamlanivimab minimally affects the endogenous immune response to COVID-19 vaccination. Sci. Transl. Med. 2022, 14, eabn3041. [Google Scholar] [CrossRef] [PubMed]
- Gottlieb, R.L.; Nirula, A.; Chen, P.; Boscia, J.; Heller, B.; Morris, J.; Huhn, G.; Cardona, J.; Mocherla, B.; Stosor, V.; et al. Effect of Bamlanivimab as Monotherapy or in Combination with Etesevimab on Viral Load in Patients With Mild to Moderate COVID-19: A Randomized Clinical Trial. JAMA 2021, 325, 632–644. [Google Scholar] [CrossRef] [PubMed]
- Deeks, E.D. Casirivimab/imdevimab: First approval. Drugs 2021, 81, 2047–2055. [Google Scholar] [CrossRef] [PubMed]
- Vellas, C.; Del Bello, A.; Gaube, G.; Tremeaux, P.; Jeanne, N.; Ranger, N.; Martin-Blondel, G.; Delobel, P.; Kamar, N.; Izopet, J. Impact of Casirivimab-Imdevimab on Severe Acute Respiratory Syndrome Coronavirus 2 Delta Variant Nasopharyngeal Virus Load and Spike Quasispecies. Open Forum Infect. Dis. 2022, 9, ofac093. [Google Scholar] [CrossRef]
- Hansen, J.; Baum, A.; Pascal, K.E.; Russo, V.; Giordano, S.; Wloga, E.; Fulton, B.O.; Yan, Y.; Koon, K.; Patel, K.; et al. Studies in humanized mice and convalescent humans yield a SARS-CoV-2 antibody cocktail. Science 2020, 369, 1010–1014. [Google Scholar] [CrossRef]
- Baumal, C.R.; Bodaghi, B.; Singer, M.; Tanzer, D.J.; Seres, A.; Joshi, M.R.; Feltgen, N.; Gale, R. Expert Opinion on Management of Intraocular Inflammation, Retinal Vasculitis, and Vascular Occlusion after Brolucizumab Treatment. Ophthalmol. Retin. 2021, 5, 519–527. [Google Scholar] [CrossRef]
- Dugel, P.U.; Singh, R.P.; Koh, A.; Ogura, Y.; Weissgerber, G.; Gedif, K.; Jaffe, G.J.; Tadayoni, R.; Schmidt-Erfurth, U.; Holz, F.G. HAWK and HARRIER: Ninety-Six-Week Outcomes from the Phase 3 Trials of Brolucizumab for Neovascular Age-Related Macular Degeneration. Ophthalmology 2021, 128, 89–99. [Google Scholar] [CrossRef]
- Nguyen, H.V.; Li, A.S.; Silva, A.R.; Leng, T. Ocular adverse events following intravitreal brolucizumab for neovascular age-related macular degeneration at a single tertiary care center. Eur. J. Ophthalmol. 2022, 32, 2747–2751. [Google Scholar] [CrossRef]
- Abu Serhan, H.; Taha, M.J.J.; Abuawwad, M.T.; Abdelaal, A.; Irshaidat, S.; Abu Serhan, L.; Abu Salim, Q.F.; Awamleh, N.; Abdelazeem, B.; Elnahry, A.G. Safety and Efficacy of Brolucizumab in the Treatment of Diabetic Macular Edema and Diabetic Retinopathy: A Systematic Review and Meta-Analysis. Semin. Ophthalmol. 2024, 39, 251–260. [Google Scholar] [CrossRef]
- Brown, D.M.; Emanuelli, A.; Bandello, F.; Barranco, J.J.E.; Figueira, J.; Souied, E.; Wolf, S.; Gupta, V.; Ngah, N.F.; Liew, G.; et al. KESTREL and KITE: 52-Week Results From Two Phase III Pivotal Trials of Brolucizumab for Diabetic Macular Edema. Am. J. Ophthalmol. 2022, 238, 157–172. [Google Scholar] [CrossRef]
- Hirano, T.; Kumazaki, A.; Tomihara, R.; Ito, S.; Hoshiyama, K.; Murata, T. Evaluating initial responses to brolucizumab in patients undergoing conventional anti-VEGF therapy for diabetic macular edema: A retrospective, single-center, observational study. Sci. Rep. 2023, 13, 10901. [Google Scholar] [CrossRef]
- Kuo, B.L.; Singh, R.P. Brolucizumab for the treatment of diabetic macular edema. Curr. Opin. Ophthalmol. 2022, 33, 167–173. [Google Scholar] [CrossRef] [PubMed]
- Singh, R.P.; Barakat, M.R.; Ip, M.S.; Wykoff, C.C.; Eichenbaum, D.A.; Joshi, S.; Warrow, D.; Sheth, V.S.; Stefanickova, J.; Kim, Y.S.; et al. Efficacy and Safety of Brolucizumab for Diabetic Macular Edema: The KINGFISHER Randomized Clinical Trial. JAMA Ophthalmol. 2023, 141, 1152–1160. [Google Scholar] [CrossRef] [PubMed]
- Ferro Desideri, L.; Traverso, C.E.; Nicolò, M.; Munk, M.R. Faricimab for the treatment of diabetic macular edema and neovascular age-related macular degeneration. Pharmaceutics 2023, 15, 1413. [Google Scholar] [CrossRef] [PubMed]
- Shimura, M.; Kitano, S.; Ogata, N.; Mitamura, Y.; Oh, H.; Ochi, H.; Ohsawa, S.; Hirakata, A.; Bolz, M.; Findl, O.; et al. Efficacy, durability, and safety of faricimab with extended dosing up to every 16 weeks in Japanese patients with diabetic macular edema: 1-year results from the Japan subgroup of the phase 3 YOSEMITE trial. Jpn. J. Ophthalmol. 2023, 67, 264–279. [Google Scholar] [CrossRef]
- Agostini, H.; Abreu, F.; Baumal, C.R.; Chang, D.S.; Csaky, K.G.; Demetriades, A.M.; Kodjikian, L.; Lim, J.I.; Margaron, P.; Monés, J.M.; et al. Faricimab for neovascular age-related macular degeneration and diabetic macular edema: From preclinical studies to phase 3 outcomes. Graefe’s Arch. Clin. Exp. Ophthalmol. 2024. [Google Scholar] [CrossRef]
- Takahashi, H.; Inoda, S.; Takahashi, H.; Takahashi, R.; Hashimoto, Y.; Yoshida, H.; Kawashima, H.; Yanagi, Y. One-year visual and anatomical outcomes of intravitreal faricimab injection for neovascular age-related macular degeneration after prior brolucizumab treatment. Sci. Rep. 2024, 14, 9087. [Google Scholar] [CrossRef]
- Khanani, A.M.; Guymer, R.H.; Basu, K.; Boston, H.; Heier, J.S.; Korobelnik, J.F.; Kotecha, A.; Lin, H.; Silverman, D.; Swaminathan, B.; et al. TENAYA and LUCERNE: Rationale and Design for the Phase 3 Clinical Trials of Faricimab for Neovascular Age-Related Macular Degeneration. Ophthalmol. Sci. 2021, 1, 100076. [Google Scholar] [CrossRef]
- Heier, J.S.; Khanani, A.M.; Quezada Ruiz, C.; Basu, K.; Ferrone, P.J.; Brittain, C.; Figueroa, M.S.; Lin, H.; Holz, F.G.; Patel, V.; et al. Efficacy, durability, and safety of intravitreal faricimab up to every 16 weeks for neovascular age-related macular degeneration (TENAYA and LUCERNE): Two randomised, double-masked, phase 3, non-inferiority trials. Lancet 2022, 399, 729–740. [Google Scholar] [CrossRef]
- Śpiewak, D.; Drzyzga, Ł.; Dorecka, M.; Wyględowska-Promieńska, D. Summary of the Therapeutic Options for Patients with Dry and Neovascular AMD. J. Clin. Med. 2024, 13, 4227. [Google Scholar] [CrossRef]
- DeCroos, F.C.; Reed, D.; Adam, M.K.; Salz, D.; Gupta, O.P.; Ho, A.C.; Regillo, C.D. Treat-and-Extend Therapy Using Aflibercept for Neovascular Age-related Macular Degeneration: A Prospective Clinical Trial. Am. J. Ophthalmol. 2017, 180, 142–150. [Google Scholar] [CrossRef] [PubMed]
- Lanzetta, P.; Korobelnik, J.F.; Heier, J.S.; Leal, S.; Holz, F.G.; Clark, W.L.; Eichenbaum, D.; Iida, T.; Xiaodong, S.; Berliner, A.J.; et al. Intravitreal aflibercept 8 mg in neovascular age-related macular degeneration (PULSAR): 48-week results from a randomised, double-masked, non-inferiority, phase 3 trial. Lancet 2024, 403, 1141–1152. [Google Scholar] [CrossRef] [PubMed]
- Adams, B.S.; Sorhaitz, W.; Stringham, J. Aflibercept. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2023. [Google Scholar]
- de Oliveira Dias, J.R.; Badaró, E.; Novais, E.A.; Colicchio, D.; Chiarantin, G.M.; Matioli, M.M.; Verna, C.; Penha, F.M.; Barros, N.M.; Meyer, C.H.; et al. Preclinical investigations of intravitreal ziv-aflibercept. Ophthalmic Surg. Lasers Imaging Retin. 2014, 45, 577–584. [Google Scholar] [CrossRef] [PubMed]
- Iyer, P.G.; Albini, T.A. Drug-related adverse effects of antivascular endothelial growth factor agents. Curr. Opin. Ophthalmol. 2021, 32, 191–197. [Google Scholar] [CrossRef]
- Avunduk, M.C.; Avunduk, A.M.; Oztekin, E.; Baltaci, A.K.; Ozyazgan, Y.; Mogolkoc, R. Etanercept treatment in the endotoxin-induced uveitis of rats. Exp. Eye Res. 2004, 79, 357–365. [Google Scholar] [CrossRef]
- Lim, L.L.; Fraunfelder, F.W.; Rosenbaum, J.T. Do tumor necrosis factor inhibitors cause uveitis? A registry-based study. Arthritis Rheum. 2007, 56, 3248–3252. [Google Scholar] [CrossRef]
- García-Quintanilla, L.; Almuiña-Varela, P.; Maroñas, O.; Gil-Rodriguez, A.; Rodríguez-Cid, M.J.; Gil-Martinez, M.; Abraldes, M.J.; Gómez-Ulla de Irazazabal, F.; González-Barcia, M.; Mondelo-Garcia, C.; et al. Influence of Genetic Polymorphisms on the Short-Term Response to Ranibizumab in Patients With Neovascular Age-Related Macular Degeneration. Investig. Ophthalmol. Vis. Sci. 2023, 64, 34. [Google Scholar] [CrossRef]
- Ferro Desideri, L.; Traverso, C.E.; Nicolò, M. Brolucizumab: A novel anti-VEGF humanized single-chain antibody fragment for treating w-AMD. Expert Opin. Biol. Ther. 2021, 21, 553–561. [Google Scholar] [CrossRef]
- Markham, A. Brolucizumab: First Approval. Drugs 2019, 79, 1997–2000. [Google Scholar] [CrossRef]
- Shepard, H.M.; Phillips, G.L.; Thanos, C.D.; Feldmann, M. Developments in therapy with monoclonal antibodies and related proteins. Clin. Med. 2017, 17, 220–232. [Google Scholar] [CrossRef]
- Tamiya, R.; Hata, M.; Tanaka, A.; Tsuchikawa, M.; Ueda-Arakawa, N.; Tamura, H.; Miyata, M.; Takahashi, A.; Kido, A.; Muraoka, Y.; et al. Therapeutic effects of faricimab on aflibercept-refractory age-related macular degeneration. Sci. Rep. 2023, 13, 21128. [Google Scholar] [CrossRef] [PubMed]
- Jaggi, D.; Nagamany, T.; Ebneter, A.; Munk, M.; Wolf, S.; Zinkernagel, M. Aflibercept for age-related macular degeneration: 4-year outcomes of a ‘treat-and-extend’ regimen with exit-strategy. Br. J. Ophthalmol. 2022, 106, 246–250. [Google Scholar] [CrossRef] [PubMed]
- Cheng, S.; Zhang, S.; Huang, M.; Liu, Y.; Zou, X.; Chen, X.; Zhang, Z. Treatment of neovascular age-related macular degeneration with anti-vascular endothelial growth factor drugs: Progress from mechanisms to clinical applications. Front. Med. 2024, 11, 1411278. [Google Scholar] [CrossRef] [PubMed]
- Quah, N.Q.X.; Javed, K.; Arbi, L.; Hanumunthadu, D. Real-World Outcomes of Faricimab Treatment for Neovascular Age-Related Macular Degeneration and Diabetic Macular Edema. Clin. Ophthalmol. 2024, 18, 1479–1490. [Google Scholar] [CrossRef]
- Schwartzman, S. Advancements in the management of uveitis. Best Pract. Res. Clin. Rheumatol. 2016, 30, 304–315. [Google Scholar] [CrossRef]
- Trivedi, A.; Katelaris, C. The use of biologic agents in the management of uveitis. Intern. Med. J. 2019, 49, 1352–1363. [Google Scholar] [CrossRef]
- Scott, I.U.; VanVeldhuisen, P.C.; Ip, M.S.; Blodi, B.A.; Oden, N.L.; Awh, C.C.; Kunimoto, D.Y.; Marcus, D.M.; Wroblewski, J.J.; King, J.; et al. Effect of Bevacizumab vs Aflibercept on Visual Acuity Among Patients with Macular Edema Due to Central Retinal Vein Occlusion: The SCORE2 Randomized Clinical Trial. JAMA 2017, 317, 2072–2087. [Google Scholar] [CrossRef]
- Virgili, G.; Parravano, M.; Evans, J.R.; Gordon, I.; Lucenteforte, E. Anti-vascular endothelial growth factor for diabetic macular oedema: A network meta-analysis. Cochrane Database Syst. Rev. 2017, 6, 1465–1858. [Google Scholar] [CrossRef]
- Shirley, M. Faricimab: First Approval. Drugs 2022, 82, 825–830. [Google Scholar] [CrossRef]
- Bressler, N.M. Treatment of Macular Edema Due to Central Retinal Vein Occlusion: Another Score for Repackaged Bevacizumab. JAMA 2017, 317, 2067–2069. [Google Scholar] [CrossRef]
- Pakzad-Vaezi, K.; Mehta, H.; Mammo, Z.; Tufail, A. Vascular endothelial growth factor inhibitor use and treatment approach for choroidal neovascularization secondary to pathologic myopia. Expert Opin. Biol. Ther. 2016, 16, 873–881. [Google Scholar] [CrossRef] [PubMed]
- Sayanagi, K.; Uematsu, S.; Hara, C.; Wakabayashi, T.; Fukushima, Y.; Sato, S.; Ikuno, Y.; Nishida, K. Effect of intravitreal injection of aflibercept or ranibizumab on chorioretinal atrophy in myopic choroidal neovascularization. Graefe’s Arch. Clin. Exp. Ophthalmol. 2019, 257, 749–757. [Google Scholar] [CrossRef] [PubMed]
- Ruiz-Moreno, J.M.; Montero, J.A.; Amat-Peral, P. Myopic choroidal neovascularization treated by intravitreal bevacizumab: Comparison of two different initial doses. Graefe’s Arch. Clin. Exp. Ophthalmol. 2011, 249, 595–599. [Google Scholar] [CrossRef] [PubMed]
- Toto, L.; Di Antonio, L.; Costantino, O.; Mastropasqua, R. Anti-VEGF Therapy in Myopic CNV. Curr. Drug Targets 2021, 22, 1054–1063. [Google Scholar] [CrossRef] [PubMed]
- Ng, D.S.C.; Fung, N.S.K.; Yip, F.L.T.; Lai, T.Y.Y. Ranibizumab for myopic choroidal neovascularization. Expert Opin. Biol. Ther. 2020, 20, 1385–1393. [Google Scholar] [CrossRef]

| Ocular Disease | Monoclonal Antibody | Target | References |
|---|---|---|---|
| Age-related macular degeneration | Ranibizumab | VEGF-A | [88] |
| Brolucizumab | VEGF-A | [89,90] | |
| Bevacizumab | VEGF | [91] | |
| Aflibercept | VEGF | [92,93] | |
| Conbercept | VEGF | [94] | |
| Faricimab | VEGF; Ang-2 | [92,95] | |
| Uveitis | Daclizumab | IL2 | [96] |
| Infliximab | TNF | [97] | |
| Etanercept | TNF | [97] | |
| Golimumab | TNF | [96] | |
| Secukinumab | IL-17A | [96] | |
| Neovascular glaucoma | Bevacizumab | VEGF | [98] |
| Aflibercept | VEGF | [98] | |
| Diabetic macular edema | Aflibercept | VEGF | [99] |
| Bevacizumab | VEGF | [99] | |
| Brolucizumab | VEGF-A | [90] | |
| Faricimab | VEGF; Ang-2 | [95] | |
| Macular edema due to retinal vein occlusion | Aflibercept | VEGF | [98] |
| Faricimab | VEGF; Ang-2 | [100] | |
| Bevacizumab | VEGF | [98,101] | |
| Myopic choroidal neovascularization | Aflibercept | VEGF | [102,103] |
| Bevacizumab | VEGF | [104,105] | |
| Ranibizumab | VEGF-A | [103,106] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Henriques, C.; da Ana, R.; Krambeck, K.; Miguel, S.; Santini, A.; Zielińska, A.; Souto, E.B. Monoclonal Antibodies for the Treatment of Ocular Diseases. J. Clin. Med. 2024, 13, 5815. https://doi.org/10.3390/jcm13195815
Henriques C, da Ana R, Krambeck K, Miguel S, Santini A, Zielińska A, Souto EB. Monoclonal Antibodies for the Treatment of Ocular Diseases. Journal of Clinical Medicine. 2024; 13(19):5815. https://doi.org/10.3390/jcm13195815
Chicago/Turabian StyleHenriques, Cristina, Raquel da Ana, Karolline Krambeck, Sónia Miguel, Antonello Santini, Aleksandra Zielińska, and Eliana B. Souto. 2024. "Monoclonal Antibodies for the Treatment of Ocular Diseases" Journal of Clinical Medicine 13, no. 19: 5815. https://doi.org/10.3390/jcm13195815
APA StyleHenriques, C., da Ana, R., Krambeck, K., Miguel, S., Santini, A., Zielińska, A., & Souto, E. B. (2024). Monoclonal Antibodies for the Treatment of Ocular Diseases. Journal of Clinical Medicine, 13(19), 5815. https://doi.org/10.3390/jcm13195815









