The Changing Landscape of Intravenous Thrombolysis for Acute Ischaemic Stroke
Abstract
1. Introduction
2. Time Window for Thrombolysis—From Time Clock to Tissue Clock
3. Clinical Trials of Tenecteplase
4. Mild Ischaemic Stroke
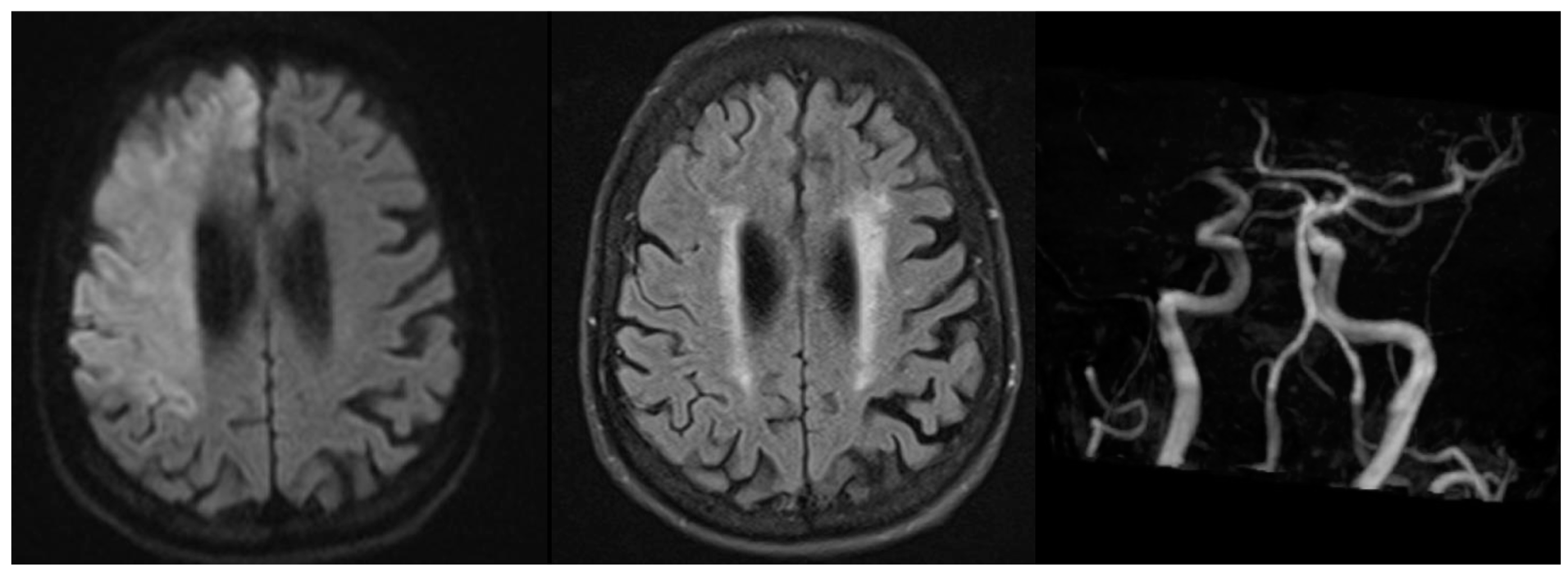
5. Non-Advanced Imaging for Wake-Up Stroke
6. Thrombolysis Prior to Endovascular Thrombectomy
7. Guideline Recommendations for Tenecteplase
8. Transitioning to Tenecteplase—Real World Application
9. Pragmatic Consideration for Transitioning to Tenecteplase Thrombolysis
10. Tenecteplase Transition to Low Resource Health Settings
11. Conclusions and Future Directions
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
References
- National Institute of Neurological Disorders and Stroke rt-PA Stroke Study Group. Tissue Plasminogen Activator for Acute Ischemic Stroke. N. Engl. J. Med. 1995, 333, 1581–1588. [Google Scholar] [CrossRef] [PubMed]
- Demeestere, J.; Wouters, A.; Christensen, S.; Lemmens, R.; Lansberg, M.G. Review of Perfusion Imaging in Acute Ischemic Stroke. Stroke 2020, 51, 1017–1024. [Google Scholar] [CrossRef] [PubMed]
- de Werf, F.V. Single-bolus tenecteplase compared with front-loaded alteplase in acute myocardial infarction: The ASSENT-2 double-blind randomised trial. Lancet 1999, 354, 716–722. [Google Scholar] [CrossRef] [PubMed]
- Campbell, B.C.V.; Mitchell, P.J.; Churilov, L.; Yassi, N.; Kleinig, T.J.; Dowling, R.J.; Yan, B.; Bush, S.J.; Dewey, H.M.; Thijs, V.; et al. Tenecteplase versus Alteplase before Thrombectomy for Ischemic Stroke. N. Engl. J. Med. 2018, 378, 1573–1582. [Google Scholar] [CrossRef] [PubMed]
- Kvistad, C.E.; Næss, H.; Helleberg, B.H.; Idicula, T.; Hagberg, G.; Nordby, L.M.; Jenssen, K.N.; Tobro, H.; Rörholt, D.M.; Kaur, K.; et al. Tenecteplase versus alteplase for the management of acute ischaemic stroke in Norway (NOR-TEST 2, part A): A phase 3, randomised, open-label, blinded endpoint, non-inferiority trial. Lancet Neurol. 2022, 21, 511–519. [Google Scholar] [CrossRef] [PubMed]
- Menon, B.K.; Buck, B.H.; Singh, N.; Deschaintre, Y.; Almekhlafi, M.A.; Coutts, S.B.; Thirunavukkarasu, S.; Khosravani, H.; Appireddy, R.; Moreau, F.; et al. Intravenous tenecteplase compared with alteplase for acute ischaemic stroke in Canada (AcT): A pragmatic, multicentre, open-label, registry-linked, randomised, controlled, non-inferiority trial. Lancet 2022, 400, 161–169. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Li, S.; Pan, Y.; Li, H.; Parsons, M.W.; Campbell, B.C.V.; Schwamm, L.H.; Fisher, M.; Che, F.; Dai, H.; et al. Tenecteplase versus alteplase in acute ischaemic cerebrovascular events (TRACE-2): A phase 3, multicentre, open-label, randomised controlled, non-inferiority trial. Lancet 2023, 401, 645–654. [Google Scholar] [CrossRef] [PubMed]
- Bivard, A.; Garcia-Esperon, C.; Churilov, L.; Spratt, N.; Russell, M.; Campbell, B.C.; Choi, P.; Kleinig, T.; Ma, H.; Markus, H.; et al. Tenecteplase versus alteplase for stroke thrombolysis evaluation (TASTE): A multicentre, prospective, randomized, open-label, blinded-endpoint, controlled phase III non-inferiority trial protocol. Int. J. Stroke 2023, 18, 751–756. [Google Scholar] [CrossRef] [PubMed]
- Xiong, Y.; Campbell, B.C.V.; Schwamm, L.H.; Meng, X.; Jin, A.; Parsons, M.W.; Fisher, M.; Jiang, Y.; Che, F.; Wang, L.; et al. Tenecteplase for Ischemic Stroke at 4.5 to 24 Hours without Thrombectomy. N. Engl. J. Med. 2024, 391, 203–212. [Google Scholar] [CrossRef]
- Alamowitch, S.; Turc, G.; Palaiodimou, L.; Bivard, A.; Cameron, A.; De Marchis, G.M.; Fromm, A.; Kõrv, J.; Roaldsen, M.B.; Katsanos, A.H.; et al. European Stroke Organisation (ESO) expedited recommendation on tenecteplase for acute ischaemic stroke. Eur. Stroke J. 2023, 8, 8–54. [Google Scholar] [CrossRef]
- Canadian Stroke Best Practices. Acute Stroke Management. Available online: https://www.strokebestpractices.ca/en/recommendations/acute-stroke-management/ (accessed on 22 September 2024).
- Hacke, W.; Guidetti, D.; Machnig, T.; Toni, D. Thrombolysis with Alteplase 3 to 4.5 Hours after Acute Ischemic Stroke. N. Engl. J. Med. 2008, 359, 1317–1329. [Google Scholar] [CrossRef] [PubMed]
- Campbell, B.C.V.; Ma, H.; Ringleb, P.A.; Parsons, M.W.; Churilov, L.; Bendszus, M.; Levi, C.R.; Hsu, C.; Kleinig, T.J.; Fatar, M.; et al. Extending thrombolysis to 4·5–9 h and wake-up stroke using perfusion imaging: A systematic review and meta-analysis of individual patient data. Lancet 2019, 394, 139–147. [Google Scholar] [CrossRef] [PubMed]
- Albers, G.W.; Jumaa, M.; Purdon, B.; Zaidi, S.F.; Streib, C.; Shuaib, A.; Sangha, N.; Kim, M.; Froehler, M.T.; Schwartz, N.E.; et al. Tenecteplase for Stroke at 4.5 to 24 Hours with Perfusion-Imaging Selection. N. Engl. J. Med. 2024, 390, 701–711. [Google Scholar] [CrossRef] [PubMed]
- Haley, E.C.; Lyden, P.D.; Johnston, K.C.; Hemmen, T.M. The TNK in Stroke Investigators A Pilot Dose-Escalation Safety Study of Tenecteplase in Acute Ischemic Stroke. Stroke 2005, 36, 607–612. [Google Scholar] [CrossRef] [PubMed]
- Logallo, N.; Novotny, V.; Assmus, J.; Kvistad, C.E.; Alteheld, L.; Rønning, O.M.; Thommessen, B.; Amthor, K.-F.; Ihle-Hansen, H.; Kurz, M.; et al. Tenecteplase versus alteplase for management of acute ischaemic stroke (NOR-TEST): A phase 3, randomised, open-label, blinded endpoint trial. Lancet Neurol. 2017, 16, 781–788. [Google Scholar] [CrossRef]
- Campbell, B.C.V.; Mitchell, P.J.; Churilov, L.; Yassi, N.; Kleinig, T.J.; Dowling, R.J.; Yan, B.; Bush, S.J.; Thijs, V.; Scroop, R.; et al. Effect of Intravenous Tenecteplase Dose on Cerebral Reperfusion Before Thrombectomy in Patients with Large Vessel Occlusion Ischemic Stroke: The EXTEND-IA TNK Part 2 Randomized Clinical Trial. JAMA 2020, 323, 1257–1265. [Google Scholar] [CrossRef] [PubMed]
- Bivard, A.; Zhao, H.; Churilov, L.; Campbell, B.C.V.; Coote, S.; Yassi, N.; Yan, B.; Valente, M.; Sharobeam, A.; Balabanski, A.H.; et al. Comparison of tenecteplase with alteplase for the early treatment of ischaemic stroke in the Melbourne Mobile Stroke Unit (TASTE-A): A phase 2, randomised, open-label trial. Lancet Neurol. 2022, 21, 520–527. [Google Scholar] [CrossRef] [PubMed]
- Roaldsen, M.B.; Eltoft, A.; Wilsgaard, T.; Christensen, H.; Engelter, S.T.; Indredavik, B.; Jatužis, D.; Karelis, G.; Kõrv, J.; Lundström, E.; et al. Safety and efficacy of tenecteplase in patients with wake-up stroke assessed by non-contrast CT (TWIST): A multicentre, open-label, randomised controlled trial. Lancet Neurol. 2023, 22, 117–126. [Google Scholar] [CrossRef]
- Coutts, S.B.; Ankolekar, S.; Appireddy, R.; Arenillas, J.F.; Assis, Z.; Bailey, P.; Barber, P.A.; Bazan, R.; Buck, B.H.; Butcher, K.S.; et al. Tenecteplase versus standard of care for minor ischaemic stroke with proven occlusion (TEMPO-2): A randomised, open label, phase 3 superiority trial. Lancet 2024, 403, 2597–2605. [Google Scholar] [CrossRef]
- Parsons, M.W.; Yogendrakumar, V.; Churilov, L.; Garcia-Esperon, C.; Campbell, B.C.; Russell, M.L.; Sharma, G.; Chen, C.; Lin, L.; Chew, B.L.; et al. Tenecteplase versus alteplase for thrombolysis in patients selected by use of perfusion imaging within 4· 5 h of onset of ischaemic stroke (TASTE): A multicentre, randomised, controlled, phase 3 non-inferiority trial. Lancet Neurol. 2024, 23, 775–786. [Google Scholar] [CrossRef]
- Muir, K.; Ford, G.; Ford, I.; Wardlaw, J.; McConnachie, A.; Greenlaw, N.; Mair, G.; Sprigg, N.; Price, C.I.; Macleod, M.J.; et al. Randomised Trial of Tenectplase Versus Alteplase for Acute Stroke within 4.5h of Onset: The Second Alteplase-Tenecteplase Trial Evaluation for Stroke Thrombolysis (ATTEST-2). 2024. Available online: https://www.ssrn.com/abstract=4831843 (accessed on 8 September 2024).
- Parsons, M.; Spratt, N.; Bivard, A.; Campbell, B.; Chung, K.; Miteff, F.; O’Brien, B.; Bladin, C.; McElduff, P.; Allen, C.; et al. A Randomized Trial of Tenecteplase versus Alteplase for Acute Ischemic Stroke. N. Engl. J. Med. 2012, 366, 1099–1107. [Google Scholar] [CrossRef] [PubMed]
- Khatri, P.; Kleindorfer, D.O.; Devlin, T.; Sawyer, R.N.; Starr, M.; Mejilla, J.; Broderick, J.; Chatterjee, A.; Jauch, E.C.; Levine, S.R.; et al. Effect of Alteplase vs Aspirin on Functional Outcome for Patients with Acute Ischemic Stroke and Minor Nondisabling Neurologic Deficits: The PRISMS Randomized Clinical Trial. JAMA 2018, 320, 156. [Google Scholar] [CrossRef] [PubMed]
- Chen, H.-S.; Cui, Y.; Zhou, Z.-H.; Zhang, H.; Wang, L.-X.; Wang, W.-Z.; Shen, L.-Y.; Guo, L.-Y.; Wang, E.-Q.; Wang, R.-X.; et al. Dual Antiplatelet Therapy vs Alteplase for Patients with Minor Nondisabling Acute Ischemic Stroke: The ARAMIS Randomized Clinical Trial. JAMA 2023, 329, 2135. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Lv, T.; Nguyen, T.N.; Wu, S.; Li, Z.; Bai, X.; Chen, D.; Zhao, C.; Lin, W.; Chen, S.; et al. Intravenous Alteplase Versus Best Medical Therapy for Patients with Minor Stroke: A Systematic Review and Meta-Analysis. Stroke 2024, 55, 883–892. [Google Scholar] [CrossRef] [PubMed]
- Seners, P.; Perrin, C.; Lapergue, B.; Henon, H.; Debiais, S.; Sablot, D.; Girard Buttaz, I.; Tamazyan, R.; Preterre, C.; Laksiri, N.; et al. Bridging Therapy or IV Thrombolysis in Minor Stroke with Large Vessel Occlusion. Ann. Neurol. 2020, 88, 160–169. [Google Scholar] [CrossRef]
- Derdeyn, C. Advances in Thrombectomy for Acute Ischemic Stroke. JAMA Surg. 2024, 159, 604. [Google Scholar] [CrossRef] [PubMed]
- Kaesmacher, J.; Cavalcante, F.; Kappelhof, M.; Treurniet, K.M.; Rinkel, L.; Liu, J.; Yan, B.; Zi, W.; Kimura, K.; Eker, O.F.; et al. Time to Treatment with Intravenous Thrombolysis Before Thrombectomy and Functional Outcomes in Acute Ischemic Stroke: A Meta-Analysis. JAMA 2024, 331, 764–777. [Google Scholar] [CrossRef]
- Canadian Stroke Best Practices. 5. Acute Ischemic Stroke Treatment. 2024. Available online: https://www.strokebestpractices.ca/en/recommendations/acute-stroke-management/acute-ischemic-stroke-treatment/ (accessed on 7 August 2024).
- Stroke. Guidelines for the Early Management of Patients with Acute Ischemic Stroke: 2019 Update to the 2018 Guidelines for the Early Management of Acute Ischemic Stroke: A Guideline for Healthcare Professionals from the American Heart Association/American Stroke Association. Available online: https://www.ahajournals.org/doi/10.1161/STR.0000000000000211 (accessed on 7 August 2024).
- Mahawish, K.; Gommans, J.; Kleinig, T.; Lallu, B.; Tyson, A.; Ranta, A. Switching to Tenecteplase for Stroke Thrombolysis: Real-World Experience and Outcomes in a Regional Stroke Network. Stroke 2021, 52, e590–e593. [Google Scholar] [CrossRef] [PubMed]
- Gerschenfeld, G.; Smadja, D.; Turc, G.; Olindo, S.; Laborne, F.-X.; Yger, M.; Caroff, J.; Gonçalves, B.; Seners, P.; Cantier, M.; et al. Functional Outcome, Recanalization, and Hemorrhage Rates After Large Vessel Occlusion Stroke Treated with Tenecteplase Before Thrombectomy. Neurology 2021, 97, E2173–E2184. [Google Scholar] [CrossRef]
- Warach, S.J.; Dula, A.N.; Milling, T.J.; Miller, S.; Allen, L.; Zuck, N.D.; Miller, C.; Jesser, C.A.; Misra, L.R.; Miley, J.T.; et al. Prospective Observational Cohort Study of Tenecteplase Versus Alteplase in Routine Clinical Practice. Stroke 2022, 53, 3583–3593. [Google Scholar] [CrossRef] [PubMed]
- Warach, S.J.; Ranta, A.; Kim, J.; Song, S.S.; Wallace, A.; Beharry, J.; Gibson, D.; Cadilhac, D.A.; Bladin, C.F.; Kleinig, T.J.; et al. Symptomatic Intracranial Hemorrhage with Tenecteplase vs Alteplase in Patients with Acute Ischemic Stroke: The Comparative Effectiveness of Routine Tenecteplase vs Alteplase in Acute Ischemic Stroke (CERTAIN) Collaboration. JAMA Neurol. 2023, 80, 732–738. [Google Scholar] [CrossRef] [PubMed]
- Pace, A.; Wai, M.; Frye, E. Implementation of a Tenecteplase Protocol for Treatment of Acute Ischemic Stroke in a Health System. Innov. Pharm. 2024, 15. Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC11107964/ (accessed on 1 September 2024).
- Zhong, C.S.; Beharry, J.; Salazar, D.; Smith, K.; Withington, S.; Campbell, B.C.V.; Wilson, D.; Le Heron, C.; Mason, D.; Duncan, R.; et al. Routine Use of Tenecteplase for Thrombolysis in Acute Ischemic Stroke. Stroke 2021, 52, 1087–1090. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.-H.; Guo, Z.-N.; Chen, M.-R.; Yao, Z.-G.; Nguyen, T.N.; Saver, J.L.; Yang, Y.; Chen, H.-S. Intravenous tenecteplase for acute ischemic stroke between 4.5 and 6 h of onset (EXIT-BT2): Rationale and Design. Eur. Stroke J. 2024. first published online. [Google Scholar] [CrossRef]
| Author | Year | Design/Trial Name | Participants | Tenecteplase dose | Comparison | Primary Outcome | Notes |
|---|---|---|---|---|---|---|---|
| Logallo et al. [16] | 2017 | Randomised, open-label, blinded, superiority trial. NOR-TEST. | 1100, across 13 stroke units in Norway | 0.4 mg/kg | Alteplase 0.9 mg/kg | mRS 0–3 at 3 months. OR 1.08 (CI 0.84–1.38) p = 0.52 | Within 4.5 h of symptom onset of awakening with symptoms. Included bridging to thrombectomy. Median NIHSS 4 (IQR 2–8). Secondary and safety outcomes: -Death at day 90 (p = 0.68) -Serious adverse effects by day 90 (p = 0.74) |
| Campbell et al. [4] | 2018 | Randomised, open-label, blinded, non-inferiority followed by superiority trial. EXTEND-IA TNK part 1. | 202, across 13 centres in Australia and New Zealand | 0.25 mg/kg | Alteplase 0.9 mg/kg | Reperfusion of >50% ischaemic territory, or absence of retrievable clot. Non inferiority: -Incidence difference 12 percentage point (CI 2–21) -p = 0.002) Superiority: -Adjusted OR 2.6 (1.1–5.9) -p = 0.02. | Within 4.5 h of symptom onset. Included bridging to thrombectomy. Large vessel occlusions (ICA, M1, M2, basilar). Median NIHSS 17 (IQR 12–22) both groups. Secondary and safety outcomes: -mRS ordinal at 90 days (TNK 2 vs. 3 p = 0.04) -Functional independence (p = 0.06) -Early neuro improvement (p = 0.70) -Safety death (p = 0.08) -sICH (p = 0.99) |
| Campbell et al. [17] | 2020 | Randomised, open-label, blinded. EXTEND-IA TNK part 2. | 300, across 27 hospitals in Australia and New Zealand | 0.4 mg/kg | 0.25 mg/kg tenecteplase | Reperfusion of >50% ischaemic territory. Risk difference 0.0% (CI −8.9%–8.9%) p = 0.89. | Within 4.5 h of symptom onset, before planned thrombectomy. Large vessel occlusions (ICA, M1, M2, basilar). Median NIHSS 17 (0.4 mg/kg) and 16 (0.25 mg/kg). Secondary and safety outcomes: -mRS 90 days (p = 0.73) -Freedom from disability (p = 0.69) -sICH 36 h (p = 0.12) -All-cause death (p = 0.35) |
| Bivard et al. [18] | 2022 | Randomised, open-label, blinded (masked), superiority. TASTE-A. | 104 across 5 tertiary Melbourne hospitals | 0.25 mg/kg | Alteplase 0.9 mg/kg | Volume of perfusion lesion on arrival to hospital on CTP. Adjusted incidence rate ratio 0.55 (CI 0.37–0.81) p = 0.003 | Within 4.5 h of symptom onset. Median NIHSS 8 both groups (IQR 5–14 and 5–17). Secondary and safety outcomes: -mRS 5–6 at 90 days (p = 0.93) -sICH 36 h (none occurred) -Death 90 days (p = 0.88) |
| Kvistad et al. [5] | 2022 | Randomised, open-label, blinded, non-inferiority (3% margin). NOR-TEST 2, part A. | 204 patients across 11 hospitals in Norway | 0.4 mg/kg | Alteplase 0.9 mg/kg | mRS 0–1 at 3 months. OR 0.45 (CI 0.25–0.8). p = 0.0064 | Within 4.5 h of symptom onset. Stopped early due to higher sICH rates in TNK group. Moderate or severe strokes, NIHSS 6 or more. Secondary and safety outcomes: -Any ICH (more TNK p = 0.0031) -sICH (more TNK p = 0.061) -Mortality (more TNK p = 0.013) |
| Menon et al. [6] | 2022 | Randomised, open-label, blinded, non-inferiority 5% margin (secondary superiority). AcT. | 1577 patients across 22 primary and comprehensive stroke centres in Canada | 0.25 mg/kg | Alteplase 0.9 mg/kg | mRS 0–1 at 90–120 days. Risk difference 2.15 (CI −2.6–6.9). Meeting non-inferiority threshold. | Within 4.5 h of symptom onset. Included bridging to thrombectomy. TNK trend to better, not superior, on secondary analysis. Median NIHSS 9 (TNK) 10 (alteplase). Secondary and safety outcomes): -sICH (no difference) -death (no difference) |
| Roaldsen et al. [19] | 2023 | Randomised, control, open-label, blinded endpoint. TWIST. | 578 patients across 77 hospitals in 10 countries. | 0.25 mg/kg | No thrombolysis | mRS at 90 days (ordinal logistic regression with ITT). OR 1.18 (CI 0.88–1.58). p = 0.27. | Within 4.5 h of awakening with symptoms. Wake-up stroke NIHSS > 2 or aphasia. Selection with non-contrast CT. Median ASPECT 10. >50% NIHSS < 8 (see table). Secondary and safety outcomes: -Mortality (p = 0.37) -sICH (p = 0.28) -Any intracranial haem (p = 0.64) |
| Wang et al. [7] | 2023 | Randomised, open-label, blinded endpoint, non-inferiority 3.74%. TRACE−2. | 1430 patients across 53 centres in China | 0.25 mg/kg | Alteplase 0.9 mg/kg | mRS 0–1 at 90 days. RR 1.07 (CI 0.98–1.16). TNK non-inferior. | Within 4.5 h of last known well. Excluded if thrombectomy candidate (ineligible or refused). NIHSS 5–25. >50% NIHSS < 8. Secondary and safety outcomes: -sICH (p = 0.74) -Mortality (0.22) |
| Albers et al. [14] | 2024 | Randomised placebo control, double-blind. TIMELESS. | 458 patients across from 112 centres across USA and Canada. | 0.25 mg/kg | Placebo | mRS at 90 days. Adjusted common odds ratio 1.13 (CI 0.82–1.57). p = 0.45. | 4.5–24 h since last known well. Bridging to thrombectomy included (77.3% of patients). MCA M1 or M2 or ICA ~only. Median NIHSS 12 both groups. Secondary and safety outcomes: -Functional independence (no difference) -sICH (no difference) -Death (no difference) -Sub-group analysis (not powered) favoured TNK in M1 occlusion. |
| Coutts et al. [20] | 2024 | Randomised, open-label control trial, TEMPO−2 | 886 patients across 48 hospitals in Australia, Austria, Brazil, Canada, Finland, Ireland, New Zealand, Singapore, Spain, and UK. | 0.25 mg/kg | Non-thrombolytic standard of care. | Return to baseline function (mRS) RR 0.96 (CI 0.88–1.04) p = 0.29 | Within 12 h of stroke onset. Stopped early for futility (no benefit and possible harm). Minor stroke NIHSS 0–5 with vessel occlusion or perfusion deficit on imaging. Secondary and safety outcomes: -sICH—higher in TNK: RR 4.2 (0.9–19.7, p = 0.059) -Death—higher in TNK: adjusted HR 3.8 (CI 1.4–10.2, p = 0.0085) |
| Xiong et al. [9] | 2024 | Randomised blinded end-point evaluation control, open-label trial TRACE-III | 516 patients across 58 centres in China. | 0.25 mg/kg | Standard medical treatment. | Absence of disability (mRS 0–1) at 90 days Relative rate (?OR) 1.37 (CI 1.04–1.81) p = 0.03 | 4.5–24 h from last known well. Large vessel occlusion (ICA or MCA branches M1 or M2). Excluded if planned for thrombectomy, but <2% (similar in each group) had rescue thrombectomy. Median NIHSS 11 in TNK and 10 in controls groups. Secondary and safety outcomes: -sICH higher in TNK group. -Death (similar between groups) |
| Parsons et al. [21] | 2024 | Randomised, open-label, blinded endpoint, non-inferiority 3%. TASTE | 601 patients (of planned 830 patients) across 35 hospitals in 8 countries. | 0.25 mg/kg | Alteplase 0.9 mg/kg | mRS 0–1 at 3 months. Standardised RD 0.03 (non-inferiority criteria less than −0.03) | Within 4.5 h of symptom onset. Stopped early due to results of previous tenecteplase trials. Non-inferiority demonstrated on per-protocol analysis. Safety Secondary and safety outcomes: -sICH -All cause mortality |
| Muir et al. [22] | Yet to be published. Preprint in the Lancet | Randomised, non-inferior and superiority. ATTEST−2. | 1858 patients across 40 hospitals in the UK. | 0.25 mg/kg | Alteplase 0.9 mg/kg | Adjusted common OR 1.07 (CI 0.90–1.27) meeting non-inferiority, but not superior. | Not published yet but presented at World Stroke Conference 2023. Within 4.5 h of symptom onset. Secondary and safety outcomes: -mRS 0–1 -mRS overall -Safety (no difference) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Donaldson, J.; Winders, J.; Alamri, Y.; Knight, D.; Wu, T.Y. The Changing Landscape of Intravenous Thrombolysis for Acute Ischaemic Stroke. J. Clin. Med. 2024, 13, 5826. https://doi.org/10.3390/jcm13195826
Donaldson J, Winders J, Alamri Y, Knight D, Wu TY. The Changing Landscape of Intravenous Thrombolysis for Acute Ischaemic Stroke. Journal of Clinical Medicine. 2024; 13(19):5826. https://doi.org/10.3390/jcm13195826
Chicago/Turabian StyleDonaldson, Jack, Joel Winders, Yassar Alamri, Dhara Knight, and Teddy Y. Wu. 2024. "The Changing Landscape of Intravenous Thrombolysis for Acute Ischaemic Stroke" Journal of Clinical Medicine 13, no. 19: 5826. https://doi.org/10.3390/jcm13195826
APA StyleDonaldson, J., Winders, J., Alamri, Y., Knight, D., & Wu, T. Y. (2024). The Changing Landscape of Intravenous Thrombolysis for Acute Ischaemic Stroke. Journal of Clinical Medicine, 13(19), 5826. https://doi.org/10.3390/jcm13195826






