Screening for Hypoglycaemia Risk and Medication Changes in Diabetes Patients Using Pharmacy Dispensing Data
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Data Source
2.2. Study Population and Setting
2.3. Outcome Variables
2.3.1. Hypoglycaemia Risk Score
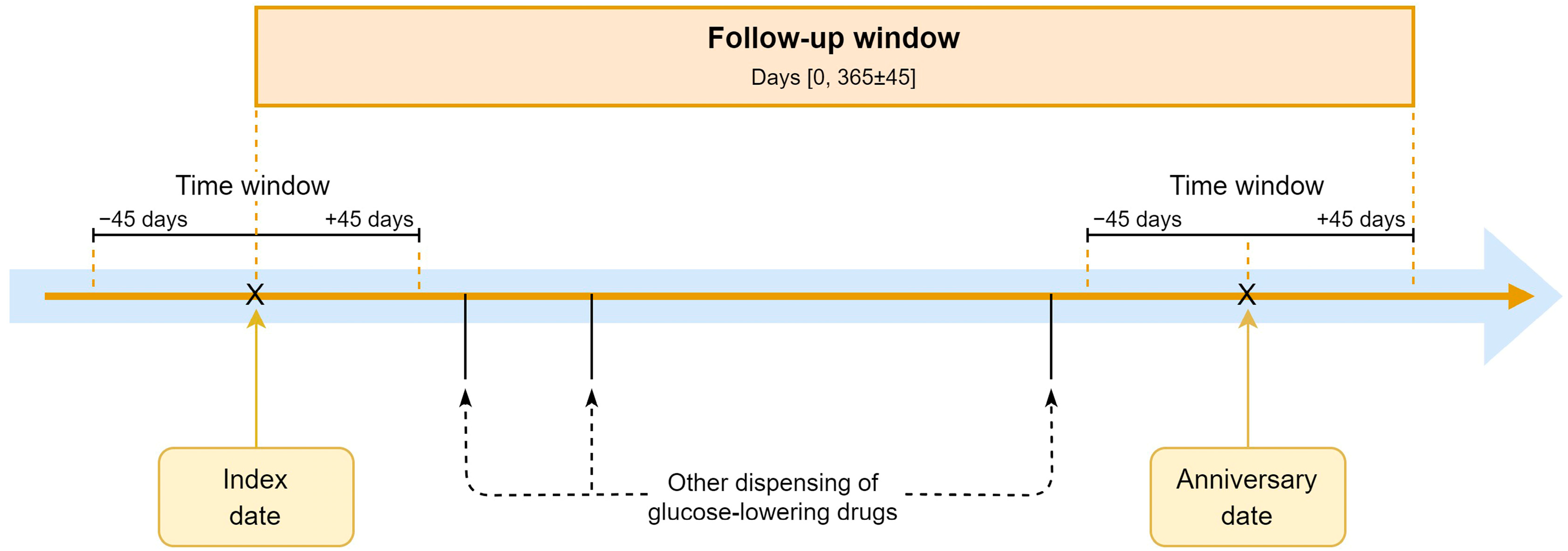
2.3.2. Medication Changes
2.4. Statistical Analysis
3. Results
3.1. Patient Characteristics at the Index Date
3.2. Hypoglycaemia Risk Score and Medication Changes
4. Discussion
4.1. Strengths and Limitations
4.2. Implications for Practice and Research
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Fidler, C.; Elmelund Christensen, T.; Gillard, S. Hypoglycemia: An Overview of Fear of Hypoglycemia, Quality-of-Life, and Impact on Costs. J. Med. Econ. 2011, 14, 646–655. [Google Scholar] [CrossRef] [PubMed]
- Frier, B.M. Hypoglycaemia in Diabetes Mellitus: Epidemiology and Clinical Implications. Nat. Rev. Endocrinol. 2014, 10, 711–722. [Google Scholar] [CrossRef] [PubMed]
- Miller, C.D.; Phillips, L.S.; Ziemer, D.C.; Gallina, D.L.; Cook, C.B.; El-Kebbi, I.M. Hypoglycemia in Patients with Type 2 Diabetes Mellitus. Arch. Intern. Med. 2001, 161, 1653–1659. [Google Scholar] [CrossRef] [PubMed]
- Heller, S.R.; Peyrot, M.; Oates, S.K.; Taylor, A.D. Hypoglycemia in Patient with Type 2 Diabetes Treated with Insulin: It Can Happen. BMJ Open Diabetes Res. Care 2020, 8, e001194. [Google Scholar] [CrossRef] [PubMed]
- Van Meijel, L.A.; De Vegt, F.; Abbink, E.J.; Rutters, F.; Schram, M.T.; Van Der Klauw, M.M.; Wolffenbuttel, B.H.R.; Siegelaar, S.; Devries, J.H.; Sijbrands, E.J.G.; et al. High Prevalence of Impaired Awareness of Hypoglycemia and Severe Hypoglycemia among People with Insulin-Treated Type 2 Diabetes: The Dutch Diabetes Pearl Cohort. BMJ Open Diabetes Res. Care 2020, 8, e000935. [Google Scholar] [CrossRef] [PubMed]
- Schopman, J.E.; Simon, A.C.R.; Hoefnagel, S.J.M.; Hoekstra, J.B.L.; Scholten, R.J.P.M.; Holleman, F. The Incidence of Mild and Severe Hypoglycaemia in Patients with Type 2 Diabetes Mellitus Treated with Sulfonylureas: A Systematic Review and Meta-Analysis. Diabetes Metab. Res. Rev. 2014, 30, 11–22. [Google Scholar] [CrossRef]
- Alwafi, H.; Alsharif, A.A.; Wei, L.; Langan, D.; Naser, A.Y.; Mongkhon, P.; Bell, J.S.; Ilomaki, J.; Al Metwazi, M.S.; Man, K.K.C.; et al. Incidence and Prevalence of Hypoglycaemia in Type 1 and Type 2 Diabetes Individuals: A Systematic Review and Meta-Analysis. Diabetes Res. Clin. Pract. 2020, 170, 108522. [Google Scholar] [CrossRef] [PubMed]
- Crutzen, S.; van den Born-Bondt, T.; Denig, P.; Taxis, K. Type 2 Diabetes Patients’ Views on Prevention of Hypoglycaemia—A Mixed Methods Study Investigating Self-Management Issues and Self-Identified Causes of Hypoglycaemia. BMC Fam. Pract. 2021, 22, 114. [Google Scholar] [CrossRef]
- Karter, A.J.; Moffet, H.H.; Liu, J.Y.; Lipska, K.J. Surveillance of Hypoglycemia-Limitations of Emergency Department and Hospital Utilization Data. JAMA Intern. Med. 2018, 178, 987–988. [Google Scholar] [CrossRef]
- Robberechts, A.; Brumer, M.; Garcia-Cardenas, V.; Dupotey, N.M.; Steurbaut, S.; De Meyer, G.R.Y.; De Loof, H. Medication Review: What’s in a Name and What Is It about? Pharmacy 2024, 12, 39. [Google Scholar] [CrossRef]
- Karter, A.J.; Warton, E.M.; Lipska, K.J.; Ralston, J.D.; Moffet, H.H.; Jackson, G.G.; Huang, E.S.; Miller, D.R. Development and Validation of a Tool to Identify Patients with Type 2 Diabetes at High Risk of Hypoglycemia-Related Emergency Department or Hospital Use. JAMA Intern. Med. 2017, 177, 1461–1470. [Google Scholar] [CrossRef]
- Ruan, Y.; Bellot, A.; Moysova, Z.; Tan, G.D.; Lumb, A.; Davies, J.; van der Schaar, M.; Rea, R. Predicting the Risk of Inpatient Hypoglycemia with Machine Learning Using Electronic Health Records. Diabetes Care 2020, 43, 1504–1511. [Google Scholar] [CrossRef] [PubMed]
- Crutzen, S.; Schuling, J.; Hugtenburg, J.G.; Verduijn, M.; Teichert, M.; Taxis, K.; Denig, P. Development and Piloting of an Algorithm to Select Older Patients for Different Types of Medication Review. Front. Pharmacol. 2019, 10, 217. [Google Scholar] [CrossRef] [PubMed]
- Chow, L.S.; Zmora, R.; Ma, S.; Seaquist, E.R.; Schreiner, P.J. Development of a Model to Predict 5-Year Risk of Severe Hypoglycemia in Patients with Type 2 Diabetes. BMJ Open Diabetes Res. Care 2018, 6, e000527. [Google Scholar] [CrossRef] [PubMed]
- Hu, X.; Xu, W.; Lin, S.; Zhang, C.; Ling, C.; Chen, M. Development and Validation of a Hypoglycemia Risk Model for Intensive Insulin Therapy in Patients with Type 2 Diabetes. J. Diabetes Res. 2020, 2020, 7292108. [Google Scholar] [CrossRef] [PubMed]
- Crutzen, S.; Belur Nagaraj, S.; Taxis, K.; Denig, P. Identifying Patients at Increased Risk of Hypoglycaemia in Primary Care: Development of a Machine Learning-Based Screening Tool. Diabetes Metab. Res. Rev. 2021, 37, e3426. [Google Scholar] [CrossRef] [PubMed]
- Crutzen, S.; Baas, G.; Denig, P.; Heringa, M.; Taxis, K. Pharmacist-Led Intervention Aimed at Deprescribing and Appropriate Use of Cardiometabolic Medication among People with Type 2 Diabetes. Res. Soc. Adm. Pharm. 2023, 19, 783–792. [Google Scholar] [CrossRef] [PubMed]
- Reeve, E.; Gnjidic, D.; Long, J.; Hilmer, S. A Systematic Review of the Emerging Definition of “deprescribing” with Network Analysis: Implications for Future Research and Clinical Practice. Br. J. Clin. Pharmacol. 2015, 80, 1254–1268. [Google Scholar] [CrossRef] [PubMed]
- Kassis, A.; Moles, R.; Carter, S. Stakeholders’ Perspectives and Experiences of the Pharmacist’s Role in Deprescribing in Ambulatory Care: A Qualitative Meta-Synthesis. Res. Soc. Adm. Pharm. 2024, 20, 697–712. [Google Scholar] [CrossRef]
- Vijayakumar, P.; Liu, S.; McCoy, R.G.; Karter, A.J.; Lipska, K.J. Changes in Management of Type 2 Diabetes before and after Severe Hypoglycemia. Diabetes Care 2020, 43, e188–e189. [Google Scholar] [CrossRef] [PubMed]
- Alexopoulos, A.S.; Kahkoska, A.R.; Pate, V.; Bradley, M.C.; Niznik, J.; Thorpe, C.; Stürmer, T.; Buse, J. Deintensification of Treatment with Sulfonylurea and Insulin after Severe Hypoglycemia among Older Adults with Diabetes. JAMA Netw. Open 2021, 4, e2132215. [Google Scholar] [CrossRef] [PubMed]
- Oktora, M.P.; Kerr, K.P.; Hak, E.; Denig, P. Rates, Determinants and Success of Implementing Deprescribing in People with Type 2 Diabetes: A Scoping Review. Diabet. Med. 2021, 38, e14408. [Google Scholar] [CrossRef] [PubMed]
- Naser, A.Y.; Alsairafi, Z.; Alwafi, H.; Mohammad Turkistani, F.; Saud Bokhari, N.; Alenazi, B.; Zmaily Dahmash, E.; Alyami, H.S. The Perspectives of Physicians Regarding Antidiabetic Therapy De-Intensification and Factors Affecting Their Treatment Choices—A Cross-Sectional Study. Int. J. Clin. Pract. 2021, 75, e13662. [Google Scholar] [CrossRef] [PubMed]
- Seidu, S.; Kunutsor, S.K.; Topsever, P.; Hambling, C.E.; Cos, F.X.; Khunti, K. Deintensification in Older Patients with Type 2 Diabetes: A Systematic Review of Approaches, Rates and Outcomes. Diabetes Obes. Metab. 2019, 21, 1668–1679. [Google Scholar] [CrossRef] [PubMed]
- Sabaté, M.; Montané, E. Pharmacoepidemiology: An Overview. J. Clin. Med. 2023, 12, 7033. [Google Scholar] [CrossRef] [PubMed]
- Rasmussen, L.; Wettermark, B.; Steinke, D.; Pottegård, A. Core Concepts in Pharmacoepidemiology: Measures of Drug Utilization Based on Individual-Level Drug Dispensing Data. Pharmacoepidemiol. Drug Saf. 2022, 31, 1015–1026. [Google Scholar] [CrossRef] [PubMed]
- Visser, S.T.; Schuiling-Veninga, C.C.; Bos, J.H.; De Jong-Van Den Berg, L.T.; Postma, M.J. The Population-Based Prescription Database IADB.Nl: Its Development, Usefulness in Outcomes Research and Challenges. Expert. Rev. Pharmacoecon Outcomes Res. 2013, 13, 285–292. [Google Scholar] [CrossRef]
- Sharma, M.; Petersen, I.; Nazareth, I.; Coton, S.J. An Algorithm for Identification and Classification of Individuals with Type 1 and Type 2 Diabetes Mellitus in a Large Primary Care Database. Clin. Epidemiol. 2016, 8, 373–380. [Google Scholar] [CrossRef] [PubMed]
- Ese, B.; Hjg, B.; Rooij, D.A.; Hart, H.; Houweling, S.; IJzerman, R.; Janssen, P.; Kerssen, A.; Oud, M.; Palmen, J.; et al. NHG-Standaard Diabetes Mellitus Type 2 (M01). Available online: https://richtlijnen.nhg.org/standaarden/diabetes-mellitus-type-2 (accessed on 20 May 2023).
- Emmerton, D.; Abdelhafiz, A. Newer Anti-Diabetic Therapies with Low Hypoglycemic Risk-Potential Advantages for Frail Older People. Hosp. Pract. 2021, 49, 164–175. [Google Scholar] [CrossRef] [PubMed]
- McAlister, F.A.; Youngson, E.; Eurich, D.T. Treatment Deintensification Is Uncommon in Adults with Type 2 Diabetes Mellitus: A Retrospective Cohort Study. Circ. Cardiovasc. Qual. Outcomes 2017, 10, e003514. [Google Scholar] [CrossRef]
- Pan, J.; Tejani, A.; Logan, A.; Brodoway, H.; Shukla, K.; Son, M.; Khosla, K.; Moradi, A.; Drummond, I.; McCarthy, L.M.; et al. Rates of Overtreatment and Deprescribing of Antihyperglycemics among Long-Term Care Residents in British Columbia. J. Am. Geriatr. Soc. 2023, 71, 2657–2661. [Google Scholar] [CrossRef]
- Kautzky-Willer, A.; Kosi, L.; Lin, J.; Mihaljevic, R. Gender-Based Differences in Glycaemic Control and Hypoglycaemia Prevalence in Patients with Type 2 Diabetes: Results from Patient-Level Pooled Data of Six Randomized Controlled Trials. Diabetes Obes. Metab. 2015, 17, 533–540. [Google Scholar] [CrossRef] [PubMed]
- Sämanna, A.; Lehmann, T.; Heller, T.; Müller, N.; Hartmann, P.; Wolf, G.B.; Müller, U.A. A Retrospective Study on the Incidence and Risk Factors of Severe Hypoglycemia in Primary Care. Fam. Pract. 2013, 30, 290–293. [Google Scholar] [CrossRef] [PubMed]
- de Vries, S.T.; Denig, P.; Ekhart, C.; Burgers, J.S.; Kleefstra, N.; Mol, P.G.M.; van Puijenbroek, E.P. Sex Differences in Adverse Drug Reactions Reported to the National Pharmacovigilance Centre in the Netherlands: An Explorative Observational Study. Br. J. Clin. Pharmacol. 2019, 85, 1507–1515. [Google Scholar] [CrossRef] [PubMed]
- Agyemang, M.B.; Peters, C.; Stronks, R.J.; Ujcic-Voortman, K.; Van Valkengoed, J.K. Diabetes Mellitus in Nederland. Eur. J. Public Health 1999, 7, 511–516. [Google Scholar]
- Seaquist, E.R.; Anderson, J.; Childs, B.; Cryer, P.; Dagogo-Jack, S.; Fish, L.; Heller, S.R.; Rodriguez, H.; Rosenzweig, J.; Vigersky, R. Hypoglycemia and Diabetes: A Report of a Workgroup of the American Diabetes Association and the Endocrine Society. Diabetes Care 2013, 36, 1384–1395. [Google Scholar] [CrossRef]
- American Diabetes Association 4. Comprehensive Medical Evaluation and Assessment of Comorbidities: Standards of Medical Care in Diabetes-2020. Diabetes Care 2020, 43, S37–S47. [Google Scholar] [CrossRef] [PubMed]
- Brunner, L.; Rodondi, N.; Aubert, C.E. Barriers and Facilitators to Deprescribing of Cardiovascular Medications: A Systematic Review. BMJ Open 2022, 12, e061686. [Google Scholar] [CrossRef] [PubMed]


| Characteristics | High-Risk Category | Low-Risk Category | Total | |||
|---|---|---|---|---|---|---|
| n | % | n | % | n | % | |
| Number of patients | 9867 | 26.9 | 26,761 | 73.1 | 36,628 | 100 |
| Risk score (median [IQR]) | 0.85 (0.79–0.88) | 0.39 (0.35–0.48) | 0.46 (0.36–0.74) | |||
| Age (mean (SD)), years ǂ | 67.9 (11.3) | 67.8 (11.4) | 67.8 (11.4) | |||
| Sex ǂ | ||||||
| Female | 4757 | 48.2 | 12,462 | 46.6 | 17,219 | 47.0 |
| Male | 5110 | 51.8 | 14,299 | 53.4 | 19,409 | 53.0 |
| Total medication count (median [IQR]) ǂ | 9 [7–13] | 7 [5–10] | 7 [5–10] | |||
| Glucose-lowering medication count (median [IQR]) ǂ | 3 [2–3] | 1 [1–2] | 2 [1–2] | |||
| Insulin countǂ | ||||||
| 0 | 2 | 0.0 | 26,755 | 100 | 26,757 | 73.1 |
| 1 | 5573 | 56.5 | 6 | 0.0 | 5579 | 15.2 |
| 2 or more | 4292 | 43.5 | - | - | 4292 | 11.7 |
| Insulin duration (mean (SD), years ǂ | 3.3 (1.6) | - | - | 0.9 (1.7) | ||
| Sulfonylurea count ǂ | ||||||
| 0 | 7068 | 71.6 | 15,574 | 58.2 | 22,642 | 61.8 |
| 1 or more | 2799 | 28.4 | 11,187 | 41.8 | 13,986 | 38.2 |
| Premixed insulin use ǂ | ||||||
| Yes | 1894 | 19.2 | - | - | 1894 | 5.2 |
| No | 7973 | 80.8 | 26,761 | 100 | 34,734 | 94.8 |
| Antidepressant use ǂ | ||||||
| Yes | 1493 | 15.1 | 3237 | 12.1 | 4730 | 12.9 |
| No | 8374 | 84.9 | 23,524 | 87.9 | 31,898 | 87.1 |
| Therapy type for diabetes | ||||||
| Monotherapy | 660 | 6.7 | 16,575 | 62 | 17,235 | 47.1 |
| Combination therapy | 9207 | 93.3 | 10,186 | 38 | 19,393 | 52.9 |
| Glucose-lowering medication classes | ||||||
| Monotherapy | ||||||
| Insulin | 660 | 6.7 | 5 | 0.0 | 665 | 1.8 |
| Metformin | - | - | 14,750 | 55.1 | 14,750 | 40.3 |
| Sulfonylureas | - | - | 1582 | 5.9 | 1582 | 4.3 |
| Alpha glucosidase inhibitors | - | - | 34 | 0.1 | 34 | 0.1 |
| Thiazolidinediones | - | - | 7 | 0.0 | 7 | 0 |
| DPP4 inhibitors | - | - | 79 | 0.3 | 79 | 0.2 |
| GLP-1 agonist | - | - | 36 | 0.1 | 36 | 0.1 |
| SGLT2 inhibitors | - | - | 11 | 0.0 | 11 | 0.0 |
| Other glucose-lowering medications | - | - | 2 | 0.0 | 2 | 0.0 |
| Combination therapy | ||||||
| Insulin combination | 4292 | 43.5 | - | - | 4292 | 11.7 |
| Insulin + sulfonylureas | 2223 | 22.5 | 0 | 0.0 | 2223 | 6.1 |
| Insulin + other medication | 2690 | 27.3 | 1 | 0.0 | 2691 | 7.3 |
| Non-insulin combination, including SU | 2 | 0.0 | 9606 | 35.9 | 9608 | 26.2 |
| Non-insulin combination without SU | 0 | 0.0 | 648 | 2.4 | 648 | 1.8 |
| Treatment Changes | High-Risk Category (n = 9867) | Low-Risk Category (n = 26,761) | Total (n = 36,628) | |||
|---|---|---|---|---|---|---|
| n | % | n | % | n | % | |
| No changes (monotherapy) | ||||||
| No modification of insulin | 557 | 5.6 | 5 | 0.0 | 562 | 1.5 |
| No modification of sulfonylurea | - | - | 1185 | 4.4 | 1185 | 3.2 |
| No modification of other medication | - | - | 12,400 | 46.3 | 12,400 | 33.9 |
| Discontinuation of other medication | - | - | 743 | 2.8 | 743 | 2.0 |
| Addition of other medication to insulin | 54 | 0.5 | - | 54 | 0.1 | |
| Addition of other medication to sulfonylurea | - | - | 180 | 0.7 | 180 | 0.5 |
| Addition of other medication to other medication | - | - | 123 | 0.5 | 123 | 0.3 |
| No changes (combination therapy) | ||||||
| No modification of insulin combination | 3890 | 39.4 | - | - | 3890 | 10.6 |
| No modification of insulin + sulfonylurea | 1683 | 17.1 | - | - | 1683 | 4.6 |
| No modification of insulin + other medication | 2303 | 23.3 | - | - | 2303 | 6.3 |
| No modification of other medication combination | - | - | 369 | 1.4 | 369 | 1.0 |
| No modification of sulfonylurea + other medication | 1 | 0.0 | 7749 | 29.0 | 7750 | 21.2 |
| Discontinuation of other medications | 288 | 2.9 | 369 | 1.4 | 657 | 1.8 |
| Addition of other medication | - | - | 12 | 0.0 | 12 | 0.0 |
| Subtotal | 8776 | 88.9 | 23,135 | 86.5 | 31,911 | 87.0 |
| Intensification (monotherapy) | ||||||
| Addition of insulin | - | - | 303 | 1.1 | 303 | 0.8 |
| Addition of sulfonylurea | 9 | 0.1 | 1359 | 5.1 | 1368 | 3.7 |
| Switching non-insulin to insulin | - | - | 27 | 0.1 | 27 | 0.1 |
| Switching other medication to sulfonylurea | - | - | 143 | 0.5 | 143 | 0.4 |
| Intensification (combination therapy) | ||||||
| Addition of insulin | - | - | 542 | 2.0 | 542 | 1.5 |
| Addition of sulfonylurea | 108 | 1.1 | 115 | 0.4 | 223 | 0.7 |
| Switching non-insulin to insulin | 100 | 1.0 | 143 | 0.5 | 243 | 1.0 |
| Switching other medication to sulfonylurea | 5 | 0.1 | 19 | 0.1 | 24 | 0.1 |
| Subtotal | 222 | 2.3 | 2651 | 9.9 | 2873 | 8.3 |
| De-intensification (monotherapy) | ||||||
| Switching insulin to non-insulin | 15 | 0.1 | - | - | 15 | 0.0 |
| Switching sulfonylurea to another medication | - | - | 29 | 0.1 | 29 | 0.1 |
| Discontinuation of sulfonylurea | - | - | 78 | 0.3 | 78 | 0.2 |
| Discontinuation of insulin | 25 | 0.3 | - | - | 25 | 0.1 |
| De-intensification (combination therapy) | ||||||
| Switching insulin to non-insulin | 37 | 0.4 | - | - | 37 | 0.1 |
| Switching sulfonylurea to another medication | 26 | 0.3 | 60 | 0.2 | 86 | 0.2 |
| Discontinuation of sulfonylurea | 230 | 2.3 | 808 | 3.0 | 1038 | 2.8 |
| Discontinuation of insulin | 536 | 5.4 | - | - | 536 | 1.5 |
| Subtotal | 869 | 8.8 | 975 | 3.6 | 1844 | 5.0 |
| Predictors | Odds Ratios (95%CI) | ||
|---|---|---|---|
| De-Intensification ǂ | Intensification ǂ | ||
| Hypoglycaemia risk category | Low-risk | Reference | Reference |
| High-risk | 2.34 (2.13–2.57) | 0.22 (0.19–0.25) | |
| Sex | Male | Reference | Reference |
| Female | 1.15 (1.03–1.25) | 1.01 (0.94–1.11) | |
| Age | Years | 0.98 (0.98–0.99) | 0.98 (0.97–0.98) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cahyaningsih, I.; Asiri, A.; de Vos, S.; Bos, J.H.J.; Schuiling-Veninga, C.C.M.; Taxis, K.; Denig, P. Screening for Hypoglycaemia Risk and Medication Changes in Diabetes Patients Using Pharmacy Dispensing Data. J. Clin. Med. 2024, 13, 5855. https://doi.org/10.3390/jcm13195855
Cahyaningsih I, Asiri A, de Vos S, Bos JHJ, Schuiling-Veninga CCM, Taxis K, Denig P. Screening for Hypoglycaemia Risk and Medication Changes in Diabetes Patients Using Pharmacy Dispensing Data. Journal of Clinical Medicine. 2024; 13(19):5855. https://doi.org/10.3390/jcm13195855
Chicago/Turabian StyleCahyaningsih, Indriastuti, Amal Asiri, Stijn de Vos, Jens H. J. Bos, Catharina C. M. Schuiling-Veninga, Katja Taxis, and Petra Denig. 2024. "Screening for Hypoglycaemia Risk and Medication Changes in Diabetes Patients Using Pharmacy Dispensing Data" Journal of Clinical Medicine 13, no. 19: 5855. https://doi.org/10.3390/jcm13195855







