Fenoldopam for Renal Protection in Cardiac Surgery: Pharmacology, Clinical Applications, and Evolving Perspectives
Abstract
:1. Introduction
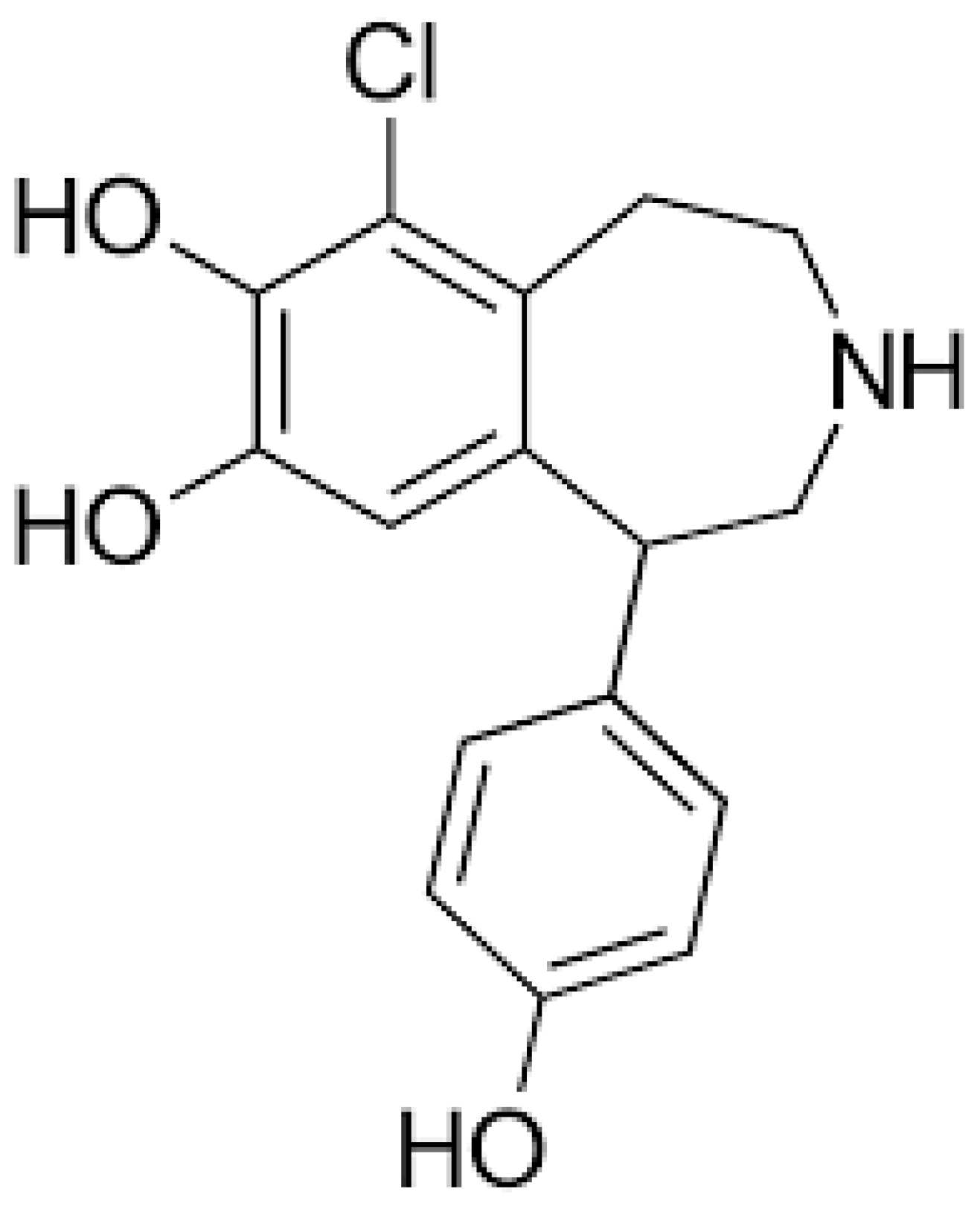
2. Pharmacology of Fenoldopam
3. Renal Protection in Cardiac Surgery
4. Clinical Applications of Fenoldopam in Cardiac Surgery
5. Evidence from Clinical Trials
6. Comparison with Other Renoprotective Strategies
6.1. Dopamine
6.2. Diuretics
6.3. N-Acetylcysteine
6.4. Statins
7. Safety Profile and Side Effects
Contraindications and Precautions
8. Cost-Effectiveness Analysis
9. Current Guidelines and Recommendations
10. Future Directions
11. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Hu, J.; Chen, R.; Liu, S.; Yu, X.; Zou, J.; Ding, X. Global Incidence and Outcomes of Adult Patients with Acute Kidney Injury After Cardiac Surgery: A Systematic Review and Meta-Analysis. J. Cardiothorac. Vasc. Anesth. 2016, 30, 82–89. [Google Scholar] [CrossRef] [PubMed]
- O’Neal, J.B.; Shaw, A.D.; Billings, F.T. Acute kidney injury following cardiac surgery: Current understanding and future directions. Crit. Care 2016, 20, 187. [Google Scholar] [CrossRef] [PubMed]
- Corredor, C.; Thomson, R.; Al-Subaie, N. Long-Term Consequences of Acute Kidney Injury After Cardiac Surgery: A Systematic Review and Meta-Analysis. J. Cardiothorac. Vasc. Anesth. 2016, 30, 69–75. [Google Scholar] [CrossRef] [PubMed]
- Dasta, J.F.; Kane-Gill, S.L.; Durtschi, A.J.; Pathak, D.S.; Kellum, J.A. Costs and outcomes of acute kidney injury (AKI) following cardiac surgery. Nephrol. Dial. Transplant. Off. Publ. Eur. Dial. Transpl. Assoc. Eur. Ren. Assoc. 2008, 23, 1970–1974. [Google Scholar] [CrossRef] [PubMed]
- Gillies, M.A.; Kakar, V.; Parker, R.J.; Honoré, P.M.; Ostermann, M. Fenoldopam to prevent acute kidney injury after major surgery-a systematic review and meta-analysis. Crit. Care 2015, 19, 449. [Google Scholar] [CrossRef]
- Landoni, G.; Biondi-Zoccai, G.G.; Tumlin, J.A.; Bove, T.; De Luca, M.; Calabrò, M.G.; Ranucci, M.; Zangrillo, A. Beneficial impact of fenoldopam in critically ill patients with or at risk for acute renal failure: A meta-analysis of randomized clinical trials. Am. J. Kidney Dis. Off. J. Natl. Kidney Found. 2007, 49, 56–68. [Google Scholar] [CrossRef]
- Meco, M.; Cirri, S. The effect of various fenoldopam doses on renal perfusion in patients undergoing cardiac surgery. Ann. Thorac. Surg. 2010, 89, 497–503. [Google Scholar] [CrossRef]
- Wang, Y.; Bellomo, R. Cardiac surgery-associated acute kidney injury: Risk factors, pathophysiology and treatment. Nature reviews. Nephrology 2017, 13, 697–711. [Google Scholar] [CrossRef]
- Putaggio, A.; Tigano, S.; Caruso, A.; La Via, L.; Sanfilippo, F. Red Blood Cell Transfusion Guided by Hemoglobin Only or Integrating Perfusion Markers in Patients Undergoing Cardiac Surgery: A Systematic Review and Meta-Analysis with Trial Sequential Analysis. J. Cardiothorac. Vasc. Anesth. 2023, 37, 2252–2260. [Google Scholar] [CrossRef]
- Coca, S.G.; Singanamala, S.; Parikh, C.R. Chronic kidney disease after acute kidney injury: A systematic review and meta-analysis. Kidney Int. 2012, 81, 442–448. [Google Scholar] [CrossRef]
- La Via, L.; Vasile, F.; Perna, F.; Zawadka, M. Prediction of fluid responsiveness in critical care: Current evidence and future perspective. Trends Anaesth. Crit. Care 2024, 54, 101316. [Google Scholar] [CrossRef]
- Meersch, M.; Schmidt, C.; Zarbock, A. Perioperative Acute Kidney Injury: An Under-Recognized Problem. Anesth. Analg. 2017, 125, 1223–1232. [Google Scholar] [CrossRef] [PubMed]
- Murphy, M.B.; Murray, C.; Shorten, G.D. Fenoldopam: A selective peripheral dopamine-receptor agonist for the treatment of severe hypertension. N. Engl. J. Med. 2001, 345, 1548–1557. [Google Scholar] [CrossRef] [PubMed]
- Mathur, V.S.; Swan, S.K.; Lambrecht, L.J.; Anjum, S.; Fellmann, J.; McGuire, D.; Epstein, M.; Luther, R.R. The effects of fenoldopam, a selective dopamine receptor agonist, on systemic and renal hemodynamics in normotensive subjects. Crit. Care Med. 1999, 27, 1832–1837. [Google Scholar] [CrossRef] [PubMed]
- Cogliati, A.A.; Vellutini, R.; Nardini, A.; Urovi, S.; Hamdan, M.; Landoni, G.; Guelfi, P. Fenoldopam infusion for renal protection in high-risk cardiac surgery patients: A randomized clinical study. J. Cardiothorac. Vasc. Anesth. 2007, 21, 847–850. [Google Scholar] [CrossRef]
- Brogden, R.N.; Markham, A. Fenoldopam: A review of its pharmacodynamic and pharmacokinetic properties and intravenous clinical potential in the management of hypertensive urgencies and emergencies. Drugs 1997, 54, 634–650. [Google Scholar] [CrossRef]
- Weber, R.R.; McCoy, C.E.; Ziemniak, J.A.; Frederickson, E.D.; Goldberg, L.I.; Murphy, M.B. Pharmacokinetic and pharmacodynamic properties of intravenous fenoldopam, a dopamine1-receptor agonist, in hypertensive patients. Br. J. Clin. Pharmacol. 1988, 25, 17–21. [Google Scholar] [CrossRef]
- Allison, N.L.; Dubb, J.W.; Ziemniak, J.A.; Alexander, F.; Stote, R.M. The effect of fenoldopam, a dopaminergic agonist, on renal hemodynamics. Clin. Pharmacol. Ther. 1987, 41, 282–288. [Google Scholar] [CrossRef]
- Chertow, G.M.; Sayegh, M.H.; Allgren, R.L.; Lazarus, J.M. Is the administration of dopamine associated with adverse or favorable outcomes in acute renal failure? Auriculin Anaritide Acute Renal Failure Study Group. Am. J. Med. 1996, 101, 49–53. [Google Scholar] [CrossRef]
- Halpenny, M.; Rushe, C.; Breen, P.; Cunningham, A.J.; Boucher-Hayes, D.; Shorten, G.D. The effects of fenoldopam on renal function in patients undergoing elective aortic surgery. Eur. J. Anaesthesiol. 2002, 19, 32–39. [Google Scholar] [CrossRef]
- Shusterman, N.H.; Elliott, W.J.; White, W.B. Fenoldopam, but not nitroprusside, improves renal function in severely hypertensive patients with impaired renal function. Am. J. Med. 1993, 95, 161–168. [Google Scholar] [CrossRef] [PubMed]
- Tumlin, J.A.; Finkel, K.W.; Murray, P.T.; Samuels, J.; Cotsonis, G.; Shaw, A.D. Fenoldopam mesylate in early acute tubular necrosis: A randomized, double-blind, placebo-controlled clinical trial. Am. J. Kidney Dis. Off. J. Natl. Kidney Found. 2005, 46, 26–34. [Google Scholar] [CrossRef] [PubMed]
- Aravindan, N.; Natarajan, M.; Shaw, A.D. Fenoldopam inhibits nuclear translocation of nuclear factor kappa B in a rat model of surgical ischemic acute renal failure. J. Cardiothorac. Vasc. Anesth. 2006, 20, 179–186. [Google Scholar] [CrossRef] [PubMed]
- Lavalle, S.; Masiello, E.; Iannella, G.; Magliulo, G.; Pace, A.; Lechien, J.R.; Calvo-Henriquez, C.; Cocuzza, S.; Parisi, F.M.; Favier, V.; et al. Unraveling the Complexities of Oxidative Stress and Inflammation Biomarkers in Obstructive Sleep Apnea Syndrome: A Comprehensive Review. Life 2024, 14, 425. [Google Scholar] [CrossRef] [PubMed]
- Bastin, A.J.; Ostermann, M.; Slack, A.J.; Diller, G.P.; Finney, S.J.; Evans, T.W. Acute kidney injury after cardiac surgery according to Risk/Injury/Failure/Loss/End-stage, Acute Kidney Injury Network, and Kidney Disease: Improving Global Outcomes classifications. J. Crit. Care 2013, 28, 389–396. [Google Scholar] [CrossRef]
- Tigano, S.; Caruso, A.; Liotta, C.; LaVia, L.; Vargas, M.; Romagnoli, S.; Landoni, G.; Sanfilippo, F. Exposure to severe hyperoxemia worsens survival and neurological outcome in patients supported by veno-arterial extracorporeal membrane oxygenation: A meta-analysis. Resuscitation 2024, 194, 110071. [Google Scholar] [CrossRef]
- Rosner, M.H.; Okusa, M.D. Acute kidney injury associated with cardiac surgery. Clin. J. Am. Soc. Nephrol. CJASN 2006, 1, 19–32. [Google Scholar] [CrossRef]
- Medalion, B.; Cohen, H.; Assali, A.; Vaknin Assa, H.; Farkash, A.; Snir, E.; Sharoni, E.; Biderman, P.; Milo, G.; Battler, A.; et al. The effect of cardiac angiography timing, contrast media dose, and preoperative renal function on acute renal failure after coronary artery bypass grafting. J. Thorac. Cardiovasc. Surg. 2010, 139, 1539–1544. [Google Scholar] [CrossRef]
- Sreeram, G.M.; Grocott, H.P.; White, W.D.; Newman, M.F.; Stafford-Smith, M. Transcranial Doppler emboli count predicts rise in creatinine after coronary artery bypass graft surgery. J. Cardiothorac. Vasc. Anesth. 2004, 18, 548–551. [Google Scholar] [CrossRef]
- Karkouti, K.; Beattie, W.S.; Wijeysundera, D.N.; Rao, V.; Chan, C.; Dattilo, K.M.; Djaiani, G.; Ivanov, J.; Karski, J.; David, T.E. Hemodilution during cardiopulmonary bypass is an independent risk factor for acute renal failure in adult cardiac surgery. J. Thorac. Cardiovasc. Surg. 2005, 129, 391–400. [Google Scholar] [CrossRef]
- Azau, A.; Markowicz, P.; Corbeau, J.J.; Cottineau, C.; Moreau, X.; Baufreton, C.; Beydon, L. Increasing mean arterial pressure during cardiac surgery does not reduce the rate of postoperative acute kidney injury. Perfusion 2014, 29, 496–504. [Google Scholar] [CrossRef] [PubMed]
- Barr, L.F.; Kolodner, K. N-acetylcysteine and fenoldopam protect the renal function of patients with chronic renal insufficiency undergoing cardiac surgery. Crit. Care Med. 2008, 36, 1427–1435. [Google Scholar] [CrossRef] [PubMed]
- Mariscalco, G.; Lorusso, R.; Dominici, C.; Renzulli, A.; Sala, A. Acute kidney injury: A relevant complication after cardiac surgery. Ann. Thorac. Surg. 2011, 92, 1539–1547. [Google Scholar] [CrossRef] [PubMed]
- Garg, A.X.; Devereaux, P.J.; Yusuf, S.; Cuerden, M.S.; Parikh, C.R.; Coca, S.G.; Walsh, M.; Novick, R.; Cook, R.J.; Jain, A.R.; et al. Kidney function after off-pump or on-pump coronary artery bypass graft surgery: A randomized clinical trial. JAMA 2014, 311, 2191–2198. [Google Scholar] [CrossRef]
- Mahmoud, A.B.; Burhani, M.S.; Hannef, A.A.; Jamjoom, A.A.; Al-Githmi, I.S.; Baslaim, G.M. Effect of modified ultrafiltration on pulmonary function after cardiopulmonary bypass. Chest 2005, 128, 3447–3453. [Google Scholar] [CrossRef]
- Zarbock, A.; Schmidt, C.; Van Aken, H.; Wempe, C.; Martens, S.; Zahn, P.K.; Wolf, B.; Goebel, U.; Schwer, C.I.; Rosenberger, P.; et al. Effect of remote ischemic preconditioning on kidney injury among high-risk patients undergoing cardiac surgery: A randomized clinical trial. JAMA 2015, 313, 2133–2141. [Google Scholar] [CrossRef]
- Chen, J.J.; Lee, T.H.; Kuo, G.; Huang, Y.T.; Chen, P.R.; Chen, S.W.; Yang, H.Y.; Hsu, H.H.; Hsiao, C.C.; Yang, C.H.; et al. Strategies for post-cardiac surgery acute kidney injury prevention: A network meta-analysis of randomized controlled trials. Front. Cardiovasc. Med. 2022, 9, 960581. [Google Scholar] [CrossRef]
- Sun, H.; Xie, Q.; Peng, Z. Does Fenoldopam Protect Kidney in Cardiac Surgery? A Systemic Review and Meta-Analysis With Trial Sequential Analysis. Shock 2019, 52, 326–333. [Google Scholar] [CrossRef]
- Ranucci, M.; De Benedetti, D.; Bianchini, C.; Castelvecchio, S.; Ballotta, A.; Frigiola, A.; Menicanti, L. Effects of fenoldopam infusion in complex cardiac surgical operations: A prospective, randomized, double-blind, placebo-controlled study. Minerva Anestesiol. 2010, 76, 249–259. [Google Scholar]
- Mancia, G.; Fagard, R.; Narkiewicz, K.; Redon, J.; Zanchetti, A.; Böhm, M.; Christiaens, T.; Cifkova, R.; De Backer, G.; Dominiczak, A.; et al. 2013 ESH/ESC guidelines for the management of arterial hypertension: The Task Force for the Management of Arterial Hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). Eur. Heart J. 2013, 34, 2159–2219. [Google Scholar] [CrossRef]
- Nadkarni, G.N.; Ferrandino, R.; Chang, A.; Surapaneni, A.; Chauhan, K.; Poojary, P.; Saha, A.; Ferket, B.; Grams, M.E.; Coca, S.G. Acute Kidney Injury in Patients on SGLT2 Inhibitors: A Propensity-Matched Analysis. Diabetes Care 2017, 40, 1479–1485. [Google Scholar] [CrossRef] [PubMed]
- Pannu, N.; Nadim, M.K. An overview of drug-induced acute kidney injury. Crit. Care Med. 2008, 36, S216–S223. [Google Scholar] [CrossRef] [PubMed]
- Bove, T.; Zangrillo, A.; Guarracino, F.; Alvaro, G.; Persi, B.; Maglioni, E.; Galdieri, N.; Comis, M.; Caramelli, F.; Pasero, D.C.; et al. Effect of fenoldopam on use of renal replacement therapy among patients with acute kidney injury after cardiac surgery: A randomized clinical trial. JAMA 2014, 312, 2244–2253. [Google Scholar] [CrossRef] [PubMed]
- Landoni, G.; Bove, T.; Pasero, D.; Comis, M.; Orando, S.; Pinelli, F.; Guarracino, F.; Corcione, A.; Galdieri, N.; Zucchetti, M.; et al. Fenoldopam to prevent renal replacement therapy after cardiac surgery. Design of the FENO-HSR study. HSR Proc. Intensive Care Cardiovasc. Anesth. 2010, 2, 111–117. [Google Scholar] [PubMed]
- Friedrich, J.O.; Adhikari, N.; Herridge, M.S.; Beyene, J. Meta-analysis: Low-dose dopamine increases urine output but does not prevent renal dysfunction or death. Ann. Intern. Med. 2005, 142, 510–524. [Google Scholar] [CrossRef]
- Sorbello, M.; Morello, G.; Paratore, A.; Cutuli, M.; Mistretta, G.; Belluoccio, A.A.; Veroux, M.; Veroux, P.; Macarone, M.; Gagliano, M.; et al. Fenoldopam vs dopamine as a nephroprotective strategy during living donor kidney transplantation: Preliminary data. Transplant. Proc. 2007, 39, 1794–1796. [Google Scholar] [CrossRef]
- Ho, K.M.; Power, B.M. Benefits and risks of furosemide in acute kidney injury. Anaesthesia 2010, 65, 283–293. [Google Scholar] [CrossRef]
- Adabag, A.S.; Ishani, A.; Bloomfield, H.E.; Ngo, A.K.; Wilt, T.J. Efficacy of N-acetylcysteine in preventing renal injury after heart surgery: A systematic review of randomized trials. Eur. Heart J. 2009, 30, 1910–1917. [Google Scholar] [CrossRef]
- Sorbello, M.; Morello, G.; Parrinello, L.; Molino, C.; Rinzivillo, D.; Pappalardo, R.; Cutuli, M.; Corona, D.; Veroux, P.; Veroux, M. Effect of N-acetyl-cysteine (NAC) added to fenoldopam or dopamine on end-tidal carbon dioxide and mean arterial pressure at time of renal artery declamping during cadaveric kidney transplantation. Transplant. Proc. 2010, 42, 1056–1060. [Google Scholar] [CrossRef]
- Kuhn, E.W.; Liakopoulos, O.J.; Stange, S.; Deppe, A.C.; Slottosch, I.; Choi, Y.H.; Wahlers, T. Preoperative statin therapy in cardiac surgery: A meta-analysis of 90,000 patients. Eur. J. Cardio-Thorac. Surg. Off. J. Eur. Assoc. Cardio Thorac. Surg. 2014, 45, 17–26, discussion 26. [Google Scholar] [CrossRef]
- Chen, X.; Huang, T.; Cao, X.; Xu, G. Comparative Efficacy of Drugs for Preventing Acute Kidney Injury after Cardiac Surgery: A Network Meta-Analysis. Am. J. Cardiovasc. Drugs 2018, 18, 49–58. [Google Scholar] [CrossRef] [PubMed]
- Tumlin, J.A.; Wang, A.; Murray, P.T.; Mathur, V.S. Fenoldopam mesylate blocks reductions in renal plasma flow after radiocontrast dye infusion: A pilot trial in the prevention of contrast nephropathy. Am. Heart J. 2002, 143, 894–903. [Google Scholar] [CrossRef] [PubMed]
- Caimmi, P.P.; Pagani, L.; Micalizzi, E.; Fiume, C.; Guani, S.; Bernardi, M.; Parodi, F.; Cordero, G.; Fregonara, M.; Kapetanakis, E.; et al. Fenoldopam for renal protection in patients undergoing cardiopulmonary bypass. J. Cardiothorac. Vasc. Anesth. 2003, 17, 491–494. [Google Scholar] [CrossRef] [PubMed]
- Allgren, R.L.; Marbury, T.C.; Rahman, S.N.; Weisberg, L.S.; Fenves, A.Z.; Lafayette, R.A.; Sweet, R.M.; Genter, F.C.; Kurnik, B.R.; Conger, J.D.; et al. Anaritide in acute tubular necrosis. Auriculin Anaritide Acute Renal Failure Study Group. N. Engl. J. Med. 1997, 336, 828–834. [Google Scholar] [CrossRef] [PubMed]
- Coca, S.G.; Yusuf, B.; Shlipak, M.G.; Garg, A.X.; Parikh, C.R. Long-term risk of mortality and other adverse outcomes after acute kidney injury: A systematic review and meta-analysis. Am. J. Kidney Dis. Off. J. Natl. Kidney Found. 2009, 53, 961–973. [Google Scholar] [CrossRef]
- Billings, F.T.t.; Hendricks, P.A.; Schildcrout, J.S.; Shi, Y.; Petracek, M.R.; Byrne, J.G.; Brown, N.J. High-Dose Perioperative Atorvastatin and Acute Kidney Injury Following Cardiac Surgery: A Randomized Clinical Trial. JAMA 2016, 315, 877–888. [Google Scholar] [CrossRef]
- Wahba, A.; Milojevic, M.; Boer, C.; De Somer, F.; Gudbjartsson, T.; van den Goor, J.; Jones, T.J.; Lomivorotov, V.; Merkle, F.; Ranucci, M.; et al. 2019 EACTS/EACTA/EBCP guidelines on cardiopulmonary bypass in adult cardiac surgery. Eur. J. Cardio-Thorac. Surg. Off. J. Eur. Assoc. Cardio Thorac. Surg. 2020, 57, 210–251. [Google Scholar] [CrossRef]
- Khwaja, A. KDIGO clinical practice guidelines for acute kidney injury. Nephron. Clin. Pract. 2012, 120, c179–c184. [Google Scholar] [CrossRef]
- Hillis, L.D.; Smith, P.K.; Anderson, J.L.; Bittl, J.A.; Bridges, C.R.; Byrne, J.G.; Cigarroa, J.E.; Disesa, V.J.; Hiratzka, L.F.; Hutter, A.M., Jr.; et al. 2011 ACCF/AHA Guideline for Coronary Artery Bypass Graft Surgery: A report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation 2011, 124, e652–e735. [Google Scholar] [CrossRef]
- Lazar, H.L.; McDonnell, M.; Chipkin, S.R.; Furnary, A.P.; Engelman, R.M.; Sadhu, A.R.; Bridges, C.R.; Haan, C.K.; Svedjeholm, R.; Taegtmeyer, H.; et al. The Society of Thoracic Surgeons practice guideline series: Blood glucose management during adult cardiac surgery. Ann. Thorac. Surg. 2009, 87, 663–669. [Google Scholar] [CrossRef]
- Joannidis, M.; Druml, W.; Forni, L.G.; Groeneveld, A.B.J.; Honore, P.M.; Hoste, E.; Ostermann, M.; Oudemans-van Straaten, H.M.; Schetz, M. Prevention of acute kidney injury and protection of renal function in the intensive care unit: Update 2017: Expert opinion of the Working Group on Prevention, AKI section, European Society of Intensive Care Medicine. Intensive Care Med. 2017, 43, 730–749. [Google Scholar] [CrossRef] [PubMed]
- La Via, L.; Sangiorgio, G.; Stefani, S.; Marino, A.; Nunnari, G.; Cocuzza, S.; La Mantia, I.; Cacopardo, B.; Stracquadanio, S.; Spampinato, S.; et al. The Global Burden of Sepsis and Septic Shock. Epidemiologia 2024, 5, 456–478. [Google Scholar] [CrossRef] [PubMed]
- Meersch, M.; Schmidt, C.; Hoffmeier, A.; Van Aken, H.; Wempe, C.; Gerss, J.; Zarbock, A. Prevention of cardiac surgery-associated AKI by implementing the KDIGO guidelines in high risk patients identified by biomarkers: The PrevAKI randomized controlled trial. Nat. Rev. Nephrol. 2017, 43, 1551–1561. [Google Scholar] [CrossRef]
- Bellomo, R.; Ronco, C.; Mehta, R.L.; Asfar, P.; Boisramé-Helms, J.; Darmon, M.; Diehl, J.L.; Duranteau, J.; Hoste, E.A.J.; Olivier, J.B.; et al. Acute kidney injury in the ICU: From injury to recovery: Reports from the 5th Paris International Conference. Intensive Care Med. 2017, 7, 49. [Google Scholar] [CrossRef] [PubMed]
- James, M.; Bouchard, J.; Ho, J.; Klarenbach, S.; LaFrance, J.P.; Rigatto, C.; Wald, R.; Zappitelli, M.; Pannu, N. Canadian Society of Nephrology commentary on the 2012 KDIGO clinical practice guideline for acute kidney injury. Am. J. Kidney Dis. Off. J. Natl. Kidney Found. 2013, 61, 673–685. [Google Scholar] [CrossRef]
- Tang, W.H.; Vagelos, R.H.; Yee, Y.G.; Fowler, M.B. Impact of angiotensin-converting enzyme gene polymorphism on neurohormonal responses to high- versus low-dose enalapril in advanced heart failure. Am. Heart J. 2004, 148, 889–894. [Google Scholar] [CrossRef]
- Hou, J.; Pan, Y.; Zhu, D.; Fan, Y.; Feng, G.; Wei, Y.; Wang, H.; Qin, K.; Zhao, T.; Yang, Q.; et al. Targeted delivery of nitric oxide via a ‘bump-and-hole’-based enzyme-prodrug pair. Nat. Chem. Biol. 2019, 15, 151–160. [Google Scholar] [CrossRef]
- Goren, O.; Matot, I. Perioperative acute kidney injury. Br. J. Anaesth. 2015, 115 (Suppl. 2), ii3–ii14. [Google Scholar] [CrossRef]
| Study | N. Patients | Dosing of Fenoldopam | Comparison | Outcomes |
|---|---|---|---|---|
| Cogliati et al. [15] | 193 (95 Fenoldopam; 98 Placebo) | 0.1 mcg/kg/min | Placebo | Fenoldopam prevented AKI in a high-risk population undergoing cardiac surgery |
| Ranucci et al. [39] | 80 (40 Fenoldopam; 40 Placebo) | 0.1 mcg/kg/min | Placebo | Fenoldopam significantly improves renal function and prevents AKI and major morbidity. |
| Barr et al. [32] | 79 (19 Fenoldopam; 20 N-acetylcysteine; 21 Fenoldopam + N-acetylcysteine; 19 Placebo) | 0.1 mcg/kg/min | N-acetylcysteine 600 mg os twice a day | Perioperative Fenoldopam and N-acetylcysteine abrogate the early postoperative decline in renal function of patients who have chronic renal insufficiency |
| Tumlin et al. [22] | 155 (80 Fenoldopam; 75 Placebo) | 0.1 mcg/kg/min | Placebo | Fenoldopam does not reduce the incidence of death or dialysis therapy in intensive care unit patients with early ATN |
| Bove et al. [43] | 667 (338 Fenoldopam; 329 Placebo) | 0.1 mcg/kg/min | Placebo | Fenoldopam did not reduce the need for renal replacement therapy or risk of 30-day mortality, but was associated with increased hypotension |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cuttone, G.; La Via, L.; Misseri, G.; Geraci, G.; Sorbello, M.; Pappalardo, F. Fenoldopam for Renal Protection in Cardiac Surgery: Pharmacology, Clinical Applications, and Evolving Perspectives. J. Clin. Med. 2024, 13, 5863. https://doi.org/10.3390/jcm13195863
Cuttone G, La Via L, Misseri G, Geraci G, Sorbello M, Pappalardo F. Fenoldopam for Renal Protection in Cardiac Surgery: Pharmacology, Clinical Applications, and Evolving Perspectives. Journal of Clinical Medicine. 2024; 13(19):5863. https://doi.org/10.3390/jcm13195863
Chicago/Turabian StyleCuttone, Giuseppe, Luigi La Via, Giovanni Misseri, Giulio Geraci, Massimiliano Sorbello, and Federico Pappalardo. 2024. "Fenoldopam for Renal Protection in Cardiac Surgery: Pharmacology, Clinical Applications, and Evolving Perspectives" Journal of Clinical Medicine 13, no. 19: 5863. https://doi.org/10.3390/jcm13195863







