The SpO2/FiO2 Ratio Combined with Prognostic Scores for Pneumonia and COVID-19 Increases Their Accuracy in Predicting Mortality of COVID-19 Patients
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Setting
2.2. Data Collection
- -
- epidemiological and demographic characteristics,
- -
- medical comorbidities,
- -
- Charlson Comorbidity Index (CCI) [20] on admission,
- -
- days from onset of symptoms to hospitalization,
- -
- days from positive swab to hospitalization,
- -
- days from onset of symptoms to positive swab,
- -
- Pneumonia Severity Index (PSI) [21] on admission,
- -
- -
- National Early Warning Score 2 (NEWS2) [24] on admission,
- -
- -
- hospitalization or outpatient management of Patients with SARS-CoV-2 (HOME-CoV) [26] on admission,
- -
- -
- CAPS-D score [27] on admission,
- -
- SOARS score, abbreviated for SpO2, obesity, age, respiratory rate, and stroke history (SOARS) [28] on admission,
- -
- COVID-19 Severity Index [29] on admission,
- -
- ASCL score, abbreviated for age, sex, CRP at hospital admission, and LDH at hospital admission (ASCL) [30] on admission,
- -
- COVID-19 Early Warning Score (COEWS) [31] on admission,
- -
- National Early Warning Score 2 Plus (NEWS2 Plus) [17] on admission,
- -
- Cascio–Zinna COVID-19-mortality Score (CZ COVID-19) [18] on admission,
- -
- clinical presentation,
- -
- vital signs at first clinical contact (blood pressure, heart rate, oxygen saturation, respiratory rate, body temperature),
- -
- respiratory function,
- -
- laboratory tests,
- -
- imaging,
- -
- oxygen therapy,
- -
- days of hospitalization.
2.3. Statistical Analyses
2.4. Combination of Risk Scores and an Independent Predictor of Mortality
3. Results
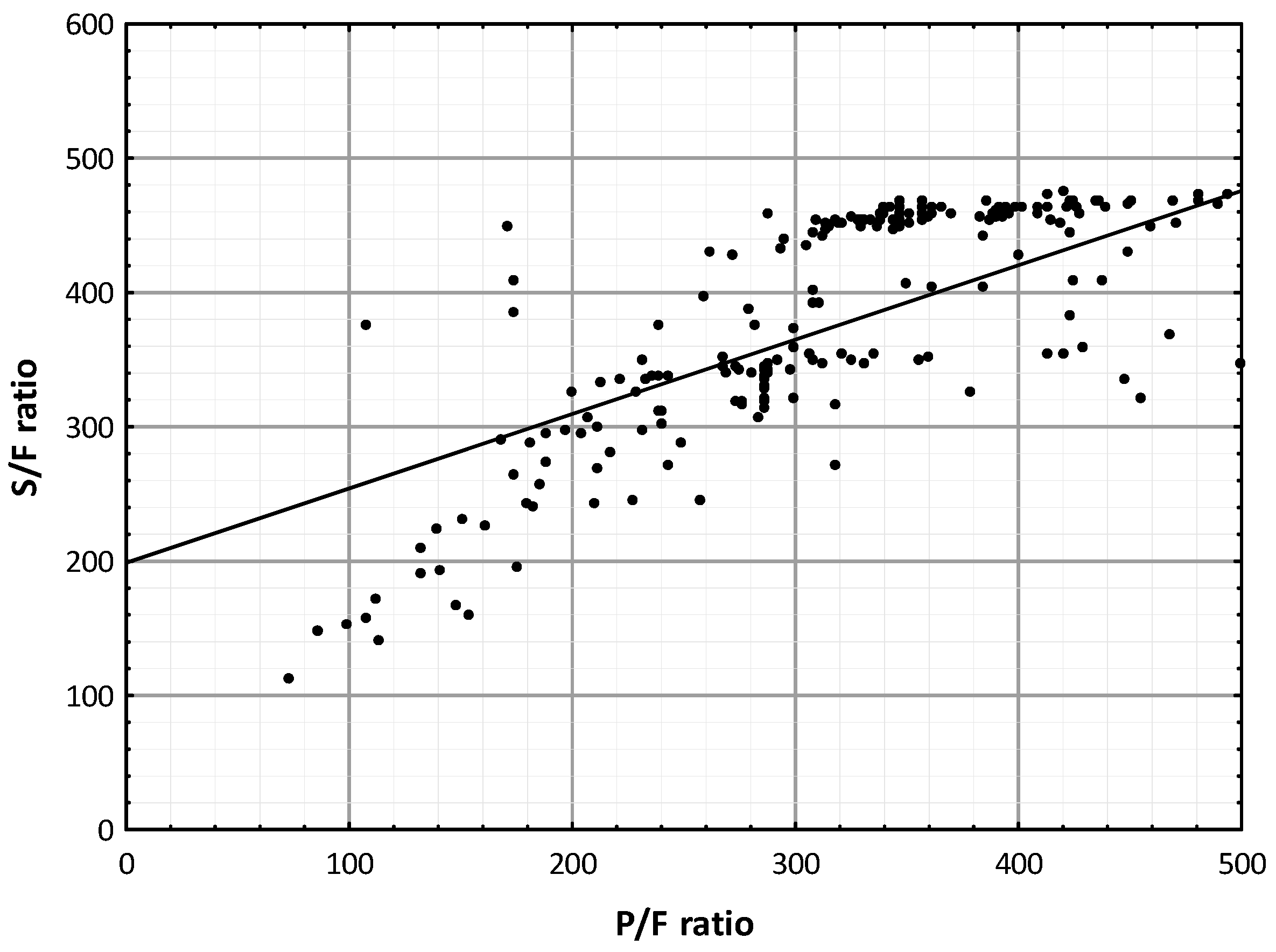
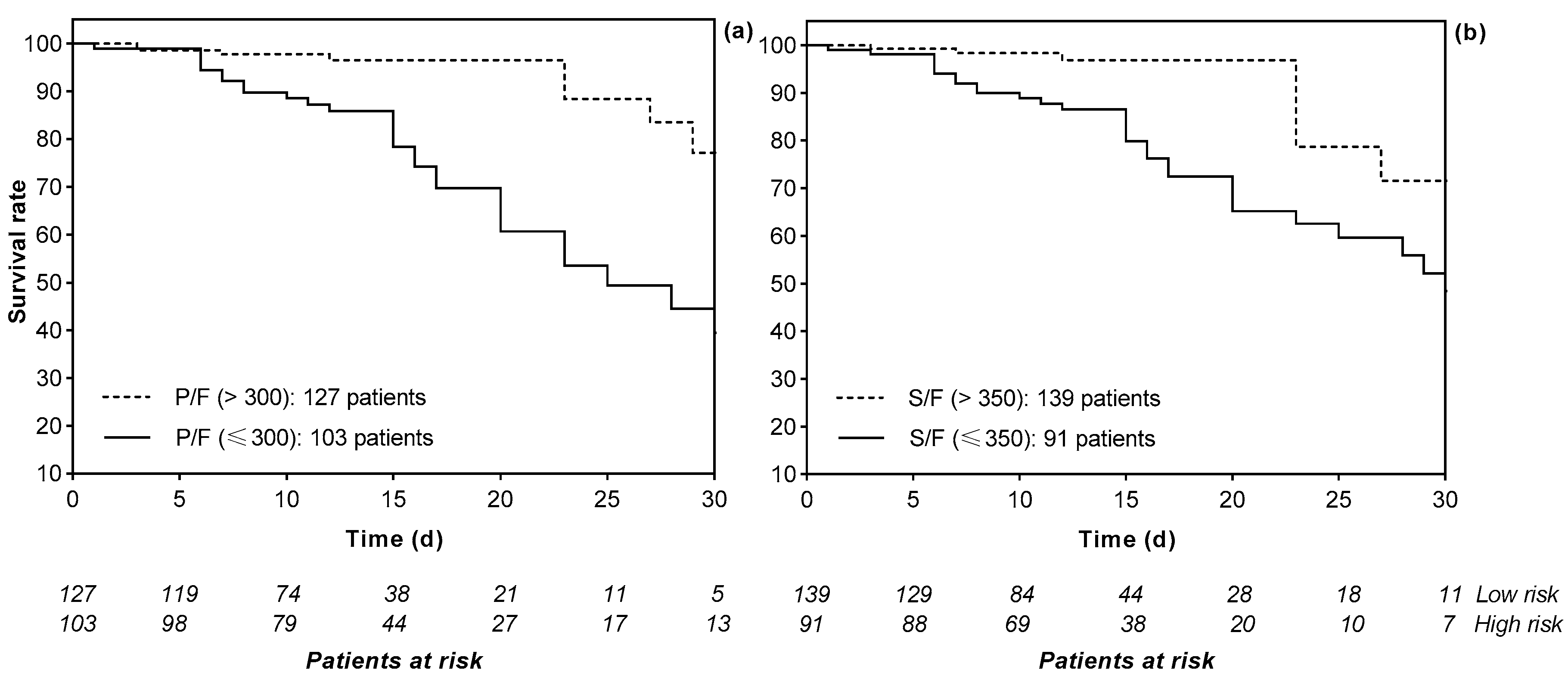
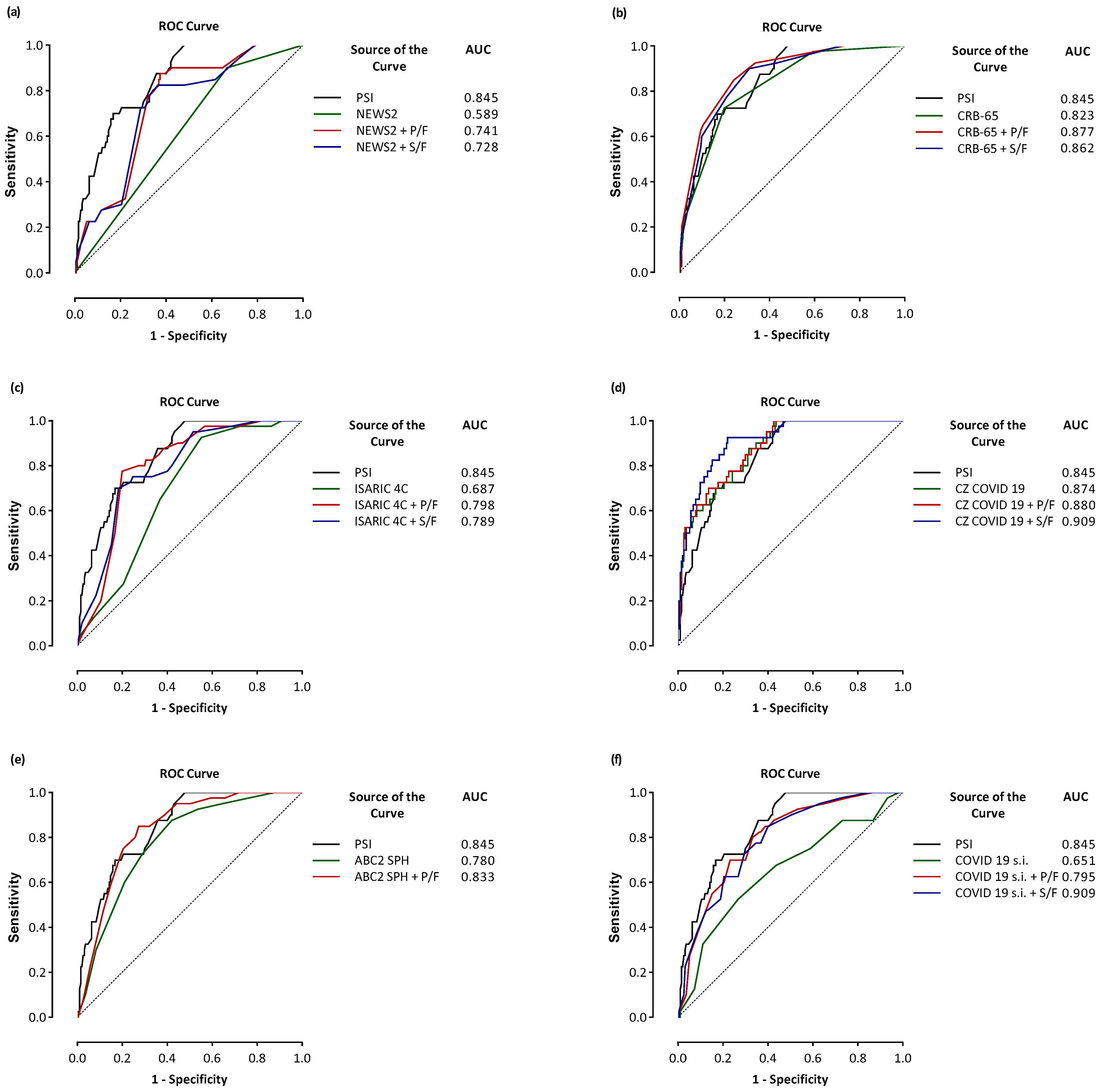
Comparison Scores and Combined Scores with the PaO2/FiO2 or SpO2/FiO2 Ratios
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Acronyms and Abbreviations
References
- Satici, M.O.; Islam, M.M.; Satici, C.; Uygun, C.N.; Ademoglu, E.; Altunok, İ.; Aksel, G.; Eroglu, S.E. The role of a noninvasive index ‘SpO2/FiO2’ in predicting mortality among patients with COVID-19 pneumonia. Am. J. Emerg. Med. 2022, 57, 54–59. [Google Scholar] [CrossRef] [PubMed]
- Abate, S.M.; Ahmed Ali, S.; Mantfardo, B.; Basu, B. Rate of Intensive Care Unit admission and outcomes among patients with coronavirus: A systematic review and Meta-analysis. PLoS ONE 2020, 15, e0235653. [Google Scholar] [CrossRef] [PubMed]
- Knight, S.R.; Ho, A.; Pius, R.; Buchan, I.; Carson, G.; Drake, T.M.; Dunning, J.; Fairfield, C.J.; Gamble, C.; Green, C.A.; et al. Risk stratification of patients admitted to hospital with COVID-19 using the ISARIC WHO Clinical Characterisation Protocol: Development and validation of the 4C Mortality Score. BMJ 2020, 370, m3339. [Google Scholar] [CrossRef]
- Stokes, E.K.; Zambrano, L.D.; Anderson, K.N.; Marder, E.P.; Raz, K.M.; El Burai Felix, S.; Tie, Y.; Fullerton, K.E. Coronavirus Disease 2019 Case Surveillance-United States, January 22–May 30, 2020. Morb. Mortal Wkly. Rep. 2020, 69, 759–765. [Google Scholar] [CrossRef] [PubMed]
- Wu, Z.; McGoogan, J.M. Characteristics of and Important Lessons From the Coronavirus Disease 2019 (COVID-19) Outbreak in China: Summary of a Report of 72,314 Cases from the Chinese Center for Disease Control and Prevention. JAMA 2020, 323, 1239–1242. [Google Scholar] [CrossRef]
- Satici, C.; Demirkol, M.A.; Sargin Altunok, E.; Gursoy, B.; Alkan, M.; Kamat, S.; Demirok, B.; Surmeli, C.D.; Calik, M.; Cavus, Z.; et al. Performance of pneumonia severity index and CURB-65 in predicting 30-day mortality in patients with COVID-19. Int. J. Infect. Dis. 2020, 98, 84–89. [Google Scholar] [CrossRef]
- Su, Y.; Tu, G.W.; Ju, M.J.; Yu, S.J.; Zheng, J.L.; Ma, G.G.; Liu, K.; Ma, J.F.; Yu, K.H.; Xue, Y.; et al. Comparison of CRB-65 and quick sepsis-related organ failure assessment for predicting the need for intensive respiratory or vasopressor support in patients with COVID-19. J. Infect. 2020, 81, 647–679. [Google Scholar] [CrossRef]
- Wibisono, E.; Hadi, U.; Bramantono; Arfijanto, M.V.; Rusli, M.; Rahman, B.E.; Asmarawati, T.P.; Choirunnisa, M.L.; Rahayu, D.R.P. National early warning score (NEWS) 2 predicts hospital mortality from COVID-19 patients. Ann. Med. Surg. 2022, 76, 103462. [Google Scholar] [CrossRef]
- Kumar, A.; Aggarwal, R.; Khanna, P.; Kumar, R.; Singh, A.K.; Soni, K.D.; Trikha, A. Correlation of the SpO2/FiO2 (S/F) ratio and the PaO2/FiO2 (P/F) ratio in patients with COVID-19 pneumonia. Med. Intensiv. (Engl. Ed.) 2022, 46, 408–410. [Google Scholar] [CrossRef]
- Rice, T.W.; Wheeler, A.P.; Bernard, G.R.; Hayden, D.L.; Schoenfeld, D.A.; Ware, L.B.; National Institutes of Health, National Heart, Lung; Blood Institute ARDS Network. Comparison of the SpO2/FiO2 ratio and the PaO2/FIO2 ratio in patients with acute lung injury or ARDS. Chest 2007, 132, 410–417. [Google Scholar] [CrossRef]
- Bilan, N.; Dastranji, A.; Ghalehgolab Behbahani, A. Comparison of the spo2/fio2 ratio and the PaO2/FiO2 ratio in patients with acute lung injury or acute respiratory distress syndrome. J. Cardiovasc. Thorac. Res. 2015, 7, 28–31. [Google Scholar] [CrossRef] [PubMed]
- Festic, E.; Bansal, V.; Kor, D.J.; Gajic, O. U.S. Critical Illness and Injury Trials Group: Lung Injury Prevention Study Investigators (USCIITG–LIPS). SpO2/FiO2 ratio on hospital admission is an indicator of early acute respiratory distress syndrome development among patients at risk. J. Intensive Care Med. 2015, 30, 209–216. [Google Scholar] [CrossRef]
- Carvalho, E.B.; Leite, T.R.S.; Sacramento, R.F.M.; Nascimento, P.R.L.D.; Samary, C.D.S.; Rocco, P.R.M.; Silva, P.L. Rationale and limitations of the SpO2/FiO2 as a possible substitute for PaO2/FiO2 in different preclinical and clinical scenarios. Rev. Bras. Ter. Intensiv. 2022, 34, 185–196. [Google Scholar] [CrossRef]
- Marcolino, M.S.; Pires, M.C.; Ramos, L.E.F.; Silva, R.T.; Oliveira, L.M.; Carvalho, R.L.R.; Mourato, R.L.S.; Sánchez-Montalvá, A.; Raventós, B.; Anschau, F.; et al. ABC2-SPH risk score for in-hospital mortality in COVID-19 patients: Development, external validation and comparison with other available scores. Int. J. Infect. Dis. 2021, 110, 281–308. [Google Scholar] [CrossRef] [PubMed]
- Cimini, C.C.R.; Delfino-Pereira, P.; Pires, M.C.; Ramos, L.E.F.; Gomes, A.G.D.R.; Jorge, A.O.; Fagundes, A.L.; Garcia, B.M.; Pessoa, B.P.; de Carvalho, C.A.; et al. Assessment of the ABC2-SPH risk score to predict invasive mechanical ventilation in COVID-19 patients and comparison to other scores. Front. Med. 2023, 10, 1259055. [Google Scholar] [CrossRef]
- Fumagalli, C.; Rozzini, R.; Vannini, M.; Coccia, F.; Cesaroni, G.; Mazzeo, F.; Cola, M.; Bartoloni, A.; Fontanari, P.; Lavorini, F.; et al. Clinical risk score to predict in-hospital mortality in COVID-19 patients: A retrospective cohort study. BMJ Open 2020, 10, e040729. [Google Scholar] [CrossRef] [PubMed]
- Trongtrakul, K.; Tajarernmuang, P.; Limsukon, A.; Theerakittikul, T.; Niyatiwatchanchai, N.; Surasit, K.; Glunriangsang, P.; Liwsrisakun, C.; Bumroongkit, C.; Pothirat, C.; et al. The National Early Warning Score 2 with Age and Body Mass Index (NEWS2 Plus) to Determine Patients with Severe COVID-19 Pneumonia. J. Clin. Med. 2024, 13, 298. [Google Scholar] [CrossRef]
- Zinna, G.; Pipitò, L.; Colomba, C.; Scichilone, N.; Licata, A.; Barbagallo, M.; Russo, A.; Almasio, P.L.; Coppola, N.; Cascio, A. The Development and Validation of a New Mortality Risk Score. J. Clin. Med. 2024, 13, 1832. [Google Scholar] [CrossRef]
- World Medical Association. World Medical Association Declaration of Helsinki: Ethical principles for medical research involving human subjects. JAMA 2013, 310, 2191–2194. [Google Scholar] [CrossRef]
- Christensen, D.M.; Strange, J.E.; Gislason, G.; Torp-Pedersen, C.; Gerds, T.; Fosbøl, E.; Phelps, M. Charlson Comorbidity Index Score and Risk of Severe Outcome and Death in Danish COVID-19 Patients. J. Gen. Intern. Med. 2020, 35, 2801–2803. [Google Scholar] [CrossRef]
- Ortega, L.; Sierra, M.; Domínguez, J.; Martínez, J.; Matas, L.; Bastart, F.; Galí, N.; Ausina, V. Utility of a pneumonia severity index in the optimization of the diagnostic and therapeutic effort for community-acquired pneumonia. Scand. J. Infect. Dis. 2005, 37, 657–663. [Google Scholar] [CrossRef] [PubMed]
- Keller, K.; Schmitt, V.H.; Sagoschen, I.; Münzel, T.; Espinola-Klein, C.; Hobohm, L. CRB-65 for Risk Stratification and Prediction of Prognosis in Pulmonary Embolism. J. Clin. Med. 2023, 12, 1264. [Google Scholar] [CrossRef] [PubMed]
- McNally, M.; Curtain, J.; O’Brien, K.K.; Dimitrov, B.D.; Fahey, T. Validity of British Thoracic Society guidance (the CRB-65 rule) for predicting the severity of pneumonia in general practice: Systematic review and meta-analysis. Br. J. Gen. Pract. 2010, 60, e42. [Google Scholar] [CrossRef] [PubMed]
- Smith, G.B.; Redfern, O.C.; Pimentel, M.A.; Gerry, S.; Collins, G.S.; Malycha, J.; Prytherch, D.; Schmidt, P.E.; Watkinson, P.J. The National Early Warning Score 2 (NEWS2). Clin. Med. 2019, 19, 260. [Google Scholar] [CrossRef]
- Crocker-Buque, T.; Myles, J.; Brentnall, A.; Gabe, R.; Duffy, S.; Williams, S.; Tiberi, S. Using ISARIC 4C mortality score to predict dynamic changes in mortality risk in COVID-19 patients during hospital admission. PLoS ONE 2022, 17, e0274158. [Google Scholar] [CrossRef]
- Douillet, D.; Riou, J.; Morin, F.; Mahieu, R.; Chauvin, A.; Gennai, S.; Ferrant, L.; Lopez, R.; Sebbane, M.; Plantefeve, G.; et al. Derivation and validation of a risk-stratification model for patients with probable or proven COVID-19 in EDs: The revised HOME-CoV score. Emerg. Med. J. 2024, 41, 218–225. [Google Scholar] [CrossRef]
- Werfel, S.; Jakob, C.E.M.; Borgmann, S.; Schneider, J.; Spinner, C.; Schons, M.; Hower, M.; Wille, K.; Haselberger, M.; Heuzeroth, H.; et al. Development and validation of a simplified risk score for the prediction of critical COVID-19 illness in newly diagnosed patients. J. Med. Virol. 2021, 93, 6703–6713. [Google Scholar] [CrossRef]
- Chua, F.; Vancheeswaran, R.; Draper, A.; Vaghela, T.; Knight, M.; Mogal, R.; Singh, J.; Spencer, L.G.; Thwaite, E.; Mitchell, H.; et al. Early prognostication of COVID-19 to guide hospitalisation versus outpatient monitoring using a point-of-test risk prediction score. Thorax 2021, 76, 696–703. [Google Scholar] [CrossRef] [PubMed]
- Huespe, I.; Carboni Bisso, I.; Di Stefano, S.; Terrasa, S.; Gemelli, N.A.; Las Heras, M. COVID-19 Severity Index: A predictive score for hospitalized patients. Med. Intensiv. (Engl. Ed.) 2022, 46, 98–101. [Google Scholar] [CrossRef]
- Scotto, R.; Lanzardo, A.; Buonomo, A.R.; Pinchera, B.; Cattaneo, L.; Sardanelli, A.; Mercinelli, S.; Viceconte, G.; Perrella, A.; Esposito, V.; et al. A Simple Non-Invasive Score Based on Baseline Parameters Can Predict Outcome in Patients with COVID-19. Vaccines 2022, 10, 2043. [Google Scholar] [CrossRef]
- Klén, R.; Huespe, I.A.; Gregalio, F.A.; Lalueza Blanco, A.L.; Pedrera Jimenez, M.; Garcia Barrio, N.; Valdez, P.R.; Mirofsky, M.A.; Boietti, B.; Gómez-Huelgas, R.; et al. Development and validation of COEWS (COVID-19 Early Warning Score) for hospitalized COVID-19 with laboratory features: A multicontinental retrospective study. Elife 2023, 12, e85618. [Google Scholar] [CrossRef] [PubMed]
- Catoire, P.; Tellier, E.; de la Rivière, C.; Beauvieux, M.C.; Valdenaire, G.; Galinski, M.; Revel, P.; Combes, X.; Gil-Jardiné, C. Assessment of the SpO2/FiO2 ratio as a tool for hypoxemia screening in the emergency department. Am. J. Emerg. Med. 2021, 44, 116–120. [Google Scholar] [CrossRef] [PubMed]
- Pripp, A.H. Pearsons eller Spearmans korrelasjonskoeffisienter [Pearson’s or Spearman’s correlation coefficients]. Tidsskr Nor Laegeforen. 2018, 138. [Google Scholar] [CrossRef] [PubMed]
- DeLong, E.R.; DeLong, D.M.; Clarke-Pearson, D.L. Comparing the areas under two or more correlated receiver operating characteristic curves: A nonparametric approach. Biometrics 1988, 44, 837–845. [Google Scholar] [CrossRef]
- Rich, J.T.; Neely, J.G.; Paniello, R.C.; Voelker, C.C.; Nussenbaum, B.; Wang, E.W. A practical guide to understanding Kaplan-Meier curves. Otolaryngol. Head. Neck Surg. 2010, 143, 331–336. [Google Scholar] [CrossRef]
- Haileamlak, A. The impact of COVID-19 on health and health systems. Ethiop. J. Health Sci. 2021, 31, 1073–1074. [Google Scholar]
- Zadeh Hosseingholi, E.; Maddahi, S.; Jabbari, S.; Molavi, G. Identification of High Death Risk Coronavirus Disease-19 Patients using Blood Tests. Adv. Biomed. Res. 2022, 11, 58. [Google Scholar] [CrossRef]
- Gibson, P.G.; Qin, L.; Puah, S.H. COVID-19 acute respiratory distress syndrome (ARDS): Clinical features and differences from typical pre-COVID-19 ARDS. Med. J. Aust. 2020, 213, 54–56.e1. [Google Scholar] [CrossRef]
- Kadkhodai, L.; Saghaei, M.; Habibzadeh, M.; Alikiaii, B.; Hashemi, S.J. Estimating the best fraction of inspired oxygen for calculation of PaO2/FiO2 ratio in acute respiratory distress syndrome due to COVID-19 pneumonia. J. Res. Med. Sci. 2022, 27, 38. [Google Scholar] [CrossRef]
- Sartini, S.; Massobrio, L.; Cutuli, O.; Campodonico, P.; Bernini, C.; Sartini, M.; Cristina, M.L.; Castellani, L.; Ceschi, L.; Spadaro, M.; et al. Role of SatO2, PaO2/FiO2 Ratio and PaO2 to Predict Adverse Outcome in COVID-19: A Retrospective, Cohort Study. Int. J. Environ. Res. Public Health 2021, 18, 11534. [Google Scholar] [CrossRef]
- Alberdi-Iglesias, A.; Martín-Rodríguez, F.; Ortega Rabbione, G.; Rubio-Babiano, A.I.; Núñez-Toste, M.G.; Sanz-García, A.; Del Pozo Vegas, C.; Castro Villamor, M.A.; Martín-Conty, J.L.; Jorge-Soto, C.; et al. Role of SpO2/FiO2 Ratio and ROX Index in Predicting Early Invasive Mechanical Ventilation in COVID-19. A Pragmatic, Retrospective, Multi-Center Study. Biomedicines 2021, 9, 1036. [Google Scholar] [CrossRef] [PubMed]
- Roozeman, J.P.; Mazzinari, G.; Serpa Neto, A.; Hollmann, M.W.; Paulus, F.; Schultz, M.J.; Pisani, L.; PRoVENT-COVID Collaborative Group. Prognostication using SpO2/FiO2 in invasively ventilated ICU patients with ARDS due to COVID-19-Insights from the PRoVENT-COVID study. J. Crit. Care 2022, 68, 31–37. [Google Scholar] [CrossRef] [PubMed]
- Lu, X.; Jiang, L.; Chen, T.; Wang, Y.; Zhang, B.; Hong, Y.; Wang, J.; Yan, F. Continuously available ratio of SpO2/FiO2 serves as a noninvasive prognostic marker for intensive care patients with COVID-19. Respir. Res. 2020, 21, 194. [Google Scholar] [CrossRef] [PubMed]
- García Clemente, M.M.; Herrero Huertas, J.; Fernández Fernández, A.; De La Escosura Muñoz, C.; Enríquez Rodríguez, A.I.; Pérez Martínez, L.; Gómez Mañas, S.; Iscar Urrutia, M.; López González, F.J.; Madrid Carbajal, C.J.; et al. Assessment of risk scores in COVID-19. Int. J. Clin. Pract. 2021, 75, e13705. [Google Scholar] [CrossRef]
- Chalmers, J.D.; Singanayagam, A.; Akram, A.R.; Mandal, P.; Short, P.M.; Choudhury, G.; Wood, V.; Hill, A.T. Severity assessment tools for predicting mortality in hospitalised patients with community-acquired pneumonia. Systematic review and meta-analysis. Thorax 2010, 65, 878–883. [Google Scholar] [CrossRef]
- Zaki, H.A.; Hamdi Alkahlout, B.; Shaban, E.; Mohamed, E.H.; Basharat, K.; Elsayed, W.A.E.; Azad, A. The Battle of the Pneumonia Predictors: A Comprehensive Meta-Analysis Comparing the Pneumonia Severity Index (PSI) and the CURB-65 Score in Predicting Mortality and the Need for ICU Support. Cureus 2023, 15, e42672. [Google Scholar] [CrossRef]
- Santana, A.R.; Amorim, F.F.; Soares, F.B.; de Souza Godoy, L.G.; de Jesus Almeida, L.; Rodrigues, T.A.; de Andrade Filho, G.M.; Silva, T.A.; da Silva Neto, O.G.; Rocha, P.H.G.; et al. Comparison of CURB-65 and CRB-65 as predictors of death in community-acquired pneumonia in adults admitted to an ICU. Crit. Care 2013, 17 (Suppl. 3), P39. [Google Scholar] [CrossRef]
- Ebell, M.H.; Walsh, M.E.; Fahey, T.; Kearney, M.; Marchello, C. Meta-analysis of Calibration, Discrimination, and Stratum-Specific Likelihood Ratios for the CRB-65 Score. J. Gen. Intern. Med. 2019, 34, 1304–1313. [Google Scholar] [CrossRef] [PubMed]
- Fan, G.; Tu, C.; Zhou, F.; Liu, Z.; Wang, Y.; Song, B.; Gu, X.; Wang, Y.; Wei, Y.; Li, H.; et al. Comparison of severity scores for COVID-19 patients with pneumonia: A retrospective study. Eur. Respir. J. 2020, 56, 2002113. [Google Scholar] [CrossRef]
- Chippa, V.; Aleem, A.; Anjum, F. Post-Acute Coronavirus (COVID-19) Syndrome; StatPearls Publishing: Treasure Island, FL, USA, 2024. [Google Scholar]
- Liang, W.; Liang, H.; Ou, L.; Chen, B.; Chen, A.; Li, C.; Li, Y.; Guan, W.; Sang, L.; Lu, J.; et al. Development and Validation of a Clinical Risk Score to Predict the Occurrence of Critical Illness in Hospitalized Patients With COVID-19. JAMA Intern. Med. 2020, 180, 1081–1089. [Google Scholar] [CrossRef]
- Doğanay, F.; Ak, R. Performance of the CURB-65, ISARIC-4C and COVID-GRAM scores in terms of severity for COVID-19 patients. Int. J. Clin. Pract. 2021, 75, e14759. [Google Scholar] [CrossRef] [PubMed]
- Albahri, A.S.; Hamid, R.A.; Alwan, J.K.; Al-Qays, Z.T.; Zaidan, A.A.; Zaidan, B.B.; Albahri, A.O.S.; AlAmoodi, A.H.; Khlaf, J.M.; Almahdi, E.M.; et al. Role of biological Data Mining and Machine Learning Techniques in Detecting and Diagnosing the Novel Coronavirus (COVID-19): A Systematic Review. J. Med. Syst. 2020, 44, 122. [Google Scholar] [CrossRef] [PubMed]
- Gupta, R.K.; Harrison, E.M.; Ho, A.; Docherty, A.B.; Knight, S.R.; van Smeden, M.; Abubakar, I.; Lipman, M.; Quartagno, M.; Pius, R.; et al. Development and validation of the ISARIC 4C Deterioration model for adults hospitalised with COVID-19: A prospective cohort study. Lancet Respir. Med. 2021, 9, 349–359. [Google Scholar] [CrossRef] [PubMed]
- Alwazzeh, M.J.; Subbarayalu, A.V.; Abu Ali, B.M.; Alabdulqader, R.; Alhajri, M.; Alwarthan, S.M.; AlShehail, B.M.; Raman, V.; Almuhanna, F.A. Performance of CURB-65 and ISARIC 4C mortality scores for hospitalized patients with confirmed COVID-19 infection in Saudi Arabia. Inform. Med. Unlocked 2023, 39, 101269. [Google Scholar] [CrossRef] [PubMed]
- Leening, M.J.; Vedder, M.M.; Witteman, J.C.; Pencina, M.J.; Steyerberg, E.W. Net reclassification improvement: Computation, interpretation, and controversies: A literature review and clinician’s guide. Ann. Intern. Med. 2014, 160, 122–131. [Google Scholar] [CrossRef]
- Kerr, K.F.; Wang, Z.; Janes, H.; McClelland, R.L.; Psaty, B.M.; Pepe, M.S. Net reclassification indices for evaluating risk prediction instruments: A critical review. Epidemiology 2014, 25, 114–121. [Google Scholar] [CrossRef]
- Grunkemeier, G.L.; Jin, R. Net reclassification index: Measuring the incremental value of adding a new risk factor to an existing risk model. Ann. Thorac. Surg. 2015, 99, 388–392. [Google Scholar] [CrossRef]

| Variables | First Cohort (n: 230) | Second Cohort (n: 1357) | ||
|---|---|---|---|---|
| mOR (95% CI) | p-Value | mOR (95% CI) | p-Value | |
| Age (years) | 1.13 (1.127–1.186) | <0.001 | 1.117 (1.093–1.142) | <0.001 |
| Hb (g/dL) | 0.586 (0.462–0.743) | <0.001 | 1.173 (0.951–1.447) | 0.128 |
| WBC (cell/μL) | 3.541 (1.305–9.607) | 0.013 | 1.117 (0.682–1.830) | 0.659 |
| PLT (×103/µL) | 0.111 (0.036–0.345) | <0.001 | 1.581 (0.991–2.521) | 0.054 |
| P/F | 0.994 (0.989–0.999) | 0.022 | 0.990 (0.897–0.993) | <0.001 |
| Value % | NEWS2 ≥ 3 | NEWS2 + P/F n * | NEWS2 + S/F * | CRB-65 ≥ 2 | CRB-65 + P/F * | CRB-65 + S/F * | PSI ≥ IV |
|---|---|---|---|---|---|---|---|
| Sensitivity | 33.2 | 87.5 | 80.0 | 72.5 | 85.0 | 90.0 | 70.0 |
| Specificity | 90.0 | 62.5 | 65.8 | 80.0 | 75.8 | 68.9 | 83.2 |
| NLR | 2.0 | 0.6 | 0.5 | 0.3 | 0.3 | 0.5 | 0.2 |
| PLR | 9.0 | 7.0 | 4.0 | 2.6 | 5.6 | 9.0 | 2.3 |
| NPV | 36.4 | 33.0 | 33.0 | 43.3 | 42.5 | 37.9 | 46.7 |
| PPV | 22.1 | 96.0 | 94.0 | 93.3 | 96.0 | 97.0 | 92.9 |
| 95% CI | 0.550–0.679 | 0.679–0.796 | 0.666–0.784 | 0.702–0.816 | 0.827–0.916 | 0.810–0.903 | 0.706–0.819 |
| p-value | 0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 |
| AUC | 0.616 | 0.741 | 0.728 | 0.763 | 0.877 | 0.862 | 0.766 |
| p-value ** | Reference | <0.001 | <0.001 | Reference | <0.001 | 0.001 | – |
| p-value *** | 0.003 | 0.631 | 0.483 | 0.891 | <0.001 | 0.005 | Reference |
| Scores | Year of Birth | Nation of Birth | Sensitivity (%) | Specificity (%) | AUC | 95% CI | p-Value | p-Value $ | p-Value $$ | p-Value | NRI (p-Value) |
|---|---|---|---|---|---|---|---|---|---|---|---|
| CCI | 1987 | USA | 72.5 | 60.0 | 0.685 | 0.621–0.745 | <0.001 | Reference | 0.001 | – | Reference |
| CCI + P/F * | 75.0 | 78.4 | 0.807 | 0.750–0.856 | <0.001 | 0.001 | 0.398 | 0.012 $$$ | 0.210 (1.613) | ||
| CCI + S/F * | 72.5 | 79.5 | 0.786 | 0.727–0.837 | <0.001 | 0.007 | 0.216 | 0.009 $$$$ | 0.194 (1.181) | ||
| PSI | 1998 | USA | 70.0 | 83.2 | 0.845 | 0.792–0.890 | <0.001 | Reference | Reference | – | Reference |
| PSI + P/F * | 90.0 | 78.4 | 0.887 | 0.838–0.924 | <0.001 | 0.052 | – | Reference $$$ | 0.153 (0.035) | ||
| PSI + S/F * | 87.5 | 75.8 | 0.875 | 0.825–0.915 | <0.001 | 0.162 | – | Reference $$$$ | 0.101 (0.142) | ||
| CRB-65 | 2002 | UK | 72.5 | 80.0 | 0.823 | 0.767–0.870 | <0.001 | Reference | 0.294 | – | Reference |
| CRB-65 + P/F * | 85.0 | 75.8 | 0.877 | 0.827–0.916 | <0.001 | 0.023 | 0.253 | 0.548 $$$ | 0.083 (0.152) | ||
| CRB-65 + S/F * | 90.0 | 68.9 | 0.862 | 0.810–0.903 | <0.001 | 0.019 | 0.572 | 0.057 $$$$ | 0.039 (0.548) | ||
| NEWS2 | 2017 | UK | 90.0 | 33.2 | 0.589 | 0.523–0.653 | 0.061 | Reference | <0.001 | – | Reference |
| NEWS2 + P/F * | 87.5 | 62.6 | 0.741 | 0.679–0.796 | <0.001 | <0.001 | 0.020 | <0.001 $$$ | 0.195 (<0.001) | ||
| NEWS2 + S/F * | 80.0 | 65.8 | 0.728 | 0.666–0.784 | <0.001 | <0.001 | 0.012 | 0.012 $$$$ | 0.226 (<0.001) | ||
| ISARIC 4C | 2020 | UK | 92.5 | 44.7 | 0.687 | 0.623–0.746 | <0.001 | Reference | <0.001 | – | Reference |
| ISARIC 4C + P/F * | 77.5 | 80.0 | 0.798 | 0.740–0.848 | <0.001 | 0.003 | 0.220 | 0.001 $$$ | 0.203 (0.006) | ||
| ISARIC 4C + S/F * | 70.0 | 81.6 | 0.789 | 0.730–0.839 | <0.001 | 0.005 | 0.156 | 0.254 $$$$ | 0.143 (0.043) | ||
| HOME-CoV | 2020 | FR | 90.0 | 40.5 | 0.666 | 0.601–0.727 | <0.001 | Reference | <0.001 | – | Reference |
| HOME-CoV + P/F * | 75.0 | 75.3 | 0.777 | 0.717–0.829 | <0.001 | 0.002 | 0.097 | <0.001 $$$ | 0.223 (0.002) | ||
| HOME-CoV + S/F * | 85.0 | 60.0 | 0.787 | 0.729–0.838 | <0.001 | 0.006 | 0.078 | 0.028 $$$$ | 0.405 (2.887) | ||
| ABC2-SPH | 2021 | ES | 87.5 | 57.9 | 0.780 | 0.721–0.832 | <0.001 | Reference | 0.116 | 0.018 $$$$ | Reference |
| ABC2-SPH + P/F * | 85.0 | 72.6 | 0.833 | 0.778–0.879 | <0.001 | 0.040 | 0.745 | 0.041 $$$ | 0.109 (0.043) | ||
| CAPS-D | 2021 | GER | 57.5 | 83.2 | 0.748 | 0.687–0.803 | <0.001 | Reference | 0.048 | – | Reference |
| CAPS-D + P/F * | 85.0 | 69.5 | 0.813 | 0.756–0.861 | <0.001 | 0.058 | 0.440 | 0.016 $$$ | 0.364 (0.007) | ||
| CAPS-D + S/F * | 82.5 | 72.6 | 0.810 | 0.753–0.858 | <0.001 | 0.085 | 0.396 | 0.039 $$$$ | 0.428 (0.001) | ||
| SOARS | 2021 | UK | 62.5 | 78.9 | 0.759 | 0.699–0.813 | <0.001 | Reference | 0.045 | – | Reference |
| SOARS + P/F * | 72.5 | 78.4 | 0.820 | 0.765–0.868 | <0.001 | 0.003 | 0.527 | 0.029 $$$ | 0.138 (0.040) | ||
| SOARS + S/F * | 67.5 | 80.5 | 0.815 | 0.759–0.863 | <0.001 | 0.005 | 0.454 | 0.036 $$$$ | 0.214 (0.007) | ||
| COVID-19 sever index | 2021 | ARG | 52.5 | 73.2 | 0.651 | 0.586–0.713 | 0.002 | Reference | <0.001 | – | Reference |
| COVID-19 Severity Index + P/F * | 80.0 | 66.8 | 0.795 | 0.737–0.845 | <0.001 | 0.002 | 0.229 | 0.001 $$$ | 0.212 (0.013) | ||
| COVID-19 Severity Index + S/F * | 92.5 | 77.9 | 0.909 | 0.864–0.943 | <0.001 | 0.005 | 0.168 | 0.002 $$$$ | 0.193 (0.039) | ||
| ASCL | 2022 | ITA | 82.5 | 43.7 | 0.669 | 0.604–0.729 | <0.001 | Reference | 0.002 | – | Reference |
| ASCL + P/F * | 85.0 | 63.2 | 0.783 | 0.725–0.835 | <0.001 | 0.005 | 0.158 | 0.001 $$$ | 0.093 (0.003) | ||
| ASCL + S/F * | 75.0 | 70.0 | 0.782 | 0.723–0.834 | <0.001 | 0.010 | 0.151 | 0.004 $$$$ | 0.275 (<0.001) | ||
| COEWS | 2023 | m | 72.5 | 56.3 | 0.658 | 0.593–0.719 | 0.001 | Reference | 0.001 | – | Reference |
| COEWS + P/F * | 95.0 | 55.8 | 0.783 | 0.724–0.834 | <0.001 | 0.005 | 0.148 | 0.001 $$$ | 0.311 (0.016) | ||
| COEWS + S/F * | 85.0 | 60.0 | 0.787 | 0.729–0.838 | <0.001 | 0.009 | 0.129 | 0.003 $$$$ | 0.307 (0.012) | ||
| NEWS2 Plus | 2024 | TH | 85.0 | 42.1 | 0.640 | 0.575–0.702 | 0.001 | Reference | <0.001 | – | Reference |
| NEWS2 Plus + P/F * | 85.0 | 66.8 | 0.766 | 0.705–0.819 | <0.001 | 0.001 | 0.063 | 0.001 $$$ | 0.395 (3.289) | ||
| NEWS2 Plus + S/F * | 80.0 | 67.4 | 0.752 | 0.691–0.806 | <0.001 | 0.002 | 0.035 | 0.001 $$$$ | 0.300 (<0.001) | ||
| CZ COVID-19 | 2024 | ITA | 100 | 56.3 | 0.874 | 0.824–0.914 | <0.001 | Reference | 0.427 | – | Reference |
| CZ COVID-19 + P/F * | 100 | 57.4 | 0.880 | 0.831–0.919 | <0.001 | 0.011 | 0.333 | 0.842 $$$ | 0.011 (0.157) | ||
| CZ COVID-19 + S/F * | 92.5 | 77.9 | 0.909 | 0.864–0.943 | <0.001 | 0.036 | 0.068 | 0.249 $$$$ | 0.160 (<0.001) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zinna, G.; Pipitò, L.; Colomba, C.; Scichilone, N.; Licata, A.; Barbagallo, M.; Russo, A.; Coppola, N.; Cascio, A. The SpO2/FiO2 Ratio Combined with Prognostic Scores for Pneumonia and COVID-19 Increases Their Accuracy in Predicting Mortality of COVID-19 Patients. J. Clin. Med. 2024, 13, 5884. https://doi.org/10.3390/jcm13195884
Zinna G, Pipitò L, Colomba C, Scichilone N, Licata A, Barbagallo M, Russo A, Coppola N, Cascio A. The SpO2/FiO2 Ratio Combined with Prognostic Scores for Pneumonia and COVID-19 Increases Their Accuracy in Predicting Mortality of COVID-19 Patients. Journal of Clinical Medicine. 2024; 13(19):5884. https://doi.org/10.3390/jcm13195884
Chicago/Turabian StyleZinna, Giuseppe, Luca Pipitò, Claudia Colomba, Nicola Scichilone, Anna Licata, Mario Barbagallo, Antonio Russo, Nicola Coppola, and Antonio Cascio. 2024. "The SpO2/FiO2 Ratio Combined with Prognostic Scores for Pneumonia and COVID-19 Increases Their Accuracy in Predicting Mortality of COVID-19 Patients" Journal of Clinical Medicine 13, no. 19: 5884. https://doi.org/10.3390/jcm13195884










