Novel Biomarkers of Grade I Left Ventricular Diastolic Dysfunction in Type 2 Diabetes Patients with Metabolic-Dysfunction-Associated Steatotic Liver Disease
Abstract
:1. Introduction
2. Materials and Methodology
2.1. Study Design and Patients
2.2. Laboratory Tests and Clinical Examinations
2.3. Echocardiac Ultrasound Protocol
2.4. Definitions and Outcomes
2.5. Statistical Analysis
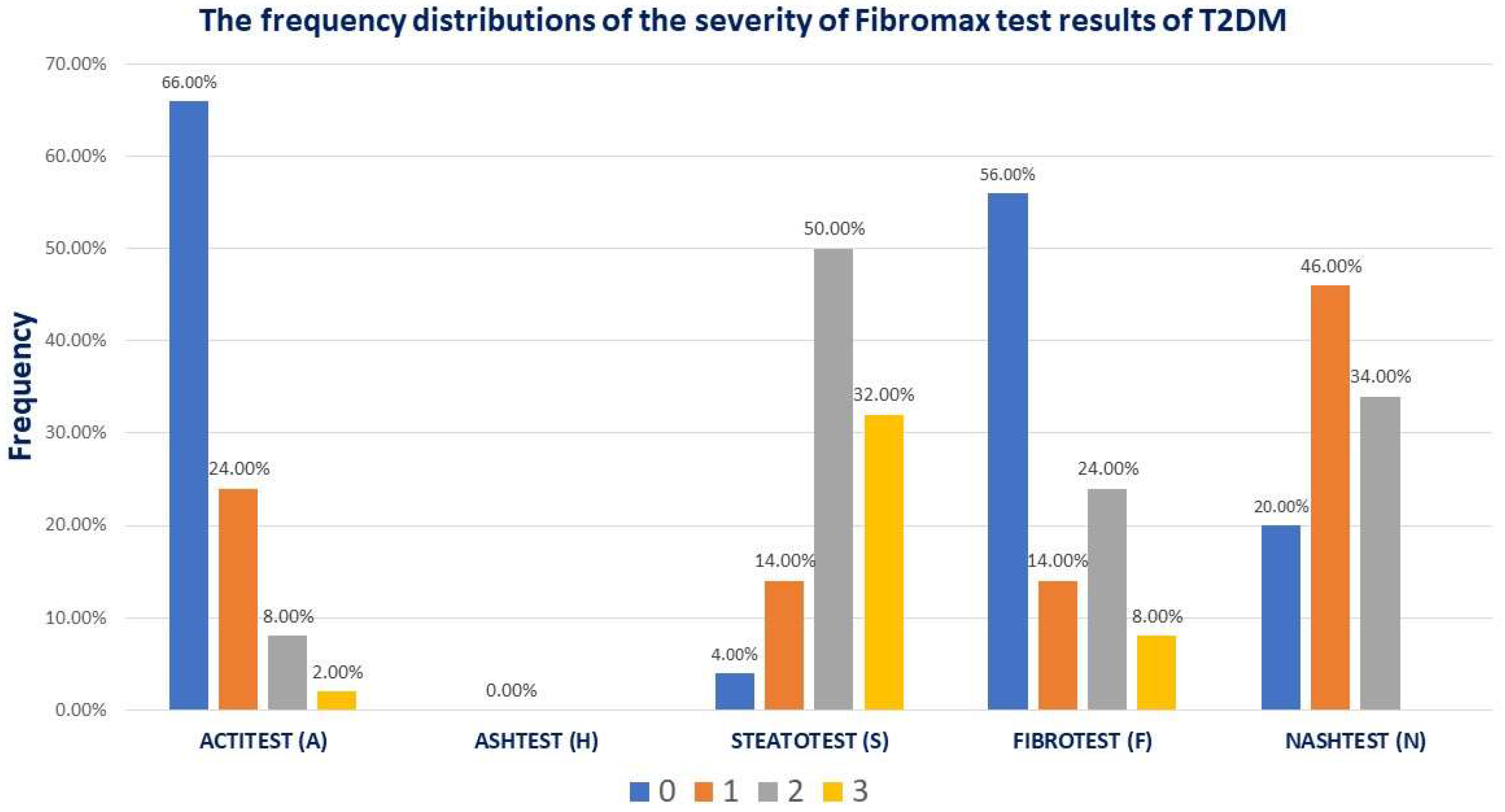
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- International Diabetes Federation. IDF Diabetes Atlas, 10th ed.; International Diabetes Federation: Brussels, Belgium, 2021; Available online: https://www.diabetesatlas.org (accessed on 5 August 2024).
- Albai, O.; Braha, A.; Timar, B.; Sima, A.; Deaconu, L.; Timar, R. Assessment of the Negative Factors for the Clinical Outcome in Patients with SARS-CoV-2 Infection and Type 2 Diabetes Mellitus. Diabetes Metab. Syndr. Obes. 2024, 17, 271–282. [Google Scholar] [CrossRef] [PubMed]
- Forumul Roman de Diabet. Barometrul Privind Diabetul Zaharat în România Romania. 2023. Available online: https://www.forumdiabet.ro/ (accessed on 5 August 2024).
- Zaharia, O.P.; Strassburger, K.; Strom, A.; Bönhof, G.J.; Karusheva, Y.; Antoniou, S.; Bódis, K.; Markgraf, D.F.; Burkart, V.; Müssig, K.; et al. German Diabetes Study Group. Risk of diabetes-associated diseases in subgroups of patients with recent-onset diabetes: A 5-year follow-up study. Lancet Diabetes Endocrinol. 2019, 7, 684–694. [Google Scholar] [CrossRef] [PubMed]
- Khan, J.; Shaw, S. Risk of cataract and glaucoma among older persons with diabetes in India: A cross-sectional study based on LASI, Wave-1. Sci. Rep. 2023, 13, 11973. [Google Scholar] [CrossRef] [PubMed]
- Gonzalez-Manzanares, R.; Anguita-Gámez, M.; Muñiz, J.; Barrios, V.; Gimeno-Orna, J.A.; Pérez, A.; Rodríguez-Padial, L.; Anguita, M.; on behalf of the DIABETIC-IC Study Investigators. Prevalence and incidence of heart failure in type 2 diabetes patients: Results from a nationwide prospective cohort-the DIABET-IC study. Cardiovasc. Diabetol. 2024, 23, 253. [Google Scholar] [CrossRef] [PubMed]
- Shuvo, S.D.; Hossen, M.T.; Riazuddin, M.; Hossain, M.S.; Mazumdar, S.; Parvin, R.; Elahi, M.T. Prevalence of comorbidities and its associated factors among type-2 diabetes patients: A hospital-based study in Jashore District, Bangladesh. BMJ Open 2023, 13, e076261. [Google Scholar] [CrossRef]
- Messina, R.; Mezuk, B.; Rosa, S.; Iommi, M.; Fantini, M.P.; Lenzi, J.; Di Bartolo, P. Age of type 2 diabetes onset as a risk factor for dementia: A 13-year retrospective cohort study. Diabetes Res. Clin. Pract. 2024, 213, 111760. [Google Scholar] [CrossRef]
- Lindblad, P.; Chow, W.H.; Chan, J.; Bergström, A.; Wolk, A.; Gridley, G.; McLaughlin, J.K.; Nyrén, O.; Adami, H.O. The role of diabetes mellitus in the aetiology of renal cell cancer. Diabetologia 1999, 42, 107–112. [Google Scholar] [CrossRef]
- Balasubramanyam, M. Diabetic oncopathy—One more yet another deadly diabetic complication! Indian J. Med. Res. 2014, 140, 15–18. [Google Scholar]
- Roman, D.; Saftescu, S.; Timar, B.; Avram, V.; Braha, A.; Negru, Ș.; Bercea, A.; Serbulescu, M.; Popovici, D.; Timar, R. Diabetes Mellitus and Other Predictors for the Successful Treatment of Metastatic Colorectal Cancer: A Retrospective Study. Medicina 2022, 58, 872. [Google Scholar] [CrossRef]
- Săftescu, S.; Popovici, D.; Oprean, C.; Negru, A.; Croitoru, A.; Zemba, M.; Yasar, I.; Preda, M.; Negru, Ș. Endurance of erythrocyte series in chemotherapy. Exp. Ther. Med. 2020, 20, 214. [Google Scholar] [CrossRef]
- Popovici, D.; Stanisav, C.; Pricop, M.; Dragomir, R.; Saftescu, S.; Ciurescu, D. Associations between Body Mass Index and Prostate Cancer: The Impact on Progression-Free Survival. Medicina 2023, 59, 289. [Google Scholar] [CrossRef] [PubMed]
- Cristea, C. Evidenţa Evoluţiei Diabetului Zaharat în Perioada 2012–2021; Ministerul Sănătăţii. Institutul Naţional de Sănătate Publică Centrul Naţional de Statistică în Sănătate Publică: Bucuresti, Romania, 2022. [Google Scholar]
- American Diabetes Association. Summary of Revisions: Standards of Care in Diabetes—2024. Diabetes Care 2023, 47 (Suppl. S1), S5–S10. [Google Scholar]
- Bui, A.L.; Horwich, T.B.; Fonarow, G.C. Epidemiology and risk profile of heart failure. Nat. Rev. Cardiol. 2011, 8, 30–41. [Google Scholar] [CrossRef] [PubMed]
- Dunlay, S.M.; Givertz, M.M.; Aguilar, D.; Allen, L.A.; Chan, M.; Desai, A.S.; Deswal, A.; Dickson, V.V.; Kosiborod, M.N.; Lekavich, C.L.; et al. Type 2 Diabetes Mellitus and Heart Failure: A Scientific Statement From the American Heart Association and the Heart Failure Society of America: This statement does not represent an update of the 2017 ACC/AHA/HFSA heart failure guideline update. Circulation 2019, 140, e294–e324. [Google Scholar] [CrossRef] [PubMed]
- Yan, T.; Zhu, S.; Yin, X.; Xie, C.; Xue, J.; Zhu, M.; Weng, F.; Zhu, S.; Xiang, B.; Zhou, X.; et al. Burden, Trends, and Inequalities of Heart Failure Globally, 1990 to 2019: A Secondary Analysis Based on the Global Burden of Disease 2019 Study. J. Am. Hear. Assoc. 2023, 12, e027852. [Google Scholar] [CrossRef]
- Gómez-Perez, A.M.; Damas-Fuentes, M.; Cornejo-Pareja, I.; Tinahones, F.J. Heart Failure in Type 1 Diabetes: A Complication of Concern? A Narrative Review. J. Clin. Med. 2021, 10, 4497. [Google Scholar] [CrossRef]
- Ng, L.L.; Sandhu, J.K.; Squire, I.B.; Davies, J.E.; Jones, D.J. Vitamin D and prognosis in acute myocardial infarction. Int. J. Cardiol. 2013, 168, 2341–2346. [Google Scholar] [CrossRef]
- Bozkurt, B.; Coats, A.J.S.; Tsutsui, H.; Abdelhamid, C.M.; Adamopoulos, S.; Albert, N.; Anker, S.D.; Atherton, J.; Böhm, M.; Butler, J.; et al. Universal definition and classification of heart failure: A report of the Heart Failure Society of America, Heart Failure Association of the European Society of Cardiology, Japanese Heart Failure Society and Writing Committee of the Universal Definition of Heart Failure: Endorsed by the Canadian Heart Failure Society, Heart Failure Association of India, Cardiac Society of Australia and New Zealand, and Chinese Heart Failure Association. Eur. J. Heart Fail. 2021, 23, 352–380. [Google Scholar]
- Bouthoorn, S.; Gohar, A.; Valstar, G.; den Ruijter, H.M.; Reitsma, J.B.; Hoes, A.W.; Rutten, F.H. Prevalence of left ventricular systolic dysfunction and heart failure with reduced ejection fraction in men and women with type 2 diabetes mellitus: A systematic review and meta-analysis. Cardiovasc. Diabetol. 2018, 17, 58. [Google Scholar] [CrossRef]
- Bouthoorn, S.; Valstar, G.B.; Gohar, A.; Ruijter, H.M.D.; Reitsma, H.B.; Hoes, A.W.; Rutten, F.H. The prevalence of left ventricular diastolic dysfunction and heart failure with preserved ejection fraction in men and women with type 2 diabetes: A systematic review and meta-analysis. Diab. Vasc. Dis. Res. 2018, 15, 477–493. [Google Scholar] [CrossRef]
- Hoek, A.G.; Canto, E.D.; Wenker, E.; Bindraban, N.; Handoko, M.L.; Elders, P.J.M.; Beulens, J.W.J. Epidemiology of heart failure in diabetes: A disease in disguise. Diabetologia 2024, 67, 574–601. [Google Scholar] [CrossRef]
- Paulus, W.J.; Tschöpe, C. A novel paradigm for heart failure with preserved ejection fraction: Comorbidities drive myocardial dysfunction and remodeling through coronary microvascular endothelial inflammation. J. Am. Coll. Cardiol. 2013, 62, 263–271. [Google Scholar] [CrossRef] [PubMed]
- Abdallah, L.R.; de Matos, R.C.; e Souza, Y.P.D.M.; Vieira-Soares, D.; Muller-Machado, G.; Pollo-Flores, P. Nonalcoholic Fatty Liver Disease and Its Links with Inflammation and Atherosclerosis. Curr. Atheroscler. Rep. 2020, 22, 7. [Google Scholar] [CrossRef] [PubMed]
- Chang, W.; Wang, Y.; Sun, L.; Yu, D.; Li, Y.; Li, G. Evaluation of left atrial function in type 2 diabetes mellitus patients with nonalcoholic fatty liver disease by two-dimensional speckle tracking echocardiography. Echocardiography 2019, 36, 1290–1297. [Google Scholar] [CrossRef] [PubMed]
- Eslam, M.; Newsome, P.N.; Sarin, S.K.; Anstee, Q.M.; Targher, G.; Romero-Gomez, M.; Zelber-Sagi, S.; Wong, V.W.-S.; Dufour, J.-F.; Schattenberg, J.M.; et al. A new definition for metabolic dysfunction-associated fatty liver disease: An international expert consensus statement. J. Hepatol. 2020, 73, 202–209. [Google Scholar] [CrossRef]
- Eslam, M.; Sanyal, A.J.; George, J. MAFLD: A Consensus-Driven Proposed Nomenclature for Metabolic Associated Fatty Liver Disease. Gastroenterology 2020, 158, 1999–2014.e1. [Google Scholar] [CrossRef]
- Younossi, Z.M.; Rinella, M.E.; Sanyal, A.J.; Harrison, S.A.; Brunt, E.M.; Goodman, Z.; Cohen, D.E.; Loomba, R. From NAFLD to MAFLD: Implications of a Premature Change in Terminology. Hepatology 2021, 73, 1194–1198. [Google Scholar] [CrossRef]
- Peng, D.; Yu, Z.; Wang, M.; Shi, J.; Sun, L.; Zhang, Y.; Zhao, W.; Chen, C.; Tang, J.; Wang, C.; et al. Association of Metabolic Dysfunction-Associated Fatty Liver Disease with Left Ventricular Diastolic Function and Cardiac Morphology. Front. Endocrinol. 2022, 13, 935390. [Google Scholar] [CrossRef]
- Anstee, Q.M.; Mantovani, A.; Tilg, H.; Targher, G. Risk of cardiomyopathy and cardiac arrhythmias in patients with nonalcoholic fatty liver disease. Nat. Rev. Gastroenterol. Hepatol. 2018, 15, 425–439. [Google Scholar] [CrossRef]
- Yong, J.N.; Ng, C.H.; Lee, C.W.; Chan, Y.Y.; Tang, A.S.P.; Teng, M.; Tan, D.J.H.; Lim, W.H.; Quek, J.; Xiao, J.; et al. Nonalcoholic fatty liver disease association with structural heart, systolic and diastolic dysfunction: A meta-analysis. Hepatol. Int. 2022, 16, 269–281. [Google Scholar] [CrossRef]
- Di Minno, M.N.; Di Minno, A.; Ambrosino, P.; Songia, P.; Tremoli, E.; Poggio, P. Aortic valve sclerosis as a marker of atherosclerosis: Novel insights from hepatic steatosis. Int. J. Cardiol. 2016, 217, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Mantovani, A.; Dauriz, M.; Sandri, D.; Bonapace, S.; Zoppini, G.; Tilg, H.; Byrne, C.D.; Targher, G. Association between nonalcoholic fatty liver disease and risk of atrial fibrillation in adult individuals: An updated meta-analysis. Liver Int. 2019, 39, 758–769. [Google Scholar] [CrossRef]
- Cai, X.; Zheng, S.; Liu, Y.; Zhang, Y.; Lu, J.; Huang, Y. Nonalcoholic fatty liver disease is associated with increased risk of atrial fibrillation. Liver Int. 2020, 40, 1594–1600. [Google Scholar] [CrossRef] [PubMed]
- Mantovani, A.; Petracca, G.; Csermely, A.; Beatrice, G.; Bonapace, S.; Rossi, A.; Tilg, H.; Byrne, C.D.; Targher, G. Nonalcoholic fatty liver disease and risk of new-onset heart failure: An updated meta-analysis of about 11 million individuals. Gut 2022, 72, 372–380. [Google Scholar] [CrossRef] [PubMed]
- Gohil, N.V.; Tanveer, N.; Makkena, V.K.; Jaramillo, A.P.; Awosusi, B.L.; Ayyub, J.; Dabhi, K.N.; Nath, T.S. Nonalcoholic Fatty Liver Disease and Its Association With Left Ventricular Diastolic Dysfunction: A Systematic Review. Cureus 2023, 15, e43013. [Google Scholar] [PubMed]
- Samouda, H.; Dutour, A.; Chaumoitre, K.; Panuel, M.; Dutour, O.; Dadoun, F. VAT = TAAT-SAAT: Innovative anthropometric model to predict visceral adipose tissue without resort to CT-Scan or, D.X.A. Obesity 2013, 21, E41–E50. [Google Scholar] [CrossRef]
- Esaote SpA. *MyLabX8 eXP*. Via Enrico Melen 77 G, Italy. 2021.
- Goff, D.C., Jr.; Lloyd-Jones, D.M.; Bennett, G.; Coady, S.; D’Agostino, R.B.; Gibbons, R.; Greenland, P.; Lackland, D.T.; Levy, D.; O’Donnell, C.J.; et al. 2013 ACC/AHA guideline on the assessment of cardiovascular risk: A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation 2014, 129, S49–S73. [Google Scholar] [CrossRef]
- Arnett, D.K.; Blumenthal, R.S.; Albert, M.A.; Buroker, A.B.; Goldberger, Z.D.; Hahn, E.J.; Himmelfarb, C.D.; Khera, A.; Lloyd-Jones, D.; McEvoy, J.W.; et al. 2019 ACC/AHA Guideline on the Primary Prevention of Cardiovascular Disease: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation 2019, 140, e596–e646. [Google Scholar] [CrossRef]
- Nagueh, S.F.; Smiseth, O.A.; Appleton, C.P.; Byrd, B.F., 3rd; Dokainish, H.; Edvardsen, T.; Flachskampf, F.A.; Gillebert, T.C.; Klein, A.L.; Lancellotti, P.; et al. Recommendations for the Evaluation of Left Ventricular Diastolic Function by Echocardiography: An Update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J. Am. Soc. Echocardiogr. 2016, 29, 277–314. [Google Scholar] [CrossRef]
- Lazarus, J.V.; Newsome, P.N.; Francque, S.M.; Kanwal, F.; Terrault, N.A.; Rinella, M.E. A multisociety Delphi consensus statement on new fatty liver disease nomenclature. J. Hepatol. 2023, 79, 1542–1556. [Google Scholar] [CrossRef]
- Morra, R.; Munteanu, M.; Imbert-Bismut, F.; Messous, D.; Ratziu, V.; Poynard, T. FibroMAX™: Towards a new universal biomarker of liver disease? Expert Rev. Mol. Diagn. 2007, 7, 481–490. [Google Scholar] [CrossRef] [PubMed]
- MedCalc® Statistical Software; Version 22.016; MedCalc Software Ltd.: Ostend, Belgium, 2023.
- Braha, A.; Albai, A.; Timar, B.; Cipu, D.; Vasiluță, L.; Potre, O.; Timar, R. Predictors of Epicardial Fat Volume Decrease after Dapagliflozin Treatment in Patients with Type 2 Diabetes. Medicina 2021, 58, 21. [Google Scholar] [CrossRef] [PubMed]
- Cohen, J.B.; Schrauben, S.J.; Zhao, L.; Basso, M.D.; Cvijic, M.E.; Li, Z.; Yarde, M.; Wang, Z.; Bhattacharya, P.T.; Chirinos, D.A.; et al. Clinical Phenogroups in Heart Failure with Preserved Ejection Fraction: Detailed Phenotypes, Prognosis, and Response to Spironolactone. JACC Heart Fail. 2020, 8, 172–184. [Google Scholar] [CrossRef] [PubMed]
- Andus, T.; Gross, V.; Tran-Thi, T.A.; Schreiber, G.; Nagashima, M.; Heinrich, P.C. The biosynthesis of acute-phase proteins in primary cultures of rat hepatocytes. Eur. J. Biochem. 1983, 133, 561–571. [Google Scholar] [CrossRef]
- Shimomura, R.; Nezu, T.; Hosomi, N.; Aoki, S.; Sugimoto, T.; Kinoshita, N.; Araki, M.; Takahashi, T.; Maruyama, H.; Matsumoto, M. Alpha-2-macroglobulin as a Promising Biological Marker of Endothelial Function. J. Atheroscler. Thromb. 2018, 25, 350–358. [Google Scholar] [CrossRef]
- de Laat-Kremers, R.; Costanzo, S.; Yan, Q.; Di Castelnuovo, A.; De Curtis, A.; Cerletti, C.; de Gaetano, G.; Donati, M.B.; de Laat, B.; Iacoviello, L. High alpha-2-macroglobulin levels are a risk factor for cardiovascular disease events: A Moli-sani cohort study. Thromb Res. 2024, 234, 94–100. [Google Scholar] [CrossRef]
- Mokou, M.; Lygirou, V.; Vlahou, A.; Mischak, H. Proteomics in cardiovascular disease: Recent progress and clinical implication and implementation. Expert Rev. Proteom. 2017, 14, 117–136. [Google Scholar] [CrossRef]
- Karakasis, P.; Pamporis, K.; Stachteas, P.; Patoulias, D.; Bougioukas, K.I.; Fragakis, N. Efficacy and safety of sodium-glucose cotransporter-2 inhibitors in heart failure with mildly reduced or preserved ejection fraction: An overview of 36 systematic reviews. Heart Fail. Rev. 2023, 28, 1033–1051. [Google Scholar] [CrossRef]

| Variable | Overall | Women (n = 27) | Men (n = 23) | p a |
|---|---|---|---|---|
| Age a (years) | 58.0 ± 11.3 | 57.5 ± 11.5 | 58.6 ± 11.2 | 0.7 |
| Diabetes duration a (years) | 7.0 (4.2; 15.0) | 8 (21.2) | 7 (22.8) | 0.6 |
| Abdominal waist a (cm) | 116.0 ± 11.0 | 115 (22.4) | 116 (27.1) | 0.2 |
| Hip waist a (cm) | 107.5 ± 11.6 | 106 (25.7) | 105 (22.1) | 0.3 |
| BMI a (kg/m2) | 34.4 ± 5.9 | 35.2 (25.5) | 33.3 (25.4) | 0.9 |
| VAT a (cm2) | 75.7 ± 45.1 | 55.7 (20.7) | 95.7 (31.1) | 0.01 |
| FG a (mg/dL) | 150.7 ± 42.3 | 143 (22.4) | 158 (29.1) | 0.1 |
| HbA1c a (%) | 7.9 ± 1.5 | 7.9 (22.5) | 8.1 (25.7) | 0.4 |
| Haptoglobin a | 1.7 ± 0.5 | 1.6 (25) | 1.6 (25.9) | 0.8 |
| α2 Macroglobulin a | 2.0 ± 0.6 | 2 (26.6) | 1.9 (24.1) | 0.5 |
| Apo A1 a | 1.4 (1.3; 1.6) | 1.5 (29.7) | 1.3 (20.5) | 0.02 |
| TG a (mg/dL) | 162.0 (130.2; 252.2) | 153 (25) | 157 (26) | 0.8 |
| TC a (mg/dL) | 177.6 ± 49.8 | 170 (29.2) | 135 (21.1) | 0.04 |
| HDLc a (mg/dL) | 43.0 (36.8; 51.7) | 46 (28.8) | 40.9 (20.2) | 0.03 |
| LDLc a (mg/dL) | 100.7 ± 40.9 | 109 (28.6) | 85 (19.1) | 0.01 |
| Uric Acid a (mg/dL) | 5.5 ± 1.2 | 5.5 (23.5) | 5.5 (25.7) | 0.5 |
| eGFR a (mL/min) | 87.6 ± 20.7 | 84.1 (16.6) | 88.2 (21.1) | 0.2 |
| Serum creatinine a (mg/dL) | 0.7 (0.6; 0.9) | 0.7 (21.3) | 0.9 (30.3) | 0.02 |
| UACr a (mg/g) | 10.7 (3.9; 41.6) | 11.1 (19.8) | 6.1 (16.2) | 0.3 |
| ALT a (u/L) | 29.0 (23.0; 39.0) | 26 (22.3) | 32 (29.2) | 0.09 |
| AST a (u/L) | 20.0 (15.0; 24.0) | 20 (24.7) | 20 (26.3) | 0.7 |
| TB a | 0.5 (0.4; 0.6) | 0.4 (22.4) | 0.5 (29) | 0.1 |
| FAL a | 76.5 (67.0; 100.0) | 87 (19.5) | 76 (15.2) | 0.2 |
| GGT a | 31.0 (20.0; 41.0) | 30 (25.4) | 32 (25.5) | 0.9 |
| EAT b (mm) | 4.0 (3.4; 4.7) | 4 ± 1.5 | 4.3 ± 1.7 | 0.6 |
| TAPSE a (cm) | 2.6 (2.3; 2.9) | 2.5 (20) | 2.6 (21.1) | 0.7 |
| GLS a (%) | 15.9 (14.5; 18.0) | 17.4 (11.5) | 14.2 (5.4) | 0.02 |
| LVEF a (%) | 57.0 (50.6; 60.5) | 56 (21.1) | 58 (24.2) | 0.4 |
| LA a (cm) | 3.7 ± 0.5 | 3.6 (19.7) | 3.8 (25.1) | 0.1 |
| MV s′ lateral wall a (cm/s) | 8.5 (7.0; 10.0) | 8 (19.7) | 9 (23.8) | 0.2 |
| MV s′ septum a (cm/s) | 7.0 (6.0; 8.0) | 7 (20.9) | 7.5 (23.5) | 0.4 |
| DTE a (ms) | 205.0 (188.2; 240.7) | 204 (21) | 207 (21) | 1 |
| MV a′ lateral wall a (cm/s) | 12.0 (9.7; 13.2) | 10.5 (19.3) | 12 (23.2) | 0.2 |
| MV a′ septum a (cm/s) | 10.0 (9.0; 11.0) | 10 (18.1) | 11 (26.5) | 0.02 |
| Ascending AO b (cm) | 2.9 (2.6; 3.2) | 2.7 ± 0.4 | 3.0 ± 0.2 | 0.04 |
| MV A-wave Vmax a (cm/s) | 80 (68.5; 90.0) | 82 (25.1) | 76.5 (17.6) | 0.05 |
| MV E-wave Vmax a (cm/s) | 65.5 (57.5; 77.5) | 67 (22.9) | 63 (21.9) | 0.8 |
| average E/e′ a | 7.1 (6.2; 8.0) | 7 (20.6) | 7.1 (21.5) | 0.8 |
| MV e′ septum a (cm/s) | 8.0 (7.0; 10.0) | 8 (23.1) | 8.5 (20.4) | 0.4 |
| MV e′ lateral wall a (cm/s) | 10.0 (8.0; 13.0) | 10 (19.7) | 10.5 (23.8) | 0.2 |
| PCE risk a (%) | 18.2 (8.5; 33.5) | 15.2 (13) | 27.9 (17.8) | 0.1 |
| FIBROTEST score a | 0.1 (0.1; 0.3) | 0.1 (21.6) | 0.2 (30) | 0.04 |
| ACTITEST score a | 0.1 (0.0; 0.2) | 0.1 (21.3) | 0.1 (30.3) | 0.03 |
| ASHTEST score a | 0.0 (0.0; 0.0) | 0.01 (29.2) | 0.0 (21) | 0.03 |
| NASHTEST score a | 0.5 (0.5; 0.7) | 0.5 (26.4) | 0.5 (23.3) | 0.4 |
| STEATOTEST score b | 0.6 (0.5; 0.7) | 0.6 ± 0.1 | 0.6 ± 0.1 | 0.9 |
| Variable | With LVDD Grade I (n = 27) | Without LVDD Grade I (n = 23) | ∆ | p a |
|---|---|---|---|---|
| Age a (years) | 63.5 (27.4) | 50.5 (11.8) | −13.1 | 0.0001 |
| Diabetes duration a (years) | 9 (19.8) | 7 (15.7) | −3.5 | 0.2 |
| Abdominal waist a (cm) | 115 (22.9) | 112.5 (19.1) | −3 | 0.3 |
| Hip waist a (cm) | 104 (20.7) | 104 (20.1) | −2 | 0.8 |
| BMI a (kg/m2) | 34.2 (22.7) | 34.2 (20.7) | −1.5 | 0.6 |
| VAT b (cm2) | 86.2 ± 46.9 | 57.7 ± 33.9 | −28.4 | 0.04 |
| FG b (mg/dL) | 145.4 ± 36.6 | 143 ± 36.3 | −2.4 | 0.8 |
| HbA1c a (%) | 7.7 (17.8) | 8.8 (24.9) | 0.8 | 0.06 |
| Haptoglobin b (g/L) | 1.8 ± 0.6 | 1.5 ± 0.3 | −0.2 | 0.08 |
| α2 Macroglobulin a (g/L) | 2.2 (26.5) | 1.6 (14.3) | −0.5 | 0.002 |
| Apo A1 a (g/L) | 1.4 (22.8) | 1.4 (20.5) | −0.0 | 0.5 |
| TG a (mg/dL) | 117 (20.1) | 167.5 (25.1) | 8.3 | 0.2 |
| TC b (mg/dL) | 158.2 ± 47.4 | 168.6 ± 46.1 | 10.4 | 0.4 |
| HDLc a (mg/dL) | 42 (22.3) | 42.5 (21.4) | −0.9 | 0.8 |
| LDLc a (mg/dL) | 91 (18.9) | 111.5 (24.2) | 15.2 | 0.1 |
| Uric Acid a (mg/dL) | 5.6 (24) | 5.3 (18.4) | −0.3 | 0.1 |
| eGFR b (mL/min) | 82.7 ± 18.3 | 95 ± 16.6 | 12.2 | 0.06 |
| Serum creatinine b (mg/dL) | 0.8 ± 0.1 | 0.7 ± 0.1 | −0.0 | 0.6 |
| UACr a (mg/g) | 13 (17) | 5.7 (11.1) | −58.3 | 0.07 |
| ALT a (u/L) | 27 (19.6) | 30.5 (25.9) | −3.9 | 0.1 |
| AST b (u/L) | 22.8 ± 16.7 | 19.3 ± 4.4 | −3.5 | 0.4 |
| TB b (µmol/L) | 0.6 ± 0.4 | 0.6 ± 0.3 | −0.0 | 0.9 |
| FAL b | 83.9 ± 22.8 | 81.9 ± 33 | −2 | 0.8 |
| GGT a (u/L) | 29 (21.9) | 31 (22.1) | −13.3 | 0.9 |
| EAT b (mm) | 4.6 ± 1.5 | 3.4 ± 1.6 | −1.2 | 0.01 |
| TAPSE a (cm) | 2.5 (17.5) | 2.8 (23.5) | 0.2 | 0.1 |
| GLS a (%) | 15.5 (8.8) | 17 (10.1) | 0.7 | 0.6 |
| LVEF a (%) | 56 (20.6) | 56.5 (24.3) | 2.0 | 0.3 |
| LA a (cm) | 3.9 (24.9) | 3.3 (14.9) | −0.4 | 0.009 |
| MV s′ lateral wall a (cm/s) | 8 (16.6) | 10 (27.8) | 2.2 | 0.002 |
| MV s′ septum a (cm/s) | 7 (20.4) | 7 (23.2) | 0.3 | 0.4 |
| DTE a (ms) | 219.5 (27.6) | 183 (9.4) | −56.9 | <0.0001 |
| MV a′ lateral wall a (cm/s) | 12 (20.5) | 12 (21.6) | 0.4 | 0.7 |
| MV a′ septum a (cm/s) | 10.5 (22.5) | 9.5 (19.7) | −0.3 | 0.4 |
| Ascending AO b (cm) | 2.9 ± 0.3 | 2.6 ± 0.3 | −0.3 | 0.005 |
| MV A-wave Vmax a (cm/s) | 86 (28) | 66 (11.8) | −20.1 | <0.0001 |
| MV E-wave Vmax a (cm/s) | 60 (18) | 71.5 (28.7) | 11.8 | <0.0001 |
| average E/e′ a | 7.6 (24.4) | 6.7 (15.6) | −1.4 | <0.0001 |
| MV e′ septum a (cm/s) | 7 (15.6) | 10.5 (30.9) | 3.5 | 0.0001 |
| MV e′ lateral wall a (cm/s) | 8 (15.1) | 12 (30.1) | 3.7 | 0.0001 |
| PCE risk a (%) | 22.8 (15.1) | 10.8 (7.5) | −13.7 | 0.02 |
| FIBROTEST score a | 0.19 (26.2) | 0.11 (14.8) | −0.1 | 0.003 |
| ACTITEST score a | 0.1 (21) | 0.1 (23.5) | −0.01 | 0.5 |
| ASHTEST score a | 0.01 (24.1) | 0 (18.4) | −0.005 | 0.1 |
| NASHTEST score a | 0.5 (22) | 0.5 (20.5) | −0.01 | 0.6 |
| STEATOTEST score b | 1.9 ± 0.8 | 2.1 ± 0.6 | 0.2 | 0.3 |
| Parameter | R2 | Coefficient | Standard Error | 95% CI | t | p |
|---|---|---|---|---|---|---|
| Age (years) | 0.39 | 0.03 | 0.00 | 0.01–0.04 | 5.13 | <0.0001 |
| Diabetes duration (years) | 0.06 | 0.01 | 0.01 | −0.00–0.04 | 1.58 | 0.12 |
| Abdominal waist (cm) | 0.02 | 0.00 | 0.00 | −0.00–0.02 | 0.91 | 0.36 |
| Hip waist (cm) | 0.00 | 0.00 | 0.00 | −0.00–0.01 | 0.51 | 0.60 |
| BMI (kg/m2) | 0.01 | 0.00 | 0.01 | −0.01–0.03 | 0.75 | 0.45 |
| VAT (cm2) | 0.09 | 0.00 | 0.00 | 0.00–0.00 | 2.11 | 0.04 |
| TyG index | 0.00 | −0.16 | 0.26 | −0.69–0.36 | −0.62 | 0.53 |
| FG (mg/dL) | 0.01 | −0.00 | 0.00 | −0.00–0.00 | −0.81 | 0.42 |
| HbA1c (%) | 0.05 | −0.06 | 0.04 | −0.16–0.02 | −1.50 | 0.13 |
| Haptoglobin (g/L) | 0.06 | 0.23 | 0.13 | −0.03–0.51 | 1.75 | 0.08 |
| α2 Macroglobulin (g/L) | 0.16 | 0.33 | 0.11 | 0.09–0.56 | 2.86 | 0.006 |
| Apo A1 (g/L) | 0.00 | 0.06 | 0.27 | −0.48–0.62 | 0.24 | 0.80 |
| TG (mg/dL) | 0.02 | 0.00 | 0.00 | −0.00–0.00 | 1.09 | 0.28 |
| TC (mg/dL) | 0.00 | −0.00 | 0.00 | −0.00–0.00 | −0.54 | 0.59 |
| HDLc (mg/dL) | 0.00 | 0.00 | 0.00 | −0.01–0.01 | 0.24 | 0.80 |
| LDLc (mg/dL) | 0.03 | −0.00 | 0.00 | −0.00–0.00 | −1.24 | 0.22 |
| Uric Acid (mg/dL) | 0.02 | 0.06 | 0.06 | −0.06–0.18 | 0.99 | 0.32 |
| eGFR (mL/min) | 0.11 | −0.00 | 0.00 | −0.01–0.00 | −1.90 | 0.06 |
| Serum creatinine (mg/dL) | 0.00 | 0.20 | 0.41 | −0.63–1.04 | 0.50 | 0.61 |
| UACr (mg/g) | 0.05 | 0.00 | 0.00 | −0.00–0.00 | 1.23 | 0.22 |
| ALT (u/L) | 0.00 | −0.00 | 0.00 | −0.01–0.00 | −0.39 | 0.69 |
| AST (u/L) | 0.01 | 0.00 | 0.00 | −0.00–0.01 | 0.81 | 0.41 |
| TB (µmol/L) | 0.00 | 0.02 | 0.19 | −0.37–0.41 | 0.11 | 0.90 |
| FAL | 0.00 | 0.00 | 0.00 | −0.00–0.00 | 0.19 | 0.84 |
| GGT (u/L) | 0.02 | 0.00 | 0.00 | −0.00–0.00 | 0.95 | 0.34 |
| EAT (mm) | 0.13 | 0.10 | 0.04 | 0.02–0.19 | 2.53 | 0.01 |
| TAPSE (cm) | 0.16 | 0.37 | 0.13 | 0.10–0.64 | 2.70 | 0.008 |
| GLS (%) | 0.02 | −0.03 | 0.05 | −0.13–0.07 | −0.60 | 0.55 |
| LVEF (%) | 0.02 | −0.01 | 0.01 | −0.03–0.01 | −1.04 | 0.30 |
| LA (cm) | 0.16 | 0.37 | 0.13 | 0.10–0.64 | 2.79 | 0.008 |
| MV s′ lateral wall (cm/s) | 0.24 | −0.10 | 0.02 | −0.16–0.04 | −3.52 | 0.001 |
| MV s′ septum (cm/s) | 0.01 | −0.03 | 0.04 | −0.12–0.06 | −0.66 | 0.50 |
| MV a′ lateral wall (cm/s) | 0.00 | −0.01 | 0.02 | −0.07–0.04 | −0.51 | 0.61 |
| MV a′ septum (cm/s) | 0.00 | 0.01 | 0.03 | −0.04–0.07 | 0.49 | 0.62 |
| Ascending AO (cm) | 0.17 | 0.50 | 0.17 | 0.15–0.85 | 2.94 | 0.005 |
| PCE risk (%) | 0.18 | 0.01 | 0.00 | 0.00–0.02 | 2.26 | 0.03 |
| FIBROTEST score | 0.10 | 0.94 | 0.42 | 0.09–1.80 | 2.24 | 0.03 |
| ACTITEST score | 0.00 | 0.21 | 0.66 | −1.12–1.55 | 0.32 | 0.74 |
| ASHTEST score | 0.07 | 12.25 | 6.86 | −1.61–26.13 | 1.78 | 0.08 |
| NASHTEST score | 0.00 | 0.10 | 0.44 | −0.78–0.99 | 0.22 | 0.82 |
| STEATOTEST score | 0.01 | −0.40 | 0.49 | −1.41–0.60 | −0.80 | 0.42 |
| Variable | Exp (β) | Nagelkerke R2 | Standard Error | Wald | p |
|---|---|---|---|---|---|
| Age (years) | 1.25 | 0.54 | 3.77 | 10.39 | 0.001 |
| VAT (cm2) | 1.01 | 0.13 | 0.00 | 3.85 | 0.04 |
| α2 Macroglobulin (g/L) | 6.05 | 0.23 | 1.42 | 4.49 | 0.03 |
| EAT (mm) | 1.94 | 0.20 | 0.31 | 4.50 | 0.03 |
| TAPSE (cm) | 0.89 | 0.00 | 0.21 | 0.25 | 0.6 |
| LA (cm) | 6.43 | 0.22 | 0.77 | 5.82 | 0.01 |
| MV s′ lateral wall (cm/s) | 0.56 | 0.31 | 0.21 | 7.31 | 0.006 |
| DTE (ms) | 1.17 | 0.75 | 0.06 | 6.86 | 0.008 |
| Ascending AO (cm) | 12.01 | 0.23 | 0.98 | 6.42 | 0.01 |
| MV e′ septum (cm/s) | 0.46 | 0.51 | 0.25 | 9.26 | 0.002 |
| MV e′ lateral wall (cm/s) | 0.53 | 0.49 | 0.19 | 10.49 | 0.001 |
| PCE risk (%) | 1.12 | 0.32 | 0.06 | 3.77 | 0.05 |
| FIBROTEST score | 309.2 | 0.16 | 2.88 | 3.94 | 0.04 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Braha, A.; Timar, B.; Ivan, V.; Balica, M.M.; Dăniluc, L.; Timar, R. Novel Biomarkers of Grade I Left Ventricular Diastolic Dysfunction in Type 2 Diabetes Patients with Metabolic-Dysfunction-Associated Steatotic Liver Disease. J. Clin. Med. 2024, 13, 5901. https://doi.org/10.3390/jcm13195901
Braha A, Timar B, Ivan V, Balica MM, Dăniluc L, Timar R. Novel Biomarkers of Grade I Left Ventricular Diastolic Dysfunction in Type 2 Diabetes Patients with Metabolic-Dysfunction-Associated Steatotic Liver Disease. Journal of Clinical Medicine. 2024; 13(19):5901. https://doi.org/10.3390/jcm13195901
Chicago/Turabian StyleBraha, Adina, Bogdan Timar, Viviana Ivan, Monica Micloș Balica, Larisa Dăniluc, and Romulus Timar. 2024. "Novel Biomarkers of Grade I Left Ventricular Diastolic Dysfunction in Type 2 Diabetes Patients with Metabolic-Dysfunction-Associated Steatotic Liver Disease" Journal of Clinical Medicine 13, no. 19: 5901. https://doi.org/10.3390/jcm13195901






