Outpatient Management Protocol for Uncomplicated Diverticulitis: A 3-Year Monocentric Experience in a Tertiary Hospital
Abstract
1. Introduction
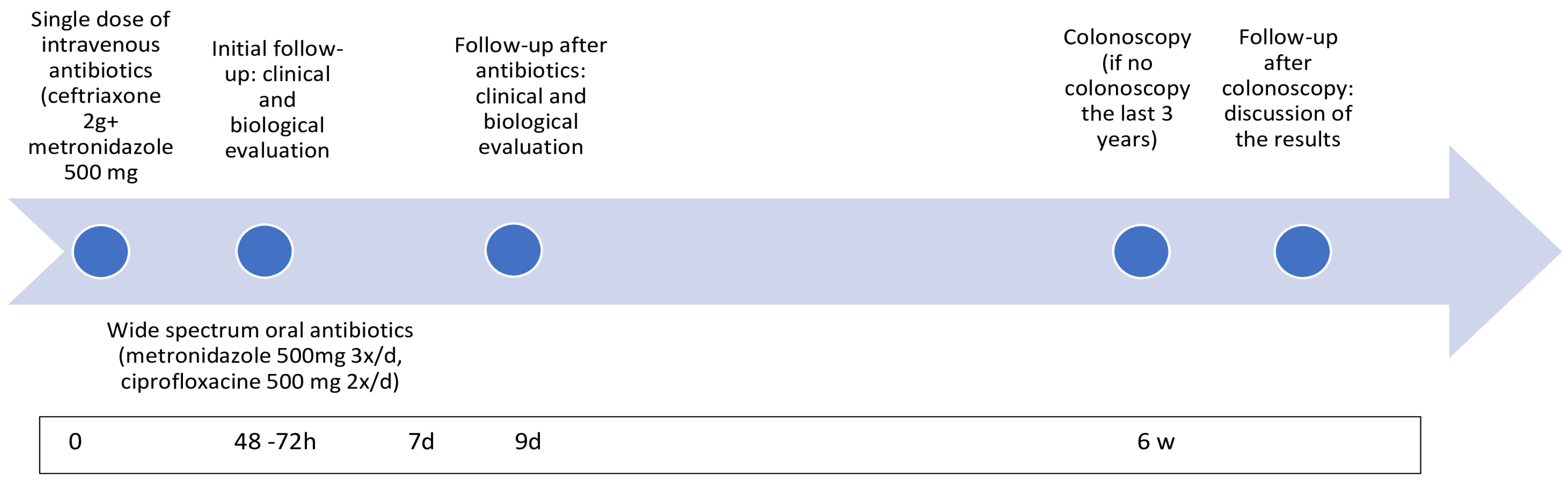
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Biondo, S.; Golda, T.; Kreisler, E.; Espin, E.; Vallribera, F.; Oteiza, F.; Codina-Cazador, A.; Pujadas, M.; Flor, B. Outpatient versus hospitalization management for uncomplicated diverticulitis: A prospective, multicenter randomized clinical trial (DIVER Trial). Ann. Surg. 2014, 259, 38–44. [Google Scholar] [CrossRef] [PubMed]
- van Dijk, S.T.; Bos, K.; de Boer, M.G.J.; Draaisma, W.A.; van Enst, W.A.; Felt, R.J.F.; Klarenbeek, B.R.; Otte, J.A.; Puylaert, J.B.C.M.; van Geloven, A.A.W.; et al. A systematic review and meta-analysis of outpatient treatment for acute diverticulitis. Int. J. Color. Dis. 2018, 33, 505–512. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Cirocchi, R.; Randolph, J.J.; Binda, G.A.; Gioia, S.; Henry, B.M.; Tomaszewski, K.A.; Allegritti, M.; Arezzo, A.; Marzaioli, R.; Ruscelli, P. Is the outpatient management of acute diverticulitis safe and effective? A systematic review and meta-analysis. Tech. Coloproctol. 2019, 23, 87–100. [Google Scholar] [CrossRef] [PubMed]
- Schultz, J.K.; Azhar, N.; Binda, G.A.; Barbara, G.; Biondo, S.; Boermeester, M.A.; Chabok, A.; Consten, E.C.J.; van Dijk, S.T.; Johanssen, A.; et al. European Society of Coloproctology: Guidelines for the management of diverticular disease of the colon. Color. Dis. 2020, 22 (Suppl. S2), 5–28. [Google Scholar] [CrossRef] [PubMed]
- Sartelli, M.; Weber, D.G.; Kluger, Y.; Ansaloni, L.; Coccolini, F.; Abu-Zidan, F.; Augustin, G.; Ben-Ishay, O.; Biffl, W.L.; Bouliaris, K.; et al. 2020 update of the WSES guidelines for the management of acute colonic diverticulitis in the emergency setting. World J Emerg. Surg. 2020, 15, 32. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Desai, M.; Fathallah, J.; Nutalapati, V.; Saligram, S. Antibiotics Versus No Antibiotics for Acute Uncomplicated Diverticulitis: A Systematic Review and Meta-analysis. Dis. Colon. Rectum. 2019, 62, 1005–1012. [Google Scholar] [CrossRef] [PubMed]
- Jaung, R.; Nisbet, S.; Gosselink, M.P.; Di Re, A.; Keane, C.; Lin, A.; Milne, T.; Su’a, B.; Rajaratnam, S.; Ctercteko, G.; et al. Antibiotics Do Not Reduce Length of Hospital Stay for Uncomplicated Diverticulitis in a Pragmatic Double-Blind Randomized Trial. Clin. Gastroenterol. Hepatol. 2021, 19, 503–510. [Google Scholar] [CrossRef] [PubMed]
- Daniels, L.; Ünlü, Ç.; De Korte, N.; Van Dieren, S.; Stockmann, H.B.; Vrouenraets, B.C.; Consten, E.C.; A Van Der Hoeven, J.; A Eijsbouts, Q.; Faneyte, I.F.; et al. Randomized clinical trial of observational versus antibiotic treatment for a first episode of CT-proven uncomplicated acute diverticulitis. Br. J. Surg. 2017, 104, 52–61. [Google Scholar] [CrossRef] [PubMed]
- Isacson, D.; Smedh, K.; Nikberg, M.; Chabok, A. Long-term follow-up of the AVOD randomized trial of antibiotic avoidance in uncomplicated diverticulitis. Br. J. Surg. 2019, 106, 1542–1548. [Google Scholar] [CrossRef] [PubMed]
- van Dijk, S.T.; Daniels, L.; Ünlü, Ç.; de Korte, N.; van Dieren, S.; Stockmann, H.B.; Vrouenraets, B.C.; Consten, E.C.; van der Hoeven, J.A.; Eijsbouts, Q.A.; et al. Long-Term Effects of Omitting Antibiotics in Uncomplicated Acute Diverticulitis. Am. J. Gastroenterol. 2018, 113, 1045–1052. [Google Scholar] [CrossRef] [PubMed]
- Francis, N.K.; Sylla, P.; Abou-Khalil, M.; Arolfo, S.; Berler, D.; Curtis, N.J.; Dolejs, S.C.; Garfinkle, R.; Gorter-Stam, M.; Hashimoto, D.A.; et al. EAES and SAGES 2018 consensus conference on acute diverticulitis management: Evidence-based recommendations for clinical practice. Surg Endosc. 2019, 33, 2726–2741. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Briere, R.; Benhamed, A.; Emond, M.; Blanchard, P.G.; Drolet, S. Evaluation of physicians’ current practices and awareness regarding the treatment of acute uncomplicated diverticulitis: Results of a provincial survey. CJEM 2023, 25, 968–975. [Google Scholar] [CrossRef] [PubMed]
- Stollman, N.; Smalley, W.; Hirano, I.; Committee AGAICG. American Gastroenterological Association Institute Guideline on the Management of Acute Diverticulitis. Gastroenterology 2015, 149, 1944–1949. [Google Scholar] [CrossRef] [PubMed]
- Unlu, C.; de Korte, N.; Daniels, L.; Consten, E.C.; A Cuesta, M.; Gerhards, M.F.; van Geloven, A.A.; van der Zaag, E.S.; AB van der Hoeven, J.; Klicks, R.; et al. A multicenter randomized clinical trial investigating the cost-effectiveness of treatment strategies with or without antibiotics for uncomplicated acute diverticulitis (DIABOLO trial). BMC Surg. 2010, 10, 23. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Emile, S.H.; Elfeki, H.; Sakr, A.; Shalaby, M. Management of acute uncomplicated diverticulitis without antibiotics: A systematic review, meta-analysis, and meta-regression of predictors of treatment failure. Tech. Coloproctol. 2018, 22, 499–509. [Google Scholar] [CrossRef] [PubMed]
- Chabok, A.; Pahlman, L.; Hjern, F.; Haapaniemi, S.; Smedh, K.; Group, A.S. Randomized clinical trial of antibiotics in acute uncomplicated diverticulitis. Br. J. Surg. 2012, 99, 532–539. [Google Scholar] [CrossRef] [PubMed]
- Mohamedahmed, A.Y.; Zaman, S.; Das, N.; Kakaniaris, G.; Vakis, S.; Eccersley, J.; Thomas, P.; Husain, N. Systematic review and meta-analysis of the management of acute uncomplicated diverticulitis: Time to change traditional practice. Int. J. Colorectal Dis. 2024, 39, 47. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Hinchey, E.J.; Schaal, P.G.; Richards, G.K. Treatment of perforated diverticular disease of the colon. Adv. Surg. 1978, 12, 85–109. [Google Scholar] [PubMed]
- Meyer, J.; Caruso, A.; Roos, E.; Balaphas, A.; Toso, C.; Poletti, P.-A.; Ris, F.; Buchs, N.C. The clinical significance of extraluminal air in Hinchey 1a diverticulitis: Results from a retrospective cohort study with 10-year follow-up. Int. J. Color. Dis. 2019, 34, 2053–2058. [Google Scholar] [CrossRef] [PubMed]
- Jaung, R.; Kularatna, M.; Robertson, J.P.; Vather, R.; Rowbotham, D.; MacCormick, A.D.; Bissett, I.P. Uncomplicated Acute Diverticulitis: Identifying Risk Factors for Severe Outcomes. World J. Surg. 2017, 41, 2258–2265. [Google Scholar] [CrossRef] [PubMed]
- Hogan, J.; Sehgal, R.; Murphy, D.; O’Leary, P.; Coffey, J.C. Do Inflammatory Indices Play a Role in Distinguishing between Uncomplicated and Complicated Diverticulitis? Dig. Surg. 2017, 34, 7–11. [Google Scholar] [CrossRef] [PubMed]
- Morini, A.; Zizzo, M.; Tumiati, D.; Mereu, F.; Bernini, D.; Fabozzi, M. Nonoperative management of acute complicated diverticulitis with pericolic and/or distant extraluminal air: A systematic review. World J. Surg. 2024, 48, 2000–2015. [Google Scholar] [CrossRef] [PubMed]
- Tejedor, P.; Pastor, C.; Pellino, G.; Di Saverio, S.; Gorter-Stam, M.; Sylla, P.; Francis, N.; on behalf of the Collaborative Study Group. Management of acute diverticulitis with pericolic free gas (ADIFAS): An international multicenter observational study. Int. J. Surg. 2023, 109, 689–697. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Karentzos, A.; Ntourakis, D.; Tsilidis, K.; Tsoulfas, G.; Papavramidis, T. Hinchey Ia acute diverticulitis with isolated pericolic air on CT imaging; to operate or not? A systematic review. Int. J. Surg. 2021, 85, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Costi, R.; Amato, A.; Annicchiarico, A.; Montali, F.; TabooSurvey, G.; Binda, G.A. Acute diverticulitis management: Evolving trends among Italian surgeons. A survey of the Italian Society of Colorectal Surgery (SICCR). In Updates in Surgery; Springer: Berlin/Heidelberg, Germany, 2024. [Google Scholar] [CrossRef] [PubMed]
- Andrade, P.; Ribeiro, A.; Ramalho, R.; Lopes, S.; Macedo, G. Routine Colonoscopy after Acute Uncomplicated Diverticulitis—Challenging a Putative Indication. Dig. Surg. 2017, 34, 197–202. [Google Scholar] [CrossRef] [PubMed]
- Rottier, S.J.; Dijk, S.T.; Geloven, A.A.W.; Schreurs, W.H.; A Draaisma, W.; A Enst, W.; Puylaert, J.B.C.M.; Boermeester, M.A.; Klarenbeek, B.R.; A Otte, J.; et al. Meta-analysis of the role of colonoscopy after an episode of left-sided acute diverticulitis. Br. J. Surg. 2019, 106, 988–997. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Daniels, L.; Unlu, C.; de Wijkerslooth, T.R.; Stockmann, H.B.; Kuipers, E.J.; Boermeester, M.A.; Dekker, E. Yield of colonoscopy after recent CT-proven uncomplicated acute diverticulitis: A comparative cohort study. Surg. Endosc. 2015, 29, 2605–2613. [Google Scholar] [CrossRef] [PubMed]
- Sharma, P.V.; Eglinton, T.; Hider, P.; Frizelle, F. Systematic review and meta-analysis of the role of routine colonic evaluation after radiologically confirmed acute diverticulitis. Ann. Surg. 2014, 259, 263–272. [Google Scholar] [CrossRef] [PubMed]
- Stegeman, I.; de Wijkerslooth, T.R.; Stoop, E.M.; van Leerdam, M.E.; Dekker, E.; van Ballegooijen, M.; Kuipers, E.J.; Fockens, P.; Kraaijenhagen, R.A.; Bossuyt, P.M. Colorectal cancer risk factors in the detection of advanced adenoma and colorectal cancer. Cancer Epidemiol. 2013, 37, 278–283. [Google Scholar] [CrossRef] [PubMed]
- Dalby, H.R.; Orrú, A.; Sundh, F.; Buchwald, P.; Brännström, F.; Hansske, B.; Haapaniemi, S.; Nikberg, M.; Chabok, A. Management of acute uncomplicated diverticulitis and adherence to current guidelines-a multicentre SNAPSHOT study. Int. J. Color. Dis. 2024, 39, 128. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- E Bharucha, A.; Parthasarathy, G.; Ditah, I.; Fletcher, J.G.; Ewelukwa, O.; Pendlimari, R.; Yawn, B.P.; Melton, J.L.; Schleck, C.; Zinsmeister, A.R. Temporal Trends in the Incidence and Natural History of Diverticulitis: A Population-Based Study. Am. J. Gastroenterol. 2015, 110, 1589–1596. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]

| Outpatient n = 216 | Hospitalization n = 4 | p | |
|---|---|---|---|
| Age, years, median (range) | 57 (25–88) | 56 (37–64) | 0.404 |
| Gender, n (%) F M | 116 (53.7%) 100 (46.3%) | 1 (25%) 3 (75%) | 0.254 |
| BMI, kg/m2, mean, (SD) | 28.7 (±5.1) | 26.5 (±7.1) | 0.565 |
| Comorbidities, n (%) HTA (%) Diabetes | 70 (32.4%) 14 (6.5%) | 3 (75%) 0 | 0.073 0.599 |
| Tobacco use, n (%) | 44 (20.4%) | 1 (25%) | 0.909 |
| History of surgery for diverticulitis, n (%) | 10 (4.6%) | 0 | 0.660 |
| Previous episodes, n (%) 0 1 2 3 4 5 6 7 8 9 | 41 (19.2%) 112 (52.3%) 27 (12.6%) 16 (7.5%) 12 (5.6%) 1 (0.5%) 3 (1.4%) 0 1 (0.5%) 1 (0.5%) | 1 (25%) 2 (25%) 1 (25%) 1 (25%) 0 0 0 0 0 0 | 0.931 |
| Episodes in the last 2 years, n (%) 0 1 2 3 4 | 176 (81.5%) 27 (12.5%) 9 (4.2%) 3 (1.4%) 1 (0.5%) | 4 (100%) 0 0 0 0 | 0.925 |
| Time since last episode, weeks mean (SD) | 160.1 (±167.8) | 198 (±59.4) | 0.753 |
| Outpatient n = 216 | Hospitalization n = 4 | p | |
|---|---|---|---|
| Time since beginning of symptoms, days, mean (SD) | 2.7 (±2.1) | 2.25 (±1.5) | 0.668 |
| HR, BPM, mean (SD) | 89.7 (±14.8) | 80 (±14.1) | 0.196 |
| Mean BP, mmHG mean (SD) | 103.8 (±13.9) | 96.3 (±14.5) | 0.284 |
| Temperature, °C, mean (SD) | 36.9 (±0.7) | 37.4 (±0.7) | 0.288 |
| Pain score, mean (SD) | 4.3 (±2.5) | 5.8 (±2.1) | 0.225 |
Lc, mean (SD)
| 10.6 (±3.4) 7.4 (±2.3) | 14 (±1.6) 10.7 (±2.1) | 0.05 0.05 |
CRP, mean (SD)
| 66.5 (±43.9) 54.2 (±48.9) | 73.5 (±60.1) 99.5 (±93.9) | 0.755 0.073 |
Affected colon segment, n (%)
| 18 (8.3%) 1 (0.5%) 34 (15.7%) 163 (75.5%) | 0 0 0 4 (100%) | 0.731 |
Free air, n (%)
| 5 (2.3%) 5 (100) 0 | 1 (25%) 1 (100%) 0 | 0.006 |
| Univariate | p | Multivariate | p | |
|---|---|---|---|---|
| Time since beginning of symptoms, days | 0.87 (0.47–1.61) | 0.667 | ||
| HR, BPM | 0.94 (0.87–1.03) | 0.203 | ||
| Mean BP, mmHG | 0.96 (0.89–1.04) | 0.289 | ||
| Temperature, °C | 1.17 (0.23–6.08) | 0.850 | 1.07 (0.38–3.00) | 0.902 |
| Pain score | 1.32 (0.83–2.11) | 0.238 | ||
Lc
| 1.42 (0.98–1.79) 1.71 (1.13–2.59) | 0.049 0.011 | 1.16 (0.8–1.69) 1.60 (0.97–2.55) | 0.436 0.092 |
CRP
| 1.01 (0.98–1.03) 1.01(0.99–1.03) | 0.754 0.093 | 1.01 (0.975–1.03) 1.02 (0.98–1.01) | 0.939 0.898 |
Affected colon segment
| 0.00 0.00 0.00 Ref | 0.99 1.00 0.98 | ||
Free air
| Ref 14.1 (1.24–159.89) | 0.033 | 11.72 (0.67–206.28) | 0.048 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Burgard, M.; Litchinko, A.; Meyer, J.; Toso, C.; Ris, F.; Delaune, V. Outpatient Management Protocol for Uncomplicated Diverticulitis: A 3-Year Monocentric Experience in a Tertiary Hospital. J. Clin. Med. 2024, 13, 5920. https://doi.org/10.3390/jcm13195920
Burgard M, Litchinko A, Meyer J, Toso C, Ris F, Delaune V. Outpatient Management Protocol for Uncomplicated Diverticulitis: A 3-Year Monocentric Experience in a Tertiary Hospital. Journal of Clinical Medicine. 2024; 13(19):5920. https://doi.org/10.3390/jcm13195920
Chicago/Turabian StyleBurgard, Marie, Alexis Litchinko, Jeremy Meyer, Christian Toso, Frédéric Ris, and Vaihere Delaune. 2024. "Outpatient Management Protocol for Uncomplicated Diverticulitis: A 3-Year Monocentric Experience in a Tertiary Hospital" Journal of Clinical Medicine 13, no. 19: 5920. https://doi.org/10.3390/jcm13195920
APA StyleBurgard, M., Litchinko, A., Meyer, J., Toso, C., Ris, F., & Delaune, V. (2024). Outpatient Management Protocol for Uncomplicated Diverticulitis: A 3-Year Monocentric Experience in a Tertiary Hospital. Journal of Clinical Medicine, 13(19), 5920. https://doi.org/10.3390/jcm13195920






