The Role of Hypertension in Cognitive Dysfunction
Abstract
1. Introduction
2. The Role of Hypertension in Cognitive Function
3. Association of Hypertension with Cognitive Dysfunction: Clinical Studies
4. Target Blood Pressure and Cognitive Function
5. The Role of Diastolic Blood Pressure in Cognitive Function
6. Age-Related Risk of Cognitive Decline
7. The Role of Imaging in Hypertension-Associated Dementia
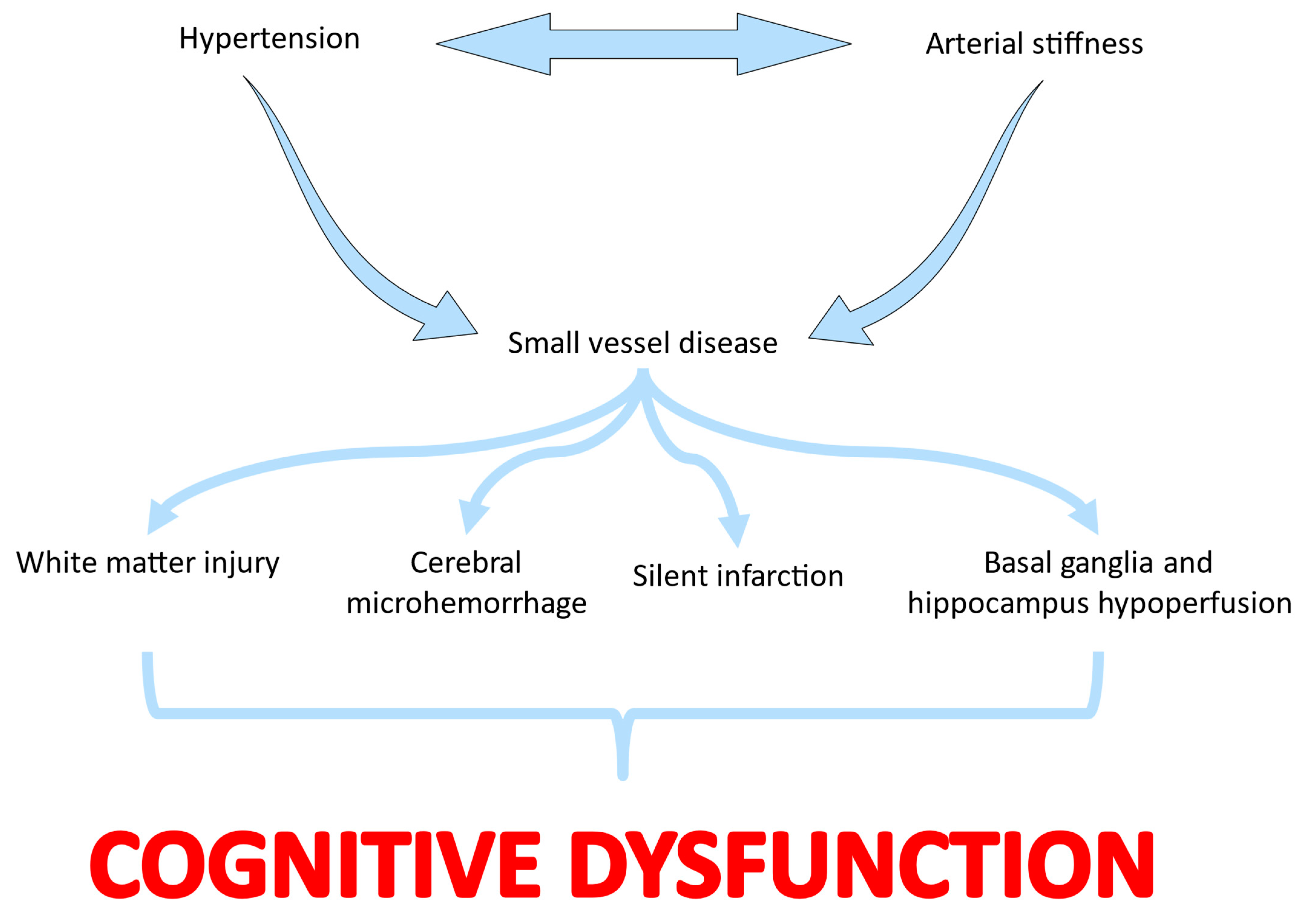
8. The Role of Arterial Stiffness in Cognitive Impairment of Hypertensive Patients
Cognitive Impairment in Coexisting Hypertension and Chronic Kidney Disease
9. Pathophysiology of Hypertension-Induced Cognitive Impairment
10. Blood Pressure Control and Improvement in Cognitive Dysfunction
11. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Mitchell, S.L.; Teno, J.M.; Kiely, D.K.; Shaffer, M.L.; Jones, R.N.; Prigerson, H.G.; Volicer, L.; Givens, J.L.; Hamel, M.B. The clinical course of advanced dementia. N. Engl. J. Med. 2009, 361, 1529–1538. [Google Scholar] [CrossRef]
- McIntyre, R.S.; Cha, D.S.; Soczynska, J.K.; Woldeyohannes, H.O.; Gallaugher, L.A.; Kudlow, P.; Alsuwaidan, M.; Baskaran, A. Cognitive deficits and functional outcomes in major depressive disorder: Determinants, substrates, and treatment interventions. Depress. Anxiety 2013, 30, 515–527. [Google Scholar] [CrossRef]
- Mancia, G.; Kreutz, R.; Brunstrom, M.; Burnier, M.; Grassi, G.; Januszewicz, A.; Muiesan, M.L.; Tsioufis, K.; Agabiti-Rosei, E.; Algharably, E.A.E.; et al. 2023 ESH Guidelines for the management of arterial hypertension The Task Force for the management of arterial hypertension of the European Society of Hypertension: Endorsed by the International Society of Hypertension (ISH) and the European Renal Association (ERA). J. Hypertens 2023, 41, 1874–2071. [Google Scholar] [CrossRef]
- Whelton, P.K.; Carey, R.M.; Aronow, W.S.; Casey, D.E., Jr.; Collins, K.J.; Dennison Himmelfarb, C.; DePalma, S.M.; Gidding, S.; Jamerson, K.A.; Jones, D.W.; et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension 2018, 71, 1269–1324. [Google Scholar] [CrossRef] [PubMed]
- Hughes, D.; Judge, C.; Murphy, R.; Loughlin, E.; Costello, M.; Whiteley, W.; Bosch, J.; O’Donnell, M.J.; Canavan, M. Association of Blood Pressure Lowering With Incident Dementia or Cognitive Impairment: A Systematic Review and Meta-analysis. JAMA 2020, 323, 1934–1944. [Google Scholar] [CrossRef]
- Scuteri, A.; Benetos, A.; Sierra, C.; Coca, A.; Chicherio, C.; Frisoni, G.B.; Gasecki, D.; Hering, D.; Lovic, D.; Manios, E.; et al. Routine assessment of cognitive function in older patients with hypertension seen by primary care physicians: Why and how-a decision-making support from the working group on ‘hypertension and the brain’ of the European Society of Hypertension and from the European Geriatric Medicine Society. J. Hypertens. 2021, 39, 90–100. [Google Scholar] [CrossRef] [PubMed]
- Waldstein, S.R.; Jennings, J.R.; Ryan, C.M.; Muldoon, M.F.; Shapiro, A.P.; Polefrone, J.M.; Fazzari, T.V.; Manuck, S.B. Hypertension and neuropsychological performance in men: Interactive effects of age. Health Psychol. 1996, 15, 102–109. [Google Scholar] [CrossRef] [PubMed]
- Goldstein, F.C.; Hajjar, I.M.; Dunn, C.B.; Levey, A.I.; Wharton, W. The Relationship Between Cognitive Functioning and the JNC-8 Guidelines for Hypertension in Older Adults. J. Gerontol. A Biol. Sci. Med. Sci. 2017, 72, 121–126. [Google Scholar] [CrossRef]
- Gottesman, R.F.; Schneider, A.L.; Albert, M.; Alonso, A.; Bandeen-Roche, K.; Coker, L.; Coresh, J.; Knopman, D.; Power, M.C.; Rawlings, A.; et al. Midlife hypertension and 20-year cognitive change: The atherosclerosis risk in communities neurocognitive study. JAMA Neurol. 2014, 71, 1218–1227. [Google Scholar] [CrossRef]
- Erkinjuntti, T. Subcortical vascular dementia. Cerebrovasc. Dis. 2002, 13 (Suppl. 2), 58–60. [Google Scholar] [CrossRef]
- Cheon, E.J. Hypertension and cognitive dysfunction: A narrative review. J. Yeungnam Med. Sci. 2023, 40, 225–232. [Google Scholar] [CrossRef] [PubMed]
- Forette, F.; Seux, M.L.; Staessen, J.A.; Thijs, L.; Birkenhager, W.H.; Babarskiene, M.R.; Babeanu, S.; Bossini, A.; Gil-Extremera, B.; Girerd, X.; et al. Prevention of dementia in randomised double-blind placebo-controlled Systolic Hypertension in Europe (Syst-Eur) trial. Lancet 1998, 352, 1347–1351. [Google Scholar] [CrossRef] [PubMed]
- Tzourio, C.; Dufouil, C.; Ducimetiere, P.; Alperovitch, A. Cognitive decline in individuals with high blood pressure: A longitudinal study in the elderly. EVA Study Group. Epidemiology of Vascular Aging. Neurology 1999, 53, 1948–1952. [Google Scholar] [CrossRef]
- Berge, E.; Whiteley, W.; Audebert, H.; De Marchis, G.M.; Fonseca, A.C.; Padiglioni, C.; de la Ossa, N.P.; Strbian, D.; Tsivgoulis, G.; Turc, G. European Stroke Organisation (ESO) guidelines on intravenous thrombolysis for acute ischaemic stroke. Eur. Stroke J. 2021, 6, I–LXII. [Google Scholar] [CrossRef]
- Iadecola, C.; Yaffe, K.; Biller, J.; Bratzke, L.C.; Faraci, F.M.; Gorelick, P.B.; Gulati, M.; Kamel, H.; Knopman, D.S.; Launer, L.J.; et al. Impact of Hypertension on Cognitive Function: A Scientific Statement From the American Heart Association. Hypertension 2016, 68, e67–e94. [Google Scholar] [CrossRef]
- Gelber, R.P.; Launer, L.J.; White, L.R. The Honolulu-Asia Aging Study: Epidemiologic and neuropathologic research on cognitive impairment. Curr. Alzheimer Res. 2012, 9, 664–672. [Google Scholar] [CrossRef]
- SPRINT MIND Investigators for the SPRINT Research Group; Williamson, J.D.; Pajewski, N.M.; Auchus, A.P.; Bryan, R.N.; Chelune, G.; Cheung, A.K.; Cleveland, M.L.; Coker, L.H.; Crowe, M.G.; et al. Effect of Intensive vs Standard Blood Pressure Control on Probable Dementia: A Randomized Clinical Trial. JAMA 2019, 321, 553–561. [Google Scholar] [CrossRef]
- Euser, S.M.; van Bemmel, T.; Schram, M.T.; Gussekloo, J.; Hofman, A.; Westendorp, R.G.; Breteler, M.M. The effect of age on the association between blood pressure and cognitive function later in life. J. Am. Geriatr. Soc. 2009, 57, 1232–1237. [Google Scholar] [CrossRef]
- Ruitenberg, A.; Skoog, I.; Ott, A.; Aevarsson, O.; Witteman, J.C.; Lernfelt, B.; van Harskamp, F.; Hofman, A.; Breteler, M.M. Blood pressure and risk of dementia: Results from the Rotterdam study and the Gothenburg H-70 Study. Dement. Geriatr. Cogn. Disord. 2001, 12, 33–39. [Google Scholar] [CrossRef]
- Jiang, C.; Li, S.; Wang, Y.; Lai, Y.; Bai, Y.; Zhao, M.; He, L.; Kong, Y.; Guo, X.; Li, S.; et al. Diastolic Blood Pressure and Intensive Blood Pressure Control on Cognitive Outcomes: Insights From the SPRINT MIND Trial. Hypertension 2023, 80, 580–589. [Google Scholar] [CrossRef]
- Perera, G.; Rijnbeek, P.R.; Alexander, M.; Ansell, D.; Avillach, P.; Duarte-Salles, T.; Gordon, M.F.; Lapi, F.; Mayer, M.A.; Pasqua, A.; et al. Vascular and metabolic risk factor differences prior to dementia diagnosis: A multidatabase case-control study using European electronic health records. BMJ Open 2020, 10, e038753. [Google Scholar] [CrossRef]
- Emdin, C.A.; Rothwell, P.M.; Salimi-Khorshidi, G.; Kiran, A.; Conrad, N.; Callender, T.; Mehta, Z.; Pendlebury, S.T.; Anderson, S.G.; Mohseni, H.; et al. Blood Pressure and Risk of Vascular Dementia: Evidence From a Primary Care Registry and a Cohort Study of Transient Ischemic Attack and Stroke. Stroke 2016, 47, 1429–1435. [Google Scholar] [CrossRef] [PubMed]
- Verhaaren, B.F.; Vernooij, M.W.; de Boer, R.; Hofman, A.; Niessen, W.J.; van der Lugt, A.; Ikram, M.A. High blood pressure and cerebral white matter lesion progression in the general population. Hypertension 2013, 61, 1354–1359. [Google Scholar] [CrossRef] [PubMed]
- Swan, G.E.; DeCarli, C.; Miller, B.L.; Reed, T.; Wolf, P.A.; Jack, L.M.; Carmelli, D. Association of midlife blood pressure to late-life cognitive decline and brain morphology. Neurology 1998, 51, 986–993. [Google Scholar] [CrossRef]
- Kilander, L.; Nyman, H.; Boberg, M.; Hansson, L.; Lithell, H. Hypertension is related to cognitive impairment: A 20-year follow-up of 999 men. Hypertension 1998, 31, 780–786. [Google Scholar] [CrossRef]
- Nation, D.A.; Preis, S.R.; Beiser, A.; Bangen, K.J.; Delano-Wood, L.; Lamar, M.; Libon, D.J.; Seshadri, S.; Wolf, P.A.; Au, R. Pulse Pressure Is Associated With Early Brain Atrophy and Cognitive Decline: Modifying Effects of APOE-epsilon4. Alzheimer Dis. Assoc. Disord. 2016, 30, 210–215. [Google Scholar] [CrossRef]
- Sabayan, B.; Wijsman, L.W.; Foster-Dingley, J.C.; Stott, D.J.; Ford, I.; Buckley, B.M.; Sattar, N.; Jukema, J.W.; van Osch, M.J.; van der Grond, J.; et al. Association of visit-to-visit variability in blood pressure with cognitive function in old age: Prospective cohort study. BMJ 2013, 347, f4600. [Google Scholar] [CrossRef]
- Hanon, O.; Haulon, S.; Lenoir, H.; Seux, M.L.; Rigaud, A.S.; Safar, M.; Girerd, X.; Forette, F. Relationship between arterial stiffness and cognitive function in elderly subjects with complaints of memory loss. Stroke 2005, 36, 2193–2197. [Google Scholar] [CrossRef]
- Hirasawa, A.; Nagai, K.; Miyazawa, T.; Koshiba, H.; Tamada, M.; Shibata, S.; Kozaki, K. Relationship between arterial stiffness and cognitive function in outpatients with dementia and mild cognitive impairment compared with community residents without dementia. J. Geriatr. Cardiol. 2022, 19, 594–602. [Google Scholar] [CrossRef]
- Kalaitzidis, R.G.; Karasavvidou, D.; Tatsioni, A.; Balafa, O.; Pappas, K.; Spanos, G.; Pelidou, S.H.; Siamopoulos, K.C. Risk factors for cognitive dysfunction in CKD and hypertensive subjects. Int. Urol. Nephrol. 2013, 45, 1637–1646. [Google Scholar] [CrossRef]
- Karasavvidou, D.; Boutouyrie, P.; Kalaitzidis, R.; Kettab, H.; Pappas, K.; Stagikas, D.; Antonakis, N.; Tsalikakis, D.; Elisaf, M.; Laurent, S. Arterial damage and cognitive decline in chronic kidney disease patients. J. Clin. Hypertens. 2018, 20, 1276–1284. [Google Scholar] [CrossRef] [PubMed]
- Kalaitzidis, R.G.; Balafa, O.; Dounousi, E.; Stagikas, D.; Tsimihodimos, V. Adherence to Treatment, Arterial Stiffness and Cognitive Function in Irbesartan- Treated Newly Diagnosed Hypertensive Patients. Curr. Vasc. Pharmacol. 2021, 19, 565–571. [Google Scholar] [CrossRef] [PubMed]
- Kalaitzidis, R.G.; Panagiotopoulou, T.; Stagikas, D.; Pappas, K.; Balafa, O.; Elisaf, M.S. Arterial Stiffness, Cognitive Dysfunction and Adherence to Antihypertensive Agents. Is there a Link to Hypertensive Patients? Curr. Vasc. Pharmacol. 2020, 18, 410–417. [Google Scholar] [CrossRef]
- Hu, X.; De Silva, T.M.; Chen, J.; Faraci, F.M. Cerebral Vascular Disease and Neurovascular Injury in Ischemic Stroke. Circ. Res. 2017, 120, 449–471. [Google Scholar] [CrossRef]
- Kaess, B.M.; Rong, J.; Larson, M.G.; Hamburg, N.M.; Vita, J.A.; Levy, D.; Benjamin, E.J.; Vasan, R.S.; Mitchell, G.F. Aortic stiffness, blood pressure progression, and incident hypertension. JAMA 2012, 308, 875–881. [Google Scholar] [CrossRef]
- Siedlinski, M.; Carnevale, L.; Xu, X.; Carnevale, D.; Evangelou, E.; Caulfield, M.J.; Maffia, P.; Wardlaw, J.; Samani, N.J.; Tomaszewski, M.; et al. Genetic analyses identify brain structures related to cognitive impairment associated with elevated blood pressure. Eur. Heart J. 2023, 44, 2114–2125. [Google Scholar] [CrossRef]
- Jefferson, A.L.; Cambronero, F.E.; Liu, D.; Moore, E.E.; Neal, J.E.; Terry, J.G.; Nair, S.; Pechman, K.R.; Rane, S.; Davis, L.T.; et al. Higher Aortic Stiffness Is Related to Lower Cerebral Blood Flow and Preserved Cerebrovascular Reactivity in Older Adults. Circulation 2018, 138, 1951–1962. [Google Scholar] [CrossRef]
- Mogi, M.; Horiuchi, M. Clinical Interaction between Brain and Kidney in Small Vessel Disease. Cardiol. Res. Pract. 2011, 2011, 306189. [Google Scholar] [CrossRef]
- Thompson, C.S.; Hakim, A.M. Living beyond our physiological means: Small vessel disease of the brain is an expression of a systemic failure in arteriolar function: A unifying hypothesis. Stroke 2009, 40, e322–e330. [Google Scholar] [CrossRef]
- Peila, R.; White, L.R.; Masaki, K.; Petrovitch, H.; Launer, L.J. Reducing the risk of dementia: Efficacy of long-term treatment of hypertension. Stroke 2006, 37, 1165–1170. [Google Scholar] [CrossRef]
- Lennon, M.J.; Lam, B.C.P.; Lipnicki, D.M.; Crawford, J.D.; Peters, R.; Schutte, A.E.; Brodaty, H.; Thalamuthu, A.; Rydberg-Sterner, T.; Najar, J.; et al. Use of Antihypertensives, Blood Pressure, and Estimated Risk of Dementia in Late Life: An Individual Participant Data Meta-Analysis. JAMA Netw. Open 2023, 6, e2333353. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Theofilis, P.; Doumani, G.; Tsatsani, G.-C.; Volis, N.; Kampourelli, A.; Thimis, V.; Xanthopoulou, E.; Kalaitzidis, R. The Role of Hypertension in Cognitive Dysfunction. J. Clin. Med. 2024, 13, 5979. https://doi.org/10.3390/jcm13195979
Theofilis P, Doumani G, Tsatsani G-C, Volis N, Kampourelli A, Thimis V, Xanthopoulou E, Kalaitzidis R. The Role of Hypertension in Cognitive Dysfunction. Journal of Clinical Medicine. 2024; 13(19):5979. https://doi.org/10.3390/jcm13195979
Chicago/Turabian StyleTheofilis, Panagiotis, Georgia Doumani, Georgia-Christina Tsatsani, Nikolaos Volis, Aikaterini Kampourelli, Vasileios Thimis, Eleni Xanthopoulou, and Rigas Kalaitzidis. 2024. "The Role of Hypertension in Cognitive Dysfunction" Journal of Clinical Medicine 13, no. 19: 5979. https://doi.org/10.3390/jcm13195979
APA StyleTheofilis, P., Doumani, G., Tsatsani, G.-C., Volis, N., Kampourelli, A., Thimis, V., Xanthopoulou, E., & Kalaitzidis, R. (2024). The Role of Hypertension in Cognitive Dysfunction. Journal of Clinical Medicine, 13(19), 5979. https://doi.org/10.3390/jcm13195979





