Influence of Endodontic Cavity Design on Interfacial Voids, Class II Resin Composites Sealing Ability and Tooth Fracture Resistance: An In Vitro Study
Abstract
:1. Introduction
2. Material and Methods
2.1. Sample Size Calculation
2.2. Samples Collection and Allocation
2.3. Class II Cavity Preparation
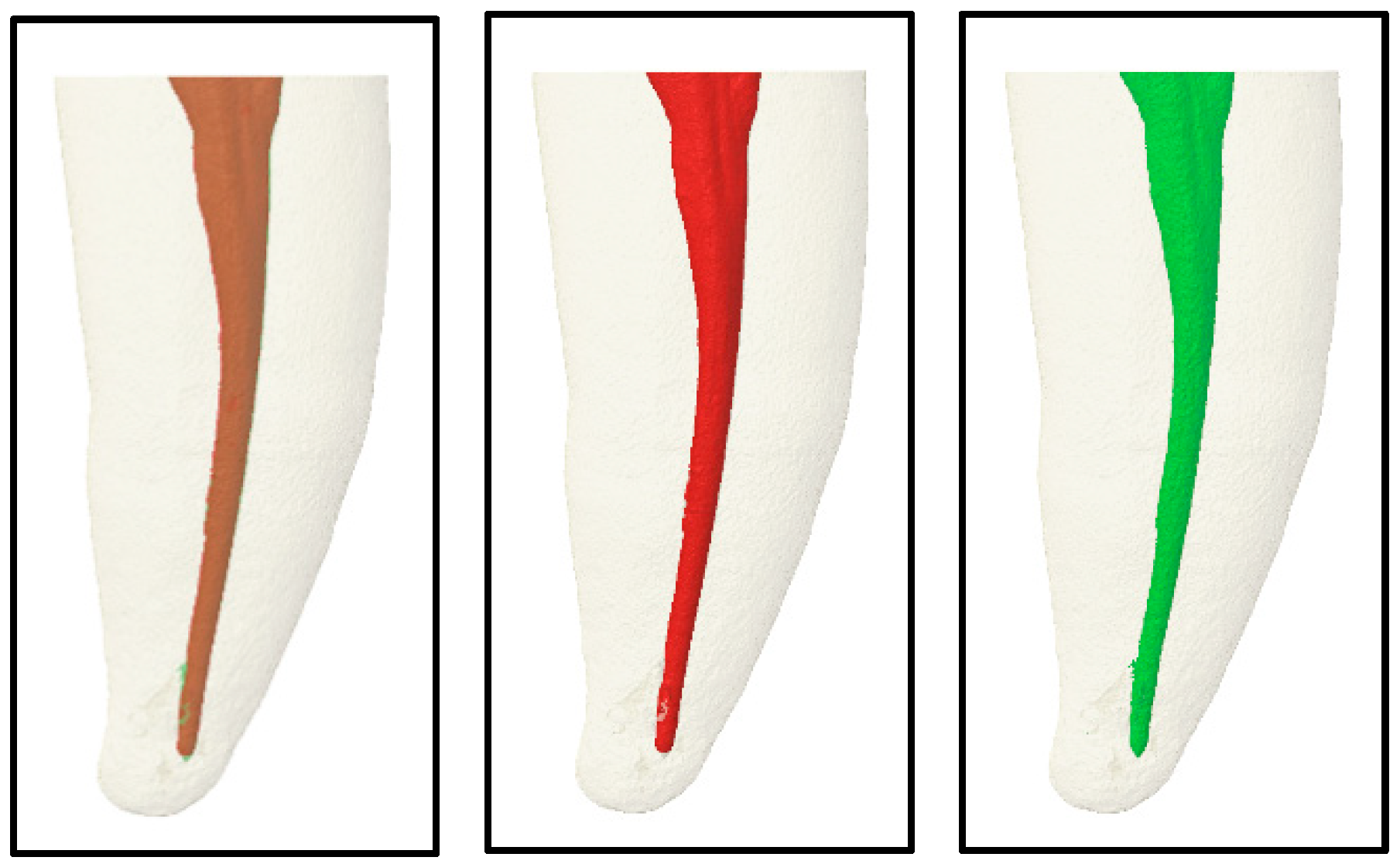
2.4. Access Cavity and Radicular Preperation
2.4.1. Group A: Traditional Access Cavity
2.4.2. Group B: Contracted Access Cavity
2.4.3. Cleaning, Shaping, and Obturation of the Root Canal
2.5. Coronal Restoration
2.5.1. Microhybrid Resin Composite (Filtek Z250) (α Groups)
2.5.2. Self-Adhesive Composite (β Groups)
2.6. Dye Penetration Test
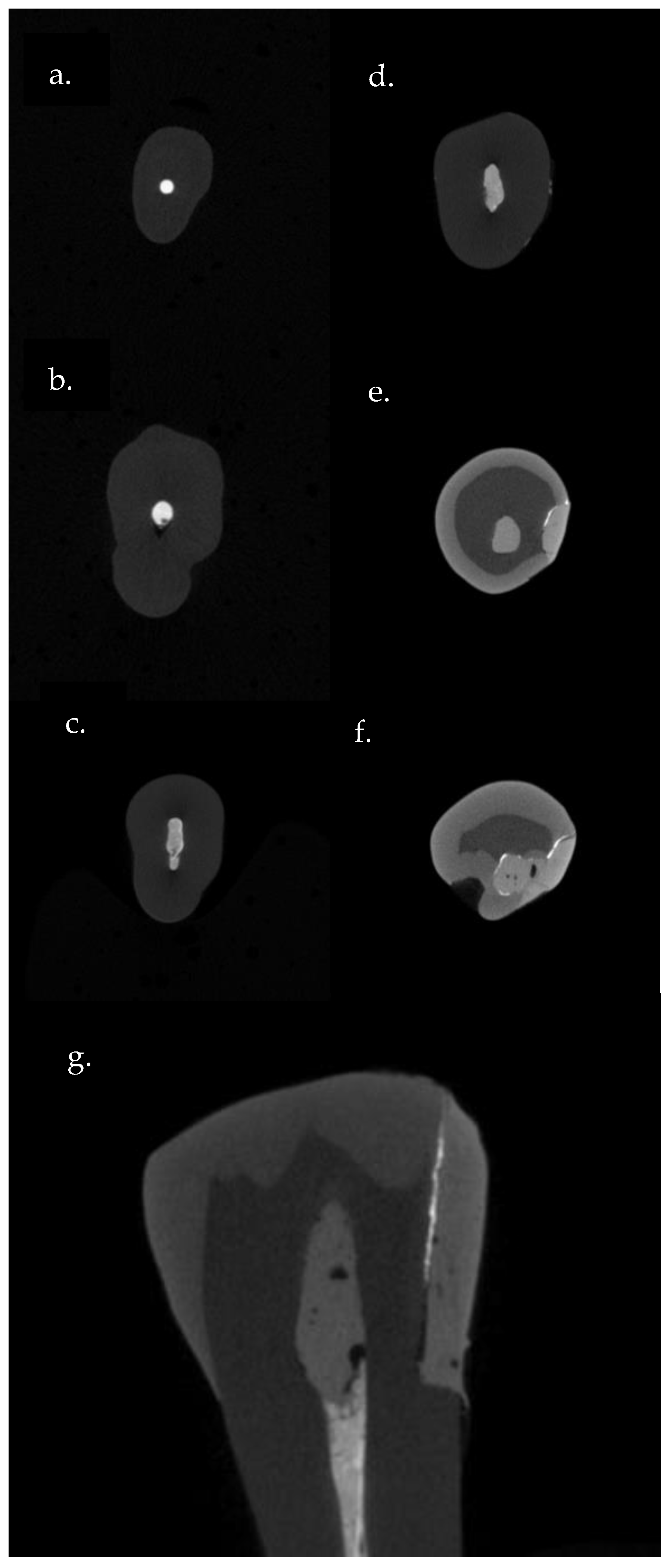
2.7. Micro CT Scan
2.8. Fracture Resistance Test
2.9. Statistical Analysis
3. Results
3.1. Obturation Interfacial Voids
3.2. Cervical Interfacial Sealing Ability
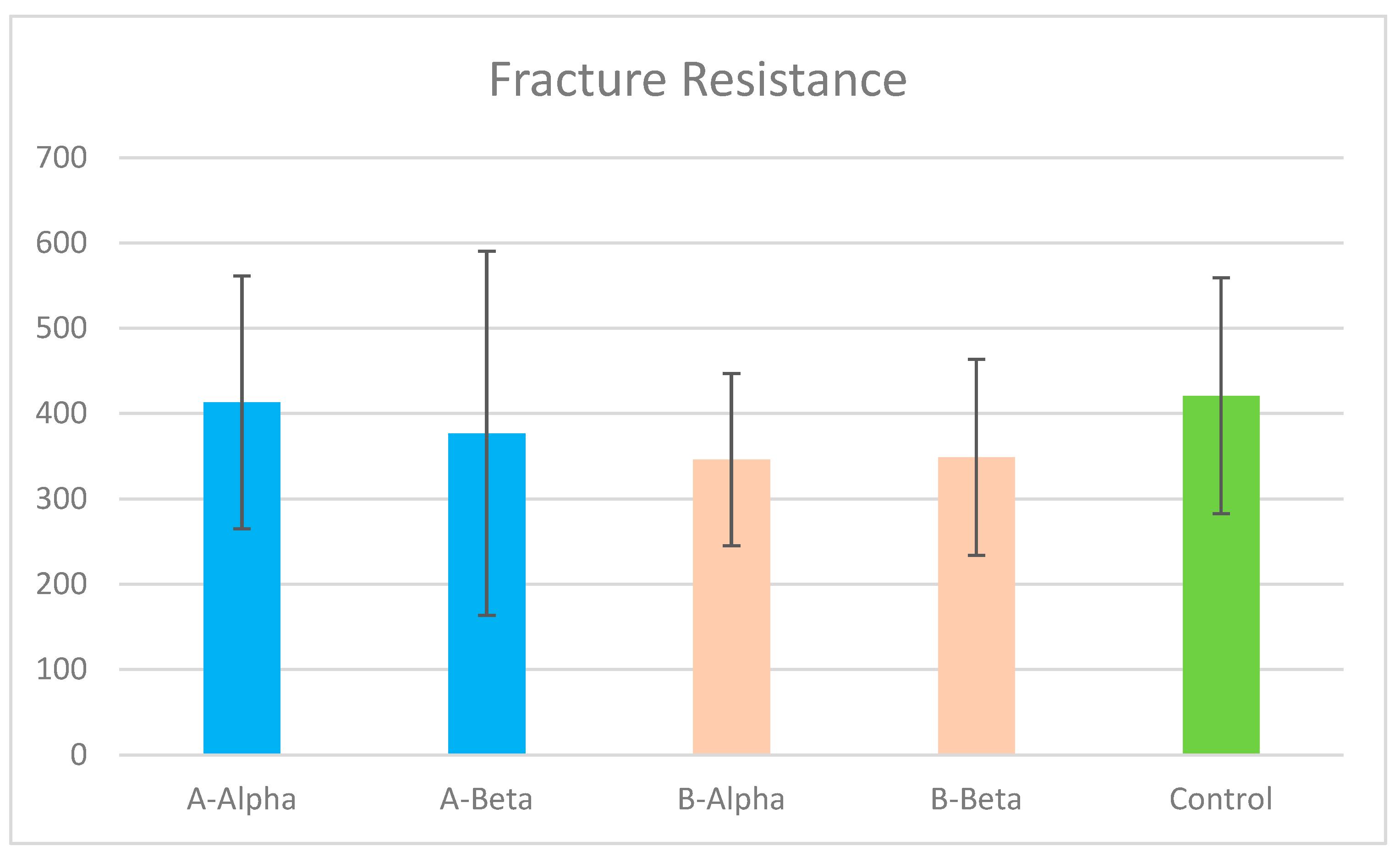
3.3. Tooth Fracture Resistance
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Silva, E.J.N.L.; Oliveira, V.B.; Silva, A.A.; Belladonna, F.G.; Prado, M.; Antunes, H.S.; De-Deus, G. Effect of access cavity design on gaps and void formation in resin composite restorations following root canal treatment on extracted teeth. Int. Endod. J. 2020, 53, 1540–1548. [Google Scholar] [CrossRef] [PubMed]
- Abou El Nasr, H.M.; Abd El Kader, K.G. Dentinal damage and fracture resistance of oval roots prepared with single-file systems using different kinematics. J. Endod. 2014, 40, 849–851. [Google Scholar] [CrossRef] [PubMed]
- Aidasani, G.L.; Mulay, S.; Borkar, A. Comparative evaluation of flexural fracture resistance of mandibular premolars after instrumentation with four different endodontic file systems: An. Indian J. Dent. Res. 2020, 31, 701–705. [Google Scholar] [CrossRef] [PubMed]
- Wu, M.K.; van der Sluis, L.W.; Wesselink, P.R. Comparison of mandibular premolars and canines with respect to their resistance to vertical root fracture. J. Dent. 2004, 32, 265–268. [Google Scholar] [CrossRef] [PubMed]
- Malakpour, M. Assessment of Fracture Resistance of Maxillary First Molars after Root Canal Preparation Using Three Different Rotary Instruments (V-Taper, ProTaper, Vortex Blue): Finite Element Analysis. Master’s Thesis, West Virginia University, Morgantown, WV, USA, 2019. Available online: https://researchrepository.wvu.edu/etd/7456 (accessed on 19 September 2024).
- Van der Vyver, P.J.; Jonker, C.; Vorster, M. Mandibular first and second premolars with challenging root canal anatomy-Part 2: Endodontic management. S. Afr. Dent. J. 2020, 75, 130–136. [Google Scholar] [CrossRef]
- Georgiev, K.; Pecheva, A. Deviant morphology of the root canal system in mandibular premolars: Clinical cases. Folia Med. 2022, 64, 176–180. [Google Scholar] [CrossRef]
- Mittal, S.; Kumar, T.; Sharma, J. Mandibular premolars with aberrant canal morphology: An endodontic challenge. J. Conserv. Dent. 2014, 17, 491–494. [Google Scholar] [CrossRef]
- Thanaruengrong, P.; Kulvitit, S.; Navachinda, M.; Charoenlarp, P. Prevalence of complex root canal morphology in the mandibular first and second premolars in Thai population: CBCT analysis. BMC Oral. Health 2021, 21, 449. [Google Scholar] [CrossRef]
- Tong, H.; Kwon, D.; Shi, J.; Sakai, N.; Enciso, R.; Sameshima, G.T. Mesiodistal angulation and faciolingual inclination of each whole tooth in 3-dimensional space in patients with near-normal occlusion. Am. J. Orthod. Dentofac. Orthop. 2012, 141, 604–617. [Google Scholar] [CrossRef]
- Acharya, N.; Hasan, M.R.; Kafle, D.; Chakradhar, A.; Saito, T. Effect of Hand and Rotary Instruments on the Fracture Resistance of Teeth: An In Vitro Study. Dent. J. 2020, 8, 38. [Google Scholar] [CrossRef]
- Lin, F.; Ordinola-Zapata, R.; Fok, A.S.L.; Lee, R. Influence of minimally invasive endodontic access cavities and bonding status of resin composites on the mechanical property of endodontically-treated teeth: A finite element study. Dent. Mater. 2022, 38, 242–250. [Google Scholar] [CrossRef] [PubMed]
- Alovisi, M.; Pasqualini, D.; Musso, E.; Bobbio, E.; Giuliano, C.; Mancino, D.; Scotti, N.; Berutti, E. Influence of Contracted Endodontic Access on Root Canal Geometry: An In Vitro Study. J. Endod. 2018, 44, 614–620. [Google Scholar] [CrossRef] [PubMed]
- Albuquerque, D.; Kottoor, J.; Hammo, M. Endodontic and clinical considerations in the management of variable anatomy in mandibular premolars: A literature review. Biomed. Res. Int. 2014, 2014, 512574. [Google Scholar] [CrossRef] [PubMed]
- Sagale, A.A.; Ramugade, M.M.; Ganga, R. Endodontic Management of Mandibular Second Premolar with Type IX Canal Configuration Using Cone-Beam Computed Tomography as a Diagnostic Aid: A Rare Case Report. Contemp. Clin. Dent. 2018, 9, S180–S184. [Google Scholar] [CrossRef] [PubMed]
- Silva, E.J.N.L.; Pinto, K.P.; Ferreira, C.M.; Belladonna, F.G.; De-Deus, G.; Dummer, P.M.H.; Versiani, M.A. Current status on minimal access cavity preparations: A critical analysis and a proposal for a universal nomenclature. Int. Endod. J. 2020, 53, 1618–1635. [Google Scholar] [CrossRef]
- Kaisarly, D.; ElGezawi, M.; Haridy, R.; Elembaby, A.; Aldegheishem, A.; Alsheikh, R.; Almulhim, K.S. Reliability of Class II Bulk-fill Composite Restorations With and Without Veneering: A Two-year Randomized Clinical Control Study. Oper. Dent. 2021, 46, 491–504. [Google Scholar] [CrossRef]
- Liu, X.; Zhang, R.; Yu, X.; Hua, F.; Zhang, L.; Chen, Z. Self-adhesive flowable composite resins and flowable composite resins in permanent teeth with occlusal cavities: A systematic review and meta-analysis. J. Dent. 2023, 138, 104691. [Google Scholar] [CrossRef]
- Salah, Z.; Sleibi, A. Effect of deep margin elevation on fracture resistance of premolars restored with ceramic onlay: In vitro comparative study. J. Clin. Exp. Dent. 2023, 15, e446–e453. [Google Scholar] [CrossRef]
- Geo, T.D.; Gupta, S.; Gupta, S.G.; Rana, K.S. Is Deep margin elevation a reliable tool for cervical margin relocation?—A comparative review. J. Oral. Biol. Craniofac Res. 2024, 14, 33–38. [Google Scholar] [CrossRef]
- Elgezawi, M.; Haridy, R.; Abdalla, M.A.; Heck, K.; Draenert, M.; Kaisarly, D. Current Strategies to Control Recurrent and Residual Caries with Resin Composite Restorations: Operator- and Material-Related Factors. J. Clin. Med. 2022, 11, 6591. [Google Scholar] [CrossRef]
- Saberi, E.A.; Pirhaji, A.; Zabetiyan, F. Effects of Endodontic Access Cavity Design and Thermocycling on Fracture Strength of Endodontically Treated Teeth. Clin. Cosmet. Investig. Dent. 2020, 12, 149–156. [Google Scholar] [CrossRef] [PubMed]
- Rippe, M.P.; Santini, M.F.; Bier, C.A.; Baldissara, P.; Valandro, L.F. Effect of root canal preparation, type of endodontic post and mechanical cycling on root fracture strength. J. Appl. Oral. Sci. 2014, 22, 165–173. [Google Scholar] [CrossRef] [PubMed]
- Lima, C.O.; Barbosa, A.F.A.; Ferreira, C.M.; Ferretti, M.A.; Aguiar, F.H.B.; Lopes, R.T.; Fidel, S.R.; Silva, E.J.N.L. Influence of ultraconservative access cavities on instrumentation efficacy with XP-endo Shaper and Reciproc, filling ability and load capacity of mandibular molars subjected to thermomechanical cycling. Int. Endod. J. 2021, 54, 1383–1393. [Google Scholar] [CrossRef] [PubMed]
- Plotino, G.; Grande, N.M.; Isufi, A.; Ioppolo, P.; Pedullà, E.; Bedini, R.; Gambarini, G.; Testarelli, L. Fracture Strength of Endodontically Treated Teeth with Different Access Cavity Designs. J. Endod. 2017, 43, 995–1000. [Google Scholar] [CrossRef] [PubMed]
- Patil, P.; Newase, P.; Pawar, S.; Gosai, H.; Shah, D.; Parhad, S.M. Comparison of Fracture Resistance of Endodontically Treated Teeth With Traditional Endodontic Access Cavity, Conservative Endodontic Access Cavity, Truss Endodontic Access Cavity, and Ninja Endodontic Access Cavity Designs: An In Vitro Study. Cureus 2022, 14, e28090. [Google Scholar] [CrossRef]
- Schneider, S.W. A comparison of canal preparations in straight and curved root canals. Oral. Surg. Oral. Med. Oral. Pathol. 1971, 32, 271–275. [Google Scholar] [CrossRef]
- Akbarian, G.; Ameri, H.; Chasteen, J.E.; Ghavamnasiri, M. Fracture resistance of premolar teeth restored with silorane-based or dimethacrylate-based composite resins. J. Esthet. Restor. Dent. 2014, 26, 200–207. [Google Scholar] [CrossRef]
- Vichi, A.; Goracci, C.; Ferrari, M. Clinical study of the self-adhering flowable composite resin Vertise Flow in Class I restorations: Six-month follow-up. Int. Dent. SA 2010, 12, 14–23. [Google Scholar]
- Eden, E.; Topaloglu-Ak, A.; Cuijpers, V.; Frencken, J.E. Micro-CT for measuring marginal leakage of Class II resin composite restorations in primary molars prepared in vivo. Am. J. Dent. 2008, 21, 393–397. [Google Scholar]
- Pereira, R.D.; Leoni, G.B.; Silva-Sousa, Y.T.; Gomes, E.A.; Dias, T.R.; Brito-Júnior, M.; Sousa-Neto, M.D. Impact of Conservative Endodontic Cavities on Root Canal Preparation and Biomechanical Behavior of Upper Premolars Restored with Different Materials. J. Endod. 2021, 47, 989–999. [Google Scholar] [CrossRef]
- Guo, J.; Wang, Z.; Li, X.; Sun, C.; Gao, E.; Li, H. A comparison of the fracture resistances of endodontically treated mandibular premolars restored with endocrowns and glass fiber post-core retained conventional crowns. J. Adv. Prosthodont. 2016, 8, 489–493. [Google Scholar] [CrossRef] [PubMed]
- Al-Fouzan, K.S. Variable taper nickel-titanium rotary instrument technique. Saudi Endod. J. 2011, 1, 27–32. [Google Scholar] [CrossRef]
- Kandaswamy, D.; Venkateshbabu, N.; Krishna, R.G.; Hannah, R.; Arathi, G.; Roohi, R. Comparison of laterally condensed, vertically compacted thermoplasticized, cold free-flow GP obturations—A volumetric analysis using spiral CT. J. Conserv. Dent. 2009, 12, 145–149. [Google Scholar] [CrossRef] [PubMed]
- Costa, J.F.; Siqueira, W.L.; Loguercio, A.D.; Reis, A.; Oliveira, E.; Alves, C.M.; Bauer, J.R.; Grande, R.H. Characterization of aqueous silver nitrate solutions for leakage tests. J. Appl. Oral. Sci. 2011, 19, 254–259. [Google Scholar] [CrossRef] [PubMed]
- Zavattini, A.; Mancini, M.; Higginson, J.; Foschi, F.; Pasquantonio, G.; Mangani, F. Micro-computed tomography evaluation of microleakage of Class II composite restorations: An. Eur. J. Dent. 2018, 12, 369–374. [Google Scholar] [CrossRef]
- Silva, E.J.N.L.; Rover, G.; Belladonna, F.G.; De-Deus, G.; da Silveira Teixeira, C.; da Silva Fidalgo, T.K. Impact of contracted endodontic cavities on fracture resistance of endodontically treated teeth: A systematic review of in vitro studies. Clin. Oral. Investig. 2018, 22, 109–118. [Google Scholar] [CrossRef]
- Mowlood, A.J.; Ali, A.H.; Mahdee, A.F. Cusp deflection and fracture strength of root canal filled premolars with two access cavities designs (Conservative vs Traditional). J. Clin. Exp. Dent. 2022, 14, e705–e711. [Google Scholar] [CrossRef]
- Krishan, R.; Paqué, F.; Ossareh, A.; Kishen, A.; Dao, T.; Friedman, S. Impacts of conservative endodontic cavity on root canal instrumentation efficacy and resistance to fracture assessed in incisors, premolars, and molars. J. Endod. 2014, 40, 1160–1166. [Google Scholar] [CrossRef]
- Selvakumar, R.J.; Surendran, S.; Sundar, S.; Arul, B.; Natanasabapathy, V. Impact of Contracted Endodontic Access Cavities on the Fracture Resistance of Endodontically Treated Teeth After Mechanical Aging by Simulated Chewing Forces. J. Endod. 2023, 49, 1176–1182. [Google Scholar] [CrossRef]
- Ballester, B.; Giraud, T.; Ahmed, H.M.A.; Nabhan, M.S.; Bukiet, F.; Guivarc’h, M. Current strategies for conservative endodontic access cavity preparation techniques-systematic review, meta-analysis, and decision-making protocol. Clin. Oral. Investig. 2021, 25, 6027–6044. [Google Scholar] [CrossRef]
- Vichi, A.; Margvelashvili, M.; Goracci, C.; Papacchini, F.; Ferrari, M. Bonding and sealing ability of a new self-adhering flowable composite resin in class I restorations. Clin. Oral. Investig. 2013, 17, 1497–1506. [Google Scholar] [CrossRef] [PubMed]
- Mishra, P.; Jaiswal, S.; Nikhil, V.; Gupta, S.; Jha, P.; Raj, S. Evaluation of marginal sealing ability of self-adhesive flowable composite resin in Class II composite restoration: An. J. Conserv. Dent. 2018, 21, 363–368. [Google Scholar] [CrossRef] [PubMed]
- Al-Rawas, M.; Johari, Y.; Yusoff, N.M.; Mohamad, D.; Husein, A. The versatility of flowable composites. Part 1: Theory and new classification. Dent. Update 2022, 49, 553–560. [Google Scholar] [CrossRef]
- Al-Rawas, M.; Johari, Y.; Yusoff, N.M.; Mohamad, D.; Husein, A. The versatility of flowable composites. Part 2: Clinical uses. Dent. Update 2022, 49, 633–636. [Google Scholar] [CrossRef]
- Atalay, C.; Yazici, A.R.; Horuztepe, A.; Nagas, E.; Ertan, A.; Ozgunaltay, G. Fracture Resistance of Endodontically Treated Teeth Restored With Bulk Fill, Bulk Fill Flowable, Fiber-reinforced, and Conventional Resin Composite. Oper. Dent. 2016, 41, E131–E140. [Google Scholar] [CrossRef]
- Loguercio, A.D.; Reis, A.; Schroeder, M.; Balducci, I.; Versluis, A.; Ballester, R.Y. Polymerization shrinkage: Effects of boundary conditions and filling technique of resin composite restorations. J. Dent. 2004, 32, 459–470. [Google Scholar] [CrossRef] [PubMed]
- Kaisarly, D.; El Gezawi, M.; Nyamaa, I.; Rösch, P.; Kunzelmann, K.H. Effects of boundary condition on shrinkage vectors of a flowable composite in experimental cavity models made of dental substrates. Clin. Oral. Investig. 2019, 23, 2403–2411. [Google Scholar] [CrossRef] [PubMed]
- Tekçe, N.; Aydemir, S.; Demirci, M.; Tuncer, S.; Bozkaya, S.; Sevilay Yıldırım, E.; Akman, Ş. Evaluation of fracture strength and total void amount in composite restorations on endodontically treated teeth. Odovtos Int. J. Dent. Sci. 2021, 23, 75–86. [Google Scholar] [CrossRef]
- Boscatto, R.H.; Prado, M.; Silva, E.J.N.L.; de Lima, C.O.; de-Jesus-Soares, A.; Frozoni, M. Influence of the endodontic access cavity design and restorative technique on hard tissue removal and fracture resistance of mandibular premolars. Res. Soc. Dev. 2022, 11, e18511124575. [Google Scholar] [CrossRef]
- Zarow, M.; Dominiak, M.; Szczeklik, K.; Hardan, L.; Bourgi, R.; Cuevas-Suárez, C.E.; Zamarripa-Calderón, J.E.; Kharouf, N.; Filtchev, D. Effect of Composite Core Materials on Fracture Resistance of Endodontically Treated Teeth: A Systematic Review and Meta-Analysis of In Vitro Studies. Polymers 2021, 13, 2251. [Google Scholar] [CrossRef]
- Özyürek, T.; Ülker, Ö.; Demiryürek, E.; Yılmaz, F. The Effects of Endodontic Access Cavity Preparation Design on the Fracture Strength of Endodontically Treated Teeth: Traditional Versus Conservative Preparation. J. Endod. 2018, 44, 800–805. [Google Scholar] [CrossRef]
- Daniel, A.; Saleh, A.R.; Al-Jadaa, A.; Kheder, W. Impact of Access Cavity Design on Fracture Resistance of Endodontically Treated Maxillary First Premolar: In Vitro. Braz. Dent. J. 2024, 35, e245676. [Google Scholar] [CrossRef] [PubMed]
- Marchesan, M.A.; James, C.M.; Lloyd, A.; Morrow, B.R.; García-Godoy, F. Effect of access design on intracoronal bleaching of endodontically treated teeth: An ex vivo study. J. Esthet. Restor. Dent. 2018, 30, E61–E67. [Google Scholar] [CrossRef] [PubMed]
- Lenherr, P.; Allgayer, N.; Weiger, R.; Filippi, A.; Attin, T.; Krastl, G. Tooth discoloration induced by endodontic materials: A laboratory study. Int. Endod. J. 2012, 45, 942–949. [Google Scholar] [CrossRef] [PubMed]
- Elgezawi, M.; Hassan, K.; Alagl, A.; Al-Thobity, A.M.; Al-Mutairi, B.; Al-Houtan, T.; Sadaf, S. Complexity of comprehensive care treatments in undergraduate dental programs: The benefits of observing and assisting experienced faculty members. Saudi Dent. J. 2017, 29, 161–166. [Google Scholar] [CrossRef]

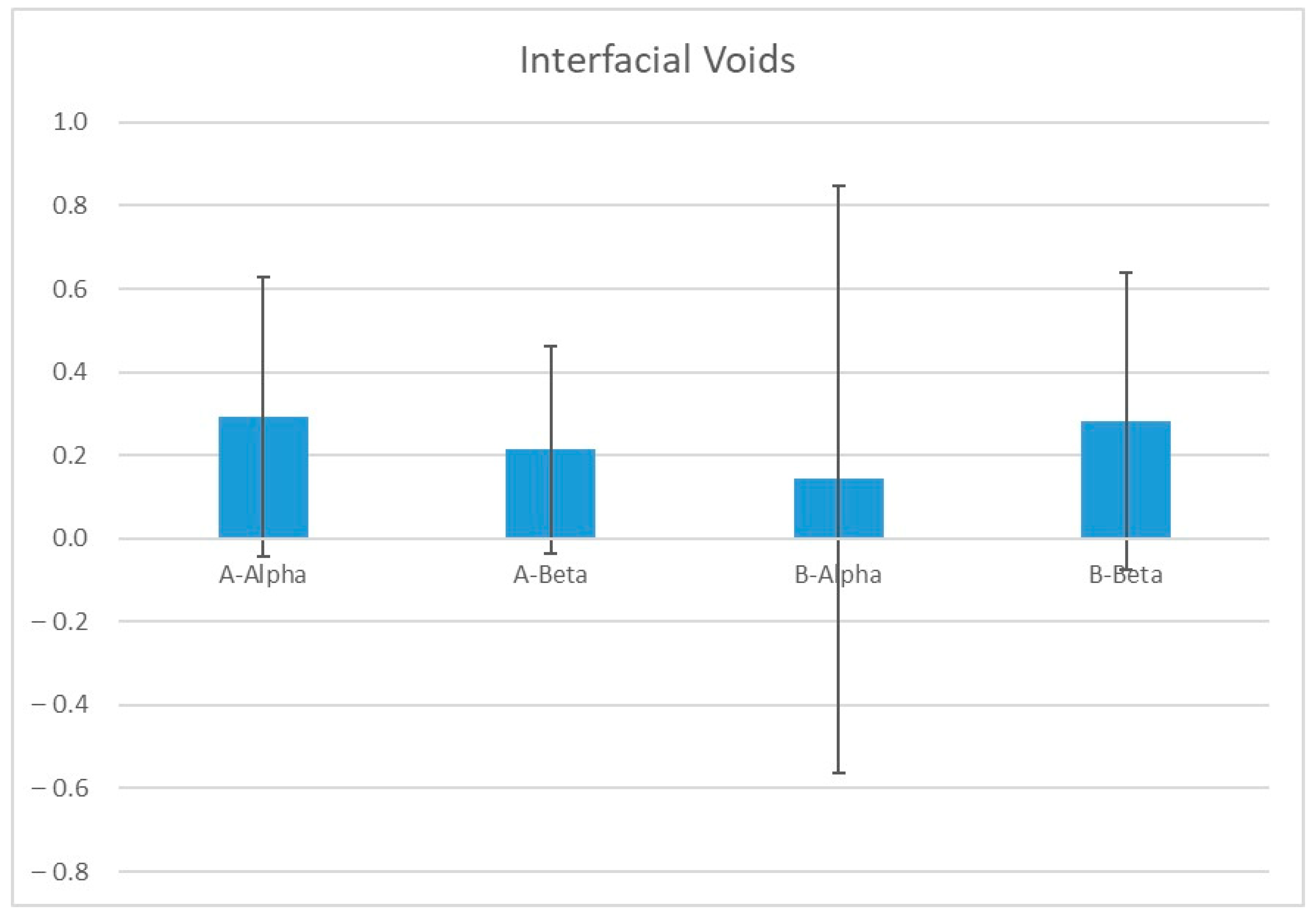
| (I) Group | (J) Group | Sig. (p-Value) | 95% Confidence Interval | |
|---|---|---|---|---|
| Lower Bound | Upper Bound | |||
| A-Alpha | A-Beta | 0.97 | −0.41 | 0.57 |
| B-Alpha | 0.85 | −0.34 | 0.64 | |
| B-Beta | 1.00 | −0.48 | 0.50 | |
| A-Beta | A-Alpha | 0.97 | −0.57 | 0.41 |
| B-Alpha | 0.98 | −0.42 | 0.56 | |
| B-Beta | 0.98 | −0.56 | 0.42 | |
| B-Alpha | A-Alpha | 0.85 | −0.64 | 0.34 |
| A-Beta | 0.98 | −0.56 | 0.42 | |
| B-Beta | 0.87 | −0.63 | 0.35 | |
| B-Beta | A-Alpha | 1.00 | −0.50 | 0.48 |
| A-Beta | 0.98 | −0.42 | 0.56 | |
| B-Alpha | 0.87 | −0.35 | 0.63 | |
| No Penetration | Silver Nitrate Reaches up to 1/2 of Gingival Seat | Silver Nitrate Reaches up to More than 1/2 of Gingival Seat | Silver Nitrate Extends beyond the Axial wall | Silver Nitrate Reach up to Root Canal System | Total | |||
|---|---|---|---|---|---|---|---|---|
| Group | A-Alpha | Count | 10 | 1 | 0 | 0 | 1 | 12 |
| % within Group | 83.3% | 8.3% | 0% | 0% | 8.3% | 100% | ||
| A-Beta | Count | 8 | 2 | 1 | 1 | 0 | 12 | |
| % within Group | 66.7% | 16.7% | 8.3% | 8.3% | 0% | 100% | ||
| B-Alpha | Count | 12 | 0 | 0 | 0 | 0 | 12 | |
| % within Group | 100% | 0% | 0% | 0% | 0% | 100% | ||
| B-Beta | Count | 7 | 1 | 4 | 0 | 0 | 12 | |
| % within Group | 58.3% | 8.3% | 33.3% | 0% | 0% | 100% | ||
| Total | Count | 37 | 4 | 5 | 1 | 1 | 48 | |
| % within Group | 77.1% | 8.3% | 10.4% | 2.1% | 2.1% | 100% | ||
| Pearson Chi-Square (p-value) | 0.110 | |||||||
| (I) Group | (J) Group | Sig. (p-Value) | 95% Confidence Interval | |
|---|---|---|---|---|
| Lower Bound | Upper Bound | |||
| A-Alpha | A-Beta | 0.97 | −134.34 | 207.13 |
| B-Alpha | 0.80 | −103.58 | 237.89 | |
| B-Beta | 0.83 | −106.46 | 235.00 | |
| Control | 1.00 | −178.41 | 163.05 | |
| A-Beta | A-Alpha | 0.97 | −207.13 | 134.34 |
| B-Alpha | 0.99 | −139.97 | 201.49 | |
| B-Beta | 0.99 | −142.86 | 198.61 | |
| Control | 0.95 | −214.81 | 126.66 | |
| B-Alpha | A-Alpha | 0.80 | −237.89 | 103.58 |
| A-Beta | 0.99 | −201.49 | 139.97 | |
| B-Beta | 1.00 | −173.62 | 167.85 | |
| Control | 0.73 | −245.57 | 95.90 | |
| B-Beta | A-Alpha | 0.83 | −235.00 | 106.46 |
| A-Beta | 0.99 | −198.61 | 142.86 | |
| B-Alpha | 1.00 | −167.85 | 173.62 | |
| Control | 0.76 | −242.68 | 98.78 | |
| Control | A-Alpha | 1.00 | −163.05 | 178.41 |
| A-Beta | 0.95 | −126.66 | 214.80 | |
| B-Alpha | 0.73 | −95.90 | 245.57 | |
| B-Beta | 0.76 | −98.78 | 242.68 | |
| Fracture Resistance | Sealing Ability | |||
|---|---|---|---|---|
| Spearman’s rho | Fracture resistance | Correlation Coefficient | 1.00 | 0.226 |
| Sig. (2-tailed) | . | 0.123 | ||
| n | 60 | 48 | ||
| Sealing Ability | Correlation Coefficient | 0.226 | 1.00 | |
| Sig. (2-tailed) | 0.123 | . | ||
| n | 48 | 48 | ||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Assalman, A.S.; Al Onaizan, F.; Elgezawi, M.; Almulhim, K.S.; Abdallah, M.A.; Kaisarly, D. Influence of Endodontic Cavity Design on Interfacial Voids, Class II Resin Composites Sealing Ability and Tooth Fracture Resistance: An In Vitro Study. J. Clin. Med. 2024, 13, 6024. https://doi.org/10.3390/jcm13196024
Assalman AS, Al Onaizan F, Elgezawi M, Almulhim KS, Abdallah MA, Kaisarly D. Influence of Endodontic Cavity Design on Interfacial Voids, Class II Resin Composites Sealing Ability and Tooth Fracture Resistance: An In Vitro Study. Journal of Clinical Medicine. 2024; 13(19):6024. https://doi.org/10.3390/jcm13196024
Chicago/Turabian StyleAssalman, Abdurrahman S., Faisal Al Onaizan, Moataz Elgezawi, Khalid S. Almulhim, Moamen A. Abdallah, and Dalia Kaisarly. 2024. "Influence of Endodontic Cavity Design on Interfacial Voids, Class II Resin Composites Sealing Ability and Tooth Fracture Resistance: An In Vitro Study" Journal of Clinical Medicine 13, no. 19: 6024. https://doi.org/10.3390/jcm13196024








