Antepartum Fetal Surveillance and Optimal Timing of Delivery in Diabetic Women: A Narrative Review
Abstract
1. Introduction
2. Methods
3. Results
3.1. Non-Stress Test
3.2. Biophysical Profile
3.3. Contraction Stress Test (CST)
3.4. Ultrasound and Amniotic Fluid Analysis
Fetal Doppler Ultrasound
3.5. Antepartum Fetal Surveillance Tests and Large for Gestational Age Neonates
3.6. Pregnancy Resolution
4. Discussion
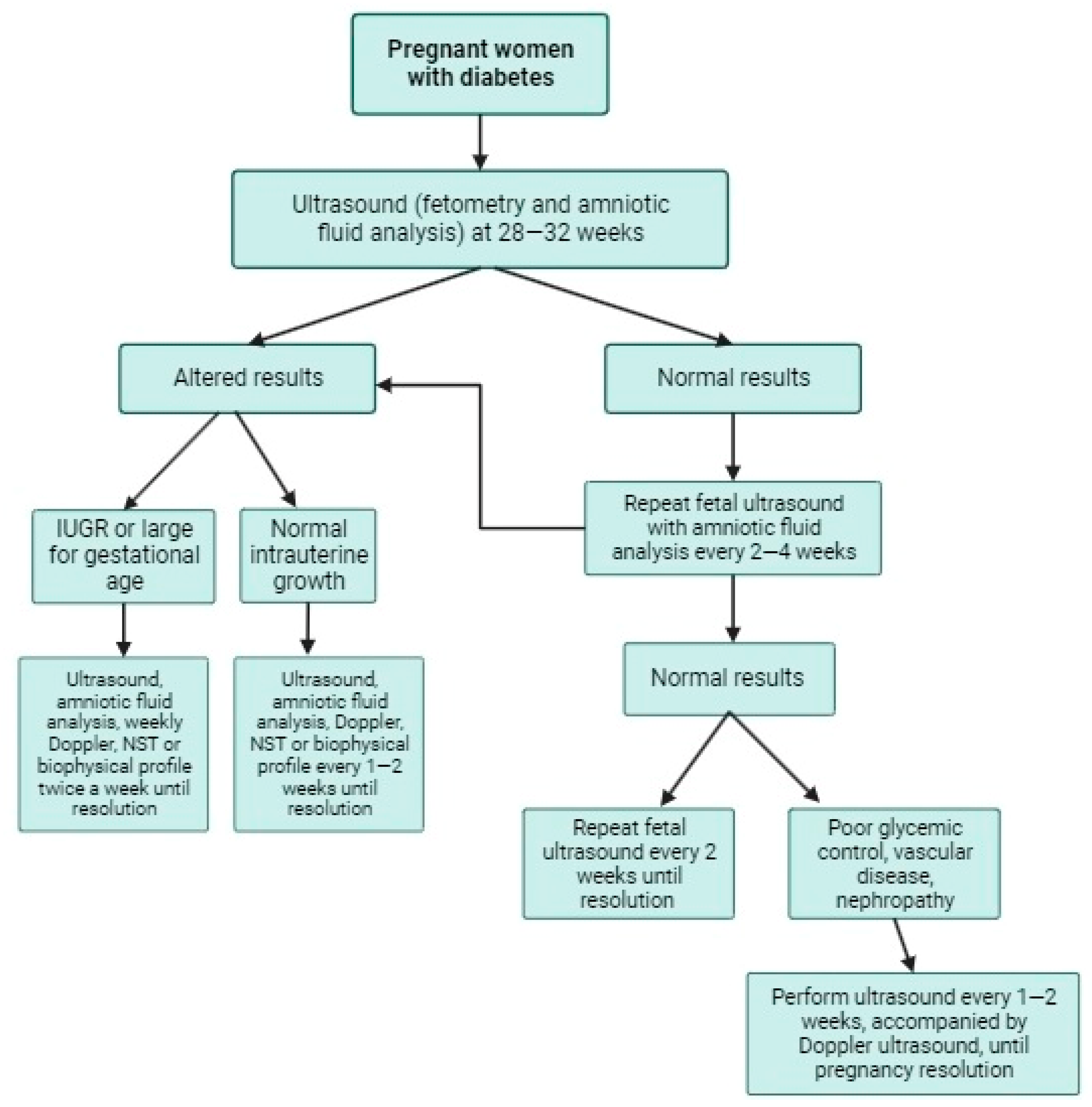
4.1. Evidence-Based Proposal for Fetal Surveillance in Diabetic Pregnant Women
4.2. Optimal Timing for Delivery in Diabetic Women
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- ElSayed, N.; Aleppo, G.; Aroda, V.; Bannuru, R.; Brown, F.; Bruemmer, D.; Collins, B.; Hilliard, M.; Isaacs, D.; Johnson, E.; et al. Management of Diabetes in Pregnancy: Standards of Care in Diabetes—2023. Diabetes Care 2023, 46 (Suppl. 1), S254–S266. [Google Scholar] [CrossRef] [PubMed]
- Biesty, L.M.; Egan, A.M.; Dunne, F.; Smith, V.; Meskell, P.; Dempsey, E.; Bhuinneain, G.M.N.; Devane, D. Planned birth at or near term for improving health outcomes for pregnant women with pre-existing diabetes and their infants. Cochrane Database Syst. Rev. 2018, 2, Cd012948. [Google Scholar] [CrossRef] [PubMed]
- American College of Obstetricians and Gynecologists. “Gestational Diabetes Mellitus” ACOG Practice Bulletin No. 190. Obstet. Gynecol. 2018, 131, e49–e64. [Google Scholar] [CrossRef] [PubMed]
- International Diabetes Federation. IDF Diabetes Atlas 10th Edition 2021. Available online: https://diabetesatlas.org/idfawp/resource-files/2021/07/IDF_Atlas_10th_Edition_2021.pdf (accessed on 20 June 2023).
- Reyes-Muñoz, E.; Parra, A.; Castillo-Mora, A.; Ortega-González, C. Effect of the diagnostic criteria of the International Association of Diabetes and Pregnancy Study Groups on the prevalence of gestational diabetes mellitus in urban Mexican women: A cross-sectional study. Endocr. Pract. 2012, 18, 146–151. [Google Scholar] [CrossRef]
- Reyes-Muñoz, E.; Castellanos-Barroso, G.; Ramírez-Eugenio, B.; Ortega-González, C.; Parra, A.; Castillo-Mora, A.; De La Jara-Díaz, J. The Risk of Gestational Diabetes Mellitus among Mexican Women with a History of Infertility and Polycystic Ovary Syndrome. Fertil. Steril. 2012, 97, 1467–1471. [Google Scholar] [CrossRef] [PubMed]
- Dainelli, L.; Prieto-Patron, A.; Silva-Zolezzi, I.; Sosa-Rubi, S.; Espino, S.; Reyes-Muñoz, E.; Lopez-Ridaura, R.; Detzel, P. Screening and Management of Gestational Diabetes in Mexico: Results from a Survey of Multilocation, Multi-Health Care Institution Practitioners. Diabetes Metab. Syndr. Obes. 2018, 11, 105–116. [Google Scholar] [CrossRef]
- ElSayed, N.A.; Aleppo, G.; Aroda, V.R.; Bannuru, R.R.; Brown, F.M.; Bruemmer, D.; Collins, B.S.; Gaglia, J.L.; Hilliard, M.E.; Isaacs, D.; et al. 2. Classification and Diagnosis of Diabetes: Standards of Care in Diabetes—2023. Diabetes Care 2023, 46 (Suppl. 1), S19–S40. [Google Scholar] [CrossRef]
- Dłuski, D.F.; Ruszała, M.; Rudziński, G.; Pożarowska, K.; Brzuszkiewicz, K.; Leszczyńska-Gorzelak, B. Evolution of Gestational Diabetes Mellitus across Continents in 21st Century. Int. J. Environ. Res. Public Health 2022, 19, 15804. [Google Scholar] [CrossRef]
- Ioannis, T.; Giouleka, S.; Mamopoulos, A.; Kourtis, A.; Athanasiadis, A.; Filopoulou, D.; Dagklis, T. Diagnosis and Management of Gestational Diabetes Mellitus: An Overview of National and International Guidelines. Obstet. Gynecol. Surv. 2021, 76, 367–381. [Google Scholar] [CrossRef]
- National Institute for Health and Care Excellence. Diabetes in Pregnancy: Management from Preconception to the Postnatal Period. National Institute for Health and Care Excellence: Guidelines; National Institute for Health and Care Excellence (NICE): London, UK, 2020. Available online: http://www.ncbi.nlm.nih.gov/books/NBK555331/ (accessed on 21 May 2023).
- Berger, H.; Gagnon, R.; Sermer, M. Guideline No. 393-Diabetes in Pregnancy. J. Obstet. Gynaecol. Can. 2019, 41, 1814–1825. [Google Scholar] [CrossRef]
- Hod, M.; Kapur, A.; Sacks, D.A.; Hadar, E.; Agarwal, M.; Di Renzo, G.C.; Cabero-Roura, L.; McIntyre, H.D.; Morris, J.L.; Divakar, H. The International Federation of Gynecology and Obstetrics (FIGO) Initiative on Gestational Diabetes Mellitus: A Pragmatic Guide for Diagnosis, Management, and Care. Int. J. Gynaecol. Obstet. 2015, 131 (Suppl. 3), S173–S211. [Google Scholar] [CrossRef] [PubMed]
- Blumer, I.; Hadar, E.; Hadden, D.; Jovanovič, L.; Mestman, J.; Murad, H.; Yogev, Y. Diabetes and pregnancy: An endocrine society clinical practice guideline. J. Clin. Endocrinol. Metab. 2013, 98, 4227–4249. [Google Scholar] [CrossRef] [PubMed]
- International Association of Diabetes and Pregnancy Study Groups Consensus Panel. International Association of Diabetes and Pregnancy Study Groups Recommendations on the Diagnosis and Classification of Hyperglycemia in Pregnancy. Diabetes Care 2010, 33, 676–682. [Google Scholar] [CrossRef]
- Lende, M.; Rijhsinghani, A. Gestational Diabetes: Overview with Emphasis on Medical Management. Int. J. Environ. Res. Public Health 2020, 17, 9573. [Google Scholar] [CrossRef] [PubMed]
- Plows, J.; Stanley, A.; Baker, P.; Reynolds, C.; Vickers, M. The Pathophysiology of Gestational Diabetes Mellitus. Int. J. Mol. Sci. 2018, 19, 3342. [Google Scholar] [CrossRef] [PubMed]
- Damhuis, S.E.; Ganzevoort, W.; Gordijn, S.J. Abnormal Fetal Growth: Small for Gestational Age, Fetal Growth Restriction, Large for Gestational Age: Definitions and Epidemiology. Obstet. Gynecol. Clin. N. Am. 2021, 48, 267–279. [Google Scholar] [CrossRef] [PubMed]
- Kondracki, A.J.; Valente, M.J.; Ibrahimou, B.; Bursac, Z. Risk of large for gestational age births at early, full and late term in relation to pre-pregnancy body mass index: Mediation by gestational diabetes status. Paediatr. Perinat. Epidemiol. 2022, 36, 566–576. [Google Scholar] [CrossRef]
- American College of Obstetricians and Gynecologists’ Committee on Practice Bulletins—Obstetrics. ACOG Practice Bulletin No. 201: Pregestational Diabetes Mellitus. Obstet. Gynecol. 2018, 132, e228–e248. [Google Scholar] [CrossRef]
- Shub, A.; Lappas, M. Pregestational Diabetes in Pregnancy: Complications, Management, Surveillance, and Mechanisms of Disease—A Review. Prenat. Diagn. 2020, 40, 1092–1098. [Google Scholar] [CrossRef]
- Alfirevic, Z.; Stampalija, T.; Dowswell, T. Fetal and umbilical Doppler ultrasound in high-risk pregnancies. Cochrane Database Syst. Rev. 2017, 6, CD007529. [Google Scholar] [CrossRef]
- Ye, W.; Luo, C.; Huang, J.; Li, C.; Liu, Z.; Liu, F. Gestational diabetes mellitus and adverse pregnancy outcomes: Systematic review and meta-analysis. BMJ 2022, 377, e067946. [Google Scholar] [CrossRef] [PubMed]
- Pillay, J.; Donovan, L.; Guitard, S.; Zakher, B.; Gates, M.; Gates, A.; Vandermeer, B.; Bougatsos, C.; Chou, R.; Hartling, L. Screening for Gestational Diabetes: Updated Evidence Report and Systematic Review for the US Preventive Services Task Force. JAMA 2021, 326, 539–562. [Google Scholar] [CrossRef] [PubMed]
- Signore, C.; Spong, C. Overview of Antepartum Fetal Assessment. UpToDate [Internet]. 2023. Available online: https://www.uptodate.com/contents/overview-of-antepartum-fetal-assessment (accessed on 19 April 2023).
- Della Gatta, A.N.; Aceti, A.; Spinedi, S.F.; Martini, S.; Corvaglia, L.; Sansavini, A.; Zuccarini, M.; Lenzi, J.; Seidenari, A.; Dionisi, C.; et al. Neurodevelopmental outcomes of very preterm infants born following early foetal growth restriction with absent end-diastolic umbilical flow. Eur. J. Pediatr. 2023, 182, 4467–4476. [Google Scholar] [CrossRef] [PubMed]
- Baschat, A.A.; Cosmi, E.; Bilardo, C.M.; Wolf, H.; Berg, C.; Rigano, S.; Germer, U.; Moyano, D.; Turan, S.; Hartung, J.; et al. Predictors of neonatal outcome in early-onset placental dysfunction. Obstet. Gynecol. 2007, 109 Pt 1, 253–261. [Google Scholar] [CrossRef] [PubMed]
- Sapoval, J.; Singh, V.; Carter, R. Ultrasound Biophysical Profile. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2023. Available online: http://www.ncbi.nlm.nih.gov/books/NBK539866/ (accessed on 21 May 2023).
- American College of Obstetricians and Gynecologists. Antepartum Fetal Surveillance: ACOG Practice Bulletin, Number 229. Obstet. Gynecol. 2021, 137, e116–e127. [Google Scholar] [CrossRef] [PubMed]
- American College of Obstetricians and Gynecologists. Practice Bulletin No. 201 Summary: Pregestational Diabetes Mellitus. Obstet. Gynecol. 2018, 132, 1514–1516. [Google Scholar] [CrossRef] [PubMed]
- Manning, F.A. Fetal biophysical profile. Obstet. Gynecol. Clin. N. Am. 1999, 26, 557–577. [Google Scholar] [CrossRef] [PubMed]
- Baschat, A.A.; Galan, H.L.; Lee, W.; DeVore, G.R.; Mari, G.; Hobbins, J.; Vintzileos, A.; Platt, L.D.; Manning, F.A. The role of the fetal biophysical profile in the management of fetal growth restriction. Am. J. Obstet. Gynecol. 2022, 226, 475–486. [Google Scholar] [CrossRef]
- David, A.L.; Spencer, R.N. Clinical Assessment of Fetal Well-Being and Fetal Safety Indicators. J. Clin. Pharmacol. 2022, 62 (Suppl. 1), S67–S78. [Google Scholar] [CrossRef]
- Salama, M.H.; Rizk, H.H.; Nawara, M. Frequency of third trimester umbilical artery Doppler for improving neonatal outcomes in high-risk pregnancies: A randomized trial. Obstet. Gynecol. Sci. 2023, 66, 161–168. [Google Scholar] [CrossRef]
- Carter, E.B.; Stockburger, J.; Tuuli, M.G.; Macones, G.A.; Odibo, A.O.; Trudell, A.S. Large-for-gestational age and stillbirth: Is there a role for antenatal testing? Ultrasound Obstet. Gynecol. 2019, 54, 334–337. [Google Scholar] [CrossRef] [PubMed]
- McElwee, E.R.; Oliver, E.A.; McFarling, K.; Haney, A.; Cuff, R.; Head, B.; Karanchi, H.; Loftley, A.; Finneran, M.M. Risk of stillbirth in pregnancies complicated by diabetes, stratified by fetal growth. Obstet. Gynecol. 2023, 141, 801–809. [Google Scholar] [CrossRef] [PubMed]
- Nompumelelo, M.; Masete, M.; Adam, S.; Dias, S.; Nyawo, T.; Pheiffer, C. A Systematic Review to Compare Adverse Pregnancy Outcomes in Women with Pregestational Diabetes and Gestational Diabetes. Int. J. Environ. Res. Public Health 2022, 19, 10846. [Google Scholar] [CrossRef]
- Ornoy, A.; Becker, M.; Weinstein-Fudim, L.; Ergaz, Z. Diabetes during Pregnancy: A Maternal Disease Complicating the Course of Pregnancy with Long-Term Deleterious Effects on the Offspring. A Clinical Review. Int. J. Mol. Sci. 2021, 22, 2965. [Google Scholar] [CrossRef]
- Xiang, A.; Wang, X.; Martinez, M.P.; Page, K.; Buchanan, T.A.; Feldman, R.K. Maternal Type 1 Diabetes and Risk of Autism in Offspring. JAMA 2018, 320, 89–91. [Google Scholar] [CrossRef]
- Li, X.; Li, T.T.; Tian, R.X.; Fei, J.J.; Wang, X.X.; Yu, H.H.; Yin, Z.Z. Gestational diabetes mellitus: The optimal time of delivery. World J. Diabetes 2023, 14, 179–187. [Google Scholar] [CrossRef]
- Metcalfe, A.; Hutcheon, J.A.; Sabr, Y.; Lyons, J.; Burrows, J.; Donovan, L.E.; Joseph, K.S. Timing of delivery in women with diabetes: A population-based study. Acta Obstet. Gynecol. Scand. 2020, 99, 341–349. [Google Scholar] [CrossRef]
| Risk Factors | ||
|---|---|---|
| Maternal age ≥ 25 years | Presence of twin pregnancy | Previous history of polycystic ovary syndrome |
| Belonging to the Hispanic, Asian, or African American ethnic group | Previous history of a child with birth weight > 4000 g or delivery of large for gestational age infant | Presence of glycosuria |
| Sedentary lifestyle | Excessive weight gain during pregnancy | Previous history of prediabetes (carbo-hydrate intolerance) |
| Family history of type 2 diabetes in a first-degree relative | Previous history of preeclampsia or hypertension during pregnancy | Presence of acanthosis nigricans |
| Hemoglobin A1C ≥ 5.7%, HDL cholesterol < 35 mg/dL, Triglycerides > 250 mg/dL | Previous history of gestational diabetes | Previous history of cardiovascular disease |
| Guideline | Glucose Load | Fasting (mg/dL)/mmol/L | 1-h (mg/dL)/mmol/L | 2-h (mg/dL)/mmol/L | 3-h (mg/dL)/mmol/L |
|---|---|---|---|---|---|
| American Diabetes Association (2023) [1] | 75 g * | ≥92/5.1 | ≥180/10 | ≥153/8.5 | |
| American Diabetes Association (2023) [1] | 100 g ** | ≥95/5.3 | ≥180/10 | ≥155/8.6 | ≥140/7.8 |
| National Institute for Health and Care Excellence (2020) [11] | 75 g * | ≥100/5.6 | − | ≥140/7.8 | |
| Society of Obstetricians and Gynaecologists of Canada (2019) *** [12] | 75 g ** | ≥95/5.3 | ≥190/10.6 | ≥162/8.9 | |
| American College of Obstetricians and Gynecologists (2018) [3] | 100 g ** | ≥95/5.3 | ≥180/10 | ≥155/8.6 | ≥140/7.8 |
| Federation of Obstetrics and Gynecology (2015) [13] | 75 g * | ≥92/5.1 | ≥180/10 | ≥153/8.5 | |
| Endocrine Society (2013) [14] | 75 g * | ≥92/5.1 | ≥180/10 | ≥153/8.5 | |
| International Association of the Diabetes and Pregnancy Study Groups (2010) [15] | 75 g * | ≥92/5.1 | ≥180/10 | ≥153/8.5 |
| ACOG | NICE | FIGO | Other | |
|---|---|---|---|---|
| Non-Stress Test | Weekly evaluation starting at 36 weeks of gestation. | No recommended | According to local protocol. | SOGC: Weekly evaluation starting at 36 weeks of gestation. |
| Biophysical Profile | Starting at 32 weeks of gestation. Follow-up twice a week in case of abnormalities. | No recommended | According to local protocol. | ADA: Starting at 32 weeks of gestation. Weekly follow-up. |
| Contraction Stress Test | Starting between 32 and 34 weeks of gestation. Controversial use. | Not discussed. | Not discussed. | Not discussed. |
| Ultrasound and Amniotic Fluid Analysis | Starting at 32 weeks of gestation. Growth ultrasound between 34 and 36 weeks of gestation. | Starting at 28 weeks of gestation, followed by evaluations at 32, 36 and 38–39 weeks of gestation. | Performing ultrasound every two to four weeks from the diagnosis until resolution of pregnancy. | SOGC: Starting with fetal ultrasound at 36 weeks of gestation, followed by weekly follow-up. |
| Fetal Doppler Ultrasound | Non-discussed. Used in high-risk pregnancies. | Used in pregnancies complicated with fetal growth restriction. | Non-discussed. Used in high-risk pregnancies. | Non-discussed. Used in high-risk pregnancies. |
| ACOG | NICE | FIGO | Other | |
|---|---|---|---|---|
| Non-Stress Test | Weekly evaluation starting at 36 weeks of gestation. | Weekly at 38 weeks of gestation. Could start before in risk of fetal growth restriction | According to local protocol. | SOGC: Weekly evaluation starting at 36 weeks of gestation. |
| Biophysical Profile | Starting at 32 weeks of gestation. Follow-up twice a week in case of abnormalities. | Recommended after 32 weeks of pregnancy and can be performed earlier in cases of high risk of stillbirth | According to local protocol. | ADA: Starting at 32 weeks of gestation. Weekly follow-up. |
| Contraction Stress Test | Starting between 32 and 34 weeks of gestation. Controversial use. | Not discussed. | Not discussed. | Not discussed. |
| Ultrasound and Amniotic Fluid Analysis | Starting at 32 weeks of gestation. Growth ultrasound between 34 and 36 weeks of gestation. Amniotic fluid assessment starting at 32 weeks. | Starting at 28 weeks of gestation, followed by evaluations at 32, 36 and 38–39 weeks of gestation. | Performing ultrasound every two to four weeks until resolution of pregnancy. | SOGC: Starting with fetal ultrasound at 36 weeks of gestation, followed by weekly follow-up. |
| Fetal Doppler Ultrasound | Non-discussed. Used in high-risk pregnancies. | Used in pregnancies complicated with fetal growth restriction. | Non-discussed. Used in high-risk pregnancies. | Non-discussed. Used in high-risk pregnancies. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Braverman-Poyastro, A.; Suárez-Rico, B.V.; Borboa-Olivares, H.; Espino y Sosa, S.; Torres-Torres, J.; Arce-Sánchez, L.; Martínez-Cruz, N.; Reyes-Muñoz, E. Antepartum Fetal Surveillance and Optimal Timing of Delivery in Diabetic Women: A Narrative Review. J. Clin. Med. 2024, 13, 313. https://doi.org/10.3390/jcm13020313
Braverman-Poyastro A, Suárez-Rico BV, Borboa-Olivares H, Espino y Sosa S, Torres-Torres J, Arce-Sánchez L, Martínez-Cruz N, Reyes-Muñoz E. Antepartum Fetal Surveillance and Optimal Timing of Delivery in Diabetic Women: A Narrative Review. Journal of Clinical Medicine. 2024; 13(2):313. https://doi.org/10.3390/jcm13020313
Chicago/Turabian StyleBraverman-Poyastro, Alan, Blanca Vianey Suárez-Rico, Héctor Borboa-Olivares, Salvador Espino y Sosa, Johnatan Torres-Torres, Lidia Arce-Sánchez, Nayeli Martínez-Cruz, and Enrique Reyes-Muñoz. 2024. "Antepartum Fetal Surveillance and Optimal Timing of Delivery in Diabetic Women: A Narrative Review" Journal of Clinical Medicine 13, no. 2: 313. https://doi.org/10.3390/jcm13020313
APA StyleBraverman-Poyastro, A., Suárez-Rico, B. V., Borboa-Olivares, H., Espino y Sosa, S., Torres-Torres, J., Arce-Sánchez, L., Martínez-Cruz, N., & Reyes-Muñoz, E. (2024). Antepartum Fetal Surveillance and Optimal Timing of Delivery in Diabetic Women: A Narrative Review. Journal of Clinical Medicine, 13(2), 313. https://doi.org/10.3390/jcm13020313







