Patient Involvement in the Rehabilitation Process Is Associated with Improvement in Function and Goal Attainment: Results from an Explorative Longitudinal Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design, Participants, Setting, and Data Collection
2.2. Variables
2.3. Statistics
2.4. Ethics
2.5. Patient Research Partner Involvement
3. Results
3.1. Patient Involvement in the Rehabilitation Process
3.2. Associations between Patient Characteristics and Involvement in Goal-Setting
3.3. Associations between Involvement in Goal-Setting and Improvements in Functioning
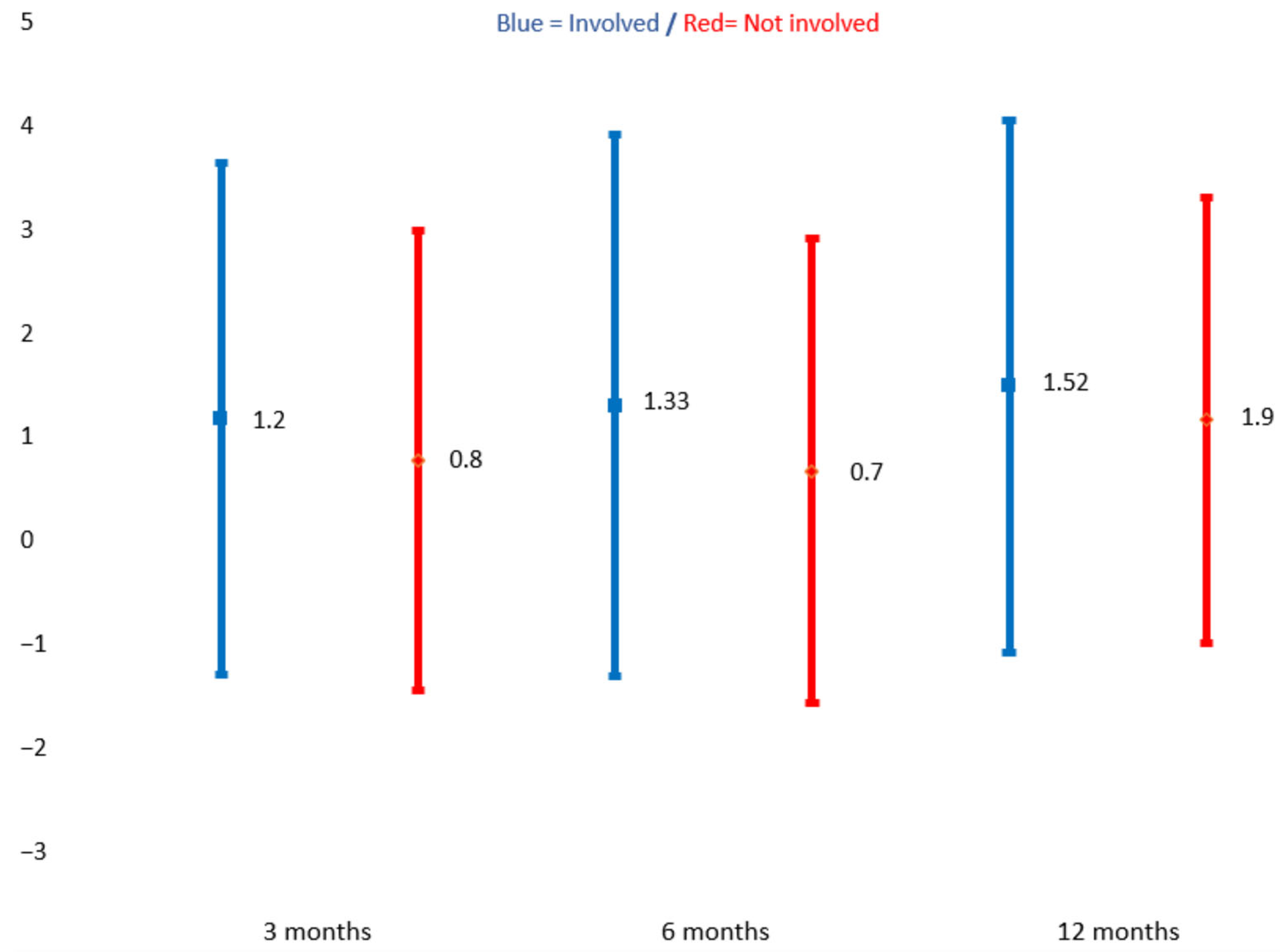
3.4. Associations between Patient Characteristics, Involvement in the Rehabilitation Process, and Goal Attainment
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization (WHO). Quality of Care. Available online: https://www.who.int/health-topics/quality-of-care#tab=tab_1 (accessed on 20 September 2023).
- Sheikh, S.A.; Donaldson, L.; Dhingra-Kumar, N.; Bates, D.; Kelley, E.; Larizgoitia, I.; Panesar, S.; Singh, C.; de Silva, D.; Valderas, J.; et al. Patient Engagement: Technical Series on Safer Primary Care; WHO: Geneva, Switzerland, 2016.
- Steele Gray, C.; Grudniewicz, A.; Armas, A.; Mold, J.; Im, J.; Boeckxstaens, P. Goal-Oriented Care: A Catalyst for Person-Centred System Integration. Int. J. Integr. Care 2020, 20, 8. [Google Scholar] [CrossRef] [PubMed]
- Coulter, A.; Oldham, J. Person-centred care: What is it and how do we get there? Future Hosp. J. 2016, 3, 114–116. [Google Scholar] [CrossRef] [PubMed]
- Andreassen, T.A. Service user involvement and repositioning of healthcare professionals: A framework for examining implications of different forms of involvement. Nordisk Välfärdsforskning|Nordic. Welfare Res. 2018, 3, 58–69. [Google Scholar] [CrossRef]
- World Health Organization. World Report on Disability; WHO: Geneva, Switzerland, 2011. Available online: https://www.who.int/publications/i/item/9789241564182. (accessed on 1 September 2023).
- Spijk-de Jonge, M.J.; Weijers, J.M.; Teerenstra, S.; Elwyn, G.; van de Laar, M.A.; van Riel, P.L.; Huis, A.M.; Hulscher, M.E. Patient involvement in rheumatoid arthritis care to improve disease activity-based management in daily practice: A randomized controlled trial. Patient Educ. Couns. 2022, 105, 1244–1253. [Google Scholar] [CrossRef] [PubMed]
- Kang, E.; Kim, M.Y.; Lipsey, K.L.; Foster, E.R. Person-Centered Goal Setting: A Systematic Review of Intervention Components and Level of Active Engagement in Rehabilitation Goal-Setting Interventions. Arch. Phys. Med. Rehabil. 2022, 103, 121–130.e123. [Google Scholar] [CrossRef] [PubMed]
- Rosengren, K.; Brannefors, P.; Carlstrom, E. Adoption of the concept of person-centred care into discourse in Europe: A systematic literature review. J. Health Organ. Manag. 2021, 35, 265–280. [Google Scholar] [CrossRef]
- Flynn, K.E.; Smith, M.A.; Vanness, D. A typology of preferences for participation in healthcare decision making. Soc. Sci. Med. 2006, 63, 1158–1169. [Google Scholar] [CrossRef]
- Sagen, J.S.; Smedslund, G.; Simonsen, A.E.; Habberstad, A.; Kjeken, I.; Dagfinrud, H.; Moe, R.H. Patient engagement in the development and delivery of healthcare services: A systematic scoping review. BMJ Open Qual. 2023, 12, e002309. [Google Scholar] [CrossRef]
- Rose, A.; Rosewilliam, S.; Soundy, A. Shared decision making within goal setting in rehabilitation settings: A systematic review. Patient Educ. Couns. 2017, 100, 65–75. [Google Scholar] [CrossRef]
- Siegert, R.J.; Taylor, W.J. Theoretical aspects of goal-setting and motivation in rehabilitation. Disabil. Rehabil. 2004, 26, 1–8. [Google Scholar] [CrossRef]
- Pasient- og brukerrettighetsloven. Lov om pasient- og brukerrettigheter (LOV-2023-12-20-106). Lovdata. 2001. §3. Available online: https://lovdata.no/lov/1999-07-02-63 (accessed on 28 December 2023).
- Sand-Svartrud, A.L.; Berdal, G.; Azimi, M.; Bø, I.; Dager, T.N.; Eppeland, S.G.; Fredheim, G.O.; Hagland, A.S.; Klokkeide, Å.; Linge, A.D.; et al. Associations between quality of health care and clinical outcomes in patients with rheumatic and musculoskeletal diseases: A rehabilitation cohort study. BMC Musculoskelet Disord. 2022, 23, 357. [Google Scholar] [CrossRef] [PubMed]
- Yun, D.; Choi, J. Person-centered rehabilitation care and outcomes: A systematic literature review. Int. J. Nurs. Stud. 2019, 93, 74–83. [Google Scholar] [CrossRef] [PubMed]
- Smit, E.B.; Bouwstra, H.; Hertogh, C.M.; Wattel, E.M.; van der Wouden, J.C. Goal-setting in geriatric rehabilitation: A systematic review and meta-analysis. Clin. Rehabil. 2019, 33, 395–407. [Google Scholar] [CrossRef] [PubMed]
- Johansen, I.; Klokkerud, M.; Anke, A.; Børke, J.B.; Glott, T.; Hauglie, U.; Høyem, A.; Klovning, A.; Lande, K.A.; Larsen, M.; et al. A quality indicator set for use in rehabilitation team care of people with rheumatic and musculoskeletal diseases; development and pilot testing. BMC Health Serv. Res. 2019, 19, 265. [Google Scholar] [CrossRef] [PubMed]
- Sand-Svartrud, A.L.; Berdal, G.; Azimi, M.; Bø, I.; Dager, T.N.; Eppeland, S.G.; Fredheim, G.O.; Hagland, A.S.; Klokkeide, Å.; Linge, A.D.; et al. A quality indicator set for rehabilitation services for people with rheumatic and musculoskeletal diseases demonstrates adequate responsiveness in a pre-post evaluation. BMC Health Serv. Res. 2021, 21, 164. [Google Scholar] [CrossRef] [PubMed]
- Santana, M.J.; Manalili, K.; Jolley, R.J.; Zelinsky, S.; Quan, H.; Lu, M. How to practice person-centred care: A conceptual framework. Health Expect 2018, 21, 429–440. [Google Scholar] [CrossRef]
- Moseng, T.; Tveter, A.T.; Holm, I.; Dagfinrud, H. Pasient-Spesifikk Funksjonsskala. Et nyttig verktøy for fysioterpaeuter i primaerhelsetjenesten. Nor. J. Physiother. 2013, 2, 20–26. [Google Scholar]
- IBM Corp. IBM SPSS Statistics for Windows, version 28; IBM Corp: Armonk, NY, USA, 2021. [Google Scholar]
- Fairley, J.L.; Seneviwickrama, M.; Yeh, S.; Anthony, S.; Chou, L.; Cicuttini, F.M.; Sullivan, K.; Briggs, A.M.; Wluka, A.E. Person-centred care in osteoarthritis and inflammatory arthritis: A scoping review of people’s needs outside of healthcare. BMC Musculoskelet Disord. 2021, 22, 341. [Google Scholar] [CrossRef]
- Chi-Lun-Chiao, A.; Chehata, M.; Broeker, K.; Gates, B.; Ledbetter, L.; Cook, C.; Ahern, M.; Rhon, D.I.; Garcia, A.N. Patients’ perceptions with musculoskeletal disorders regarding their experience with healthcare providers and health services: An overview of reviews. Arch. Physiother. 2020, 10, 17. [Google Scholar] [CrossRef]
- Bergström, M.; Larsson Ranada, Å.; Sverker, A.; Thyberg, I.; Björk, M. A dyadic exploration of support in everyday life of persons with RA and their significant others. Scand J. Occup. Ther. 2023, 30, 616–627. [Google Scholar] [CrossRef]
- Jones, F. Strategies to enhance chronic disease self-management: How can we apply this to stroke? Disabil. Rehabil. 2006, 28, 841–847. [Google Scholar] [CrossRef] [PubMed]
- Valaas, H.L.; Klokkerud, M.; Hildeskår, J.; Hagland, A.S.; Kjønli, E.; Mjøsund, K.; Øie, L.; Wigers, S.H.; Eppeland, S.G.; Høystad, T.; et al. Follow-up care and adherence to self-management activities in rehabilitation for patients with rheumatic and musculoskeletal diseases: Results from a multicentre cohort study. Disabil. Rehabil. 2022, 44, 8001–8010. [Google Scholar] [CrossRef] [PubMed]
- Sand-Svartrud, A.L.; Berdal, G.; Aanerud, G.J.; Azimi, M.; Bjørnerud, A.M.; Nygaard Dager, T.; Van den Ende, C.H.M.; Johansen, I.; Lindtvedt Valaas, H.; Dagfinrud, H.; et al. Delivery of a quality improvement program in team-based rehabilitation for patients with rheumatic and musculoskeletal diseases: A mixed methods study. Disabil. Rehabil. 2023, 1–13. [Google Scholar] [CrossRef]
- Cott, C. Client-centred rehabilitation: Client perspectives. Disabil. Rehabil. 2004, 26, 1411–1422. [Google Scholar] [CrossRef] [PubMed]
- Leach, E.; Cornwell, P.; Fleming, J.; Haines, T. Patient centered goal-setting in a subacute rehabilitation setting. Disabil. Rehabil. 2010, 32, 159–172. [Google Scholar] [CrossRef] [PubMed]
- Kaplan, S.H.; Greenfield, S.; Ware, J.E., Jr. Assessing the effects of physician-patient interactions on the outcomes of chronic disease. Med. Care 1989, 27, S110–S127. [Google Scholar] [CrossRef] [PubMed]
- Le, C.; Finbråten, H.S.; Pettersen, K.S.; Joranger, P.; Guttersrud, Ø. Befolkningens Helsekompetanse, del I. The International Health Literacy Population Survey 2019–2021 (HLS19)–et Samarbeidsprosjekt Med Nettverket M-POHL tilknyttet WHO-EHII. Rapport IS-2959. 2021. Available online: https://www.researchgate.net/publication/348834876_Befolkningens_helsekompetanse_del_I_The_International_Health_Literacy_Population_Survey_2019-2021_HLS19_-_et_samarbeidsprosjekt_med_nettverket_M-POHL_tilknyttet_WHO-EHII_Rapport_IS-2959 (accessed on 28 December 2023).
- Aimée Hartford Kvæl, L.; Gautun, H. Social inequality in navigating the healthcare maze: Care trajectories from hospital to home via intermediate care for older people in Norway. Soc. Sci. Med. 2023, 333, 116142. [Google Scholar] [CrossRef]
- Chen, Z.-J.; Tang, F.-P.; Chang, S.-Y.; Chung, H.-L.; Tsai, W.-H.; Chou, S.-S.; Yeh, H.-C.; Tung, H.-H. Resilience-happiness nexus in community-dwelling middle-aged and older adults: Results from Gan-Dau Healthy Longevity Plan. Arch. Gerontol. Geriatr. 2024, 116, 105162. [Google Scholar] [CrossRef]
- Lin, Y.H.; Han, D.S.; Lee, Y.H.; Chan, D.C.; Chang, C.H.; Yang, K.C.; Chang, F.C. Social network associated with depressed mood and sarcopenia among older adults in Taiwan. J. Formos. Med. Assoc. 2023. Preprint. [Google Scholar] [CrossRef]
- Preede, L.; Soberg, H.L.; Dalen, H.; Nyquist, A.; Jahnsen, R.; Saebu, M.; Bautz-Holter, E.; Røe, C. Rehabilitation Goals and Effects of Goal Achievement on Outcome Following an Adapted Physical Activity-Based Rehabilitation Intervention. Patient Prefer. Adherence 2021, 15, 1545–1555. [Google Scholar] [CrossRef]
- Feiring, M. Rehabilitation—Between management and knowledge practices: An historical overview of public action in Norwegian welfare reforms. Policy Soc. 2012, 31, 119–129. [Google Scholar] [CrossRef]
- Institute of Medicine Committee on Quality of Health Care in America. Crossing the Quality Chasm: A New Health System for the 21st Century; National Academies Press (US): Washington, DC, USA, 2001. [Google Scholar]
- Kvæl, L.A.H.; Debesay, J.; Bye, A.; Langaas, A.; Bergland, A. Choice, Voice, and Coproduction in Intermediate Care: Exploring Geriatric Patients’ and Their Relatives’ Perspectives on Patient Participation. SAGE Open 2019, 9, 2158244019876318. [Google Scholar] [CrossRef]
- Valaas, H.L.; Klokkerud, M.; Hildeskår, J.; Hagland, A.S.; Kjønli, E.; Mjøsund, K.; Øie, L.; Wigers, S.H.; Eppeland, S.G.; Høystad, T.; et al. Rehabilitation goals described by patients with rheumatic and musculoskeletal diseases: Content and attainment during the first year after rehabilitation. Disabil. Rehabil. 2022, 44, 7947–7957. [Google Scholar] [CrossRef]
- Amundsen, O.; Vøllestad, N.K.; Meisingset, I.; Robinson, H.S. Associations between treatment goals, patient characteristics, and outcome measures for patients with musculoskeletal disorders in physiotherapy practice. BMC Musculoskelet Disord. 2021, 22, 182. [Google Scholar] [CrossRef] [PubMed]
- Ashford, S.; Turner-Stokes, L.; Rose, H.; Singer, B. Patient engagement and satisfaction with goal planning: Impact on outcome from rehabilitation. Int. J. Ther. Rehabil. 2015, 22, 210–216. [Google Scholar] [CrossRef]
- Grine, L.; Janssens, R.; van Overbeeke, E.; Derijcke, D.; Silva, M.; Delys, B.; Dusart, I.; Aertsen, V.; Mertens de Wilmars, M.; Robaczewska, J.; et al. Improving Patient Involvement in the Lifecycle of Medicines: Insights From the EUPATI BE Survey. Front. Med. 2020, 7, 36. [Google Scholar] [CrossRef] [PubMed]
- de Wit, M.P.T.; Berlo, S.E.; Aanerud, G.J.; Aletaha, D.; Bijlsma, J.W.; Croucher, L.; Da Silva, J.A.P.; Glusing, B.; Gossec, L.; Hewlett, S.; et al. European League Against Rheumatism recommendations for the inclusion of patient representatives in scientific projects. Ann. Rheum. Dis. 2011, 70, 722–726. [Google Scholar] [CrossRef]
- Rosenman, R.; Tennekoon, V.; Hill, L.G. Measuring bias in self-reported data. Int. J. Behav. Healthc. Res. 2011, 2, 320–332. [Google Scholar] [CrossRef]
- Howard, G.S. Response-Shift Bias: A Problem in Evaluating Interventions with Pre/Post Self-Reports. Eval. Rev. 1980, 4, 93–106. [Google Scholar] [CrossRef]
- Zini, M.L.L.; Banfi, G. A Narrative Literature Review of Bias in Collecting Patient Reported Outcomes Measures (PROMs). Int. J. Environ. Res. Public Health 2021, 18, 12445. [Google Scholar] [CrossRef]

| Women, n, % | 1470 | 70 |
| Age, years, mean, SD | 53.5 | 13.5 |
| Living with partner, n, % | 1080 | 58 |
| Higher education ≥ 12 years, n, % | 1035 | 49 |
| Full-time paid work, n, % | 620 | 29 |
| Part-time paid work, n, % | 432 | 20 |
| Not in paid work, n, % | 789 | 43 |
| Pain ≥ 3 months, n, % | 1418 | 92 |
| RMDs *, n, % | 1117 | 53 |
| Lifestyle disease, n, % | 235 | 11 |
| Neurological injuries and diseases, n, % | 270 | 10 |
| Other diseases or injuries, n, % | 491 | 23 |
| Actively Involved in Goal-Setting n = 2007/95% | Actively Involved in Preparing the Rehab Plan n = 1666/79% | Participated in at Least Two Meetings n = 774/84% | Relatives Invited to Participate in Meetings n = 478/23% | External Professionals Invited to Participate in Meetings n = 391/19% | |
|---|---|---|---|---|---|
| % | % | % | % | % | |
| Male | 92 | 77 | 84 | 27 | 22 |
| Female | 96 | 80 | 84 | 21 | 17 |
| ≥18–39 yrs. | 96 | 84 | 93 | 34 | 26 |
| 40–49 yrs. | 97 | 84 | 87 | 26 | 25 |
| 50–59 yrs. | 96 | 84 | 87 | 22 | 19 |
| 60–69 yrs. | 95 | 75 | 81 | 18 | 11 |
| 70–>80 yrs. | 89 | 61 | 68 | 10 | 6 |
| Single | 95 | 76 | 84 | 19 | 18 |
| Living with partner | 95 | 81 | 84 | 24 | 18 |
| Higher education ≥ 12 Years | 95 | 79 | 86 | 22 | 19 |
| Education ˂ 12 years | 96 | 80 | 82 | 22 | 16 |
| Full-time paid work | 96 | 81 | 87 | 20 | 16 |
| Part-time paid work | 96 | 83 | 84 | 26 | 23 |
| Not in paid work | 93 | 76 | 82 | 21 | 17 |
| Pain ˂ 3 months | 92 | 71 | 73 | 22 | 13 |
| Pain ≥ 3 months | 95 | 79 | 86 | 21 | 19 |
| RMDs * | 95 | 78 | 83 | 18 | 18 |
| Lifestyle disease | 95 | 83 | 88 | 24 | 14 |
| Neurological injuries and diseases | 94 | 75 | 82 | 30 | 19 |
| Other diseases or injuries | 95 | 82 | 86 | 29 | 22 |
| 95% CI for OR | ||||
|---|---|---|---|---|
| OR | Lower | Upper | p-Value | |
| Sex, women ref men | 1.87 | 1.15 | 3.02 | 0.01 |
| Age | 0.97 | 0.95 | 0.99 | 0.004 |
| Living with partner ref single | 0.95 | 0.59 | 1.53 | 0.85 |
| Higher education ≥ 12 years ref˂12 months | 0.77 | 0.47 | 1.24 | 0.28 |
| Part-time paid work ref not in work | 1.71 | 0.89 | 3.27 | 0.10 |
| Full-time paid work ref not in work | 1.70 | 0.96 | 2.99 | 0.066 |
| ˂3 months of pain ref ≥3 months pain | 0.66 | 0.32 | 1.35 | 0.26 |
| RMDs * ref other | 1.23 | 0.69 | 2.20 | 0.47 |
| Lifestyle disease ref other | 1.00 | 0.41 | 2.46 | 0.99 |
| Neurological diseases or injuries ref other | 1.11 | 0.48 | 2.57 | 0.79 |
| 95% CI for OR | ||||
|---|---|---|---|---|
| OR | Lower | Upper | p-Value | |
| Sex, women ref men | 1.26 | 0.92 | 1.76 | 0.14 |
| Age | 1.03 | 1.02 | 1.04 | <0.001 |
| Living with partner ref single | 1.06 | 0.81 | 1.40 | 0.64 |
| Higher education ≥ 12 years ref ˂ 12 months | 0.71 | 0.54 | 0.95 | 0.02 |
| Work participation | ||||
| Part-time paid work ref not in paid work | 1.20 | 0.85 | 1.69 | 0.28 |
| Full-time paid work ref not in paid work | 1.34 | 0.97 | 1.85 | 0.74 |
| ˂3 months of pain ref ≥3 months of pain | 2.17 | 1.17 | 4.00 | 0.01 |
| RMDs * ref other | 1.09 | 0.76 | 1.56 | 0.63 |
| Neurological diseases ref other | 0.79 | 0.49 | 1.28 | 0.34 |
| Lifestyle disease ref other | 4.93 | 2.35 | 10.35 | <0.001 |
| Involvement in the rehabilitation process | ||||
| Actively involved in goal-setting | 2.79 | 1.60 | 4.87 | <0.001 |
| Actively involved in the rehab plan | 2.04 | 1.44 | 2.87 | <0.001 |
| Participated in a minimum of two meetings | 1.25 | 0.84 | 1.84 | 0.25 |
| Next of kin asked to participate in meetings | 1.22 | 0.84 | 1.77 | 0.29 |
| External personnel asked to participate in meetings | 1.08 | 0.74 | 1.57 | 0.68 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sagen, J.S.; Kjeken, I.; Habberstad, A.; Linge, A.D.; Simonsen, A.E.; Lyken, A.D.; Irgens, E.L.; Framstad, H.; Lyby, P.S.; Klokkerud, M.; et al. Patient Involvement in the Rehabilitation Process Is Associated with Improvement in Function and Goal Attainment: Results from an Explorative Longitudinal Study. J. Clin. Med. 2024, 13, 320. https://doi.org/10.3390/jcm13020320
Sagen JS, Kjeken I, Habberstad A, Linge AD, Simonsen AE, Lyken AD, Irgens EL, Framstad H, Lyby PS, Klokkerud M, et al. Patient Involvement in the Rehabilitation Process Is Associated with Improvement in Function and Goal Attainment: Results from an Explorative Longitudinal Study. Journal of Clinical Medicine. 2024; 13(2):320. https://doi.org/10.3390/jcm13020320
Chicago/Turabian StyleSagen, Joachim Støren, Ingvild Kjeken, Andreas Habberstad, Anita Dyb Linge, Ann Elisabeth Simonsen, Anne Dorte Lyken, Eirik Lind Irgens, Heidi Framstad, Peter Solvoll Lyby, Mari Klokkerud, and et al. 2024. "Patient Involvement in the Rehabilitation Process Is Associated with Improvement in Function and Goal Attainment: Results from an Explorative Longitudinal Study" Journal of Clinical Medicine 13, no. 2: 320. https://doi.org/10.3390/jcm13020320
APA StyleSagen, J. S., Kjeken, I., Habberstad, A., Linge, A. D., Simonsen, A. E., Lyken, A. D., Irgens, E. L., Framstad, H., Lyby, P. S., Klokkerud, M., Dagfinrud, H., & Moe, R. H., on behalf of the RehabNytte Consortium. (2024). Patient Involvement in the Rehabilitation Process Is Associated with Improvement in Function and Goal Attainment: Results from an Explorative Longitudinal Study. Journal of Clinical Medicine, 13(2), 320. https://doi.org/10.3390/jcm13020320





