Inflammation as a New Therapeutic Target among Older Patients with Ischemic Heart Disease
Abstract
:1. Introduction
2. Inflammation and Ischemic Heart Disease
3. Inflammation, Aging, and Ischemic Heart Disease
4. Anti-Inflammation Strategies in Ischemic Heart Disease
4.1. Pharmacological Anti-Inflammatory Therapy
4.1.1. Traditional Pharmacological Anti-Inflammatory Therapy
4.1.2. Novel Pharmacological Anti-Inflammatory Therapy
Canakinumab
Colchicine
Methotrexate
Ziltivekimab
Others
4.2. Lifestyle Modifications and Dietary Interventions
5. Clinical Implications and Future Directions
6. Conclusions
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
References
- Murray, C.J.L.; Afshin, A.; Alam, T.; Ashbaugh, C.; Barthelemy, C.; Biehl, M.; Brauer, M.; Compton, K.; Cromwell, E.; Dandona, L.; et al. Global Burden of 369 Diseases and Injuries in 204 Countries and Territories, 1990–2019: A Systematic Analysis for the Global Burden of Disease Study 2019. Lancet 2020, 396, 1204–1222. [Google Scholar] [CrossRef] [PubMed]
- Vaduganathan, M.; Mensah, G.A.; Turco, J.V.; Fuster, V.; Roth, G.A. The Global Burden of Cardiovascular Diseases and Risk: A Compass for Future Health. J. Am. Coll. Cardiol. 2022, 80, 2361–2371. [Google Scholar] [CrossRef] [PubMed]
- Dégano, I.R.; Elosua, R.; Marrugat, J. Epidemiology of Acute Coronary Syndromes in Spain: Estimation of the Number of Cases and Trends from 2005 to 2049. Rev. Española De Cardiol. (Engl. Ed.) 2013, 66, 472–481. [Google Scholar] [CrossRef]
- Hansson, G.K. Inflammation, Atherosclerosis, and Coronary Artery Disease. N. Engl. J. Med. 2005, 352, 1685–1695. [Google Scholar] [CrossRef] [PubMed]
- Sanchis, J.; Bonanad, C.; Ruiz, V.; Fernández, J.; García-Blas, S.; Mainar, L.; Ventura, S.; Rodríguez-Borja, E.; Chorro, F.J.; Hermenegildo, C.; et al. Frailty and Other Geriatric Conditions for Risk Stratification of Older Patients with Acute Coronary Syndrome. Am. Heart J. 2014, 168, 784–791.e2. [Google Scholar] [CrossRef]
- Cepas-Guillén, P.L.; Borrego-Rodriguez, J.; Flores-Umanzor, E.; Echarte-Morales, J.; Fernandez-Valledor, A.; Menendez-Suarez, P.; Vazquez, S.; Alonso, N.; Ortiz, J.T.; Regueiro, A.; et al. Outcomes of Nonagenarians with ST Elevation Myocardial Infarction. Am. J. Cardiol. 2020, 125, 11–18. [Google Scholar] [CrossRef]
- Libby, P. Inflammation in Atherosclerosis. Arterioscler. Thromb. Vasc. Biol. 2012, 32, 2045–2051. [Google Scholar] [CrossRef]
- Agca, R.; Smulders, Y.; Nurmohamed, M. Cardiovascular Disease Risk in Immune-Mediated Inflammatory Diseases: Recommendations for Clinical Practice. Heart 2022, 108, 73–79. [Google Scholar] [CrossRef]
- Badimon, L.; Padró, T.; Vilahur, G. Atherosclerosis, Platelets and Thrombosis in Acute Ischaemic Heart Disease. Eur. Heart J. Acute Cardiovasc. Care 2012, 1, 60–74. [Google Scholar] [CrossRef]
- Stefanadis, C.; Antoniou, C.K.; Tsiachris, D.; Pietri, P. Coronary Atherosclerotic Vulnerable Plaque: Current Perspectives. J. Am. Heart Assoc. 2017, 6, e005543. [Google Scholar] [CrossRef]
- Bentzon, J.F.; Otsuka, F.; Virmani, R.; Falk, E. Mechanisms of Plaque Formation and Rupture. Circ. Res. 2014, 114, 1852–1866. [Google Scholar] [CrossRef] [PubMed]
- Burke, A.P.; Kolodgie, F.D.; Farb, A.; Weber, D.K.; Malcom, G.T.; Smialek, J.; Virmani, R. Healed Plaque Ruptures and Sudden Coronary Death: Evidence That Subclinical Rupture Has a Role in Plaque Progression. Circulation 2001, 103, 934–940. [Google Scholar] [CrossRef] [PubMed]
- Stone, G.W.; Maehara, A.; Lansky, A.J.; de Bruyne, B.; Cristea, E.; Mintz, G.S.; Mehran, R.; McPherson, J.; Farhat, N.; Marso, S.P.; et al. A Prospective Natural-History Study of Coronary Atherosclerosis. N. Engl. J. Med. 2011, 364, 226–235. [Google Scholar] [CrossRef] [PubMed]
- Ferencik, M.; Mayrhofer, T.; Bittner, D.O.; Emami, H.; Puchner, S.B.; Lu, M.T.; Meyersohn, N.M.; Ivanov, A.V.; Adami, E.C.; Patel, M.R.; et al. Use of High-Risk Coronary Atherosclerotic Plaque Detection for Risk Stratification of Patients with Stable Chest Pain: A Secondary Analysis of the PROMISE Randomized Clinical Trial. JAMA Cardiol. 2018, 3, 144–152. [Google Scholar] [CrossRef]
- Matter, M.A.; Paneni, F.; Libby, P.; Frantz, S.; Stähli, B.E.; Templin, C.; Mengozzi, A.; Wang, Y.-J.; Kündig, T.M.; Räber, L.; et al. Inflammation in Acute Myocardial Infarction: The Good, the Bad and the Ugly. Eur. Heart J. 2024, 45, 89–103. [Google Scholar] [CrossRef]
- Koenig, W. Low-Grade Inflammation Modifies Cardiovascular Risk Even at Very Low LDL-C Levels: Are We Aiming for a Dual Target Concept? Circulation 2018, 138, 150–153. [Google Scholar] [CrossRef] [PubMed]
- Kaptoge, S.; Di Angelantonio, E.; Lowe, G.; Pepys, M.B.; Thompson, S.G.; Collins, R.; Danesh, J.; Tipping, R.W.; Ford, C.E.; Pressel, S.L.; et al. C-Reactive Protein Concentration and Risk of Coronary Heart Disease, Stroke, and Mortality: An Individual Participant Meta-Analysis. Lancet 2010, 375, 132–140. [Google Scholar] [CrossRef]
- Visseren, F.; Mach, F.; Smulders, Y.M.; Carballo, D.; Koskinas, K.C.; Bäck, M.; Benetos, A.; Biffi, A.; Boavida, J.M.; Capodanno, D.; et al. 2021 ESC Guidelines on Cardiovascular Disease Prevention in Clinical Practice. Eur. Heart J. 2021, 42, 3227–3337. [Google Scholar] [CrossRef]
- Paneni, F.; Diaz Cañestro, C.; Libby, P.; Lüscher, T.F.; Camici, G.G. The Aging Cardiovascular System: Understanding It at the Cellular and Clinical Levels. J. Am. Coll. Cardiol. 2017, 69, 1952–1967. [Google Scholar] [CrossRef]
- Kontis, V.; Bennett, J.E.; Mathers, C.D.; Li, G.; Foreman, K.; Ezzati, M. Future Life Expectancy in 35 Industrialised Countries: Projections with a Bayesian Model Ensemble. Lancet 2017, 389, 1323–1335. [Google Scholar] [CrossRef]
- López-Otín, C.; Blasco, M.A.; Partridge, L.; Serrano, M.; Kroemer, G. The Hallmarks of Aging. Cell 2013, 153, 1194. [Google Scholar] [CrossRef] [PubMed]
- Liberale, L.; Badimon, L.; Montecucco, F.; Lüscher, T.F.; Libby, P.; Camici, G.G. Inflammation, Aging, and Cardiovascular Disease: JACC Review Topic of the Week. J. Am. Coll. Cardiol. 2022, 79, 837–847. [Google Scholar] [CrossRef]
- Liberale, L.; Montecucco, F.; Tardif, J.C.; Libby, P.; Camici, G.G. Inflamm-Ageing: The Role of Inflammation in Age-Dependent Cardiovascular Disease. Eur. Heart J. 2020, 41, 2974–2982. [Google Scholar] [CrossRef] [PubMed]
- Di Micco, R.; Krizhanovsky, V.; Baker, D.; d’Adda di Fagagna, F. Cellular Senescence in Ageing: From Mechanisms to Therapeutic Opportunities. Nat. Rev. Mol. Cell Biol. 2021, 22, 75–95. [Google Scholar] [CrossRef] [PubMed]
- Franceschi, C.; Garagnani, P.; Vitale, G.; Capri, M.; Salvioli, S. Inflammaging and “Garb-Aging”. Trends Endocrinol. Metab. 2017, 28, 199–212. [Google Scholar] [CrossRef]
- Sovran, B.; Hugenholtz, F.; Elderman, M.; Van Beek, A.A.; Graversen, K.; Huijskes, M.; Boekschoten, M.V.; Savelkoul, H.F.J.; De Vos, P.; Dekker, J.; et al. Age-Associated Impairment of the Mucus Barrier Function Is Associated with Profound Changes in Microbiota and Immunity. Sci. Rep. 2019, 9, 1437. [Google Scholar] [CrossRef] [PubMed]
- Jaiswal, S.; Natarajan, P.; Silver, A.J.; Gibson, C.J.; Bick, A.G.; Shvartz, E.; McConkey, M.; Gupta, N.; Gabriel, S.; Ardissino, D.; et al. Clonal Hematopoiesis and Risk of Atherosclerotic Cardiovascular Disease. N. Engl. J. Med. 2017, 377, 111–121. [Google Scholar] [CrossRef]
- Burton, J.K.; Yates, L.C.; Whyte, L.; Fitzsimons, E.; Stott, D.J. New Horizons in Iron Deficiency Anaemia in Older Adults. Age Ageing 2020, 49, 309–318. [Google Scholar] [CrossRef]
- Jankowska, E.A.; Wojtas, K.; Kasztura, M.; Mazur, G.; Butrym, A.; Kalicinska, E.; Rybinska, I.; Skiba, J.; Von Haehling, S.; Doehner, W.; et al. Bone Marrow Iron Depletion Is Common in Patients with Coronary Artery Disease. Int. J. Cardiol. 2015, 182, 517–522. [Google Scholar] [CrossRef]
- Wunderer, F.; Traeger, L.; Sigurslid, H.H.; Meybohm, P.; Bloch, D.B.; Malhotra, R. The Role of Hepcidin and Iron Homeostasis in Atherosclerosis. Pharmacol. Res. 2020, 153, 104664. [Google Scholar] [CrossRef]
- Schrage, B.; Rübsamen, N.; Ojeda, F.M.; Thorand, B.; Peters, A.; Koenig, W.; Söderberg, S.; Söderberg, M.; Mathiesen, E.B.; Njølstad, I.; et al. Association of Iron Deficiency with Incident Cardiovascular Diseases and Mortality in the General Population. ESC Heart Fail. 2021, 8, 4584–4592. [Google Scholar] [CrossRef] [PubMed]
- Savarese, G.; von Haehling, S.; Butler, J.; Cleland, J.G.F.; Ponikowski, P.; Anker, S.D. Iron Deficiency and Cardiovascular Disease. Eur. Heart J. 2023, 44, 14–27. [Google Scholar] [CrossRef] [PubMed]
- Jain, M.K.; Ridker, P.M. Anti-Inflammatory Effects of Statins: Clinical Evidence and Basic Mechanisms. Nat. Rev. Drug Discov. 2005, 4, 977–987. [Google Scholar] [CrossRef] [PubMed]
- Andreotti, F.; Maggioni, A.P.; Campeggi, A.; Iervolino, A.; Scambia, G.; Massetti, M. Anti-Inflammatory Therapy in Ischaemic Heart Disease: From Canakinumab to Colchicine. Eur. Heart J. Suppl. 2021, 23, E13–E18. [Google Scholar] [CrossRef] [PubMed]
- Jacobsen, A.P.; Raber, I.; Mccarthy, C.P.; Blumenthal, R.S.; Bhatt, D.L.; Cusack, R.W.; Serruys, P.W.J.C.; Wijns, W.; Mcevoy, J.W. Lifelong Aspirin for All in the Secondary Prevention of Chronic Coronary Syndrome: Still Sacrosanct or Is Reappraisal Warranted? Circulation 2020, 142, 1579–1590. [Google Scholar] [CrossRef] [PubMed]
- Gao, X.; Adhikari, C.M.; Peng, L.; Guo, X.; Zhai, Y.; He, X.; Zhang, L.-Y.; Lin, J.; Zuo, Z. Efficacy of Different Doses of Aspirin in Decreasing Blood Levels of Inflammatory Markers in Patients with Cardiovascular Metabolic Syndrome. J. Pharm. Pharmacol. 2009, 61, 1505–1510. [Google Scholar] [CrossRef]
- Ikonomidis, I.; Andreotti, F.; Economou, E.; Stefanadis, C.; Toutouzas, P.; Nihoyannopoulos, P. Increased Proinflammatory Cytokines in Patients with Chronic Stable Angina and Their Reduction by Aspirin. Circulation 1999, 100, 793–798. [Google Scholar] [CrossRef]
- Aul, P.; Idker, M.R.; Ary, M.; Ushman, C.; Eir, M.; Tampfer, J.S.; Ussell, R.; Racy, P.T.; Harles, C.; Ennekens, H.H. Inflammation, Aspirin, and the Risk of Cardiovascular Disease in Apparently Healthy Men. N. Engl. J. Med. 1997, 336, 973–979. [Google Scholar] [CrossRef]
- McNeil, J.J.; Wolfe, R.; Woods, R.L.; Tonkin, A.M.; Donnan, G.A.; Nelson, M.R.; Reid, C.M.; Lockery, J.E.; Kirpach, B.; Storey, E.; et al. Effect of Aspirin on Cardiovascular Events and Bleeding in the Healthy Elderly. N. Engl. J. Med. 2018, 379, 1509–1518. [Google Scholar] [CrossRef]
- Ridker, P.M.; Rifai, N.; Pfeifer, M.A.; Sacks, F.; Braunwald, E. Long-Term Effects of Pravastatin on Plasma Concentration of C-Reactive Protein. The Cholesterol and Recurrent Events (CARE) Investigators. Circulation 1999, 100, 230–235. [Google Scholar] [CrossRef]
- Ridker, P.M.; Cannon, C.P.; Morrow, D.; Rifai, N.; Rose, L.M.; McCabe, C.H.; Pfeffer, M.A.; Braunwald, E. C-Reactive Protein Levels and Outcomes after Statin Therapy. N. Engl. J. Med. 2005, 8, 8–9. [Google Scholar] [CrossRef]
- Cannon, C.P.; Braunwald, E.; McCabe, C.H.; Rader, D.J.; Rouleau, J.L.; Belder, R.; Joyal, S.V.; Hill, K.A.; Pfeffer, M.A.; Skene, A.M. Intensive versus Moderate Lipid Lowering with Statins after Acute Coronary Syndromes. N. Engl. J. Med. 2004, 350, 1495–1504. [Google Scholar] [CrossRef] [PubMed]
- Ridker, P.M.; Danielson, E.; Fonseca, F.A.H.; Genest, J.; Gotto, A.M., Jr.; Kastelein, J.J.P.; Koenig, W.; Libby, P.; Lorenzatti, A.J.; MacFadyen, J.G.; et al. Rosuvastatin to Prevent Vascular Events in Men and Women with Elevated C-Reactive Protein. N. Engl. J. Med. 2008, 359, 2195–2207. [Google Scholar] [CrossRef] [PubMed]
- Räber, L.; Ueki, Y.; Otsuka, T.; Losdat, S.; Häner, J.D.; Lonborg, J.; Fahrni, G.; Iglesias, J.F.; van Geuns, R.-J.; Ondracek, A.S.; et al. Effect of Alirocumab Added to High-Intensity Statin Therapy on Coronary Atherosclerosis in Patients with Acute Myocardial Infarction: The PACMAN-AMI Randomized Clinical Trial. JAMA 2022, 327, 1771–1781. [Google Scholar] [CrossRef] [PubMed]
- Nicholls, S.J.; Puri, R.; Anderson, T.; Ballantyne, C.M.; Cho, L.; Kastelein, J.J.P.; Koenig, W.; Somaratne, R.; Kassahun, H.; Yang, J.; et al. Effect of Evolocumab on Progression of Coronary Disease in Statin-Treated Patients: The GLAGOV Randomized Clinical Trial. JAMA-J. Am. Med. Assoc. 2016, 316, 2373–2384. [Google Scholar] [CrossRef] [PubMed]
- Ota, H.; Omori, H.; Kawasaki, M.; Hirakawa, A.; Matsuo, H. Clinical Impact of PCSK9 Inhibitor on Stabilization and Regression of Lipid-Rich Coronary Plaques: A near-Infrared Spectroscopy Study. Eur. Heart J. Cardiovasc. Imaging 2022, 23, 217–228. [Google Scholar] [CrossRef] [PubMed]
- Perez De Isla, L.; Diaz-Diaz, J.L.; Romero, M.J.; Muniz-Grijalvo, O.; Mediavilla, J.D.; Argueso, R.; Sanchez Munoz-Torrero, J.F.; Rubio, P.; Alvarez-Banos, P.; Ponte, P.; et al. Alirocumab and Coronary Atherosclerosis in Asymptomatic Patients with Familial Hypercholesterolemia: The ARCHITECT Study. Circulation 2023, 147, 1436–1443. [Google Scholar] [CrossRef]
- Schwartz, G.G.; Steg, P.G.; Szarek, M.; Bhatt, D.L.; Bittner, V.A.; Diaz, R.; Edelberg, J.M.; Goodman, S.G.; Hanotin, C.; Harrington, R.A.; et al. Alirocumab and Cardiovascular Outcomes after Acute Coronary Syndrome. N. Engl. J. Med. 2018, 379, 2097–2107. [Google Scholar] [CrossRef]
- Ridker, P.M.; Everett, B.M.; Thuren, T.; MacFadyen, J.G.; Chang, W.H.; Ballantyne, C.; Fonseca, F.; Nicolau, J.; Koenig, W.; Anker, S.D.; et al. Antiinflammatory Therapy with Canakinumab for Atherosclerotic Disease. N. Engl. J. Med. 2017, 377, 1119–1131. [Google Scholar] [CrossRef]
- Orkaby, A.R.; Thomson, A.; MacFadyen, J.; Besdine, R.; Forman, D.E.; Travison, T.G.; Ridker, P.M. Effect of Canakinumab on Frailty: A Post Hoc Analysis of the CANTOS Trial. Aging Cell 2023, e14029. [Google Scholar] [CrossRef]
- Zhang, F.S.; He, Q.Z.; Qin, C.H.; Little, P.J.; Weng, J.P.; Xu, S.W. Therapeutic Potential of Colchicine in Cardiovascular Medicine: A Pharmacological Review. Acta Pharmacol. Sin. 2022, 43, 2173–2190. [Google Scholar] [CrossRef] [PubMed]
- Nidorf, S.M.; Eikelboom, J.W.; Budgeon, C.A.; Thompson, P.L. Low-Dose Colchicine for Secondary Prevention of Cardiovascular Disease. J. Am. Coll. Cardiol. 2013, 61, 404–410. [Google Scholar] [CrossRef]
- Nidorf, S.M.; Fiolet, A.T.L.; Mosterd, A.; Eikelboom, J.W.; Schut, A.; Opstal, T.S.J.; The, S.H.K.; Xu, X.-F.; Ireland, M.A.; Lenderink, T.; et al. Colchicine in Patients with Chronic Coronary Disease. N. Engl. J. Med. 2020, 383, 1838–1847. [Google Scholar] [CrossRef] [PubMed]
- Deftereos, S.G.; Beerkens, F.J.; Shah, B.; Giannopoulos, G.; Vrachatis, D.A.; Giotaki, S.G.; Siasos, G.; Nicolas, J.; Arnott, C.; Patel, S.; et al. Colchicine in Cardiovascular Disease: In-Depth Review. Circulation 2022, 145, 61–78. [Google Scholar] [CrossRef] [PubMed]
- Tong, D.C.; Quinn, S.; Nasis, A.; Hiew, C.; Roberts-Thomson, P.; Adams, H.; Sriamareswaran, R.; Htun, N.M.; Wilson, W.; Stub, D.; et al. Colchicine in Patients with Acute Coronary Syndrome. Circulation 2020, 142, 1890–1900. [Google Scholar] [CrossRef] [PubMed]
- Mewton, N.; Roubille, F.; Bresson, D.; Prieur, C.; Bouleti, C.; Bochaton, T.; Ivanes, F.; Dubreuil, O.; Biere, L.; Hayek, A.; et al. Effect of Colchicine on Myocardial Injury in Acute Myocardial Infarction. Circulation 2021, 144, 859–869. [Google Scholar] [CrossRef]
- Tardif, J.-C.; Kouz, S.; Waters, D.D.; Bertrand, O.F.; Diaz, R.; Maggioni, A.P.; Pinto, F.J.; Ibrahim, R.; Gamra, H.; Kiwan, G.S.; et al. Efficacy and Safety of Low-Dose Colchicine after Myocardial Infarction. N. Engl. J. Med. 2019, 381, 2497–2505. [Google Scholar] [CrossRef] [PubMed]
- Ridker, P.M.; Everett, B.M.; Pradhan, A.; MacFadyen, J.G.; Solomon, D.H.; Zaharris, E.; Mam, V.; Hasan, A.; Rosenberg, Y.; Iturriaga, E.; et al. Low-Dose Methotrexate for the Prevention of Atherosclerotic Events. N. Engl. J. Med. 2019, 380, 752–762. [Google Scholar] [CrossRef]
- Ridker, P.M.; Devalaraja, M.; Baeres, F.M.M.; Engelmann, M.D.M.; Hovingh, G.K.; Ivkovic, M.; Lo, L.; Kling, D.; Pergola, P.; Raj, D.; et al. IL-6 Inhibition with Ziltivekimab in Patients at High Atherosclerotic Risk (RESCUE): A Double-Blind, Randomised, Placebo-Controlled, Phase 2 Trial. Lancet 2021, 397, 2060–2069. [Google Scholar] [CrossRef]
- Ridker, P.M. From RESCUE to ZEUS: Will Interleukin-6 Inhibition with Ziltivekimab Prove Effective for Cardiovascular Event Reduction? Cardiovasc. Res. 2021, 117, E138–E140. [Google Scholar] [CrossRef]
- Tardif, J.C.; McMurray, J.J.; Klug, E.; Small, R.; Schumi, J.; Choi, J.; Cooper, J.; Scott, R.; Lewis, E.F.; L’Allier, P.L.; et al. Effects of Succinobucol (AGI-1067) after an Acute Coronary Syndrome: A Randomised, Double-Blind, Placebo-Controlled Trial. Lancet 2008, 371, 1761–1768. [Google Scholar] [CrossRef] [PubMed]
- Morton, A.C.; Rothman, A.M.K.; Greenwood, J.P.; Gunn, J.; Chase, A.; Clarke, B.; Hall, A.S.; Fox, K.; Foley, C.; Banya, W.; et al. The Effect of Interleukin-1 Receptor Antagonist Therapy on Markers of Inflammation in Non-ST Elevation Acute Coronary Syndromes: The MRC-ILA Heart Study. Eur. Heart J. 2015, 36, 377–384. [Google Scholar] [CrossRef] [PubMed]
- The Stability Investigators. Darapladib for Preventing Ischemic Events in Stable Coronary Heart Disease. N. Engl. J. Med. 2014, 370, 1702–1711. [Google Scholar] [CrossRef] [PubMed]
- O’Donoghue, M.L.; Braunwald, E.; White, H.D.; Steen, D.P.; Lukas, M.A.; Tarka, E.; Steg, P.G.; Hochman, J.S.; Bode, C.; Maggioni, A.P.; et al. Effect of Darapladib on Major Coronary Events after an Acute Coronary Syndrome: The SOLID-TIMI 52 Randomized Clinical Trial. JAMA 2014, 312, 1006–1015. [Google Scholar] [CrossRef] [PubMed]
- Nicholls, S.J.; Kastelein, J.J.P.; Schwartz, G.G.; Bash, D.; Rosenson, R.S.; Cavender, M.A.; Brennan, D.M.; Koenig, W.; Jukema, J.W.; Nambi, V.; et al. Varespladib and Cardiovascular Events in Patients with an Acute Coronary Syndrome: The VISTA-16 Randomized Clinical Trial. JAMA 2014, 311, 252–262. [Google Scholar] [CrossRef] [PubMed]
- Giugliano, D.; Ceriello, A.; Esposito, K. The Effects of Diet on Inflammation: Emphasis on the Metabolic Syndrome. J. Am. Coll. Cardiol. 2006, 48, 677–685. [Google Scholar] [CrossRef] [PubMed]
- Gleeson, M.; Bishop, N.C.; Stensel, D.J.; Lindley, M.R.; Mastana, S.S.; Nimmo, M.A. The Anti-Inflammatory Effects of Exercise: Mechanisms and Implications for the Prevention and Treatment of Disease. Nat. Rev. Immunol. 2011, 11, 607–615. [Google Scholar] [CrossRef]
- Ouchi, N.; Parker, J.L.; Lugus, J.J.; Walsh, K. Adipokines in Inflammation and Metabolic Disease. Nat. Rev. Immunol. 2011, 11, 85–97. [Google Scholar] [CrossRef]
- Samper-Ternent, R.; Al Snih, S. Obesity in Older Adults: Epidemiology and Implications for Disability and Disease. Rev. Clin. Gerontol. 2012, 22, 10. [Google Scholar] [CrossRef]
- De Backer, G.; Jankowski, P.; Kotseva, K.; Mirrakhimov, E.; Reiner, Ž.; Rydén, L.; Tokgözoğlu, L.; Wood, D.; De Bacquer, D.; Jankowski, P.; et al. Management of Dyslipidaemia in Patients with Coronary Heart Disease: Results from the ESC-EORP EUROASPIRE V Survey in 27 Countries. Atherosclerosis 2019, 285, 135–146. [Google Scholar] [CrossRef]
- Valenzuela, P.L.; Ruilope, L.M.; Santos-Lozano, A.; Wilhelm, M.; Kränkel, N.; Fiuza-Luces, C.; Lucia, A. Exercise Benefits in Cardiovascular Diseases: From Mechanisms to Clinical Implementation. Eur. Heart J. 2023, 44, 1874–1889. [Google Scholar] [CrossRef] [PubMed]
- Zheng, G.; Qiu, P.; Xia, R.; Lin, H.; Ye, B.; Tao, J.; Chen, L. Effect of Aerobic Exercise on Inflammatory Markers in Healthy Middle-Aged and Older Adults: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Front. Aging Neurosci. 2019, 11, 98. [Google Scholar] [CrossRef] [PubMed]
- Banach, M.; Lewek, J.; Surma, S.; Penson, P.E.; Sahebkar, A.; Martin, S.S.; Bajraktari, G.; Henein, M.Y.; Reiner, Ž.; Bielecka-Dąbrowa, A.; et al. The Association between Daily Step Count and All-Cause and Cardiovascular Mortality: A Meta-Analysis. Eur. J. Prev. Cardiol. 2023, 30, 1975–1985. [Google Scholar] [CrossRef] [PubMed]
- Taylor, R.S.; Dalal, H.M.; McDonagh, S.T.J. The Role of Cardiac Rehabilitation in Improving Cardiovascular Outcomes. Nat. Rev. Cardiol. 2022, 19, 180. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, P.K.; Terashima, M.; Fair, J.M.; Varady, A.; Taylor-Piliae, R.E.; Iribarren, C.; Go, A.S.; Haskell, W.L.; Hlatky, M.A.; Fortmann, S.P.; et al. Physical Activity in Older Subjects Is Associated with Increased Coronary Vasodilation: The ADVANCE Study. JACC Cardiovasc. Imaging 2011, 4, 622–629. [Google Scholar] [CrossRef] [PubMed]
- Audelin, M.C.; Savage, P.D.; Ades, P.A. Exercise-Based Cardiac Rehabilitation for Very Old Patients (> or =75 Years): Focus on Physical Function. J. Cardiopulm. Rehabil. Prev. 2008, 28, 163–173. [Google Scholar] [CrossRef] [PubMed]
- Schopfer, D.W.; Forman, D.E. Cardiac Rehabilitation in Older Adults. Can. J. Cardiol. 2016, 32, 1088–1096. [Google Scholar] [CrossRef]
- Chrysohoou, C.; Panagiotakos, D.B.; Pitsavos, C.; Das, U.N.; Stefanadis, C. Adherence to the Mediterranean Diet Attenuates Inflammation and Coagulation Process in Healthy Adults: The Attica Study. J. Am. Coll. Cardiol. 2004, 44, 152–158. [Google Scholar] [CrossRef]
- Estruch, R.; Ros, E.; Salas-Salvadó, J.; Covas, M.-I.; Corella, D.; Arós, F.; Gómez-Gracia, E.; Ruiz-Gutiérrez, V.; Fiol, M.; Lapetra, J.; et al. Primary prevention of cardiovascular disease with a Mediterranean diet. N. Engl. J. Med. 2013, 368, 1279–1290, Erratum in N. Engl. J. Med. 2018, 378, 2441–2442. [Google Scholar] [CrossRef]
- Delgado-Lista, J.; Alcala-Diaz, J.F.; Torres-Peña, J.D.; Quintana-Navarro, G.M.; Fuentes, F.; Garcia-Rios, A.; Ortiz-Morales, A.M.; Gonzalez-Requero, A.I.; Perez-Caballero, A.I.; Yubero-Serrano, E.M.; et al. Long-Term Secondary Prevention of Cardiovascular Disease with a Mediterranean Diet and a Low-Fat Diet (CORDIOPREV): A Randomised Controlled Trial. Lancet 2022, 399, 1876–1885. [Google Scholar] [CrossRef]
- Domínguez, F.; Fuster, V.; Fernández-Alvira, J.M.; Fernández-Friera, L.; López-Melgar, B.; Blanco-Rojo, R.; Fernández-Ortiz, A.; García-Pavía, P.; Sanz, J.; Mendiguren, J.M.; et al. Association of Sleep Duration and Quality with Subclinical Atherosclerosis. J. Am. Coll. Cardiol. 2019, 73, 134–144. [Google Scholar] [CrossRef] [PubMed]
- Steptoe, A.; Kivimäki, M. Stress and Cardiovascular Disease. Nat. Rev. Cardiol. 2012, 9, 360–370. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.Z.; Wang, Y.X.; Jiang, C.L. Inflammation: The Common Pathway of Stress-Related Diseases. Front. Hum. Neurosci. 2017, 11, 316. [Google Scholar] [CrossRef] [PubMed]
- Lenze, E.J.; Voegtle, M.; Miller, J.P.; Ances, B.M.; Balota, D.A.; Barch, D.; Depp, C.A.; Diniz, B.S.; Eyler, L.T.; Foster, E.R.; et al. Effects of Mindfulness Training and Exercise on Cognitive Function in Older Adults: A Randomized Clinical Trial. JAMA 2022, 328, 2218–2229. [Google Scholar] [CrossRef] [PubMed]
- Lenze, E.J.; Hickman, S.; Hershey, T.; Wendleton, L.; Ly, K.; Dixon, D.; Doré, P.; Wetherell, J.L. Mindfulness-Based Stress Reduction for Older Adults with Worry Symptoms and Co-Occurring Cognitive Dysfunction. Int. J. Geriatr. Psychiatry 2014, 29, 991–1000. [Google Scholar] [CrossRef]
- Dhindsa, D.S.; Sandesara, P.B.; Shapiro, M.D.; Wong, N.D. The Evolving Understanding and Approach to Residual Cardiovascular Risk Management. Front. Cardiovasc. Med. 2020, 7, 527483. [Google Scholar] [CrossRef]
- Foreman, K.J.; Marquez, N.; Dolgert, A.; Fukutaki, K.; Fullman, N.; McGaughey, M.; Pletcher, M.A.; Smith, A.E.; Tang, K.; Yuan, C.W.; et al. Forecasting Life Expectancy, Years of Life Lost, and All-Cause and Cause-Specific Mortality for 250 Causes of Death: Reference and Alternative Scenarios for 2016–40 for 195 Countries and Territories. Lancet 2018, 392, 2052–2090. [Google Scholar] [CrossRef]
- Cepas-Guillén, P.L.; Echarte-Morales, J.; Caldentey, G.; Gómez, E.M.; Flores-Umanzor, E.; Borrego-Rodriguez, J.; Llagostera, M.; Viana Tejedor, A.; Vidal, P.; Benito-Gonzalez, T.; et al. Outcomes of Nonagenarians with Acute Coronary Syndrome. J. Am. Med. Dir. Assoc. 2022, 23, 81–86.e4. [Google Scholar] [CrossRef]
- Sehested, T.S.G.; Bjerre, J.; Ku, S.; Chang, A.; Jahansouz, A.; Owens, D.K.; Hlatky, M.A.; Goldhaber-Fiebert, J.D. Cost-Effectiveness of Canakinumab for Prevention of Recurrent Cardiovascular Events. JAMA Cardiol. 2019, 4, 128–135. [Google Scholar] [CrossRef]
- Samuel, M.; Tardif, J.C.; Khairy, P.; Roubille, F.; Waters, D.D.; Grégoire, J.C.; Pinto, F.J.; Maggioni, A.P.; Diaz, R.; Berry, C.; et al. Cost-Effectiveness of Low-Dose Colchicine after Myocardial Infarction in the Colchicine Cardiovascular Outcomes Trial (COLCOT). Eur. Heart J. Qual. Care Clin. Outcomes 2021, 7, 486–495. [Google Scholar] [CrossRef]
- Nelson, K.; Fuster, V.; Ridker, P.M. Low-Dose Colchicine for Secondary Prevention of Coronary Artery Disease: JACC Review Topic of the Week. J. Am. Coll. Cardiol. 2023, 82, 648–660. [Google Scholar] [CrossRef] [PubMed]
- Lorenzatti, A.J. Anti-Inflammatory Treatment and Cardiovascular Outcomes: Results of Clinical Trials. Eur. Cardiol. Rev. 2021, 16, e15. [Google Scholar] [CrossRef] [PubMed]
- Ridker, P.M. The Time to Initiate Anti-Inflammatory Therapy for Patients with Chronic Coronary Atherosclerosis Has Arrived. Circulation 2023, 148, 1071–1073. [Google Scholar] [CrossRef] [PubMed]
- Ridker, P.M.; Bhatt, D.L.; Pradhan, A.D.; Glynn, R.J.; MacFadyen, J.G.; Nissen, S.E. Inflammation and Cholesterol as Predictors of Cardiovascular Events among Patients Receiving Statin Therapy: A Collaborative Analysis of Three Randomised Trials. Lancet 2023, 401, 1293–1301. [Google Scholar] [CrossRef]
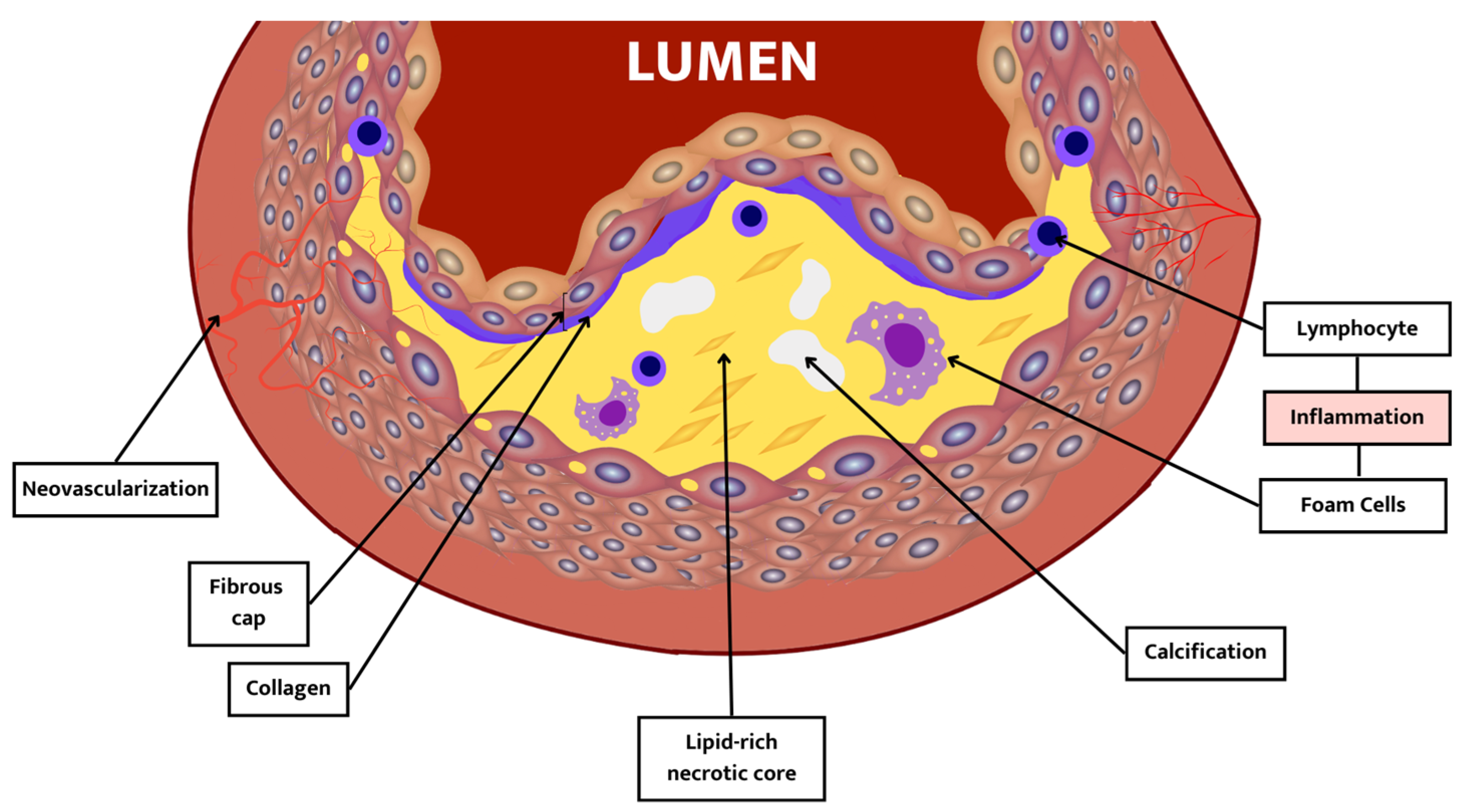

| Component | Description |
|---|---|
| Thin fibrous cap | Cap thickness < 65 μm. It occurs due to an imbalance between collagen synthesis and breakdown. |
| Lipid-rich necrotic core | A lipid-rich atheromatous core: hypocellular, low grade of supporting collagen, with high free cholesterol content in the core. |
| Inflammation | Inflammation is mainly distributed under the fibrous cap, not in the plaque core. |
| Calcification | Vulnerable plaques are less calcified than stable plaques. |
| Neovascularization | Higher micro-vessel density in vulnerable plaque than in stable plaque. |
| Element | Characteristics |
|---|---|
| Cellular Senescence |
|
| Immunosenescence |
|
| Garbaging |
|
| Microbiome |
|
| Clonal Hematopoiesis of Indeterminate Potential (CHIP) |
|
| Epigenetic/genetic clock |
|
| Study | Population | Control | Main Results |
|---|---|---|---|
| LoDoCo trial | CCS n = 532 | Conventional treatment | Follow-up 3 years Primary endpoint (ACS, cardiac arrest, stroke): 5.3% vs. 16%; p < 0.001 GI intolerance (2.5%) in Colchicine group |
| LoDoCo2 trial | CCS n = 5522 | Placebo | Follow-up 28.5 months Primary endpoint (CV death, MI, stroke, ischemia-driven coronary revascularization): 6.8% vs. 9.6%; p < 0.001 Trend to ↑ rate of non-CV death (1.9%; HR, 1.51 [95% CI, 0.99–2.31]) Myalgia 21.2% and GI intolerance 15.4% |
| COPS trial | ACS n = 795 | Placebo | Follow-up 12 years Primary endpoint (death, ACS, stroke, ischemia-driven coronary revascularization): 6.1% vs. 9.5%; p = 0.09 Significant higher rate of non-cardiovascular death (5 vs. 0; p = 0.024) |
| COLCOT trial | ACS n = 4745 | Placebo | Follow-up 22.6 months Primary endpoint (CV death, ACS, cardiac arrest, stroke, coronary revascularization): 5.5% vs. 7.1%; p = 0.02 Significant higher rate of Pneumonia (0.9% vs. 0.4%; p = 0.03) |
| Study | Drug | Population | Main Results |
|---|---|---|---|
| ARISE | Succinobucol | ACS n = 6144 | Failure to reduce fatal and non-fatal cardiovascular events in patients with recent ACS. |
| MRC-ILA Heart | Anakinra | ACS n = 182 | Reduction in inflammatory markers 14 days after ACS. Excess of MACE events 1 year after the treatment. |
| SOLID-TIMI-52 | Darapladib | ACS n = 13,026 | Failure to reduce major coronary events in patients with recent ACS. |
| STABILITY | Darapladib | CCS n = 15,828 | Failure to reduce fatal and non-fatal cardiovascular events in patients with CCS. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Maidana, D.; Arroyo-Álvarez, A.; Arenas-Loriente, A.; Barreres-Martín, G.; Muñoz-Alfonso, C.; Bompart Berroteran, D.; Esteve Claramunt, F.; Blanco del Burgo, R.; Cepas-Guillén, P.; Garcia-Blas, S.; et al. Inflammation as a New Therapeutic Target among Older Patients with Ischemic Heart Disease. J. Clin. Med. 2024, 13, 363. https://doi.org/10.3390/jcm13020363
Maidana D, Arroyo-Álvarez A, Arenas-Loriente A, Barreres-Martín G, Muñoz-Alfonso C, Bompart Berroteran D, Esteve Claramunt F, Blanco del Burgo R, Cepas-Guillén P, Garcia-Blas S, et al. Inflammation as a New Therapeutic Target among Older Patients with Ischemic Heart Disease. Journal of Clinical Medicine. 2024; 13(2):363. https://doi.org/10.3390/jcm13020363
Chicago/Turabian StyleMaidana, Daniela, Andrea Arroyo-Álvarez, Andrea Arenas-Loriente, Guillermo Barreres-Martín, Carles Muñoz-Alfonso, Daznia Bompart Berroteran, Francisca Esteve Claramunt, Regina Blanco del Burgo, Pedro Cepas-Guillén, Sergio Garcia-Blas, and et al. 2024. "Inflammation as a New Therapeutic Target among Older Patients with Ischemic Heart Disease" Journal of Clinical Medicine 13, no. 2: 363. https://doi.org/10.3390/jcm13020363
APA StyleMaidana, D., Arroyo-Álvarez, A., Arenas-Loriente, A., Barreres-Martín, G., Muñoz-Alfonso, C., Bompart Berroteran, D., Esteve Claramunt, F., Blanco del Burgo, R., Cepas-Guillén, P., Garcia-Blas, S., & Bonanad, C. (2024). Inflammation as a New Therapeutic Target among Older Patients with Ischemic Heart Disease. Journal of Clinical Medicine, 13(2), 363. https://doi.org/10.3390/jcm13020363








