Lower Lip Reconstruction after Skin Cancer Excision: A Tailored Algorithm for Elderly Patients
Abstract
1. Introduction
2. Patients and Methods
3. Surgical Technique
3.1. Pearls and Pitfalls
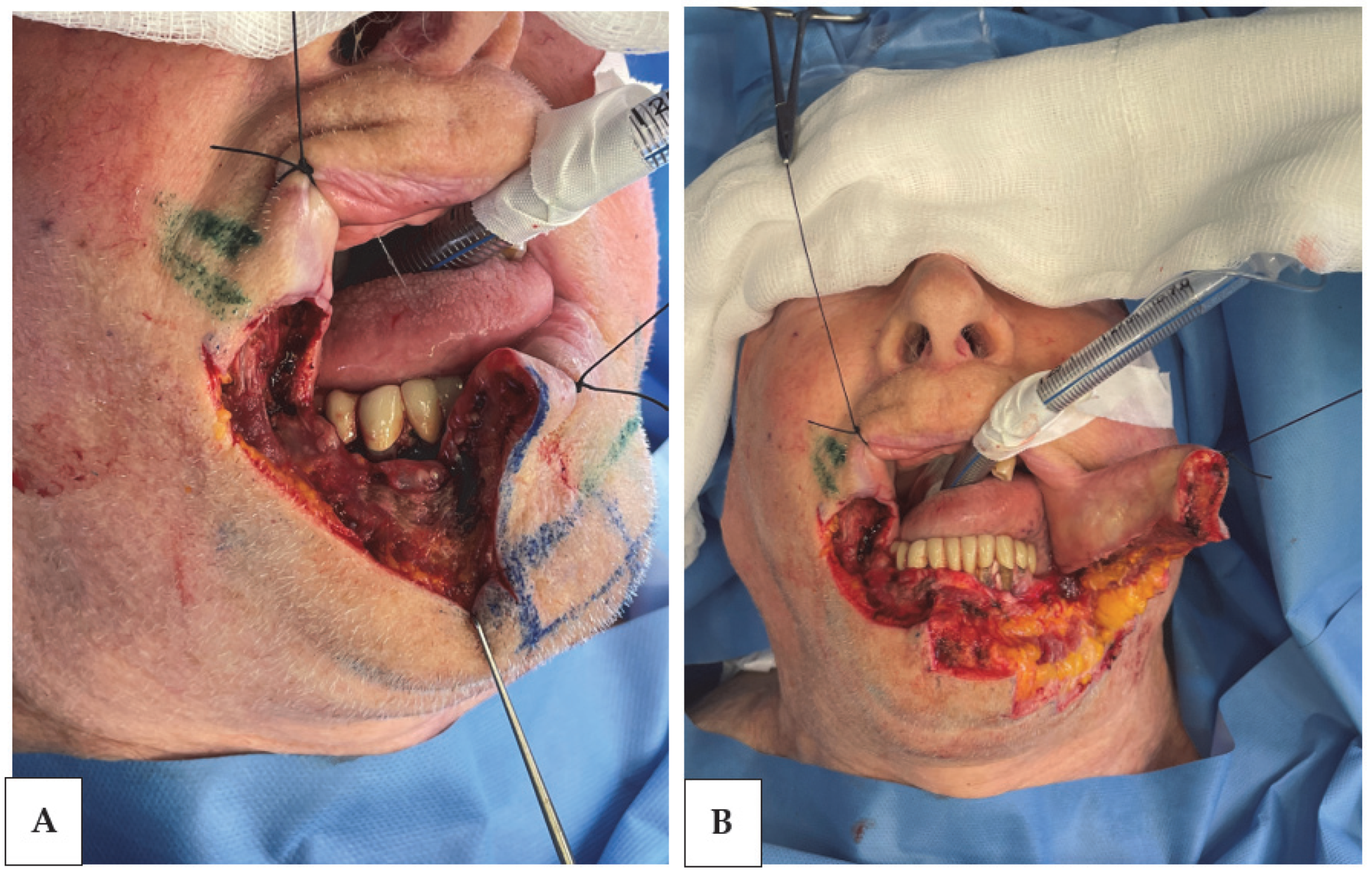
- Prior to excision, a meticulous technique involving the placement of a 0-silk ligature is employed; it was previously introduced as a “traction ligature” (Figure 1).
- During the excision process, our approach diverges from some authors who choose to preserve the mucosal layer, especially in less extensive defects. We opt for a more aggressive stance, creating a full-thickness defect every time the vermillion is involved. This approach ensures not only a higher degree of oncological radicality [6] but also a pleasing labial contour without redundancies.
- On the superficial layer, a vertical mattress suture [7,8] is often preferred for the suture of vermillion to achieve margin eversion and prevent invagination. The cutaneous sutures are applied as interrupted simple stitches, employing the vertical mattress technique “on demand” to prevent invagination in areas that may appear to be prone. Furthermore, Allgöwer–Donati [7] stitches are the chosen technique to suture the corners of the flaps. Within the mucosa, Vicryl rapide 4-0 is employed to reduce patient discomfort.
3.2. Statistical Analysis
4. Results
5. Discussion
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Czerninski, R.; Zini, A.; Sgan-Cohen, H.D. Lip cancer: Incidence, trends, histology, and survival: 1970–2006. Br. J. Dermatol. 2010, 162, 1103–1109. [Google Scholar] [PubMed]
- Losco, L.; Bolletta, A.; Pierazzi, D.M.; Spadoni, D.; Cuomo, R.; Marcasciano, M.; Cavalieri, E.; Roxo, A.C.; Ciamarra, P.; Cantisani, C.; et al. Reconstruction of the Nose: Management of Nasal Cutaneous Defects According to Aesthetic Subunit and Defect Size. A Review. Medicina 2020, 56, 639. [Google Scholar] [CrossRef] [PubMed]
- Roh, D.S.; Panayi, A.C.; Bhasin, S.; Orgill, D.P.; Sinha, I. Implications of Aging in Plastic Surgery. Plast. Reconstr. Surg. Glob. Open 2019, 7, e2085. [Google Scholar] [CrossRef] [PubMed]
- Shaikh, A.I.; Khan, A.H.; Tated, S.; Khubchandani, N. Functional and aesthetic outcome of different methods of reconstruction of full thickness lip defects. GMS Interdiscip. Plast Reconstr. Surg. DGPW 2022, 11, Doc02. [Google Scholar] [CrossRef] [PubMed]
- Simman, R. Wound closure and the reconstructive ladder in plastic surgery. J. Am. Coll. Certif. Wound Spéc. 2009, 1, 6–11. [Google Scholar] [CrossRef]
- Sanniec, K.; Harirah, M.; Thornton, J.F. Lip Reconstruction after Mohs Cancer Excision: Lessons Learned from 615 Consecutive Cases. Plast. Reconstr. Surg. 2020, 145, 533–542. [Google Scholar] [CrossRef]
- Dietz, U.A.; Kuhfuß, I.; Debus, E.; Thiede, A. Mario Donati and the vertical mattress suture of the skin. Mol. Med. 2006, 30, 141–148. [Google Scholar] [CrossRef]
- Park, L.; Lum, Z.; Joo, J.S. Allgöwer-Donati suture: A technique to preserve skin microcirculation in dermatologic surgery. J. Am. Acad. Dermatol. 2023. epub ahead of print. [Google Scholar] [CrossRef]
- Sun, Q.; Chen, X.; Luo, H.; Meng, C.; Zhu, D. Cancer stem cells of head and neck squamous cell carcinoma; distance towards clinical application; a systematic review of literature. Am. J. Cancer Res. 2023, 13, 4315–4345. [Google Scholar]
- Losco, L.; Aksoyler, D.; Chen, S.H.; Bolletta, A.; Velazquez-Mujica, J.; Di Taranto, G.; Lo Torto, F.; Marcasciano, M.; Cigna, E.; Chen, H.C. Pharyngoesophageal reconstruction with free jejunum or radial forearm flap as diversionary conduit: Functional outcomes of patients with persistent dysphagia and aspiration. Microsurgery 2020, 40, 630–638. [Google Scholar] [CrossRef]
- Howard, A.; Agrawal, N.; Gooi, Z. Lip and Oral Cavity Squamous Cell Carcinoma. Hematol. Clin. N. Am. 2021, 35, 895–911. [Google Scholar] [CrossRef] [PubMed]
- Biasoli, R.; Valente, V.B.; Mantovan, B.; Collado, F.U.; Neto, S.C.; Sundefeld, M.L.M.M.; Miyahara, G.I.; Bernabé, D.G. Lip Cancer: A Clinicopathological Study and Treatment Outcomes in a 25-Year Experience. J. Oral Maxillofac. Surg. 2016, 74, 1360–1367. [Google Scholar] [CrossRef] [PubMed]
- Alhabbab, R.; Johar, R. Lip cancer prevalence, epidemiology, diagnosis, and management: A review of the litera-ture. Adv. Oral Maxillofac. Surg. 2022, 6, 100276. [Google Scholar] [CrossRef]
- Paolino, G.; Cardone, M.; Didona, D.; Moliterni, E.; Losco, L.; Corsetti, P.; Schipani, G.; Lopez, T.; Calvieri, S.; Bottoni, U. Prognostic factors in head and neck melanoma according to facial aesthetic units. G Ital. Dermatol. Venereol. 2020, 155, 41–45. [Google Scholar] [CrossRef] [PubMed]
- Yotsuyanagi, T.; Yamashita, K.; Urushidate, S.; Yokoi, K.; Sawada, Y. Reconstruction of large nasal defects with a combination of local flaps based on the aesthetic subunit principle. Plast. Reconstr. Surg. 2001, 107, 1358–1362. [Google Scholar] [CrossRef] [PubMed]
- Yotsuyanagi, T.; Yamashita, K.; Urushidate, S.; Yokoi, K.; Sawada, Y. Nasal reconstruction based on aesthetic subunits in Orientals. Plast. Reconstr. Surg. 2000, 106, 36–44. [Google Scholar] [CrossRef] [PubMed]
- Lo Torto, F.; Losco, L.; Bernardini, N.; Greco, M.; Scuderi, G.; Ribuffo, D. Surgical Treatment with Locoregional Flaps for the Eyelid: A Review. BioMed Res. Int. 2017, 2017, 6742537. [Google Scholar] [CrossRef]
- Sarici, M.; Şirinoğlu, H.; Yeşiloğlu, N.; Temiz, G. May Local Flaps Be an Alternative to Free Flaps in Total Lower Lip and Chin Reconstruction in Elderly Patients. J. Craniofacial Surg. 2016, 27, 1112–1113. [Google Scholar] [CrossRef]
- Nishiguchi, M.A.; Spencer, C.A.; Leung, D.H.; Leung, T.H. Aging Suppresses Skin-Derived Circulating SDF1 to Promote Full-Thickness Tissue Regeneration. Cell Rep. 2018, 24, 3383–3392.e5. [Google Scholar] [CrossRef]
- Colboc, H.; Meaume, S. Scar and Scarring in the Elderly. In Textbook on Scar Management: State of the Art Management and Emerging Technologies; Téot, L., Mustoe, T.A., Middelkoop, E., Gauglitz, G.G., Eds.; Springer: Berlin/Heidelberg, Germany, 2020. [Google Scholar]
- Burgess, J.L.; Wyant, W.A.; Abujamra, B.A.; Kirsner, R.S.; Jozic, I. Diabetic Wound-Healing Science. Medicina 2021, 57, 1072. [Google Scholar] [CrossRef]
- Lo Torto, F.; Redi, U.; Cigna, E.; Losco, L.; Marcasciano, M.; Casella, D.; Ciudad, P.; Ribuffo, D. Nasal Reconstruction With Two Stages Versus Three Stages Forehead Fap: What is Better for Patients With High Vascular Risk? J. Craniofacial Surg. 2020, 31, e57–e60. [Google Scholar] [CrossRef]
- Soliman, S.; Hatef, D.A.; Hollier, L.H.; Thornton, J.F. The Rationale for Direct Linear Closure of Facial Mohs’ Defects. Plast. Reconstr. Surg. 2011, 127, 142–149. [Google Scholar] [CrossRef] [PubMed]
- Johanson, B.; Aspelund, E.; Breine, U.; Holmström, H. Surgical treat-ment of non-traumatic lower lip lesions with special ref-erence to the step technique. Scand. J. Plast. Reconstr. Surg. 1974, 8, 232–240. [Google Scholar]
- Kuttenberger, J.; Hardt, N. Results of a modified staircase technique for reconstruction of the lower lip. J. Cranio-Maxillofac. Surg. 1997, 25, 239–244. [Google Scholar] [CrossRef] [PubMed]
- Pirgousis, P.; Fernandes, R. Reconstruction of subtotal defects of the lower lip: A review of current techniques and a proposed modification. J. Oral Maxillofac. Surg. 2010, 69, 295–299. [Google Scholar] [CrossRef] [PubMed]
- Blomgren, I.; Blomqvist, G.; Lauritzen, C.; Lilja, J.; Peterson, L.-E.; Holmström, H. The step technique for the reconstruction of lower lip defects after cancer resection. A follow-up study of 165 cases. Scand. J. Plast. Reconstr. Surg. 1988, 22, 103–111. [Google Scholar] [CrossRef]
- Dado, D.V.; Angelats, J. Upper and lower lip reconstruction using the step technique. Ann. Plast. Surg. 1985, 15, 204–211. [Google Scholar] [CrossRef]
- Aryanian, Z.; Balighi, K.; Goodarzi, A.; Nia, A.S.; Afshar, Z.M.; Hatami, P. The impact of the COVID-19 pandemic on the diagnosis and treatment of skin cancers, a mini review. Cancer Rep. 2023, 6, e1854. [Google Scholar] [CrossRef]
- Cocuz, I.-G.; Cocuz, M.-E.; Niculescu, R.; Șincu, M.C.; Tinca, A.C.; Sabău, A.-H.; Chiorean, D.M.; Morariu, S.H.; Cotoi, O.S. The Impact of and Adaptations Due to the COVID-19 Pandemic on the Histopathological Diagnosis of Skin Pathologies, Including Non-Melanocyte and Melanoma Skin Cancers—A Single-Center Study in Romania. Medicina 2021, 57, 533. [Google Scholar] [CrossRef]
- Dessinioti, C.; Garbe, C.; Stratigos, A.J. The impact of the COVID-19 pandemic on diagnostic delay of skin cancer: A call to restart screening activities. J. Eur. Acad. Dermatol. Venereol. 2021, 35, E836–E837. [Google Scholar] [CrossRef]
- Slotman, E.; Schreuder, K.; Nijsten, T.; Wakkee, M.; Hollestein, L.; Mooyaart, A.; Siesling, S.; Louwman, M. The impact of the COVID-19 pandemic on keratinocyte carcinoma in the Netherlands: Trends in diagnoses and magnitude of diagnostic delays. J. Eur. Acad. Dermatol. Venereol. 2022, 36, 680–687. [Google Scholar] [CrossRef] [PubMed]
- Alam, M.; Goldberg, L.H.; Silapunt, S.; Gardner, E.S.; Strom, S.S.; Rademaker, A.W.; Margolis, D.J. Delayed treatment and continued growth of nonmelanoma skin cancer. J. Am. Acad. Dermatol. 2011, 64, 839–848. [Google Scholar] [CrossRef]
- Gudzhabidze, K.V.; Mardaleishvili, K.M.; Okropiridze, T.V. The local and general complications after the lower lip cancer treat-ment. Georgian Med. News 2007, 25–28. [Google Scholar]
- Gudmundsson Astrup, J.; Yadete, D. Forsømt non-melanom-hudkræft [Neglected non-melanoma skin cancer]. Ugeskr Laeger. 2012, 174, 876–877. [Google Scholar] [PubMed]
- Wei, F.-C.; Tan, B.-K.; Chen, I.-H.; Hau, S.-P.; Liau, C.-T. Mimicking lip features in free-flap reconstruction of lip defects. Br. J. Plast. Surg. 2001, 54, 8–11. [Google Scholar] [CrossRef]
- Shukla, A.; Loy, K.; Lu, G.N. Total lower lip reconstruction: A review of recent advances. Curr. Opin. Otolaryngol. Head Neck Surg. 2023, 31, 441–451. [Google Scholar] [CrossRef]


| Inclusion Criteria | Exclusion Criteria |
|---|---|
| Reconstruction after cancer excision | Microsurgical technique |
| Involvement of vermillion | Multiple stages reconstruction |
| Age > 65 years | Lack of documentation |
| Follow-up > 6 months | Loss to follow-up |
| Criteria | ||
|---|---|---|
| Subjective | Objective | |
| Normal |
| Both commissure equidistant to NLF and at the level of a vertical line departing from the medial cantus (medial limbus) |
| Moderate |
| One or both commissure lateral to alar groove but medial to medial limbus |
| Severe |
| One or both commissure medial to alar groove |
| V1 | 1 d | 3 d | 7 d | 15 d | 30 d | 3 m | 6 m | |
|---|---|---|---|---|---|---|---|---|
| Informed consent | ● | |||||||
| Evaluation of admission criteria | ● | ● | ● | ● | ● | ● | ● | ● |
| Demographic and anamnestic data | ● | |||||||
| Photographs | ● | ● | ● | ● | ● | ● | ● | ● |
| Associated therapies | ● | ● | ● | ● | ● | ● | ● | ● |
| Vitality of the flap | ● | ● | ● | |||||
| Wound healing | ● | ● | ● | ● | ● | |||
| Complications | ● | ● | ● | ● | ● | ● | ● | |
| Lip functionality * | ● | ● | ● | ● |
| Variable | n (%) |
|---|---|
| Patients | 78 |
| Mean age, years | 81.5 |
Gender
| 49 (62.8%) 29 (37.2%) |
Smoking habit
| 32 (41.0%) 46 (58.9%) |
Anticoagulant assumption
| 42 (53.8%) 36 (45.1%) |
Histology
| 64 (82%) 11 (14.1%) 3 (3.8%) |
| Variable | n (%) |
|---|---|
| Mean area of defect, cm2 | 3308 cm2 |
Area of defect, cm2
| 10 (12.8%) 21 (26.9%) 47 (50.1%) |
| Variable | n (%) |
|---|---|
Area of lesion, cm2
| 16 (20.5%) 27 (34.6%) 34 (43.6%) |
| 1 (1.2%) |
| Technique | Total Patients, n (%) | Average Operation Time (±SD) | Mean Defect Size, cm2 (±SD) |
|---|---|---|---|
| Wedge Resection | 24 (30.7%) | 28 (±2.7 min) | 2.38 (±0.36) |
| Step Technique Flap | 16 (20.5%) | 45.2 (±4.4 min) | 3.2 (±0.2) |
| Karapandzic Flap | 13 (16.6%) | 85.4 (±3.8 min) | 3.9 (±0.2) |
| Gillies Fan Flap | 6 (7.6%) | 84 (±4.4 min) | 3.6 (±0.2) |
| Estlander Flap + Step | 7 (8.9%) | 69.4 (±10.3 min) | 4.1 (±0.1) |
| Estlander Flap | 6 (7.6%) | 44.7 (±1.4 min) | 3.7 (±0.1) |
| Webster flap | 6 (7.6%) | 88.2 (±1.5 min) | 4.4 (±0.1) |
| Complication | n (%) |
|---|---|
| Infection | 0 (0%) |
| Recurrence | 2 (1.5%) |
| Subjective Microstomia | 22 (19.3%) |
| Objective Microstomia | 32 (24.9%) |
| Wound dehiscence | 2 (1.5%) |
| Flap failure | 0 (0%) |
| Bleeding | 0 (0%) |
| Hypoesthesia * | 0 (0%) |
| Technique | Subjective Microstomia, n (%) | Objective Microstomia, n (%) |
|---|---|---|
| Wedge Resection | 1 (4.2%) | 2 (8.3%) |
| Step Technique Flap | 1 (6.3%) | 3 (16.8%) |
| Karapandzic Flap | 9 (69.2%) | 13 (100%) |
| Gillies Fan Flap | 3 (50%%) | 5 (83.3%) |
| Estlander Flap + Step Technique | 3 (42.8%) | 4 (57.1%) |
| Estlander Flap | 1 (16.6%) | 1 (16.6%) |
| Webster flap | 4 (66.6%) | 4 (66.6%) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Russo, R.; Pentangelo, P.; Ceccaroni, A.; Losco, L.; Alfano, C. Lower Lip Reconstruction after Skin Cancer Excision: A Tailored Algorithm for Elderly Patients. J. Clin. Med. 2024, 13, 554. https://doi.org/10.3390/jcm13020554
Russo R, Pentangelo P, Ceccaroni A, Losco L, Alfano C. Lower Lip Reconstruction after Skin Cancer Excision: A Tailored Algorithm for Elderly Patients. Journal of Clinical Medicine. 2024; 13(2):554. https://doi.org/10.3390/jcm13020554
Chicago/Turabian StyleRusso, Raffaele, Paola Pentangelo, Alessandra Ceccaroni, Luigi Losco, and Carmine Alfano. 2024. "Lower Lip Reconstruction after Skin Cancer Excision: A Tailored Algorithm for Elderly Patients" Journal of Clinical Medicine 13, no. 2: 554. https://doi.org/10.3390/jcm13020554
APA StyleRusso, R., Pentangelo, P., Ceccaroni, A., Losco, L., & Alfano, C. (2024). Lower Lip Reconstruction after Skin Cancer Excision: A Tailored Algorithm for Elderly Patients. Journal of Clinical Medicine, 13(2), 554. https://doi.org/10.3390/jcm13020554










