The True Dislocation Incidence following Elective Total Hip Replacement in Sweden: How Does It Relate to the Revision Rate?
Abstract
:1. Introduction
1.1. Background
1.2. Rationale
- a.
- What is the cumulative dislocation incidence after elective primary THA in Sweden, and how does this compare to the revision incidence for dislocation or for any reason?
- b.
- Is there a difference in patient- and surgery-related characteristics between patients dislocating once vs. multiple times within 1 year of index surgery?
- c.
- Is there a difference in patient- and surgery related characteristics between patients revised vs. not revised for dislocation?
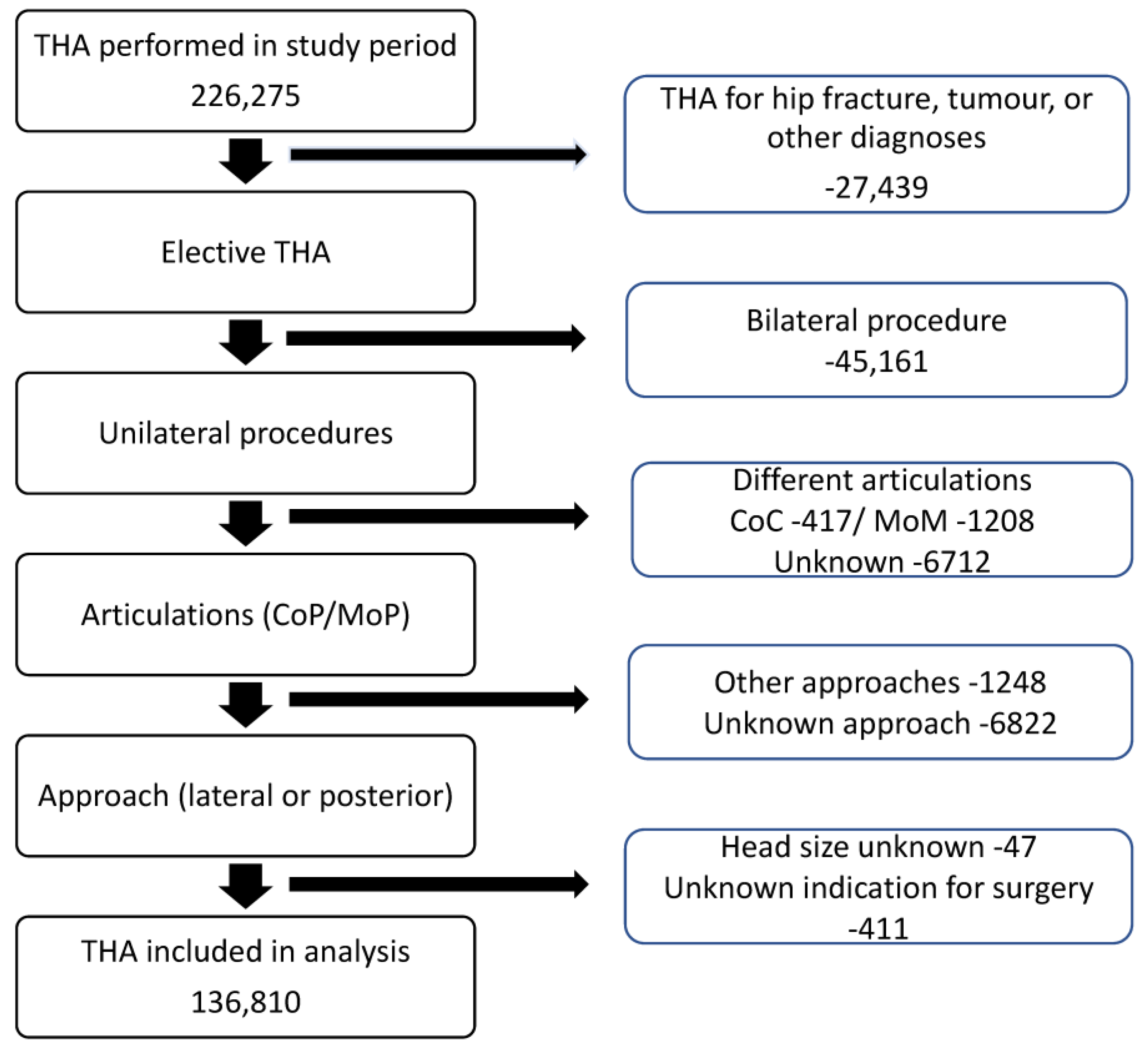
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Wright-Chisem, J.; Elbuluk, A.M.; Mayman, D.J.; Jerabek, S.A.; Sculco, P.K.; Vigdorchik, J.M. The journey to preventing dislocation after total hip arthroplasty: How did we get here? Bone Jt. J. 2022, 104-B, 8–11. [Google Scholar] [CrossRef] [PubMed]
- Van Steenbergen, L.N.; Makela, K.T.; Karrholm, J.; Rolfson, O.; Overgaard, S.; Furnes, O.; Pedersen, A.B.; Eskelinen, A.; Hallan, G.; Schreurs, B.W.; et al. Total hip arthroplasties in the Dutch Arthroplasty Register (LROI) and the Nordic Arthroplasty Register Association (NARA): Comparison of patient and procedure characteristics in 475,685 cases. Acta Orthop. 2021, 92, 15–22. [Google Scholar] [CrossRef] [PubMed]
- Hermansen, L.L.; Viberg, B.; Overgaard, S. Patient-reported outcome after dislocation of primary total hip arthroplasties: A cross-sectional study derived from the Danish Hip Arthroplasty Register. Acta Orthop. 2022, 93, 29–36. [Google Scholar] [CrossRef] [PubMed]
- Gillinov, S.M.; Joo, P.Y.; Zhu, J.R.; Moran, J.; Rubin, L.E.; Grauer, J.N. Incidence, Timing, and Predictors of Hip Dislocation after Primary Total Hip Arthroplasty for Osteoarthritis. J. Am. Acad. Orthop. Surg. 2022, 30, 1047–1053. [Google Scholar] [CrossRef] [PubMed]
- Wyles, C.C.; Maradit-Kremers, H.; Larson, D.R.; Lewallen, D.G.; Taunton, M.J.; Trousdale, R.T.; Pagnano, M.W.; Berry, D.J.; Sierra, R.J. Creation of a Total Hip Arthroplasty Patient-Specific Dislocation Risk Calculator. J. Bone Jt. Surg. 2022, 104, 1068–1080. [Google Scholar] [CrossRef]
- Hermansen, L.L.; Viberg, B.; Overgaard, S. Risk Factors for Dislocation and Re-revision after First-Time Revision Total Hip Arthroplasty due to Recurrent Dislocation—A Study from the Danish Hip Arthroplasty Register. J. Arthroplast. 2021, 36, 1407–1412. [Google Scholar] [CrossRef]
- Toyoda, T.; Oe, K.; Iida, H.; Nakamura, T.; Okamoto, N.; Saito, T. Treatment strategies for recurrent dislocation following total hip arthroplasty: Relationship between cause of dislocation and type of revision surgery. BMC Musculoskelet. Disord. 2023, 24, 238. [Google Scholar] [CrossRef]
- Jo, S.; Jimenez Almonte, J.H.; Sierra, R.J. The Cumulative Risk of Re-dislocation after Revision THA Performed for Instability Increases Close to 35% at 15 years. J. Arthroplast. 2015, 30, 1177–1182. [Google Scholar] [CrossRef]
- Khoshbin, A.; Haddad, F.S.; Ward, S.; O’ hEireamhoin, S.; Wu, J.; Nherera, L.; Atrey, A. A cost-effectiveness assessment of dual-mobility bearings in revision hip arthroplasty. Bone Jt. J. 2020, 102-B, 1128–1135. [Google Scholar] [CrossRef]
- Phillips, J.L.H.; Rondon, A.J.; Vannello, C.; Fillingham, Y.A.; Austin, M.S.; Courtney, P.M. How Much Does a Readmission Cost the Bundle Following Primary Hip and Knee Arthroplasty? J. Arthroplast. 2019, 34, 819–823. [Google Scholar] [CrossRef]
- Koenig, L.; Feng, C.; He, F.; Nguyen, J.T. The Effects of Revision Total Hip Arthroplasty on Medicare Spending and Beneficiary Outcomes: Implications for the Comprehensive Care for Joint Replacement Model. J. Arthroplast. 2018, 33, 2764–2769.e2. [Google Scholar] [CrossRef] [PubMed]
- Abdel, M.P.; Cross, M.B.; Yasen, A.T.; Haddad, F.S. The functional and financial impact of isolated and recurrent dislocation after total hip arthroplasty. Bone Jt. J. 2015, 97-B, 1046–1049. [Google Scholar] [CrossRef] [PubMed]
- Galvain, T.; Mantel, J.; Kakade, O.; Board, T.N. Treatment patterns and clinical and economic burden of hip dislocation following primary total hip arthroplasty in England. Bone Jt. J. 2022, 104-B, 811–819. [Google Scholar] [CrossRef] [PubMed]
- Hermansen, L.L.; Viberg, B.; Hansen, L.; Overgaard, S. “True” Cumulative Incidence of and Risk Factors for Hip Dislocation within 2 Years after Primary Total Hip Arthroplasty Due to Osteoarthritis: A Nationwide Population-Based Study from the Danish Hip Arthroplasty Register. J. Bone Jt. Surg. 2021, 103, 295–302. [Google Scholar] [CrossRef] [PubMed]
- Farey, J.E.; Masters, J.; Cuthbert, A.R.; Iversen, P.; van Steenbergen, L.N.; Prentice, H.A.; Adie, S.; Sayers, A.; Whitehouse, M.R.; Paxton, E.W.; et al. Do Dual-mobility Cups Reduce Revision Risk in Femoral Neck Fractures Compared with Conventional THA Designs? An International Meta-analysis of Arthroplasty Registries. Clin. Orthop. Relat. Res. 2022, 480, 1912–1925. [Google Scholar] [CrossRef] [PubMed]
- Kreipke, R.; Rogmark, C.; Pedersen, A.B.; Kärrholm, J.; Hallan, G.; Havelin, L.I.; Mäkelä, K.; Overgaard, S. Dual Mobility Cups: Effect on Risk of Revision of Primary Total Hip Arthroplasty Due to Osteoarthritis: A Matched Population-Based Study Using the Nordic Arthroplasty Register Association Database. J. Bone Jt. Surg. 2019, 101, 169–176. [Google Scholar] [CrossRef]
- van Steenbergen, L.N.; de Reus, I.M.; Hannink, G.; Vehmeijer, S.B.; Schreurs, B.W.; Zijlstra, W.P. Femoral head size and surgical approach affect dislocation and overall revision rates in total hip arthroplasty: Up to 9-year follow-up data of 269,280 procedures in the Dutch Arthroplasty Register (LROI). Hip Int. 2023, 33, 1056–1062. [Google Scholar] [CrossRef]
- Hoskins, W.; Rainbird, S.; Holder, C.; Stoney, J.; Graves, S.E.; Bingham, R. A Comparison of Revision Rates and Dislocation after Primary Total Hip Arthroplasty with 28, 32, and 36-mm Femoral Heads and Different Cup Sizes: An Analysis of 188,591 Primary Total Hip Arthroplasties. J. Bone Jt. Surg. 2022, 104, 1462–1474. [Google Scholar] [CrossRef]
- Hoskins, W.; Rainbird, S.; Dyer, C.; Graves, S.E.; Bingham, R. In Revision THA, Is the Re-revision Risk for Dislocation and Aseptic Causes Greater in Dual-mobility Constructs or Large Femoral Head Bearings? A Study from the Australian Orthopaedic Association National Joint Replacement Registry. Clin. Orthop. Relat. Res. 2022, 480, 1091–1101. [Google Scholar] [CrossRef]
- Hoskins, W.; Griffin, X.; Hatton, A.; de Steiger, R.N.; Bingham, R. THA for a Fractured Femoral Neck: Comparing the Revision and Dislocation Rates of Standard-head, Large-head, Dual-mobility, and Constrained Liners. Clin. Orthop. Relat. Res. 2021, 479, 72–81. [Google Scholar] [CrossRef]
- Hoskins, W.; Bingham, R.; Dyer, C.; Rainbird, S.; Graves, S.E. A Comparison of Revision Rates for Dislocation and Aseptic Causes Between Dual Mobility and Large Femoral Head Bearings in Primary Total Hip Arthroplasty with Subanalysis by Acetabular Component Size: An Analysis of 106,163 Primary Total Hip Arthroplasties. J. Arthroplast. 2021, 36, 3233–3240. [Google Scholar] [CrossRef] [PubMed]
- Rogmark, C.; Natman, J.; Jobory, A.; Hailer, N.P.; Cnudde, P. The association of surgical approach and bearing size and type with dislocation in total hip arthroplasty for acute hip fracture. Bone Jt. J. 2022, 104-B, 844–851. [Google Scholar] [CrossRef] [PubMed]
- Cnudde, P.H.J.; Nåtman, J.; Hailer, N.P.; Rogmark, C. Total, hemi, or dual-mobility arthroplasty for the treatment of femoral neck fractures in patients with neurological disease: Analysis of 9638 patients from the Swedish Hip Arthroplasty Register. Bone Jt. J. 2022, 104-B, 134–141. [Google Scholar] [CrossRef] [PubMed]
- Cnudde, P.; Rolfson, O.; Nemes, S.; Karrholm, J.; Rehnberg, C.; Rogmark, C.; Timperley, J.; Garellick, G. Linking Swedish health data registers to establish a research database and a shared decision-making tool in hip replacement. BMC Musculoskelet. Disord. 2016, 17, 414. [Google Scholar] [CrossRef] [PubMed]
- Rolfson, O.E.A. Annual Report 2022; The Swedish Arthroplasty Register: Gothenburg, Sweden, 2022; pp. 1654–5982. [Google Scholar]
- Hermansen, L.L.; Viberg, B.; Overgaard, S. Development of a diagnostic algorithm identifying cases of dislocation after primary total hip arthroplasty-based on 31,762 patients from the Danish Hip Arthroplasty Register. Acta Orthop. 2021, 92, 137–142. [Google Scholar] [CrossRef] [PubMed]
- Blumenfeld, T.J. How Prescient Can We Be?: Commentary on an article by Cody, C., Wyles, M.D., et al.: “Creation of a Total Hip Arthroplasty Patient-Specific Dislocation Risk Calculator”. J. Bone Jt. Surg. 2022, 104, 1129. [Google Scholar] [CrossRef] [PubMed]
- von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gotzsche, P.C.; Vandenbroucke, J.P.; Initiative, S. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: Guidelines for reporting observational studies. Lancet 2007, 370, 1453–1457. [Google Scholar] [CrossRef]
- Malkani, A.L.; Ong, K.L.; Lau, E.; Kurtz, S.M.; Justice, B.J.; Manley, M.T. Early- and Late-Term Dislocation Risk after Primary Hip Arthroplasty in the Medicare Population. J. Arthroplast. 2010, 25, 21–25. [Google Scholar] [CrossRef]
- Sirignano, M.N.; Nessler, J.M.; Rhea, E.B.; Ong, K.L.; Watson, H.N.; Yakkanti, M.R.; Malkani, A.L. Incidence of Instability Following Primary Total Hip Arthroplasty Continues to Decline in the Medicare Population. J. Arthroplast. 2023, 38, S89–S94.e1. [Google Scholar] [CrossRef]
- Norambuena, G.A.; Wyles, C.C.; Van Demark, R.E., 3rd; Trousdale, R.T. Effect of dislocation timing following primary total hip arthroplasty on the risk of redislocation and revision. Hip Int. 2019, 29, 489–495. [Google Scholar] [CrossRef]
- Itokawa, T.; Nakashima, Y.; Yamamoto, T.; Motomura, G.; Ohishi, M.; Hamai, S.; Akiyama, M.; Hirata, M.; Hara, D.; Iwamoto, Y. Late dislocation is associated with recurrence after total hip arthroplasty. Int. Orthop. 2013, 37, 1457–1463. [Google Scholar] [CrossRef] [PubMed]
- Cnudde, P.; Nemes, S.; Bulow, E.; Timperley, J.; Malchau, H.; Karrholm, J.; Garellick, G.; Rolfson, O. Trends in hip replacements between 1999 and 2012 in Sweden. J. Orthop. Res. 2017, 36, 432–442. [Google Scholar] [CrossRef] [PubMed]
- Sanchez-Sotelo, J.; Haidukewych, G.J.; Boberg, C.J. Hospital Cost of Dislocation after Primary Total Hip Arthroplasty. J. Bone Jt. Surg. 2006, 88, 290–294. [Google Scholar] [CrossRef] [PubMed]
- Browne, J.A.; Springer, B.; Spindler, K.P. Optimizing Use of Large Databases in Joint Arthroplasty and Orthopaedics. J. Bone Jt. Surg. 2022, 104, 28–32. [Google Scholar] [CrossRef] [PubMed]
- Pugely, A.J.; Martin, C.T.; Harwood, J.; Ong, K.L.; Bozic, K.J.; Callaghan, J.J. Database and Registry Research in Orthopaedic Surgery: Part 2: Clinical Registry Data. J. Bone Jt. Surg. 2015, 97, 1799–1808. [Google Scholar] [CrossRef]
- Pugely, A.J.; Martin, C.T.; Harwood, J.; Ong, K.L.; Bozic, K.J.; Callaghan, J.J. Database and Registry Research in Orthopaedic Surgery: Part I: Claims-Based Data. J. Bone Jt. Surg. 2015, 97, 1278–1287. [Google Scholar] [CrossRef]
- Abdel, M.P.; von Roth, P.; Jennings, M.T.; Hanssen, A.D.; Pagnano, M.W. What safe zone? The vast majority of dislocated THAs are within the Lewinnek safe zone for acetabular component position. Clin. Orthop. Relat. Res. 2016, 474, 386–391. [Google Scholar] [CrossRef]
- Cnudde, P.H.J.; Nemes, S.; Bulow, E.; Timperley, A.J.; Whitehouse, S.L.; Karrholm, J.; Rolfson, O. Risk of further surgery on the same or opposite side and mortality after primary total hip arthroplasty: A multi-state analysis of 133,654 patients from the Swedish Hip Arthroplasty Register. Acta Orthop. 2018, 89, 386–393. [Google Scholar] [CrossRef]

| Absolute Number | % | ||
|---|---|---|---|
| Study group | 136,810 | 100 | |
| Indication for primary surgery | Primary OA | 122,751 | 89.7 |
| Secondary OA, unspecified | 5139 | 3.8 | |
| Sequelae from childhood hip disorders | 3205 | 2.3 | |
| Inflammatory joint disease | 2832 | 2.1 | |
| Avascular necrosis femoral head (primary) | 2877 | 2.1 | |
| Sex | Female | 77,644 | 57.8 |
| Male | 59,166 | 43.2 | |
| Hospital category | University or regional hospitals | 12,773 | 9.4 |
| County hospitals | 46,021 | 33.9 | |
| Rural hospitals | 55,489 | 40.9 | |
| Private hospitals | 21,505 | 15.8 | |
| Fixation | Fully cemented | 102,659 | 75.0 |
| Hybrid | 4986 | 3.6 | |
| Reverse hybrid | 12,732 | 9.3 | |
| Uncemented | 16,433 | 12.0 | |
| Approach | Posterior | 77,013 | 56.3 |
| Lateral | 59,797 | 43.7 | |
| Bearing type and size | cTHA < 32 mm | 89,608 | 65.5 |
| cTHA 32 mm | 40,930 | 29.9 | |
| cTHA > 32 mm | 4670 | 3.4 | |
| THA-DMC | 1602 | 1.2 | |
| Year of surgery | 1999–2000 | 6428 | 4.7 |
| 2001–2002 | 14,353 | 10.5 | |
| 2003–2004 | 16,507 | 12.1 | |
| 2005–2006 | 18,116 | 13.2 | |
| 2007–2008 | 18,344 | 13.4 | |
| 2009–2010 | 20,843 | 15.2 | |
| 2011–2012 | 21,024 | 15.4 | |
| 2013–2014 | 21,205 | 15.5 | |
| Preoperative diagnosis of a neurological disorder | Yes | 3013 | 2.2 |
| No | 133,797 | 97.8 | |
| Preoperative diagnosis of spinal disease | Yes | 11,573 | 8.5 |
| No | 125,237 | 91.5 | |
| Elixhauser comorbidity index (mean) (SD) | 0.58 (0.96) | ||
| Elixhauser comorbidity category | 0 | 87,236 | 63.8 |
| 1 | 29,804 | 21.8 | |
| 2 | 12,727 | 9.3 | |
| 3 | 4739 | 3.5 | |
| 4+ | 2304 | 1.7 | |
| Age (mean) SD | 67.9 (10.7) | ||
| Age category | <55 | 14,393 | 10.5 |
| 55–69 | 58,035 | 42.4 | |
| 70–84 | 59,038 | 43.2 | |
| 85+ | 5344 | 3.9 | |
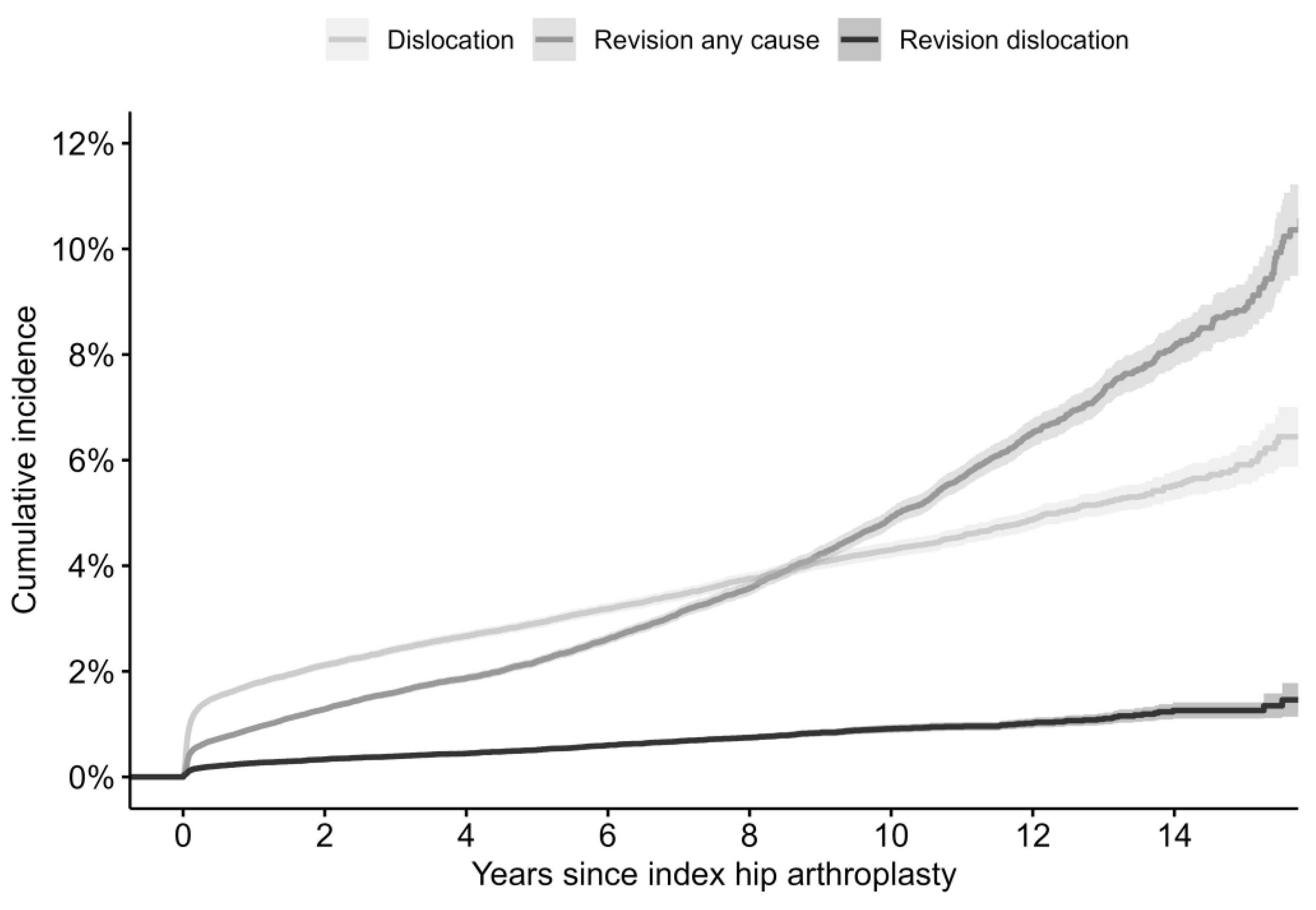
| Cumulative Dislocation Incidence (%) | Cumulative Revision for Dislocation Incidence (%) | Cumulative Revision for Any Reason Incidence (%) | |
|---|---|---|---|
| 30 days | 0.9 (0.9–1.0) | 0.1 (0.1–0.1) | 0.4 (0.4–0.4) |
| 90 days | 1.3 (1.3–1.4) | 0.2 (0.1–0.2) | 0.6 (0.6–0.6) |
| 1 year | 1.8 (1.7–1.8) | 0.3 (0.2–0.3) | 0.9 (0.9–1.0) |
| 2 years | 2.1 (2.0–2.2) | 0.3 (0.3–0.4) | 1.3 (1.2–1.3) |
| 3 years | 2.4 (2.3–2.5) | 0.4 (0.4–0.4) | 1.6 (1.5–1.7) |
| 4 years | 2.7 (2.6–2.8) | 0.4 (0.4–0.5) | 1.9 (1.8–1.9) |
| 5 years | 2.9 (2.8–3.0) | 0.5 (0.5–0.6) | 2.2 (2.1–2.3) |
| 10 years | 4.3 (4.1–4.4) | 0.9 (0.8–1.0) | 4.9 (4.7–5.1) |
| 15 years | 5.9 (5.5–6.3) | 1.3 (1.1–1.4) | 8.9 (8.4–9.4) |
| Single Dislocation | Multiple Dislocations | p-Value | ||
|---|---|---|---|---|
| Study group | 1178 | 1049 | ||
| Indication for primary surgery (%) | Primary OA | 1017 (86.3) | 867 (82.7) | 0.035 |
| Secondary OA, unspecified | 64 (5.4) | 56 (5.3) | ||
| Sequelae from childhood hip disorders | 20 (1.7) | 18 (1.7) | ||
| Inflammatory joint disease | 31 (2.6) | 43 (4.1) | ||
| Avascular necrosis femoral head (primary) | 46 (3.9) | 65 (6.2) | ||
| Sex (%) | Female | 606 (51.4) | 538 (51.3) | 0.975 |
| Male | 572 (48.6) | 511 (48.7) | ||
| Hospital category (%) | University or regional hospitals | 87 (7.5) | 119 (11.4) | 0.001 |
| County hospitals | 446 (38.3) | 414 (39.5) | ||
| Rural hospitals | 455 (39.0) | 396 (37.8) | ||
| Private hospitals | 178 (15.3) | 118 (11.3) | ||
| Fixation (%) | Fully cemented | 948 (80.5) | 851 (81.1) | 0.514 |
| Hybrid | 34 (2.9) | 33 (3.1) | ||
| Reverse hybrid | 79 (6.7) | 55 (5.2) | ||
| Uncemented | 117 (9.9) | 110 (10.5) | ||
| Approach (%) | Posterior | 848 (72.0) | 752 (71.7) | 0.913 |
| Lateral | 330 (28.0) | 297 (28.3) | ||
| Bearing type and size (%) | cTHA < 32 mm | 838 (71.1) | 764 (72.8) | 0.808 |
| cTHA 32 mm | 305 (25.9) | 256 (24.4) | ||
| cTHA > 32 mm | 33 (2.8) | 28 (2.7) | ||
| THA-DMC | 2 (0.2) | 1 (0.1) | ||
| Year of surgery (%) | 1999–2000 | 69 (5.9) | 39 (3.7) | 0.115 |
| 2001–2002 | 140 (11.9) | 126 (12.0) | ||
| 2003–2004 | 160 (13.6) | 150 (14.3) | ||
| 2005–2006 | 153 (13.0) | 166 (15.8) | ||
| 2007–2008 | 163 (13.8) | 150 (14.3) | ||
| 2009–2010 | 170 (14.4) | 159 (15.2) | ||
| 2011–2012 | 168 (14.3) | 123 (11.7) | ||
| 2013–2014 | 155 (13.2) | 136 (13.0) | ||
| Preoperative diagnosis of a neurological disorder (%) | Yes | 45 (3.8) | 60 (5.7) | 0.044 |
| No | 1133 (96.2) | 989 (94.3) | ||
| Preoperative diagnosis of spinal disease (%) | Yes | 155 (13.2) | 139 (13.3) | 0.998 |
| No | 1023 (86.8) | 910 (86.7) | ||
| Elixhauser comorbidity index (mean) (SD) | 0.75 (1.10) | 0.95 (1.17) | <0.001 | |
| Elixhauser category | 0 | 667 (56.6) | 485 (46.2) | 0.524 |
| 1 | 292 (24.8) | 301 (28.7) | ||
| 2 | 129 (11.0) | 162 (15.4) | ||
| 3 | 51 (4.3) | 57 (5.4) | ||
| 4+ | 39 (3.3) | 44 (4.2) | ||
| Age (mean) (SD) | 70.40 (10.28) | 71.28 (10.05) | 0.044 | |
| Age category (%) | <55 | 75 (6.4) | 64 (6.1) | 0.495 |
| 55–69 | 445 (37.8) | 367 (35.0) | ||
| 70–84 | 585 (49.7) | 544 (51.9) | ||
| 85+ | 73 (6.2) | 74 (7.1) | ||
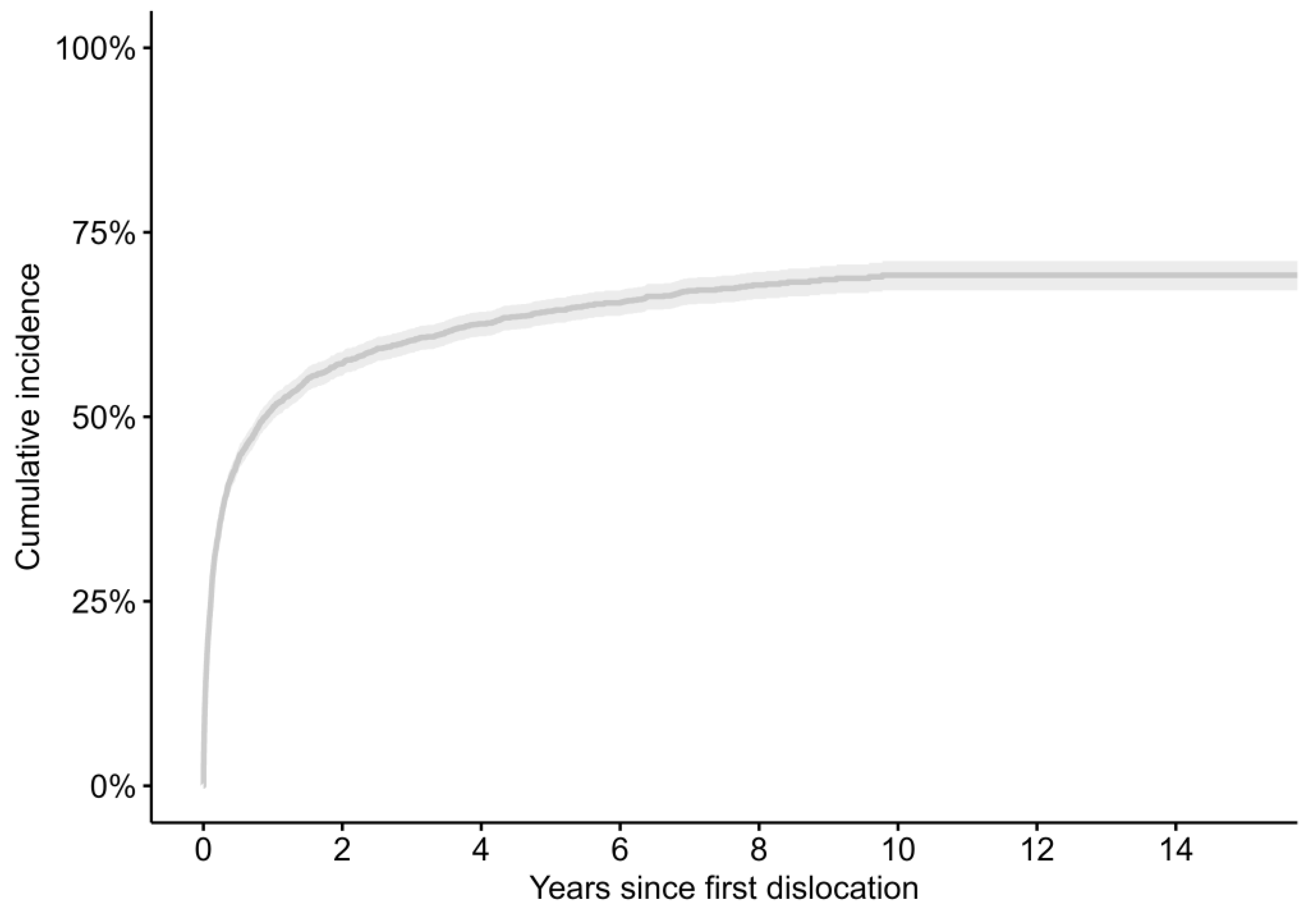
| Kaplan–Meier Estimates for Time between Dislocation and Revision for Dislocation (%) (95% CI) | Kaplan–Meier Estimates for Time between Dislocation and Revision for Any Cause (%) (95% CI) | |
|---|---|---|
| 30 days | 4.2 (3.6–4.8) | 5.8 (5.1–6.5) |
| 90 days | 6.1 (5.3–6.8) | 8.2 (7.3–9) |
| 6 months | 8.2 (7.3–9) | 10.5 (9.5–11.4) |
| 1 year | 10.9 (9.9–11.9) | 13.6 (12.5–14.6) |
| 2 years | 14.5 (13.3–15.6) | 17.5 (16.2–18.7) |
| 3 years | 16.4 (15.2–17.7) | 19.8 (18.5–21.1) |
| 4 years | 17.8 (16.5–19.1) | 21.5 (20.1–22.8) |
| 5 years | 19.4 (18–20.8) | 23.3 (21.8–24.8) |
| 10 years | 24.3 (22.4–26.2) | 30.1 (27.9–32.2) |
| 15 years | 24.6 (22.6–26.5) | 31.9 (29–34.7) |
| Not Revised within a Year after First Dislocation | Revised within a Year after First Dislocation | p-Value | ||
|---|---|---|---|---|
| Study group | 1677 | 296 | ||
| Indication for primary surgery (%) | Primary OA | 1427 (85.1) | 243 (82.1) | 0.171 |
| Secondary OA, unspecified | 95 (5.7) | 15 (5.1) | ||
| Sequelae from childhood hip disorders | 25 (1.5) | 10 (3.4) | ||
| Inflammatory joint disease | 56 (3.3) | 12 (4.1) | ||
| Avascular necrosis femoral head (primary) | 74 (4.4) | 16 (5.4) | ||
| Sex (%) | Female | 871 (51.9) | 152 (51.4) | 0.902 |
| Male | 806 (48.1) | 144 (48.6) | ||
| Hospital category (%) | University or regional hospitals | 141 (8.4) | 39 (13.2) | 0.004 |
| County hospitals | 672 (40.3) | 99 (33.6) | ||
| Rural hospitals | 658 (39.4) | 109 (36.9) | ||
| Private hospitals | 198 (11.9) | 48 (16.3) | ||
| Fixation (%) | Fully cemented | 1415 (84.4) | 212 (71.6) | <0.001 |
| Hybrid | 49 (2.9) | 11 (3.7) | ||
| Reverse hybrid | 86 (5.1) | 31 (10.5) | ||
| Uncemented | 127 (7.6) | 42 (14.2) | ||
| Approach (%) | Posterior | 1256 (74.9) | 171 (57.8) | <0.001 |
| Lateral | 421 (25.1) | 125 (42.2) | ||
| Bearing type and size (%) | cTHA < 32 mm | 1284 (76.6) | 214 (72.3) | 0.344 |
| cTHA 32 mm | 351 (20.9) | 74 (25.0) | ||
| cTHA > 32 mm | 40 (2.4) | 7 (2.4) | ||
| THA-DMC | 2 (0.1) | 1 (0.3) | ||
| Year of surgery (%) | 1999–2000 | 89 (5.3) | 11 (3.7) | 0.010 |
| 2001–2002 | 224 (13.4) | 27 (9.1) | ||
| 2003–2004 | 255 (15.2) | 43 (14.5) | ||
| 2005–2006 | 260 (15.5) | 45 (15.2) | ||
| 2007–2008 | 242 (14.4) | 59 (19.9) | ||
| 2009–2010 | 263 (15.7) | 43 (14.5) | ||
| 2011–2012 | 239 (14.3) | 36 (12.2) | ||
| 2013–2014 | 105 (6.3) | 32 (10.8) | ||
| Preoperative diagnosis of a neurological disorder (%) | Yes | 71 (4.2) | 19 (6.4) | 0.131 |
| No | 1606 (95.8) | 277 (93.4) | ||
| Preoperative diagnosis of spinal disease (%) | Yes | 198 (11.8) | 40 (13.5) | 0.463 |
| No | 1479 (88.2) | 256 (86.5) | ||
| Elixhauser comorbidity index (mean) (SD) | 0.80 (1.11) | 0.87 (1.11) | 0.320 | |
| Elixhauser category | 0 | 888 (53.0) | 142 (48.0) | 0.524 |
| 1 | 450 (26.8) | 89 (30.1) | ||
| 2 | 209 (12.5) | 40 (13.5) | ||
| 3 | 72 (4.3) | 16 (5.4) | ||
| 4+ | 58 (3.5) | 9 (3.0) | ||
| Age (mean) (SD) | 70.94 (10.03) | 69.35 (10.47) | 0.013 | |
| Age category (%) | <55 | 92 (5.5) | 27 (9.1) | 0.050 |
| 55–69 | 619 (36.9) | 115 (38.9) | ||
| 70–84 | 856 (51.0) | 140 (47.3) | ||
| 85+ | 110 (6.6) | 14 (4.7) | ||
| Number of dislocations in the first year (mean (SD)) | 1.78 (1.27) | 3.81 (2.63) | <0.001 | |
| Number of patients with multiple dislocations in the first year (%) | 698 (41.6) | 237 (80.1) | <0.001 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cnudde, P.H.J.; Nåtman, J.; Rolfson, O.; Hailer, N.P. The True Dislocation Incidence following Elective Total Hip Replacement in Sweden: How Does It Relate to the Revision Rate? J. Clin. Med. 2024, 13, 598. https://doi.org/10.3390/jcm13020598
Cnudde PHJ, Nåtman J, Rolfson O, Hailer NP. The True Dislocation Incidence following Elective Total Hip Replacement in Sweden: How Does It Relate to the Revision Rate? Journal of Clinical Medicine. 2024; 13(2):598. https://doi.org/10.3390/jcm13020598
Chicago/Turabian StyleCnudde, Peter H. J., Jonatan Nåtman, Ola Rolfson, and Nils P. Hailer. 2024. "The True Dislocation Incidence following Elective Total Hip Replacement in Sweden: How Does It Relate to the Revision Rate?" Journal of Clinical Medicine 13, no. 2: 598. https://doi.org/10.3390/jcm13020598





