Cervical Multifidus and Longus Colli Ultrasound Differences among Patients with Cervical Disc Bulging, Protrusion and Extrusion and Asymptomatic Controls: A Cross-Sectional Study
Abstract
1. Introduction
2. Methods
2.1. Study Design
2.2. Participants
2.3. Sample Size Calculation
2.4. Outcomes
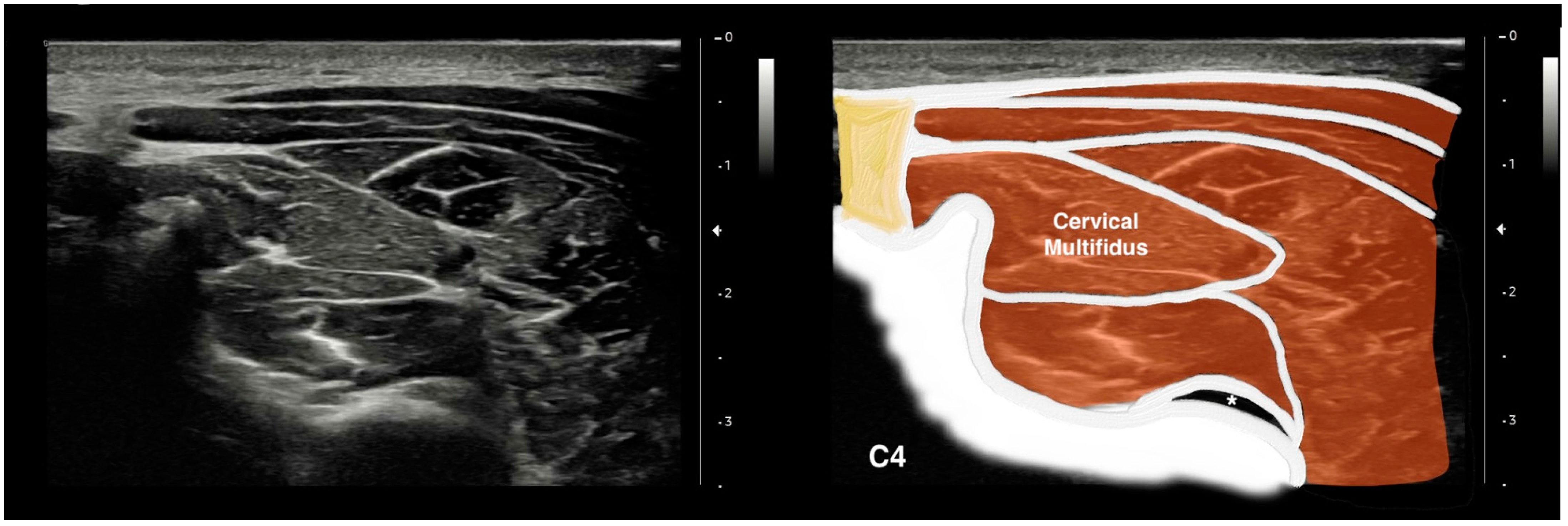
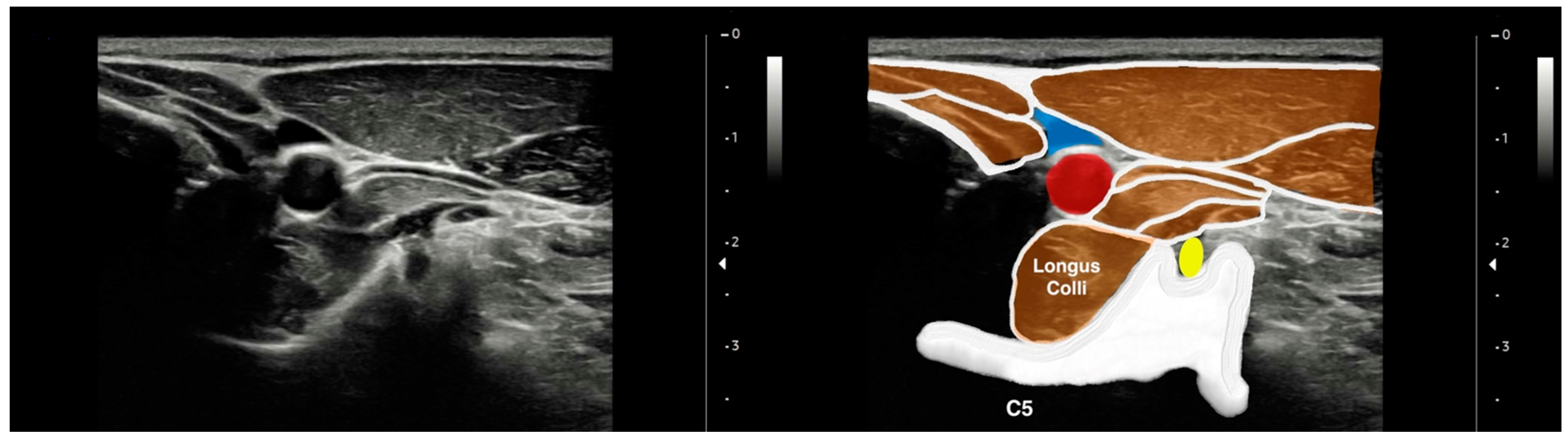
2.4.1. Cervical Multifidus and Longus Colli Imaging Acquisition
2.4.2. Ultrasound Imaging Measurement
2.4.3. Clinical Features: Neck Pain Intensity and Related Disability
2.5. Statistical Analyses
3. Results
3.1. Participants
3.2. Ultrasound Measurements of the Cervical Multifidus
3.3. Ultrasound Measurements of the Longus Colli
3.4. Effects of Covariates in Ultrasound Measurements
3.5. Correlation Analysis
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Anderson, J.S.; Hsu, A.W.; Vasavada, A.N. Morphology, architecture, and biomechanics of human cervical multifidus. Spine 2005, 30, E86–E91. [Google Scholar] [CrossRef] [PubMed]
- Schomacher, J.; Falla, D. Function and structure of the deep cervical extensor muscles in patients with neck pain. Man. Ther. 2013, 18, 360–366. [Google Scholar] [CrossRef] [PubMed]
- Abbott, R.; Pedler, A.; Sterling, M.; Hides, J.; Murphey, T.; Hoggarth, M.; Elliott, J.M. The geography of fatty infiltrates within the cervical multifidus and semispinalis cervicis in individuals with chronic whiplash-associated disorders. J. Orthop. Sports Phys. Ther. 2015, 45, 281–288. [Google Scholar] [CrossRef] [PubMed]
- Snodgrass, S.J.; Stanwell, P.; Weber, K.A.; Shepherd, S.; Kennedy, O.; Thompson, H.J.; Elliott, J.M. Greater muscle volume and muscle fat infiltrate in the deep cervical spine extensor muscles (multifidus with semispinalis cervicis) in individuals with chronic idiopathic neck pain compared to age and sex-matched asymptomatic controls: A cross-sectional study. BMC Musculoskelet. Disord. 2022, 23, 973. [Google Scholar] [CrossRef]
- Yun, Y.; Lee, E.J.; Kim, Y.; Kim, J.C.; Lee, S.A.; Chon, J. Asymmetric atrophy of cervical multifidus muscles in patients with chronic unilateral cervical radiculopathy. Medicine 2019, 98, e16041. [Google Scholar] [CrossRef]
- Li, Z.; Liang, Q.; Li, H.; Lin, X.; Meng, J.; Yang, D.; Li, C.; Liang, Y.; Yang, Y.; Lin, Y.; et al. Fatty infiltration of the cervical multifidus musculature and its clinical correlation to cervical spondylosis. BMC Musculoskelet. Disord. 2023, 24, 613. [Google Scholar] [CrossRef]
- Cloney, M.; Smith, A.C.; Coffey, T.; Paliwal, M.; Dhaher, Y.; Parrish, T.; Elliott, J.; Smith, Z.A. Fatty infiltration of the cervical multifidus musculature and their clinical correlates in spondylotic myelopathy. J. Clin. Neurosci. 2018, 57, 208–213. [Google Scholar] [CrossRef]
- Fortin, M.; Wilk, N.; Dobrescu, O.; Martel, P.; Santaguida, C.; Weber, M.H. Relationship between cervical muscle morphology evaluated by MRI, cervical muscle strength and functional outcomes in patients with degenerative cervical myelopathy. Musculoskelet. Sci. Pract. 2018, 38, 1–7. [Google Scholar] [CrossRef]
- Owers, D.S.; Perriman, D.M.; Smith, P.N.; Neeman, T.; Webb, A.L. Evidence for cervical muscle morphometric changes on magnetic resonance images after whiplash: A systematic review and meta-analysis. Injury 2018, 49, 165–176. [Google Scholar] [CrossRef]
- Siasios, I.; Samara, E.; Fotiadou, A.; Tsoleka, K.; Vadikolias, K.; Mantatzis, M.; Birbilis, T. The role of cervical muscles morphology in the surgical treatment of degenerative disc disease: Clinical correlations based on magnetic resonance imaging studies. J. Clin. Med. Res. 2021, 13, 367–376. [Google Scholar] [CrossRef]
- Fortin, M.; Dobrescu, O.; Courtemanche, M.; Sparrey, C.J.; Santaguida, C.; Fehlings, M.G.; Weber, M.H. Association between paraspinal muscle morphology, clinical symptoms, and functional status in patients with degenerative cervical myelopathy. Spine 2017, 42, 232–239. [Google Scholar] [CrossRef] [PubMed]
- Blanpied, P.R.; Gross, A.R.; Elliott, J.M.; Devaney, L.L.; Clewley, D.; Walton, D.M.; Sparks, C.; Robertson, E.K. Neck Pain: Revision 2017. J. Orthop. Sports Phys. Ther. 2017, 47, A1–A83. [Google Scholar] [CrossRef] [PubMed]
- Martín-Vera, D.; Sánchez-Sierra, A.; González-de-la-Flor, Á.; García-Pérez-de-Sevilla, G.; Domínguez-Balmaseda, D.; Del-Blanco-Muñiz, J.Á. Efficacy of a strength-based exercise program in patients with chronic tension type headache: A randomized controlled trial. Front. Neurol. 2023, 14, 1256303. [Google Scholar] [CrossRef]
- Peng, Q.; Zhang, Y.; Yang, S.; Meng, B.; Chen, H.; Liu, X.; Zhao, W.; Hu, M.; Zhang, L.; Tao, Y. Morphologic changes of cervical musculature in relation to chronic nonspecific neck pain: A systematic review and meta-analysis. World Neurosurg. 2022, 168, 79–88. [Google Scholar] [CrossRef]
- Purushotham, S.; Stephenson, R.S.; Sanderson, A.; Abichandani, D.; Greig, C.; Gardner, A.; Falla, D. Microscopic changes in the spinal extensor musculature in people with chronic spinal pain: A systematic review. Spine J. 2022, 22, 1205–1221. [Google Scholar] [CrossRef]
- Fernández-de-las-Peñas, C.; Albert-Sanchís, J.C.; Buil, M.; Benitez, J.C.; Alburquerque-Sendín, F. Cross-sectional area of cervical multifidus muscle in females with chronic bilateral neck pain compared to controls. J. Orthop. Sports Phys. Ther. 2008, 38, 175–180. [Google Scholar] [CrossRef]
- De Loose, V.; Van den Oord, M.; Keser, I.; Burnotte, F.; Van Tiggelen, D.; Dumarey, A.; Cagnie, B.; Witvrouw, E.; Danneels, L. MRI study of the morphometry of the cervical musculature in F-16 pilots. Aviat. Space Environ. Med. 2009, 80, 727–731. [Google Scholar] [CrossRef]
- De Pauw, R.; Coppieters, I.; Kregel, J.; De Meulemeester, K.; Danneels, L.; Cagnie, B. Does muscle morphology change in chronic neck pain patients?—A systematic review. Man. Ther. 2016, 22, 42–49. [Google Scholar] [CrossRef] [PubMed]
- Javanshir, K.; Rezasoltani, A.; Mohseni-Bandpei, M.A.; Amiri, M.; Ortega-Santiago, R.; Fernández-de-Las-Peñas, C. Ultrasound assessment of bilateral longus colli muscles in subjects with chronic bilateral neck pain. Am. J. Phys. Med. Rehabil. 2011, 90, 293–301. [Google Scholar] [CrossRef]
- Thongton, J.; Sriburee, S.; Sremakaew, M.; Uthaikhup, S. Pain-side related difference in cross-sectional area of the longus colli muscle and its relationship with standing balance in persons with non-specific neck pain. Musculoskelet. Sci. Pract. 2022, 62, 102638. [Google Scholar] [CrossRef]
- Daly, E.; Prodoehl, J. Real time ultrasound imaging shows changes in deep neck flexor activation during exercise in individuals with mechanical neck pain. J. Back Musculoskelet. Rehabil. 2023, 37, 147–156. [Google Scholar] [CrossRef]
- Noormohammadpour, P.; Dehghani-Firouzabadi, A.; Mansournia, M.A.; Mohseni-Bandpei, M.A.; Moghaddam, N.; Miri, M.; Kordi, R. Comparison of the cross-sectional area of longus colli muscle between patients with cervical radicular pain and healthy controls. PM&R 2017, 9, 120–126. [Google Scholar]
- Amiri-Arimi, S.; Mohseni Bandpei, M.A.; Rezasoltani, A.; Javanshir, K.; Biglarian, A. Asymmetry of cervical multifidus and longus colli muscles size in participants with and without cervical radicular pain. J. Manip. Physiol. Ther. 2020, 43, 206–211. [Google Scholar] [CrossRef] [PubMed]
- Abaspour, O.; Javanshir, K.; Amiri, M.; Karimlou, M. Relationship between cross sectional area of longus colli muscle and pain laterality in patients with cervicogenic headache. J. Back Musculoskelet. Rehabil. 2015, 28, 393–399. [Google Scholar] [CrossRef] [PubMed]
- Wu, X.; Malhotra, A.; Geng, B.; Liu, R.; Abbed, K.; Forman, H.P.; Sanelli, P. Cost-effectiveness of Magnetic Resonance Imaging in cervical spine clearance of neurologically intact patients with blunt trauma. Ann. Emerg. Med. 2018, 71, 64–73. [Google Scholar] [CrossRef]
- Whittaker, J.L.; Ellis, R.; Hodges, P.W.; Osullivan, C.; Hides, J.; Fernandez-Carnero, S.; Arias-Buria, J.L.; Teyhen, D.S.; Stokes, M.J. Imaging with ultrasound in physical therapy: What is the PT’s scope of practice? A competency-based educational model and training recommendations. Br. J. Sports Med. 2019, 53, 1447–1453. [Google Scholar] [CrossRef] [PubMed]
- Paris, M.T.; Bell, K.E.; Avrutin, E.; Mourtzakis, M. Ultrasound image resolution influences analysis of skeletal muscle composition. Clin. Physiol. Funct. Imaging. 2020, 40, 277–283. [Google Scholar] [CrossRef]
- Palmer, T.B.; Akehi, K.; Thiele, R.M.; Smith, D.B.; Thompson, B.J. Reliability of panoramic ultrasound imaging in simultaneously examining muscle size and quality of the hamstring muscles in young, healthy males and females. Ultrasound Med. Biol. 2015, 41, 675–684. [Google Scholar] [CrossRef]
- Jenkins, N.D.; Miller, J.M.; Buckner, S.L.; Cochrane, K.C.; Bergstrom, H.C.; Hill, E.C.; Smith, C.M.; Housh, T.J.; Cramer, J.T. Test-Retest Reliability of Single Transverse versus Panoramic Ultrasound Imaging for Muscle Size and Echo Intensity of the Biceps Brachii. Ultrasound Med. Biol. 2015, 41, 1584–1591. [Google Scholar] [CrossRef]
- Abaspour, O.; Akbari, M. Relationship between echogenicity of deep cervical muscles and pain laterality in subjects suffering from cervicogenic headache. Cranio. 2023, 41, 446–453. [Google Scholar] [CrossRef]
- Akima, H.; Yoshiko, A.; Radaelli, R.; Ogawa, M.; Shimizu, K.; Tomita, A.; Maeda, H.; Neske, R.; Teodoro, J.; Maeda, K.; et al. Comparison of muscle quality and functional capacity between Japanese and Brazilian older individuals. PLoS ONE 2020, 15, e0243589. [Google Scholar] [CrossRef] [PubMed]
- Kwon, H.-J.; Kim, C.-S.; Kim, S.; Yoon, S.H.; Koh, J.; Kim, Y.K.; Choi, S.-S.; Shin, J.-W.; Kim, D.-H. Association between fatty infiltration in the cervical multifidus and treatment response following cervical interlaminar epidural steroid injection. Korean J. Pain 2023, 36, 358–368. [Google Scholar] [CrossRef]
- Passias, P.G.; Segreto, F.A.; Horn, S.R.; Lafage, V.; Lafage, R.; Smith, J.S.; Naessig, S.; Bortz, C.; Klineberg, E.O.; Diebo, B.G.; et al. Fatty infiltration of the cervical extensor musculature, cervical sagittal balance, and clinical outcomes: An analysis of operative adult cervical deformity patients. J. Clin. Neurosci. 2020, 72, 134–141. [Google Scholar] [CrossRef] [PubMed]
- Cuschieri, S. The STROBE guidelines. Saudi J. Anaesth. 2019, 13 (Suppl. S1), S31–S34. [Google Scholar] [CrossRef] [PubMed]
- Konarski, W.; Poboży, T.; Hordowicz, M.; Poboży, K.; Domańska, J. Current concepts of natural course and in management of frozen shoulder: A clinical overview. Orthop. Rev. 2021, 12, 8832. [Google Scholar] [CrossRef] [PubMed]
- Ernst, C.W.; Stadnik, T.W.; Peeters, E.; Breucq, C.; Osteaux, M.J. Prevalence of annular tears and disc herniations on MR images of the cervical spine in symptom free volunteers. Eur. J. Radiol. 2005, 55, 409–414. [Google Scholar] [CrossRef] [PubMed]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences; Lawrence Erlbaum Associates Inc.: Hillsdale, MI, USA, 1988; pp. 131–132. [Google Scholar]
- Rezasoltani, A.; Ahmadipoor, A.; Khademi-Kalantari, K.; Javanshir, K. The sign of unilateral neck semispinalis capitis muscle atrophy in patients with chronic non-specific neck pain. J. Back Musculoskelet. Rehabil. 2012, 25, 67–72. [Google Scholar] [CrossRef]
- Lee, J.P.; Tseng, W.Y.; Shau, Y.W.; Wang, C.L.; Wang, H.K.; Wang, S.F. Measurement of segmental cervical multifidus contraction by ultrasonography in asymptomatic adults. Man. Ther. 2007, 12, 286–294. [Google Scholar] [CrossRef]
- Amiri Arimi, S.; Mohseni Bandpei, M.A.; Rezasoltani, A.; Peolsson, A.; Mohammadi, M. Multifidus muscle size changes at different directions of head and neck movements in females with unilateral chronic non-specific neck pain and healthy subjects using ultrasonography. J. Bodyw. Mov. Ther. 2017, 22, 560–565. [Google Scholar] [CrossRef]
- Valera-Calero, J.A.; Gallego-Sendarrubias, G.M.; Fernández-de-las-Peñas, C.; Cleland, J.A.; Ortega-Santiago, R.; Arias-Buría, J.L. Panoramic ultrasound examination of posterior neck extensors in healthy subjects: Intra-examiner reliability study. Diagnostics 2020, 10, 740. [Google Scholar] [CrossRef]
- Cadore, E.L.; González-Izal, M.; Pallarés, J.G.; Rodriguez-Falces, J.; Häkkinen, K.; Kraemer, W.J.; Pinto, R.S.; Izquierdo, M. Muscle conduction velocity, strength, neural activity, and morphological changes after eccentric and concentric training. Scand. J. Med. Sci. Sports 2014, 24, e343–e352. [Google Scholar] [CrossRef] [PubMed]
- Young, I.A.; Dunning, J.; Butts, R.; Mourad, F.; Cleland, J.A. Reliability, construct validity, and responsiveness of the neck disability index and numeric pain rating scale in patients with mechanical neck pain without upper extremity symptoms. Physiother. Theory Pract. 2019, 35, 1328–1335. [Google Scholar] [CrossRef] [PubMed]
- Yu, Z.; Guindani, M.; Grieco, S.F.; Chen, L.; Holmes, T.C.; Xu, X. Beyond t test and ANOVA: Applications of mixed-effects models for more rigorous statistical analysis in neuroscience research. Neuron 2022, 110, 21–35. [Google Scholar] [CrossRef] [PubMed]
- Chan, Y.H. Biostatistics 104: Correlational analysis. Singap. Med. J. 2003, 44, 614–619. [Google Scholar]
- Yang, X.; Arts, M.P.; Bartels, R.H.M.A.; Vleggeert-Lankamp, C.L.A. The type of cervical disc herniation on MRI does not correlate to clinical outcomes. Bone Jt. J. 2022, 104-B, 1242–1248. [Google Scholar] [CrossRef] [PubMed]
- Costello, J.E.; Shah, L.M.; Peckham, M.E.; Hutchins, T.A.; Anzai, Y. Imaging appropriateness for neck pain. J. Am. Coll. Radiol. 2020, 17, 584–589. [Google Scholar] [CrossRef]
- Huang, Z.; Bai, Z.; Yan, J.; Zhang, Y.; Li, S.; Yuan, L.; Huang, D.; Ye, W. Association between muscle morphology changes, cervical spine degeneration, and clinical features in patients with chronic nonspecific neck pain: A magnetic resonance imaging analysis. World Neurosurg. 2022, 159, e273–e284. [Google Scholar] [CrossRef]
- Lee, T.H.; Kim, S.J.; Lim, S.M. Prevalence of disc degeneration in asymptomatic korean subjects. Part 2: Cervical spine. J. Korean Neurosurg. Soc. 2013, 53, 89–95. [Google Scholar] [CrossRef]
- Kim, J.H.; Sharan, A.; Cho, W.; Emam, M.; Hagen, M.; Kim, S.Y. The Prevalence of Asymptomatic Cervical and Lumbar Facet Arthropathy: A Computed Tomography Study. Asian Spine J. 2019, 13, 417–422. [Google Scholar] [CrossRef]
| Controls | Disc Bulging | Disc Protrusion | Disc Extrusion | p-Value | |
|---|---|---|---|---|---|
| Age(year) | 40.4 ± 9.7 | 48.5 ± 7.5 | 43.1 ± 8.0 | 43.9 ± 8.0 | 0.07 |
| BMI (kg/m2) | 26 ± 3.9 | 29.2 ± 6.4 | 26.7 ± 3.6 | 27.8 ± 4.8 | 0.29 |
| Sex (female/male) | 9/6 | 12/3 | 14/1 | 9/6 | 0.1 |
| Dominant side (Right/left) | 15/0 | 14/1 | 15/0 | 13/2 | 0.28 |
| Pain side (Left/Right) | - | 6/9 | 7/8 | 7/8 | 0.91 |
| NDI (0–100) † | - | 28.4 ± 7.6 | 33.9 ± 7.8 | 45.2 ± 12.1 | <0.001 |
| Pain duration (months) | - | 8.6 ± 4.5 | 10.7 ± 8.1 | 6.5 ± 3.3 | 0.14 |
| NPRS (0–10) † | - | 5.3 ± 1.2 | 5.9 ± 1.2 | 6.8 ± 1.1 | 0.003 |
| Group | Side | Cervical Multifidus | Longus Colli | ||||||
|---|---|---|---|---|---|---|---|---|---|
| APD | LD | CSA | MEI | APD | LD | CSA | MEI | ||
| Baseline Scores | |||||||||
| Disc Bulging | Non-symptomatic | 6.8 ± 1.0 | 23.4 ± 2.6 | 120.8 ± 21.6 | 60.9 ± 12.5 | 7.5 ± 1.1 | 12.5 ± 1.1 | 80.3 ± 8.4 | 79.7 ± 10.4 |
| Symptomatic | 6.5 ± 0.9 | 23.9 ± 2.3 | 117.7 ± 19.3 | 62.8 ± 14.1 | 7.5 ± 0.7 | 12.1 ± 1.4 | 78.9 ± 9.2 | 82.3 ± 11.9 | |
| Disc Protrusion | Non-symptomatic | 6.3 ± 0.4 | 23.5 ± 2.5 | 117.4 ± 15.2 | 65.5 ± 9.8 | 6.8 ± 0.5 | 12.1 ± 1.6 | 75.2 ± 8.3 | 72.3 ± 7.4 |
| Symptomatic | 6.1 ± 0.5 | 22.9 ± 2.4 | 107.0 ± 15.3 | 65.9 ± 12.2 | 6.5 ± 0.5 | 11.6 ± 0.9 | 68.6 ± 6.4 | 77.7 ± 6.0 | |
| Disc Extrusion | Non-symptomatic | 6.3 ± 0.8 | 22.5 ± 1.9 | 113.4 ± 14.9 | 63.7 ± 15.0 | 7.0 ± 0.8 | 11.7 ± 1.6 | 71.8 ± 8.7 | 85.2 ± 10.1 |
| Symptomatic | 5.8 ± 0.7 | 22.0 ± 1.7 | 109.4 ± 11.1 | 65.6 ± 12.3 | 6.5 ± 0.5 | 11.6 ± 0.9 | 68.6 ± 6.4 | 87.5 ± 12.4 | |
| Controls | Non-symptomatic (Right) | 6.6 ± 0.2 | 23.1 ± 0.5 | 120.5 ± 4.1 | 57.0 ± 1.9 | 7.5 ± 0.2 | 12.1 ± 0.4 | 80.3 ± 2.2 | 72.1 ± 2.4 |
| Non-symptomatic (Left) | 6.7 ± 0.2 | 23.3 ± 0.5 | 121.1 ± 4.2 | 56.5 ± 1.9 | 7.3 ± 0.2 | 12.2 ± 0.4 | 79.4 ± 2.2 | 72.4 ± 2.4 | |
| Differences Analysis | |||||||||
| Group | F | 4.408 | 2.441 | 1.215 | 9.292 | 8461 | 1.091 | 9.954 | 16.808 |
| p Value | 0.006 | 0.068 | 0.308 | <0.001 | <0.001 | 0.356 | <0.001 | <0.001 | |
| 0.108 | 0.063 | 0.032 | 0.204 | 0.189 | 0.029 | 0.215 | 0.316 | ||
| Side | F | 5.186 | 0.151 | 3.228 | 0.360 | 2.582 | 1.153 | 5.467 | 2.365 |
| p Value | 0.025 | 0.698 | 0.075 | 0.499 | 0.111 | 0.285 | 0.021 | 0.127 | |
| 0.045 | 0.001 | 0.029 | 0.003 | 0.023 | 0.010 | 0.048 | 0.021 | ||
| Group ×Side | F | 0.784 | 0.501 | 0.795 | 0.083 | 0.887 | 0.278 | 1.213 | 0.435 |
| p Value | 0.505 | 0.682 | 0.499 | 0.969 | 0.451 | 0.841 | 0.308 | 0.728 | |
| 0.021 | 0.014 | 0.021 | 0.002 | 0.024 | 0.008 | 0.032 | 0.012 | ||
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | |
|---|---|---|---|---|---|---|---|---|---|---|
| 1. Neck Disability Index | ||||||||||
| 2. Pain Intensity | 0.448 ** | |||||||||
| 3. Pain Duration | −0.366 ** | n.s. | ||||||||
| 4. Longus Colli—CSA | n.s. | n.s. | n.s. | |||||||
| 5. Longus Colli—APD | −0.386 ** | −0.237 * | n.s. | 0.530 ** | ||||||
| 6. Longus Colli—LD | n.s. | −0.225 * | n.s. | 0.548 ** | n.s. | |||||
| 7. Longus Colli—MEI | n.s. | n.s. | n.s. | −0.269 ** | n.s. | n.s. | ||||
| 8. Cervical Multifidus—CSA | n.s. | n.s. | n.s. | 0.355 ** | 0.418 ** | n.s. | n.s. | |||
| 9. Cervical Multifidus—APD | −0.217 * | n.s. | n.s. | 0.319 ** | 0.342 ** | n.s. | n.s. | 0.664 ** | ||
| 10. Cervical Multifidus—LD | −0.316 ** | n.s. | n.s. | 0.262 ** | 0.408 ** | n.s. | n.s. | 0.619 ** | n.s. | |
| 11. Cervical Multifidus—MEI | n.s. | n.s. | n.s. | n.s. | n.s. | n.s. | 0.326 ** | n.s. | n.s. | n.s. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Javanshir, K.; Ghafouri-Rouzbehani, P.; Zohrehvand, A.; Naeimi, A.; Fernández-de-las-Peñas, C.; Nikbakht, H.-A.; Mousavi-Khatir, S.R.; Valera-Calero, J.A. Cervical Multifidus and Longus Colli Ultrasound Differences among Patients with Cervical Disc Bulging, Protrusion and Extrusion and Asymptomatic Controls: A Cross-Sectional Study. J. Clin. Med. 2024, 13, 624. https://doi.org/10.3390/jcm13020624
Javanshir K, Ghafouri-Rouzbehani P, Zohrehvand A, Naeimi A, Fernández-de-las-Peñas C, Nikbakht H-A, Mousavi-Khatir SR, Valera-Calero JA. Cervical Multifidus and Longus Colli Ultrasound Differences among Patients with Cervical Disc Bulging, Protrusion and Extrusion and Asymptomatic Controls: A Cross-Sectional Study. Journal of Clinical Medicine. 2024; 13(2):624. https://doi.org/10.3390/jcm13020624
Chicago/Turabian StyleJavanshir, Khodabakhsh, Payam Ghafouri-Rouzbehani, Amirhossein Zohrehvand, Arvin Naeimi, César Fernández-de-las-Peñas, Hossein-Ali Nikbakht, Seyedeh Roghayeh Mousavi-Khatir, and Juan Antonio Valera-Calero. 2024. "Cervical Multifidus and Longus Colli Ultrasound Differences among Patients with Cervical Disc Bulging, Protrusion and Extrusion and Asymptomatic Controls: A Cross-Sectional Study" Journal of Clinical Medicine 13, no. 2: 624. https://doi.org/10.3390/jcm13020624
APA StyleJavanshir, K., Ghafouri-Rouzbehani, P., Zohrehvand, A., Naeimi, A., Fernández-de-las-Peñas, C., Nikbakht, H.-A., Mousavi-Khatir, S. R., & Valera-Calero, J. A. (2024). Cervical Multifidus and Longus Colli Ultrasound Differences among Patients with Cervical Disc Bulging, Protrusion and Extrusion and Asymptomatic Controls: A Cross-Sectional Study. Journal of Clinical Medicine, 13(2), 624. https://doi.org/10.3390/jcm13020624







