Ankle Taping Does Not Affect Running Kinematics During a Treadmill Protocol in Well-Trained Runners: A Secondary Analysis from a Randomized Cross-Over Controlled Trial
Abstract
1. Introduction
2. Materials and Methods
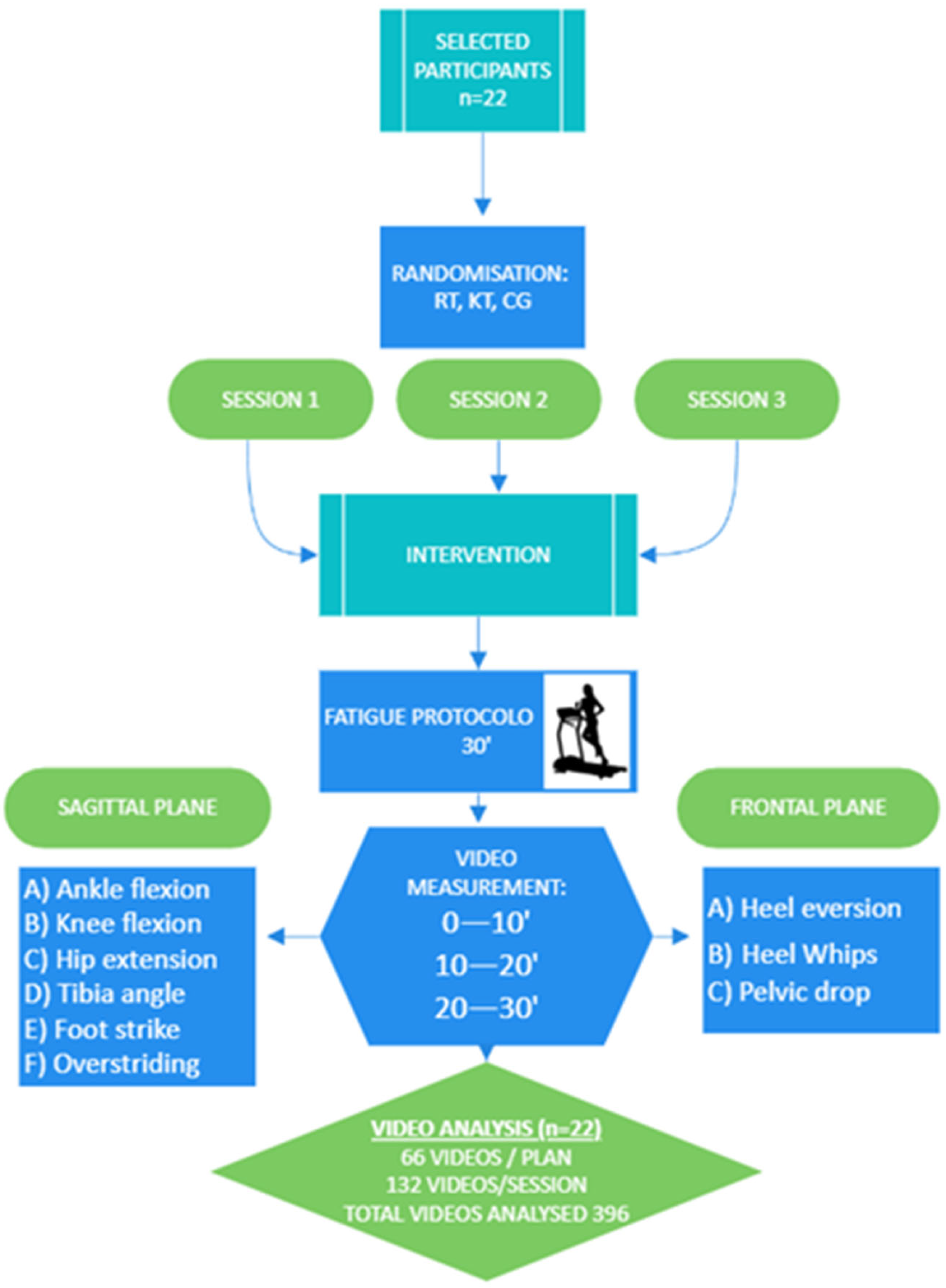
2.1. Study Design
2.2. Participants
2.3. Interventions
2.3.1. Running with KT Ankle Taping
2.3.2. Running with RT Ankle Taping
2.3.3. Control Group (CG)
2.4. Adverse Events
2.5. Fatigue Protocol
2.6. Data Collection
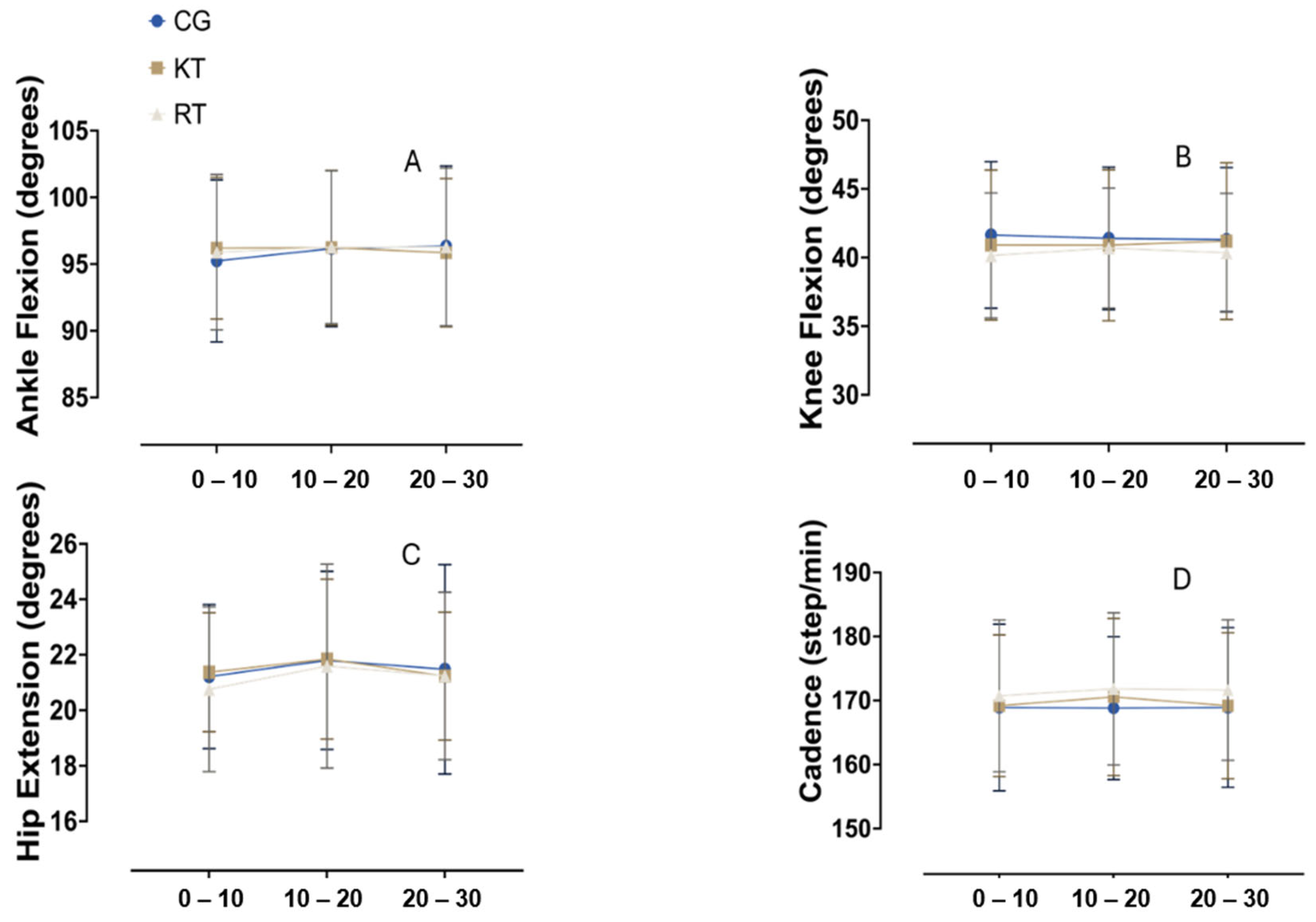
- Ankle dorsiflexion angle at initial contact: This angle was measured by drawing a line from the midpoint of the lateral malleolus to the head of the fifth metatarsal, and another line from the midpoint of the lateral malleolus to the lateral condyle of the tibia. The angle formed between these two lines at the moment of initial ground contact indicates the degree of ankle dorsiflexion.
- Maximum knee flexion angle during the stance phase: The knee flexion angle was assessed by drawing a line from the greater trochanter to the lateral epicondyle of the femur and another line from the lateral epicondyle to the lateral malleolus. The maximum angle formed between these two lines during the stance phase represents the peak knee flexion.
- Maximum hip extension angle during the late phase: The hip extension angle was measured by drawing one line vertically and another line from the greater trochanter to the lateral epicondyle of the femur. The maximum angle formed between these two lines, as the leg extends behind the body during the late phase of movement, indicates peak hip extension.
- Tibial angle during the stance phase: This angle was measured by drawing a line from the midpoint of the lateral malleolus to the lateral condyle of the tibia. The angle between this line and the vertical axis represents the tibial angle, which provides information on tibial inclination during the stance phase. The tibial angle was then classified as either extension or neutral.
- Foot strike pattern: Foot strike pattern was determined by evaluating the point of initial contact between the foot and the ground, using the relative position of the calcaneus and metatarsal heads. The initial contact was classified as heel strike, midfoot strike, or forefoot strike depending on which region of the foot made first contact with the ground.
- Overstriding: Overstriding in runners was assessed during the loading response phase by drawing a vertical line from the lateral malleolus to evaluate its alignment with the pelvis. Two categories were defined: overstriding, where the vertical line appeared anterior to the pelvis, and no overstriding, where the vertical line fell within the pelvis.
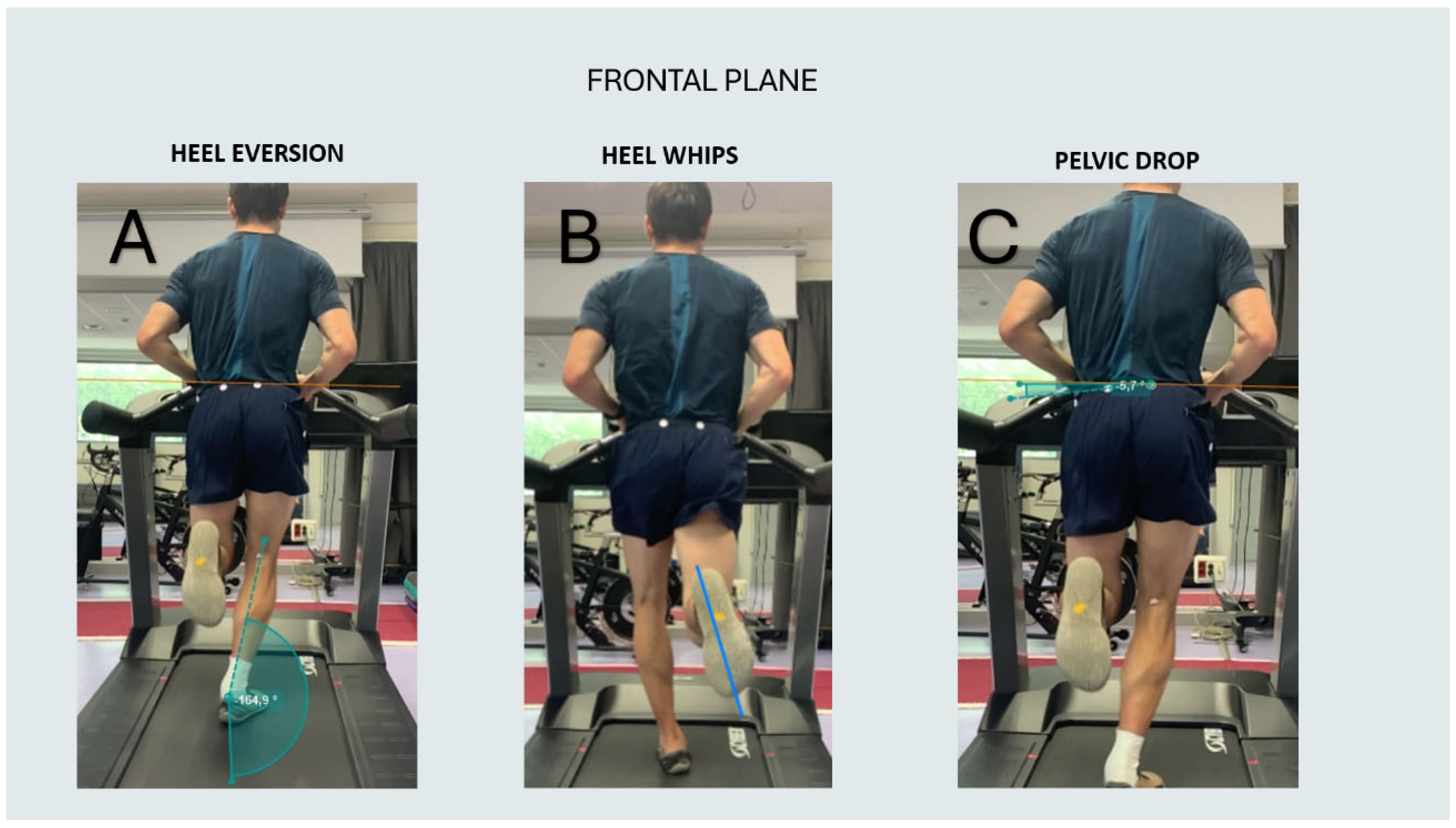
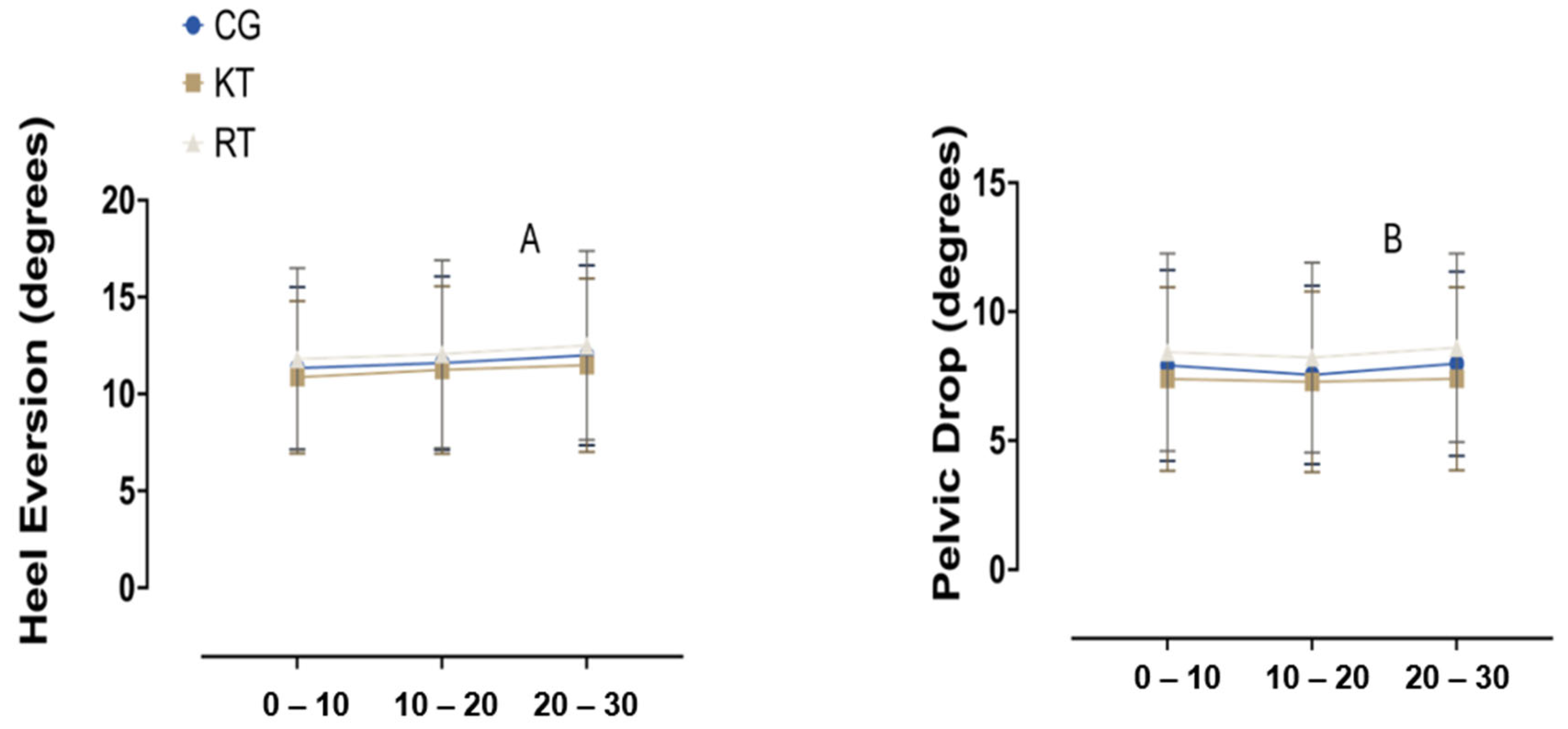
- Heel eversion was measured by identifying the mid-stance phase by placing markers at the top and bottom of the heel counter of the shoe. One line was drawn from the midpoint of the popliteal fossa to the top of the heel counter, and another line was drawn from the top to the bottom of the heel counter. The angle formed between these two lines represents the degree of heel eversion relative to the leg.
- Heel whips were assessed by tracking the rotation of the heel relative to the forefoot during the swing phase of the gait cycle. To measure this, a line was drawn from the midpoint of the calcaneus to the midpoint of the forefoot, and its displacement in the medial or lateral direction was recorded throughout the swing phase. Based on this analysis, runners were categorized into medial or lateral heel whips. Three groups were categorized based on medial deviation: less than 5 degrees, between 5 and 10 degrees, and greater than 10 degrees, as well as a lateral category of less than 5 degrees.
- Pelvic tilt was evaluated by marking the anterosuperior iliac spines (ASIS) on both sides of the pelvis and drawing a horizontal line between them. The angle between this reference line and the horizontal plane represents the degree of pelvic tilt.
2.7. Statistical Analysis
3. Results
3.1. Sagittal Plane
3.2. Frontal Plane
4. Discussion
4.1. Sagittal Plane
4.2. Frontal Plane
5. Clinical Implications, Limitations and Future Lines of Research
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Teixeira, R.N.; Lunardi, A.; da Silva, R.A.; Lopes, A.D.; Carvalho, C.R. Prevalence of musculoskeletal pain in marathon runners who compete at the elite level. Int. J. Sports Phys. Ther. 2016, 11, 126–131. [Google Scholar] [PubMed]
- Van Gent, R.N.; Siem, D.; Van Middelkoop, M.; Van Os, A.G.; Bierma-Zeinstra, S.M.A.; Koes, B.W. Incidence and determinants of lower extremity running injuries in long distance runners: A systematic review. Br. J. Sports Med. 2007, 41, 469–480. [Google Scholar] [CrossRef] [PubMed]
- Fong, D.T.P.; Hong, Y.; Chan, L.K.; Yung, P.S.H.; Chan, K.M. A systematic review on ankle injury and ankle sprain in sports. Sports Med. 2007, 37, 73–94. [Google Scholar] [CrossRef] [PubMed]
- Yin, Y.; Yu, Z.; Wang, J.; Sun, J. Effectiveness of the Rehabilitation Training Combined with Maitland Mobilization for the Treatment of Chronic Ankle Instability: A Randomized Controlled Trial. Int. J. Environ. Res. Public Health 2022, 19, 15328. [Google Scholar] [CrossRef]
- Gribble, P.A.; Bleakley, C.M.; Caulfield, B.M.; Docherty, C.L.; Fourchet, F.; Fong, D.T.P.; Hertel, J.; Hiller, C.E.; Kaminski, T.W.; McKeon, P.O.; et al. 2016 consensus statement of the International Ankle Consortium: Prevalence, impact and long-term consequences of lateral ankle sprains. Br. J. Sports Med. 2016, 50, 1493–1495. [Google Scholar] [CrossRef]
- Ghai, S.; Ghai, I.; Narciss, S. Influence of taping on joint proprioception: A systematic review with between and within group meta-analysis. BMC Musculoskelet. Disord. 2024, 25, 480. [Google Scholar] [CrossRef]
- Williams, S.A.; Ng, L.; Stephens, N.; Klem, N.; Wild, C. Effect of prophylactic ankle taping on ankle and knee biomechanics during basketball-specific tasks in females. Phys. Ther. Sport 2018, 32, 200–206. [Google Scholar] [CrossRef]
- Rao, Y.; Yang, N.; Gao, T.; Zhang, S.; Shi, H.; Lu, Y.; Ren, S.; Huang, H. Effects of peak ankle dorsiflexion angle on lower extremity biomechanics and pelvic motion during walking and jogging. Front. Neurol. 2023, 14, 1269061. [Google Scholar] [CrossRef]
- Backman, L.J.; Danielson, P. Low Range of Ankle Dorsiflexion Predisposes for Patellar Tendinopathy in Junior Elite Basketball Players: A 1-Year Prospective Study. Am. J. Sports Med. 2011, 39, 2626–2633. [Google Scholar] [CrossRef]
- Schiltz, M.; dric Lehance, C.; Maquet, D.; Bury, T.; Crielaard, J.M.; Croisier, J.L. Explosive Strength Imbalances in Professional Basketball Players. J. Ath. Train 2009, 44, 39–47. [Google Scholar] [CrossRef]
- Tudini, F.; Jordon, M.; Levine, D.; Healy, M.; Cathey, S.; Chui, K. Evaluating the effects of two different kinesiology taping techniques on shoulder range of motion and proprioception in patients with hypermobile Ehlers–Danlos syndrome: A randomized controlled trial. Front. Rehabil. Sci. 2024, 5, 1383551. [Google Scholar] [CrossRef] [PubMed]
- Heddon, S.; Saulnier, N.; Mercado, J.; Shalmiyev, M.; Berteau, J.P. Systematic review shows no strong evidence regarding the use of elastic taping for pain improvement in patients with primary knee osteoarthritis. Medicine 2021, 100, E25382. [Google Scholar] [CrossRef] [PubMed]
- Watcharakhueankhan, P.; Chapman, G.J.; Sinsurin, K.; Jaysrichai, T.; Richards, J. The immediate effects of Kinesio Taping on running biomechanics, muscle activity, and perceived changes in comfort, stability and running performance in healthy runners, and the implications to the management of Iliotibial band syndrome. Gait Posture 2022, 91, 179–185. [Google Scholar] [CrossRef] [PubMed]
- Halseth, T.; McChesney, J.W.; Debeliso, M.; Vaughn, R.; Lien, J. The effects of kinesio™ taping on proprioception at the ankle. J. Sci. Med. Sport 2004, 3, 1. [Google Scholar]
- Briem, K.; Eythörsdöttir, H.; Magnúsdóttir, R.G.; Pálmarsson, R.; Rúnarsdöttir, T.; Sveinsson, T. Effects of Kinesio Tape compared with nonelastic sports tape and the untaped ankle during a sudden inversion perturbation in male athletes. J. Orthop. Sports Phys. Ther. 2011, 41, 328–335. [Google Scholar] [CrossRef]
- Cordova, M.L.; Ingersoll, C.D.; Palmieri, R.M. Efficacy of Prophylactic Ankle Support: An Experimental Perspective. J. Athl. Train 2002, 37, 446–457. [Google Scholar]
- Fernández-González, P.; Koutsou, A.; Cuesta-Gómez, A.; Carratalá-Tejada, M.; Miangolarra-Page, J.C.; Molina-Rueda, F. Reliability of kinovea® software and agreement with a three-dimensional motion system for gait analysis in healthy subjects. Sensors 2020, 20, 3154. [Google Scholar] [CrossRef]
- Puig-Diví, A.; Escalona-Marfil, C.; Padullés-Riu, J.M.; Busquets, A.; Padullés-Chando, X.; Marcos-Ruiz, D. Validity and reliability of the Kinovea program in obtaining angles and distances using coordinates in 4 perspectives. PLoS ONE 2019, 14, e0216448. [Google Scholar] [CrossRef]
- Damsted, C.; Nielsen, R.O.; Larsen, L.H. Reliability of video-based quantification of the knee- and hip angle at foot strike during running. Int. J. Sports Phys. Ther. 2015, 10, 147–154. [Google Scholar]
- Sarvestan, J.; Ataabadi, P.A.; Svoboda, Z.; Kovačikova, Z.; Needle, A.R. The effect of ankle KinesioTM taping on ankle joint biomechanics during unilateral balance status among collegiate athletes with chronic ankle sprain. Phys. Ther. Sport 2020, 45, 161–167. [Google Scholar] [CrossRef]
- Romero-Morales, C.; Matilde-Cruz, A.; García-Arrabe, M.; Higes-Núñez, F.; Lópes, A.D.; Saiz, S.J.; Pareja-Galeano, H.; López-López, D. Assessing the effect of prophylactic ankle taping on ankle and knee biomechanics during landing tasks in healthy individuals: A cross-sectional observational study. Sao Paulo Med. J. 2024, 142, e2022548. [Google Scholar] [CrossRef] [PubMed]
- Slevin, Z.M.; Arnold, G.P.; Wang, W.; Abboud, R.J. Immediate effect of kinesiology tape on ankle stability. BMJ Open Sport Exerc. Med. 2020, 6, e000604. [Google Scholar] [CrossRef] [PubMed]
- García-Pérez, J.A.; Pérez-Soriano, P.; Llana Belloch, S.; Lucas-Cuevas, Á.G.; Sánchez-Zuriaga, D. Effects of treadmill running and fatigue on impact acceleration in distance running. Sports Biomech. 2014, 13, 259–266. [Google Scholar] [CrossRef] [PubMed]
- Souza, R.B. An Evidence-Based Videotaped Running Biomechanics Analysis. Phys. Med. Rehabil. Clin. N. Am. 2016, 27, 217–236. [Google Scholar] [CrossRef]
- Pipkin, A.; Kotecki, K.; Hetzel, S.; Heiderscheit, B. Reliability of a qualitative video analysis for running. J. Orthop. Sports Phys. Ther. 2016, 46, 556–561. [Google Scholar] [CrossRef]
- Atkins, L.T.; James, C.R.; Sizer, P.S.; Jonely, H.; Brismée, J.M. Reliability and concurrent criterion validity of a novel technique for analyzing hip kinematics during running. Physiother. Theory Pract. 2014, 30, 210–217. [Google Scholar] [CrossRef]
- Utku, B.; Bähr, G.; Knoke, H.; Mai, P.; Paganini, F.; Hipper, M.; Braun, L.; Denis, Y.; Helwig, J.; Willwacher, S. The effect of fresh and used ankle taping on lower limb biomechanics in sports specific movements. J. Sci. Med. Sport 2024, 27, 772–778. [Google Scholar] [CrossRef]
- Chinn, L.; Dicharry, J.; Hart, J.M.; Saliba, S.; Wilder, R.; Hertel, J. Gait kinematics after taping in participants with chronic ankle instability. J. Athl. Train 2014, 49, 322–330. [Google Scholar] [CrossRef]
- Kwon, Y.; Shin, G. Foot kinematics and leg muscle activation patterns are altered in those with limited ankle dorsiflexion range of motion during incline walking. Gait Posture 2022, 92, 315–320. [Google Scholar] [CrossRef]
- Almeida, M.O.; Davis, I.S.; Lopes, A.D. Biomechanical Differences of Foot-Strike Patterns During Running: A Systematic Review With Meta-analysis. J. Orthop. Sports Phys. Ther. 2015, 45, 738–755. [Google Scholar] [CrossRef]
- Moffit, T.J.; Montgomery, M.M.; Lockie, R.G.; Pamukoff, D.N. Association Between Knee- and Hip-Extensor Strength and Running-Related Injury Biomechanics in Collegiate Distance Runners. J. Athl. Train 2020, 55, 1262–1269. [Google Scholar] [CrossRef] [PubMed]
- Baker, L.M.; Yawar, A.; Lieberman, D.E.; Walsh, C.J. Predicting overstriding with wearable IMUs during treadmill and overground running. Sci. Rep. 2024, 14, 6347. [Google Scholar] [CrossRef] [PubMed]
- Rowe, P.L.; Bryant, A.L.; Egerton, T.; Paterson, K.L. External Ankle Support and Ankle Biomechanics in Chronic Ankle Instability: Systematic Review and Meta-Analysis. J. Athl. Train 2023, 58, 635–647. [Google Scholar] [CrossRef] [PubMed]
- Gregory, C.; Koldenhoven, R.M.; Higgins, M.; Hertel, J. External ankle supports alter running biomechanics: A field-based study using wearable sensors. Physiol. Meas. 2019, 40, 044003. [Google Scholar] [CrossRef]
- Deschamps, K.; Dingenen, B.; Pans, F.; Van Bavel, I.; Matricali, G.A.; Staes, F. Effect of taping on foot kinematics in persons with chronic ankle instability. J. Sci. Med. Sport 2016, 19, 541–546. [Google Scholar] [CrossRef]
- Koblbauer, I.F.; van Schooten, K.S.; Verhagen, E.A.; van Dieën, J.H. Kinematic changes during running-induced fatigue and relations with core endurance in novice runners. J. Sci. Med. Sport 2014, 17, 419–424. [Google Scholar] [CrossRef]
- Tsatalas, T.; Giakas, G.; Spyropoulos, G.; Sideris, V.; Lazaridis, S.; Kotzamanidis, C.; Koutedakis, Y. The effects of eccentric exercise-induced muscle damage on running kinematics at different speeds. J. Sports Sci. 2013, 31, 288–298. [Google Scholar] [CrossRef]
- Van Hooren, B.; Fuller, J.T.; Buckley, J.D.; Miller, J.R.; Sewell, K.; Rao, G.; Barton, C.; Bishop, C.; Willy, R.W. Is Motorized Treadmill Running Biomechanically Comparable to Overground Running? A Systematic Review and Meta-Analysis of Cross-Over Studies. Sports Med. 2020, 50, 785–813. [Google Scholar] [CrossRef]
- Biz, C.; Nicoletti, P.; Tomasin, M.; Bragazzi, N.L.; Di Rubbo, G.; Ruggieri, P. Is Kinesio Taping Effective for Sport Performance and Ankle Function of Athletes with Chronic Ankle Instability (CAI)? A Systematic Review and Meta-Analysis. Medicina 2022, 58, 620. [Google Scholar] [CrossRef]
- Cheraghi, M.; Boozari, S.; Svoboda, Z.; Kovačikova, Z.; Needle, A.R.; Sarvestan, J. Effects of ankle KinesioTM taping on jump biomechanics in collegiate athletes with chronic ankle instability. Sport Sci. Health 2022, 18, 839–846. [Google Scholar] [CrossRef]



| Interval (Minutes) | Group | Heel Whips (Frontal Plane) | Chi-Square (p-Value) | Tibia Angle (Sagital Plane) | Chi-Square (p-Value) | Foot Strike (Sagital Plane) | Chi-Square (p-Value) | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Medial (<5) | Medial 5–10 | Medial >10 | Lateral <5 | Extension | Neutral | Heel strike | Midfoot | Forefoot | |||||
| 0–10 | CG | 2 (9.1%) | 6 (27.3%) | 13 (59.1%) | 1 (4.5%) | χ2 = 2.591 (p = 0.858) | 19 (86.4%) | 3 (13.6%) | χ2 = 0.236 (p = 0.889) | 17 (77.3%) | 3 (13.6%) | 2 (9.1%) | χ2 = 0.668 (p = 0.953) |
| KT | 2 (9.1%) | 5 (22.7%) | 14 (63.6%) | 1 (4.5%) | 19 (86.4%) | 3 (13.6%) | 18 (81.8%) | 2 (9.1%) | 2 (9.1%) | ||||
| RT | 2 (9.1%) | 2 (9.1%) | 17 (77.3%) | 1 (4.5%) | 18 (81.8%) | 4 (18.2%) | 18 (81.8%) | 3 (13.6%) | 1 (4.5%) | ||||
| 10–20 | CG | 2 (9.1%) | 5 (22.7%) | 14 (63.6%) | 1 (4.5%) | χ2 = 1.415 (p = 0.965) | 19 (86.4%) | 3 (13.6%) | χ2 = 0.236 (p = 0.889) | 17 (77.3%) | 4 (18.2%) | 1 (4.5%) | χ2 = 1.220 (p = 0.875) |
| KT | 2 (9.1%) | 5 (22.7%) | 14 (63.6%) | 1 (4.5%) | 19 (86.4%) | 3 (13.6%) | 18 (81.8%) | 3 (13.6%) | 1 (4.5%) | ||||
| RT | 1 (4.5%) | 3 (13.6%) | 17 (77.3%) | 1 (4.5%) | 18 (81.8%) | 4 (18.2%) | 18 (81.8%) | 4 (18.2%) | 0 (0%) | ||||
| 20–30 | CG | 1 (4.5%) | 6 (27.3%) | 14 (63.6%) | 1 (4.5%) | 19 (86.4%) | 3 (13.6%) | χ2 = 0.236 (p = 0.889) | 18 (81.8%) | 3 (13.6%) | 1 (4.5%) | χ2 = 0.321 (p = 0.988) | |
| KT | 2 (9.1%) | 5 (22.7%) | 14 (63.6%) | 1 (4.5%) | χ2 = 1.900 (p = 0.929) | 19 (86.4%) | 3 (13.6%) | 19 (86.4%) | 2 (9.1%) | 1 (4.5%) | |||
| RT | 1 (4.5%) | 3 (13.6%) | 17 (77.3%) | 1 (4.5%) | 18 (81.8%) | 4 (18.2%) | 19 (86.4%) | 2 (9.1%) | 1 (4.5%) | ||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Salniccia, F.; López-Ruiz, J.; García-Pérez-de-Sevilla, G.; González-de-la-Flor, Á.; García-Arrabé, M. Ankle Taping Does Not Affect Running Kinematics During a Treadmill Protocol in Well-Trained Runners: A Secondary Analysis from a Randomized Cross-Over Controlled Trial. J. Clin. Med. 2024, 13, 6740. https://doi.org/10.3390/jcm13226740
Salniccia F, López-Ruiz J, García-Pérez-de-Sevilla G, González-de-la-Flor Á, García-Arrabé M. Ankle Taping Does Not Affect Running Kinematics During a Treadmill Protocol in Well-Trained Runners: A Secondary Analysis from a Randomized Cross-Over Controlled Trial. Journal of Clinical Medicine. 2024; 13(22):6740. https://doi.org/10.3390/jcm13226740
Chicago/Turabian StyleSalniccia, Federico, Javier López-Ruiz, Guillermo García-Pérez-de-Sevilla, Ángel González-de-la-Flor, and María García-Arrabé. 2024. "Ankle Taping Does Not Affect Running Kinematics During a Treadmill Protocol in Well-Trained Runners: A Secondary Analysis from a Randomized Cross-Over Controlled Trial" Journal of Clinical Medicine 13, no. 22: 6740. https://doi.org/10.3390/jcm13226740
APA StyleSalniccia, F., López-Ruiz, J., García-Pérez-de-Sevilla, G., González-de-la-Flor, Á., & García-Arrabé, M. (2024). Ankle Taping Does Not Affect Running Kinematics During a Treadmill Protocol in Well-Trained Runners: A Secondary Analysis from a Randomized Cross-Over Controlled Trial. Journal of Clinical Medicine, 13(22), 6740. https://doi.org/10.3390/jcm13226740







