Intraoperative Periprosthetic Fractures in Total Hip Arthroplasty: A 1.6-Million-Patient Analysis of Complications, Costs, and the Challenges in AI-Based Prediction
Abstract
:1. Introduction
Research Questions
2. Methods
2.1. Dataset Acquisition and Inclusion Criteria
2.2. Patient Identification and Exclusions
2.3. Statistical Analyses and Propensity Score Matching
2.4. Outcome Measures and Procedure Identification
2.5. Intraoperative Periprosthetic Fracture Prediction Models
2.6. Ethical Aspects
3. Results
3.1. Analysis of Comorbidities in Patients with and Without Intraoperative Periprosthetic Fractures
3.2. Propensity-Score-Matched Analysis
3.3. Comparison of Length of Stay and Total Charges Between Patients with and Without Intraoperative Periprosthetic Fracture in Propensity-Score-Matched Cohorts
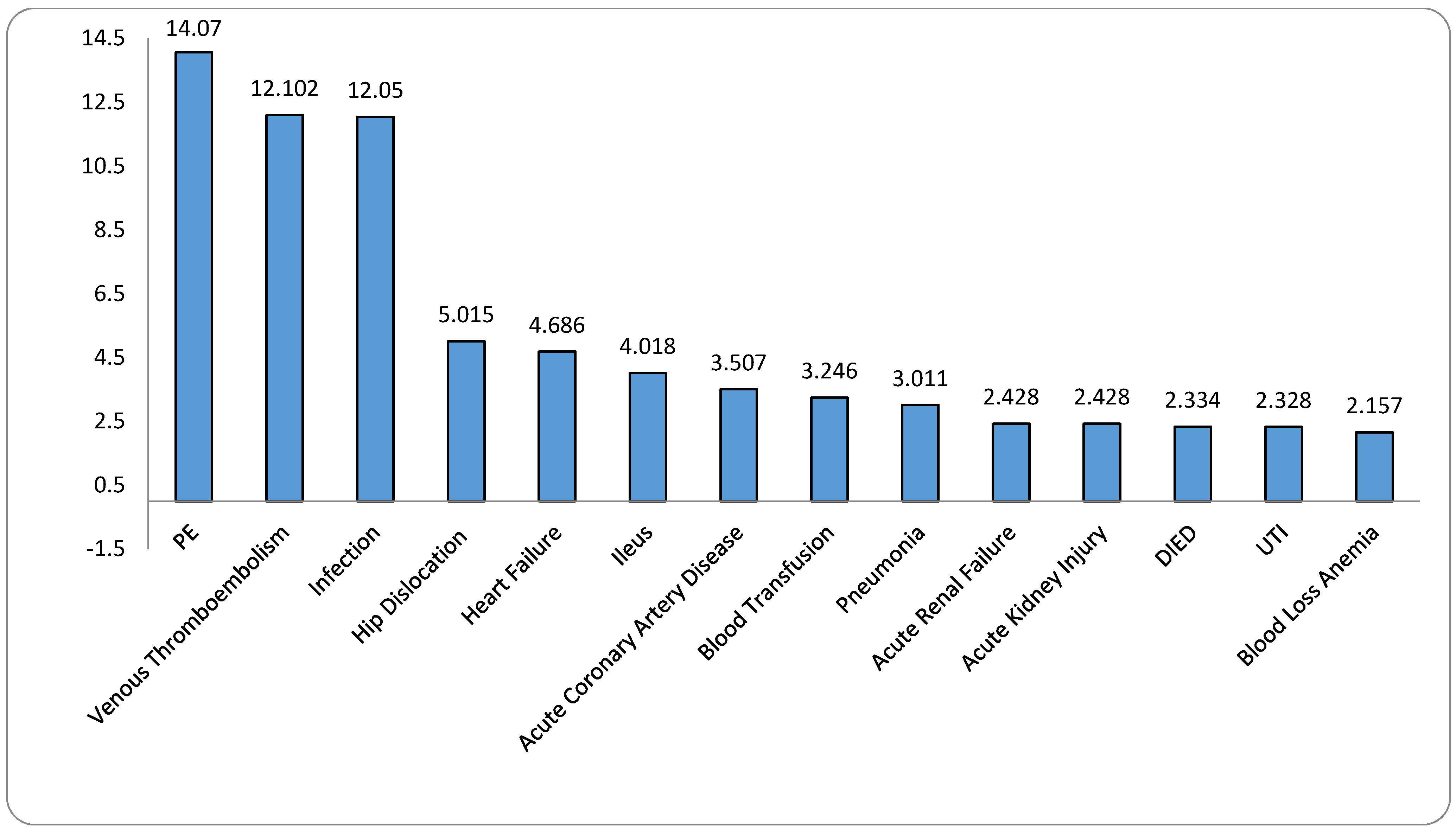
3.4. Odds Ratios of Complications in Patients with Intraoperative Periprosthetic Fractures Compared to Those Without Fractures
3.5. Intraoperative Periprosthetic Fracture Prediction Models
4. Discussion
- Main Findings
- Clinical Implications of Periprosthetic Fractures and Dislocations
- Economic Burden and Healthcare Resource Utilization
4.1. Challenges in Predicting Periprosthetic Fractures
4.2. Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| AUC | Area under the curve |
| HCUP | Healthcare Cost and Utilization Project |
| IBD | Inflammatory bowel disease |
| DNN | Deep neural network |
| ICD-10 | International Classification of Diseases, 10th Revision |
| LOS | Length of stay |
| NIS | Nationwide Inpatient Sample |
| SPSS | Statistical Package for the Social Sciences |
| THA | Total hip arthroplasty |
References
- Abdel, M.P.; Watts, C.D.; Houdek, M.T.; Lewallen, D.G.; Berry, D.J. Epidemiology of periprosthetic fracture of the femur in 32 644 primary total hip arthroplasties: A 40-year experience. Bone Jt. J. 2016, 98-B, 461–467. Available online: https://boneandjoint.org.uk/article/10.1302/0301-620X.98B4.37201 (accessed on 1 November 2024). [CrossRef] [PubMed]
- Falez, F.; Casella, F.; Zaccagno, S. Incidence of Postoperative Periprosthetic Femoral Fractures Using Short Stems in Total Hip Arthroplasty. Orthop. Proc. 2024, 106-B (Suppl. 16), 48. Available online: https://boneandjoint.org.uk/article/10.1302/1358-992X.2024.16.048 (accessed on 1 November 2024). [CrossRef]
- Akshay, G.; Krishnan, V.V.; Philip, S.; Tyler, Y.; Varatharaj, M.; Senthil, S. Ankylosing spondylitis substantially increases health-care costs and length of hospital stay following total hip arthroplasty—National in-patient database study. J. Clin. Orthop. Trauma 2023, 39, 102151. Available online: https://pmc.ncbi.nlm.nih.gov/articles/PMC10130334/ (accessed on 1 November 2024).
- Christian, H.; Sebastian, H.; Carsten, P. Management of Intraoperative Acetabular Fractures in Total Hip Arthroplasty: A Current Concept Review. Hip Pelvis 2024, 36, 179–186. Available online: https://pmc.ncbi.nlm.nih.gov/articles/PMC11380538/ (accessed on 1 November 2024).
- Masanobu, H.; Kazumasa, M.; Ryohei, T.; Tetsuya, T.; Atsushi, O.; Tetsuya, J. Periprosthetic fragility fracture of the femur after primary cementless total hip arthroplasty. Mod. Rheumatol. 2022, 32, 626–633. Available online: https://academic.oup.com/mr/article-abstract/32/3/626/6349345?redirectedFrom=fulltext&login=false (accessed on 1 November 2024).
- Kremers, H.M.; Abdel, M.P.; Ransom, J.E.; Larson, D.R.; Lewallen, D.G.; Berry, D.J. Mortality After Periprosthetic Femur Fractures During and After Primary and Revision Total Hip Arthroplasty. J. Am. Acad. Orthop. Surg. 2019, 27, 375–380. Available online: https://journals.lww.com/jaaos/abstract/2019/05150/mortality_after_periprosthetic_femur_fractures.7.aspx (accessed on 1 November 2024). [CrossRef]
- Lamb, J.N.; Matharu, G.S.; Redmond, A.; Judge, A.; West, R.M.; Pandit, H.G. Risk Factors for Intraoperative Periprosthetic Femoral Fractures During Primary Total Hip Arthroplasty. An Analysis from the National Joint Registry for England and Wales and the Isle of Man. J. Arthroplast. 2019, 34, 3065–3073.e1. Available online: https://www.arthroplastyjournal.org/article/S0883-5403(19)30653-9/abstract (accessed on 1 November 2024). [CrossRef]
- Lewis, S.R.; Macey, R.; Parker, M.J.; Cook, J.A.; Griffin, X.L. Arthroplasties for hip fracture in adults. Cochrane Database Syst. Rev. 2022, 2, CD013410. Available online: https://pmc.ncbi.nlm.nih.gov/articles/PMC8841979/ (accessed on 1 November 2024).
- Hans, L.; Göran, G.; Hans, R.; Peter, H.; Henrik, M. Three hundred and twenty-one periprosthetic femoral fractures. J. Bone Jt. Surg. Am. 2006, 88, 1215–1222. Available online: https://journals.lww.com/jbjsjournal/abstract/2006/06000/three_hundred_and_twenty_one_periprosthetic.7.aspx (accessed on 1 November 2024).
- Lindberg-Larsen, M.; Jørgensen, C.C.; Solgaard, S.; Kjersgaard, A.G.; Kehlet, H. Increased risk of intraoperative and early postoperative periprosthetic femoral fracture with uncemented stems. Acta Orthop. 2017, 88, 390–394. Available online: https://actaorthop.org/actao/article/view/9690 (accessed on 1 November 2024). [CrossRef]
- Bo, L.; Wenhui, M.; Huijie, L.; Tao, W.; Jia, H.; Han, Y. Incidence, Classification, and Risk Factors for Intraoperative Periprosthetic Femoral Fractures in Patients Undergoing Total Hip Arthroplasty with a Single Stem: A Retrospective Study. J. Arthroplasty 2019, 34, 1400–1411. Available online: https://www.arthroplastyjournal.org/article/S0883-5403(19)30254-2/abstract (accessed on 1 November 2024).
- Krishnan, V.V.; Surabhi, S.; Hunter, J.; Varatharaj, M.; Senthil, S. Patient disposition after discharge following primary total hip arthroplasty: Home versus skilled nursing facility-a study based on national inpatient sample database. Arch. Orthop. Trauma Surg. 2024, 144, 937–945. Available online: https://link.springer.com/article/10.1007/s00402-023-05081-9 (accessed on 1 November 2024).
- Matthew, S.; Ajay, P.; Sheth, N.P. Projected Volume of Primary Total Joint Arthroplasty in the U.S., 2014 to 2030. J. Bone Jt. Surg. Am. 2018, 100, 1455–1460. Available online: https://journals.lww.com/jbjsjournal/abstract/2018/09050/projected_volume_of_primary_total_joint.3.aspx (accessed on 1 November 2024).
- Stauffer, T.P.; Purcell, K.F.; Pean, C.; DeBaun, M.; Bolognesi, M.; Ryan, S.; Chun, D.; Seyler, T. Management of Intraoperative Acetabular Fractures During Total Hip Arthroplasty. Orthop. Clin. N. Am. 2024, 55, 9–17. Available online: https://www.sciencedirect.com/science/article/abs/pii/S0030589823001062?via%3Dihub (accessed on 1 November 2024). [CrossRef]
- Van Flandern, G.J. Periprosthetic fractures in total hip arthroplasty. Orthopedics 2005, 28 (Suppl. 9), s1089–s1095. Available online: https://journals.healio.com/doi/10.3928/0147-7447-20050902-18?url_ver=Z39.88-2003&rfr_id=ori:rid:crossref.org&rfr_dat=cr_pub%20%200pubmed (accessed on 1 November 2024). [CrossRef]
- Cai, S.; Liu, W.; Cai, X.; Xu, C.; Hu, Z.; Quan, X.; Deng, Y.; Yao, H.; Chen, B.; Li, W.; et al. Predicting osteoporotic fractures post-vertebroplasty: A machine learning approach with a web-based calculator. BMC Surg. 2024, 24, 142. Available online: https://pmc.ncbi.nlm.nih.gov/articles/PMC11080251/ (accessed on 1 November 2024). [CrossRef]
- Darin, D.; Jeffre, P.; Donald, G.; Duncan, C.P.; Masri, B.A. Intraoperative periprosthetic fractures during total hip arthroplasty. Evaluation and management. J. Bone Jt. Surg. Am. 2008, 90, 2000–2012. Available online: https://journals.lww.com/jbjsjournal/abstract/2008/09000/intraoperative_periprosthetic_fractures_during.25.aspx (accessed on 1 November 2024).
- Yi, D.; David, K.; Michael, W.; Mark, S.; Christopher, F.; Gary, H. Risk factors for periprosthetic femoral fractures around total hip arthroplasty: A systematic review and meta-analysis. ANZ J. Surg. 2020, 90, 441–447. Available online: https://onlinelibrary.wiley.com/doi/10.1111/ans.15473 (accessed on 1 November 2024).
- Davenport, D.; Hutt, J.R.; Mitchell, P.A.; Trompeter, A.; Kendoff, D.; Sandiford, N.A. Management of peri-prosthetic fractures around total hip arthroplasty: A contemporary review of surgical options. Ann. Jt. 2018, 3, 65. Available online: https://aoj.amegroups.org/article/view/4492/html (accessed on 1 November 2024). [CrossRef]
- Faizal, R.; Fares, H. Periprosthetic femoral fractures in total hip arthroplasty—A review. Hip Int. 2010, 20, 418–426. Available online: https://journals.sagepub.com/doi/10.1177/112070001002000402?url_ver=Z39.88-2003&rfr_id=ori:rid:crossref.org&rfr_dat=cr_pub%20%200pubmed (accessed on 1 November 2024).
- Nicola, M.; Elisa, T.; Andrea, F.; Roberta, G.; Martina, D.M.; Nicolò, N.; Giacomo, P.; Pietro, A.; Battista, C.G.; Stefano, G. Treatment Algorithm of Periprosthetic Femoral Fracturens. Geriatr. Orthop. Surg. Rehabil. 2022, 13, 21514593221097608. Available online: https://pmc.ncbi.nlm.nih.gov/articles/PMC9096211/ (accessed on 1 November 2024).
- Katherine, W.; Eustathios, K.; Mark, M.; Eleftherios, T.; Mehran, M. Periprosthetic fracture fixation of the femur following total hip arthroplasty: A review of biomechanical testing—Part II. Clin. Biomech. 2019, 61, 144–162. Available online: https://linkinghub.elsevier.com/retrieve/pii/S0268-0033(18)30733-2 (accessed on 1 November 2024).
- Ohly, N.E.; Whitehouse, M.R.; Duncan, C.P. Periprosthetic femoral fractures in total hip arthroplasty. Hip Int. 2014, 24, 556–567. Available online: https://journals.sagepub.com/doi/10.5301/hipint.5000155?url_ver=Z39.88-2003&rfr_id=ori:rid:crossref.org&rfr_dat=cr_pub%20%200pubmed (accessed on 1 November 2024). [CrossRef] [PubMed]
- Siddiqi, A.; Springer, B.D.; Chen, A.F.; Piuzzi, N.S. Diagnosis and Management of Intraoperative Fractures in Primary Total Hip Arthroplasty. J. Am. Acad. Orthop. Surg. 2021, 29, e497–e512. Available online: https://journals.lww.com/jaaos/abstract/2021/05150/diagnosis_and_management_of_intraoperative.6.aspx (accessed on 1 November 2024). [CrossRef] [PubMed]
- Siddiqi, A.; Tozzi, D.; Springer, B.D.; Rosen, A. Diagnosis and Management of Intraoperative Periprosthetic Fractures in Primary Total Knee Arthroplasty. J. Am. Acad. Orthop. Surg. 2023, 31, e760–e768. Available online: https://journals.lww.com/jaaos/abstract/2023/10010/diagnosis_and_management_of_intraoperative.5.aspx (accessed on 1 November 2024). [CrossRef]
- Mansukhani, S.A.; Agorastides, I.; Bose, D.; Sahni, H.; Bull, A.M.; Cobb, J.P. Machine learning models for predicting periprosthetic fractures: Early explorations. J. Orthop. Surg. Res. 2020, 15, 81. [Google Scholar]
- Watts, C.D.; Abdel, M.P.; Lewallen, D.G.; Berry, D.J.; Hanssen, A.D. Increased Risk of Periprosthetic Femur Fractures Associated With a Unique Cementless Stem Design. Clin. Orthop. Relat. Res. 2014, 473, 2045–2053. Available online: https://journals.lww.com/clinorthop/abstract/2015/06000/increased_risk_of_periprosthetic_femur_fractures.29.aspx (accessed on 1 November 2024). [CrossRef]
- Liu, B.; Liu, S.-K.; Wu, T.; Liu, Z.-M.; Chen, X.; Li, M.-N.; Li, H.-J.; Han, Y.-T. Risk Factors for Intraoperative Periprosthetic Femoral Fractures in Patients with Hip Dysplasia Undergoing Total Hip Arthroplasty with Uncemented Prostheses. Orthop. Surg. 2021, 13, 1870–1881. Available online: https://pmc.ncbi.nlm.nih.gov/articles/PMC8523755/ (accessed on 1 November 2024). [CrossRef]
- Liu, Y.; Li, C.; Cao, Z.; Wang, X.; Wen, J.; Ping, H.; Kong, X.; Chai, W. Undetected Intraoperative Periprosthetic Femoral Fractures in Patients Undergoing Primary Total Hip Arthroplasty: A Retrospective Case Series and Literature Review. Orthop. Surg. 2023, 15, 758–765. Available online: https://pmc.ncbi.nlm.nih.gov/articles/PMC9977600/ (accessed on 1 November 2024). [CrossRef]
- Yao, Z.-Y.; Fan, S.-Y.; Zhao, W.-Q.; Huang, J.-F. The History of Classification Systems for Periprosthetic Femoral Fractures: A Literature Review. Orthop. Surg. 2024, 16, 1816–1831. Available online: https://onlinelibrary.wiley.com/doi/10.1111/os.14149 (accessed on 1 November 2024). [CrossRef]
- Sarvilinna, R.; Huhtala, H.S.A.; Sovelius, R.T.; Halonen, P.J.; Nevalainen, J.K.; Pajamäki, K.J.K. Factors predisposing to periprosthetic fracture after hip arthroplasty: A case (n = 31)-control study. Acta Orthop. Scand. 2004, 75, 16–20. Available online: https://www.tandfonline.com/doi/abs/10.1080/00016470410001708030 (accessed on 1 November 2024). [CrossRef] [PubMed]
- Assil-Ramin, A.; Julie, S.P.; Jan, H.; Christian, R.; Timo, B.F.; Tim, R. Risk factors and prevention strategies for periprosthetic femoral fractures in hip arthroplasty. Orthopadie 2024. [Google Scholar] [CrossRef]
- Alsaleem, M.K.; Alalwan, H.A.; Alkhars, A.M.; Al Huwaiyshil, A.H.; Alamri, W.M. Intraoperative Periprosthetic Fractures in Total Hip Arthroplasty in Patients with Sickle Cell Disease at King Fahad Hospital Hofuf: A Cross-Sectional Study. Cureus 2020, 12, e11390. Available online: https://pmc.ncbi.nlm.nih.gov/articles/PMC7725205/ (accessed on 1 November 2024). [CrossRef]
- Heinrich, B.; Ingvild, D.; Kristin, B.-M.L.; Marie, F.A.; Geir, H.; Lars, F. Incidence and risk factors of intraoperative periprosthetic femoral fractures during primary total hip arthroplasty: 218,423 cases reported to the Norwegian Arthroplasty Register between 1987 and 2020. Acta Orthop. 2022, 93, 405–412. Available online: https://pmc.ncbi.nlm.nih.gov/articles/PMC8985217/ (accessed on 1 November 2024).
- Michele, F.; Nicolas, N.; Eric, L.; Peter, C. The Effect of Advancing Age on Total Joint Replacement Outcomes. Geriatr. Orthop. Surg. Rehabil. 2015, 6, 173–179. Available online: https://pmc.ncbi.nlm.nih.gov/articles/PMC4536505/ (accessed on 1 November 2024).
- Li, Z.; Zhao, W.; Lin, X.; Li, F. AI algorithms for accurate prediction of osteoporotic fractures in patients with diabetes: An up-to-date review. J. Orthop. Surg. Res. 2023, 18, 956. Available online: https://pmc.ncbi.nlm.nih.gov/articles/PMC10714483/ (accessed on 1 November 2024). [CrossRef]
- Maman, D.; Laver, L.; Becker, R.; Mahamid, A.; Berkovich, Y. Robotic-assisted total knee arthroplasty reduces postoperative complications and length of stay without increased cost compared to navigation-guided techniques: A national analysis. Knee Surg. Sports Traumatol. Arthrosc. 2024, 1–7. [Google Scholar] [CrossRef]
- David, M.; Lior, L.; Roland, B.; Ahmad, T.L.; Assil, M.; Binyamin, F.; Hadar, G.-O.; Yaniv, Y.; Yaron, B. Trends and epidemiology in robotic-assisted total knee arthroplasty: Reduced complications and shorter hospital stays. Knee Surg. Sports Traumatol. Arthrosc. 2024. [Google Scholar] [CrossRef]
- David, M.; Assil, M.; Binyamin, F.; Hadar, G.-O.; Linor, F.; Yaron, B.; Eyal, B. Comparative evaluation of postoperative outcomes and expenditure between robotic and conventional single-level lumbar fusion surgery: A comprehensive analysis of nationwide inpatient sample data. Eur. Spine J. 2024, 33, 2637–2645. Available online: https://link.springer.com/article/10.1007/s00586-024-08273-y (accessed on 1 November 2024).
- Maman, D.; Mahamid, A.; Yonai, Y.; Berkovich, Y. Comparing Complication Rates, Costs, and Length of Stay between Unicompartmental and Total Knee Arthroplasty: Insights from a Big Data Analysis Using the National Inpatient Sample Dataset. J. Clin. Med. 2024, 13, 3888. [Google Scholar] [CrossRef]
| Parameter | No Intraoperative Periprosthetic Fracture | Intraoperative Periprosthetic Fracture | Significance |
|---|---|---|---|
| Average age (y) | 65.5 | 66.8 | p < 0.0001 |
| Female (%) | 55.3% | 65.3% | p < 0.0001 |
| Primary expected payer—Medicare (%) | 54.6% | 60.9% | p < 0.001 |
| Primary expected payer—Medicaid (%) | 5.0% | 7.7% | p < 0.001 p < 0.001 |
| Primary expected payer—private, including HMO (%) | 37.2% | 28.2% | |
| Primary expected payer—self-pay (%) | 0.7% | 1.0% | |
| Primary expected payer—no charge (%) | 0.1% | 0.1% | |
| Primary expected payer—other (%) | 2.4% | 2.1% | |
| Location/teaching status of hospital (STRATA)—Rural (%) | 7.6% | 10.7% | |
| Location/teaching status of hospital (STRATA)—Urban nonteaching (%) | 24.8% | 22.7% | p < 0.001 |
| Location/teaching status of hospital (STRATA)—Urban teaching (%) | 67.6% | 66.6% |
| Parameter | No Intraoperative Periprosthetic Fracture | Intraoperative Periprosthetic Fracture | Significance |
|---|---|---|---|
| Hypertension | 52.1% | 54.1% | p < 0.001 |
| Dyslipidemia | 42.3% | 42.7% | p = 0.401 |
| Obstructive Sleep Apnea | 10.1% | 9.3% | p = 0.005 |
| Chronic Anemia | 5.7% | 7.9% | p < 0.001 |
| Alcohol Abuse | 1.5% | 2.5% | p < 0.001 |
| Osteoporosis | 4.6% | 8.8% | p < 0.001 |
| Type 2 Diabetes Mellitus | 14.9% | 17.0% | p < 0.001 |
| Chronic Kidney Disease | 6.4% | 8.9% | p < 0.001 |
| Congestive Heart Failure | 1.2% | 2.1% | p < 0.001 |
| Chronic Lung Disease | 6.6% | 10.2% | p < 0.001 |
| History of Myocardial Infarction | 3.4% | 4.4% | p < 0.001 |
| History of Cerebrovascular Accident | 3.8% | 5.5% | p < 0.001 |
| Dementia | 0.5% | 1.5% | p < 0.001 |
| Neoplasms | 1.4% | 1.5% | p = 0.123 |
| Neoplasms of Lymphoid and Hematopoietic Tissue | 0.6% | 0.5% | p = 0.152 |
| Peripheral Vascular Disease | 1.7% | 2.0% | p = 0.010 |
| BMI < 30 | 76.5% | 75.9% | p < 0.001 |
| Obesity | 11.2% | 10.3% | p < 0.001 |
| Morbid Obesity | 12.2% | 13.8% | p < 0.001 |
| Parameter | No Intraoperative Periprosthetic Fracture | Intraoperative Periprosthetic Fracture | Significance |
|---|---|---|---|
| Total Surgeries (Number) | 12,905 | 12,905 | |
| Average Age (Years) | 66.8 | 66.8 | p = 0.90 |
| Female (%) | 65.4 | 65.3 | p = 0.89 |
| Payer—Medicare (%) | 61.3 | 60.9 | p = 0.06 |
| Payer—Medicaid (%) | 7.5 | 7.7 | |
| Payer—Private (%) | 28.4 | 28.2 | |
| Payer—Self-pay (%) | 0.7 | 1.0 | |
| Payer—No charge(%) | 0.0 | 0.1 | |
| Payer—Other (including Self-pay) (%) | 2.1 | 2.1 | |
| Hypertension Diagnosis (%) | 54.2 | 54.1 | p = 0.80 |
| Dyslipidemia Diagnosis (%) | 43.1 | 42.7 | p = 0.53 |
| Sleep Apnea Diagnosis (%) | 9.5 | 9.3 | p = 0.59 |
| Chronic Anemia (%) | 7.3 | 7.9 | p = 0.08 |
| Alcohol Abuse (%) | 2.4 | 2.5 | p = 0.55 |
| Osteoporosis (%) | 8.9 | 8.8 | p = 0.83 |
| Type 2 Diabetes (%) | 17.2 | 17.0 | p = 0.68 |
| Renal Disease (%) | 8.8 | 8.9 | p = 0.66 |
| Chronic Heart Failure (%) | 2.1 | 2.1 | p = 0.65 |
| Chronic Lung Disease (%) | 10.3 | 10.2 | p = 0.68 |
| History of MI (%) | 4.2 | 4.4 | p = 0.07 |
| Peripheral Vascular Disease (%) | 2.1 | 2.0 | p = 0.51 |
| History of CVA (%) | 5.3 | 5.5 | p = 0.07 |
| Neoplasms (%) | 1.3 | 1.5 | p = 0.07 |
| Neoplasms (Lymphoid/Hematopoietic) (%) | 0.6 | 0.5 | p = 0.09 |
| BMI < 30 | 75.8 | 75.9 | p = 0.09 |
| Obesity | 10.5 | 10.3 | |
| Morbid Obesity | 13.7 | 13.8 |
| Parameter | No Intraoperative Periprosthetic Fracture | Intraoperative Periprosthetic Fracture | Significance |
|---|---|---|---|
| Length of stay mean in days | 2.5 (Std. deviation 1.7) | 3.8 (Std. deviation 6.0) | p < 0.0001 |
| Total charges mean in USD | 60,413 (Std. deviation 32,800) | 93,184 (Std. deviation 78,611) | p < 0.0001 |
| Metric | Logistic Regression (Periprosthetic Fracture) | Decision Tree (Periprosthetic Fracture) | Deep Neural Network (Periprosthetic Fracture) | Deep Neural Network (Blood Transfusions) |
|---|---|---|---|---|
| AUC (Test Set) | 0.60 | 0.50 | 0.60 | 0.820 |
| Calibration Intercept (Test Set) | −5.46 | −4.84 | −4.86 | −0.50 |
| Brier Score (Test Set) | 0.008 | 0.009 | 0.008 | 0.120 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Maman, D.; Steinfeld, Y.; Yonai, Y.; Fournier, L.; Bar, O.; Safir, O.; Berkovich, Y. Intraoperative Periprosthetic Fractures in Total Hip Arthroplasty: A 1.6-Million-Patient Analysis of Complications, Costs, and the Challenges in AI-Based Prediction. J. Clin. Med. 2024, 13, 6862. https://doi.org/10.3390/jcm13226862
Maman D, Steinfeld Y, Yonai Y, Fournier L, Bar O, Safir O, Berkovich Y. Intraoperative Periprosthetic Fractures in Total Hip Arthroplasty: A 1.6-Million-Patient Analysis of Complications, Costs, and the Challenges in AI-Based Prediction. Journal of Clinical Medicine. 2024; 13(22):6862. https://doi.org/10.3390/jcm13226862
Chicago/Turabian StyleMaman, David, Yaniv Steinfeld, Yaniv Yonai, Linor Fournier, Ofek Bar, Oleg Safir, and Yaron Berkovich. 2024. "Intraoperative Periprosthetic Fractures in Total Hip Arthroplasty: A 1.6-Million-Patient Analysis of Complications, Costs, and the Challenges in AI-Based Prediction" Journal of Clinical Medicine 13, no. 22: 6862. https://doi.org/10.3390/jcm13226862
APA StyleMaman, D., Steinfeld, Y., Yonai, Y., Fournier, L., Bar, O., Safir, O., & Berkovich, Y. (2024). Intraoperative Periprosthetic Fractures in Total Hip Arthroplasty: A 1.6-Million-Patient Analysis of Complications, Costs, and the Challenges in AI-Based Prediction. Journal of Clinical Medicine, 13(22), 6862. https://doi.org/10.3390/jcm13226862






