Proximal Fibula Resection for Tumors—Case Series and Technical Note
Abstract
1. Introduction
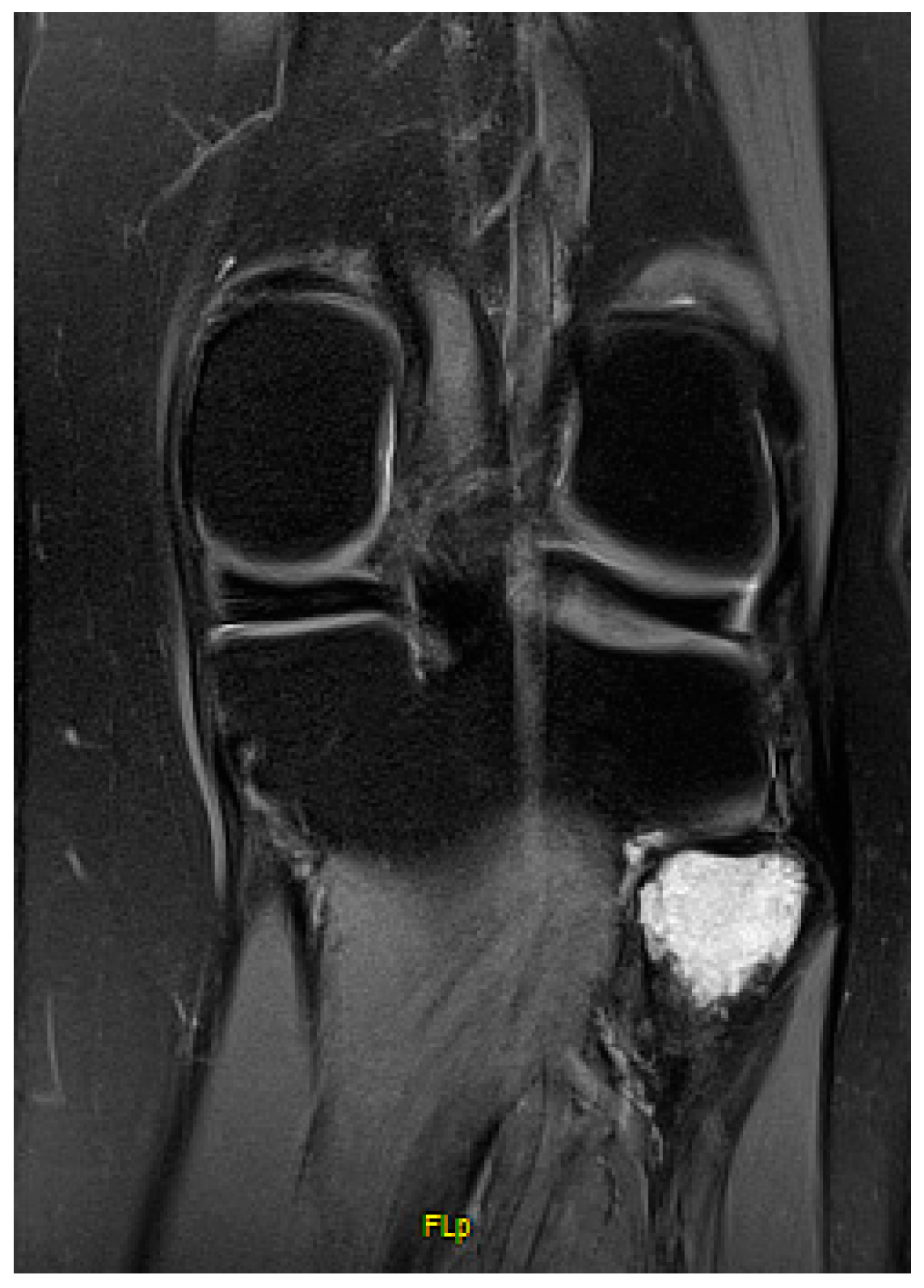
2. Methods
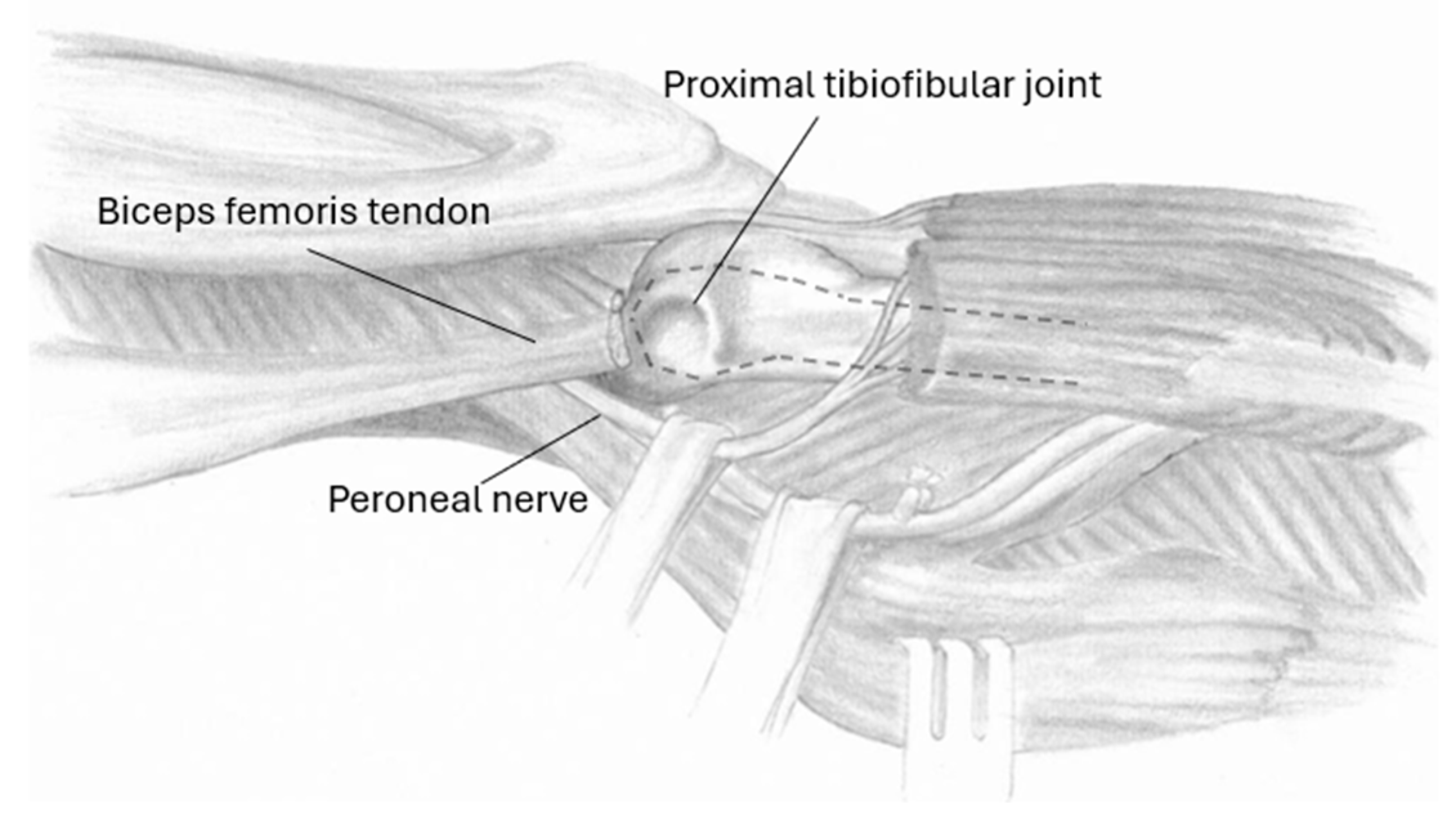
2.1. Surgical Technique
2.2. Clinical Evaluations
2.3. Stability Testing
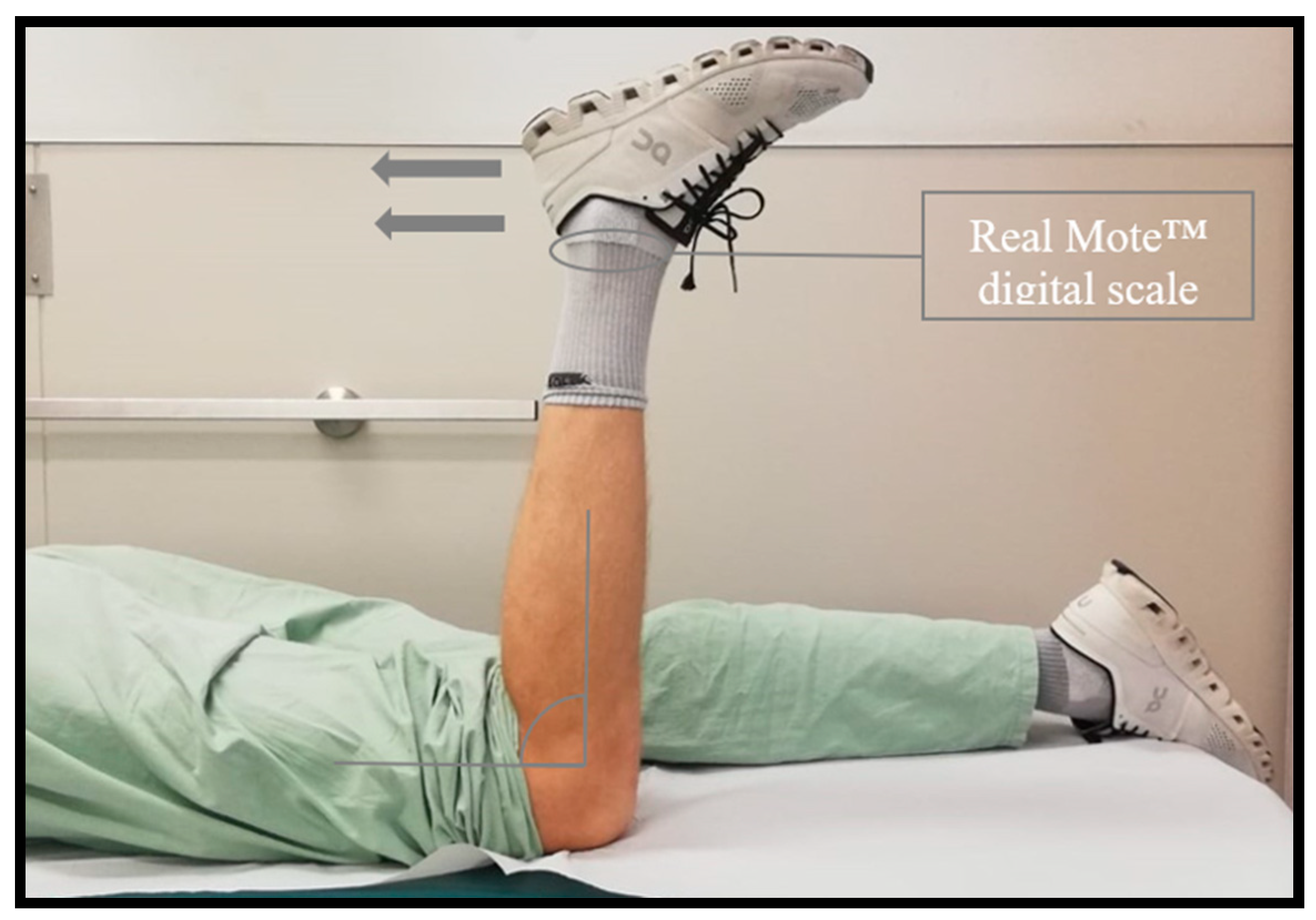
2.4. Flexion-Strength Testing
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
List of Abbreviations
| GCT | Giant cell tumors |
| ACT | Atypical cartilaginous tumors |
| PTFJ | Proximal tibiofibular joint |
| LCL | Lateral collateral ligament |
| BFT | Biceps femoris tendon |
| ROM | Range of motion |
| MSTS | Musculoskeletal Tumor Society Score |
References
- Dorfman, H.D.; Czerniak, B. Bone cancers. Cancer 1995, 75, 203–210. [Google Scholar] [CrossRef] [PubMed]
- Dahlin, D.C.; Unni, K.K. Dahlin’s bone tumors: General aspects and data on 11,087 cases. Am. J. Surg. Pathol. 1996, 20, 1298. [Google Scholar]
- Draganich, L.F.; Nicholas, R.W.; Shuster, J.K.; Sathy, M.R.; Chang, A.F.; Simon, M.A. The effects of resection of the proximal part of the fibula on stability of the knee and on gait. J. Bone Jt. Surg. Am. 1991, 73, 575–583. [Google Scholar] [CrossRef]
- Erler, K.; Demiralp, B.; Ozdemir, M.T.; Basbozkurt, M. Treatment of proximal fibular tumors with en bloc resection. Knee 2004, 11, 489–496. [Google Scholar] [CrossRef]
- Malawer, M.M. Surgical management of aggressive and malignant tumors of the proximal fibula. Clin. Orthop. Relat. Res. 1984, 186, 172–181. [Google Scholar] [CrossRef]
- Raines, B.T.; Pomajzl, R.J.; Ray, T.E.; Bley, J.A.; Sherman, S.L. Isolated Complete Rupture of the Biceps Femoris Insertion: A Surgical Repair Technique Manuscript. Arthrosc. Tech. 2019, 8, e407–e411. [Google Scholar] [CrossRef]
- Hsu, D.; Anand, P.; Mabrouk, A.; Chang, K.V. Biceps Tendon Rupture of the Lower Limb. In StatPearls [Internet]; StatPearls Publishing: Treasure Island, FL, USA, 2023. [Google Scholar]
- Grood, E.S.; Noyes, F.R.; Butler, D.L.; Suntay, W.J. Ligamentous and capsular restraints preventing straight medial and lateral laxity in intact human cadaver knees. J. Bone Jt. Surg. Am. 1981, 63, 1257–1269. [Google Scholar] [CrossRef]
- Draganich, L.F.; Vahey, J.W. An in vitro study of anterior cruciate ligament strain induced by quadriceps and hamstrings forces. J. Orthop. Res. 1990, 8, 57–63. [Google Scholar] [CrossRef]
- Bozkurt, M.; Yilmaz, E.; Atlihan, D.; Tekdemir, I.; Havitçioğlu, H.; Günal, I. The proximal tibiofibular joint: An anatomic study. Clin. Orthop. Relat. Res. 2003, 406, 136–140. [Google Scholar] [CrossRef]
- Charles, M.D.; Christian, D.R.; Cole, B.J. The Role of Biologic Therapy in Rotator Cuff Tears and Repairs. Curr. Rev. Musculoskelet. Med. 2018, 11, 150–161. [Google Scholar] [CrossRef]
- Hughston, J.C.; Andrews, J.R.; Cross, M.J.; Moschi, A. Classification of knee ligament instabilities. Part I. The medial compartment and cruciate ligaments. J. Bone Jt. Surg. Am. 1976, 58, 159–172. [Google Scholar] [CrossRef]
- Figueroa, F.; Figueroa, D.; Putnis, S.; Guiloff, R.; Caro, P.; Espregueira-Mendes, J. Posterolateral corner knee injuries: A narrative review. EFORT Open Rev. 2021, 6, 676–685. [Google Scholar] [CrossRef] [PubMed]
- Arikan, Y.; Misir, A.; Gur, V.; Kizkapan, T.B.; Dincel, Y.M.; Akman, Y.E. Clinical and radiologic outcomes following resection of primary proximal fibula tumors: Proximal fibula resection outcomes. J. Orthop. Surg. 2019, 27, 2309499019837411. [Google Scholar] [CrossRef] [PubMed]
- Huntley, K.; Al-Hardan, W.; Pretell-Mazzini, J. Surgical management of benign tumors of the proximal fibula. J. Am. Acad. Orthop. Surg. Glob. Res. Rev. 2021, 5, e21.00207. [Google Scholar] [CrossRef]
- Zhao, S.C.; Zhang, C.Q.; Zhang, C.L. Reconstruction of lateral knee joint stability following resection of proximal fibula tumors. Exp. Ther. Med. 2014, 7, 405–410. [Google Scholar] [CrossRef]
- Abdel, M.P.; Papagelopoulos, P.J.; Morrey, M.E.; Inwards, C.Y.; Wenger, D.E.; Rose, P.S.; Sim, F.H. Malignant proximal fibular tumors: Surgical management of 112 cases. J. Bone Jt. Surg. Am. 2012, 94, e165. [Google Scholar] [CrossRef]
- Bickels, J.; Kollender, Y.; Pritsch, T.; Meller, I.; Malawer, M.M. Knee stability after resection of the proximal fibula. Clin. Orthop. Relat. Res. 2007, 454, 198–201. [Google Scholar] [CrossRef]
- Dieckmann, R.; Gebert, C.; Streitbürger, A.; Henrichs, M.P.; Dirksen, U.; Rödl, R.; Gosheger, G.; Hardes, J. Proximal fibula resection in the treatment of bone tumours. Int. Orthop. 2011, 35, 1689–1694. [Google Scholar] [CrossRef] [PubMed]
- Pu, F.; Yu, Y.; Zhang, Z.; Liu, J.; Shao, Z.; Chen, F.; Feng, J. Clinical effect of surgical resection on primary malignant and invasive bone tumours of the proximal fibula. Mol. Clin. Oncol. 2023, 18, 27. [Google Scholar] [CrossRef] [PubMed]
- Fromm, J.; Klein, A.; Baur-Melnyk, A.; Knösel, T.; Lindner, L.; Birkenmaier, C.; Roeder, F.; Jansson, V.; Dürr, H.R. Survival and prognostic factors in conventional G1 chondrosarcoma. World J. Surg. Oncol. 2019, 17, 155. [Google Scholar] [CrossRef]
- Saiz, P.; Virkus, W.; Piasecki, P.; Templeton, A.; Shott, S.; Gitelis, S. Results of giant cell tumor of bone treated with intralesional excision. Clin. Orthop. Relat. Res. 2004, 424, 221–226. [Google Scholar] [CrossRef] [PubMed]
- Abdel, M.P.; Papagelopoulos, P.J.; Morrey, M.E.; Wenger, D.E.; Rose, P.S.; Sim, F.H. Surgical management of 121 benign proximal fibula tumors. Clin. Orthop. Relat. Res. 2010, 468, 3056–3062. [Google Scholar] [CrossRef] [PubMed]


| Case N° | Year of Birth | Age at OP (Years) | Gender | Diagnosis | Follow Up (Months) | MSTS Score (Points, /30) | Knee Flexion Power (Operated/Non Operated Limb, Percent) | Lateral Stability (Grade, Modified Hughston Classification) |
|---|---|---|---|---|---|---|---|---|
| 1 | 1972 | 48 | F | ACT | 23 | 29 | 5.3/6.3, 84.1% | 1 |
| 2 | 1997 | 22 | F | GCT | 29 | 30 | 9.1/8.8, 103.4% | 1 |
| 3 | 1993 | 27 | M | GCT | 14 | 21 | 10.1/12.2, 81.9% | 1 |
| 4 | 1983 | 37 | M | ACT | 16 | 30 | 8.1/9.9, 81.8% | 1 |
| 5 | 1978 | 42 | F | ACT | 19 | 29 | 11.8/12.3, 95.9% | 1 |
| 6 | 1961 | 59 | F | ACT | 14 | 28 | 2.8/2.9, 96.5% | 1 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hofer, R.; Valentini, M.; Smolle, M.A.; Leithner, A.; Bergovec, M. Proximal Fibula Resection for Tumors—Case Series and Technical Note. J. Clin. Med. 2024, 13, 7138. https://doi.org/10.3390/jcm13237138
Hofer R, Valentini M, Smolle MA, Leithner A, Bergovec M. Proximal Fibula Resection for Tumors—Case Series and Technical Note. Journal of Clinical Medicine. 2024; 13(23):7138. https://doi.org/10.3390/jcm13237138
Chicago/Turabian StyleHofer, Reinhard, Marisa Valentini, Maria Anna Smolle, Andreas Leithner, and Marko Bergovec. 2024. "Proximal Fibula Resection for Tumors—Case Series and Technical Note" Journal of Clinical Medicine 13, no. 23: 7138. https://doi.org/10.3390/jcm13237138
APA StyleHofer, R., Valentini, M., Smolle, M. A., Leithner, A., & Bergovec, M. (2024). Proximal Fibula Resection for Tumors—Case Series and Technical Note. Journal of Clinical Medicine, 13(23), 7138. https://doi.org/10.3390/jcm13237138





