Computerised Attention Functions Training Versus Computerised Executive Functions Training for Children with Attention Deficit/Hyperactivity Disorder: A Randomised Controlled Trial
Abstract
1. Introduction
1.1. Background
1.2. The Current Study
2. Materials and Methods
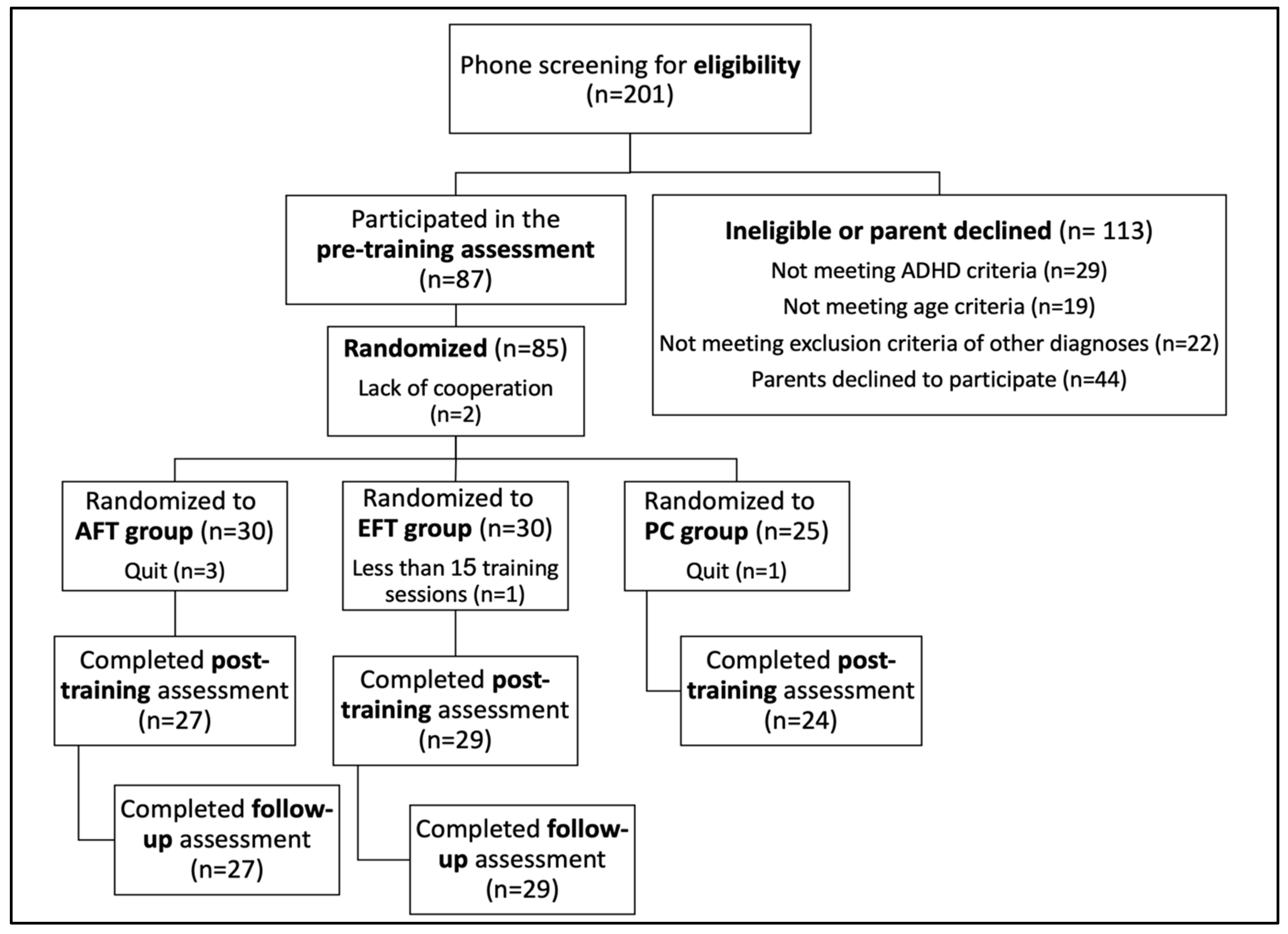
2.1. Participants
2.2. Assessment Tools
2.2.1. Continuous Performance Test (CPT)—Sustained Attention
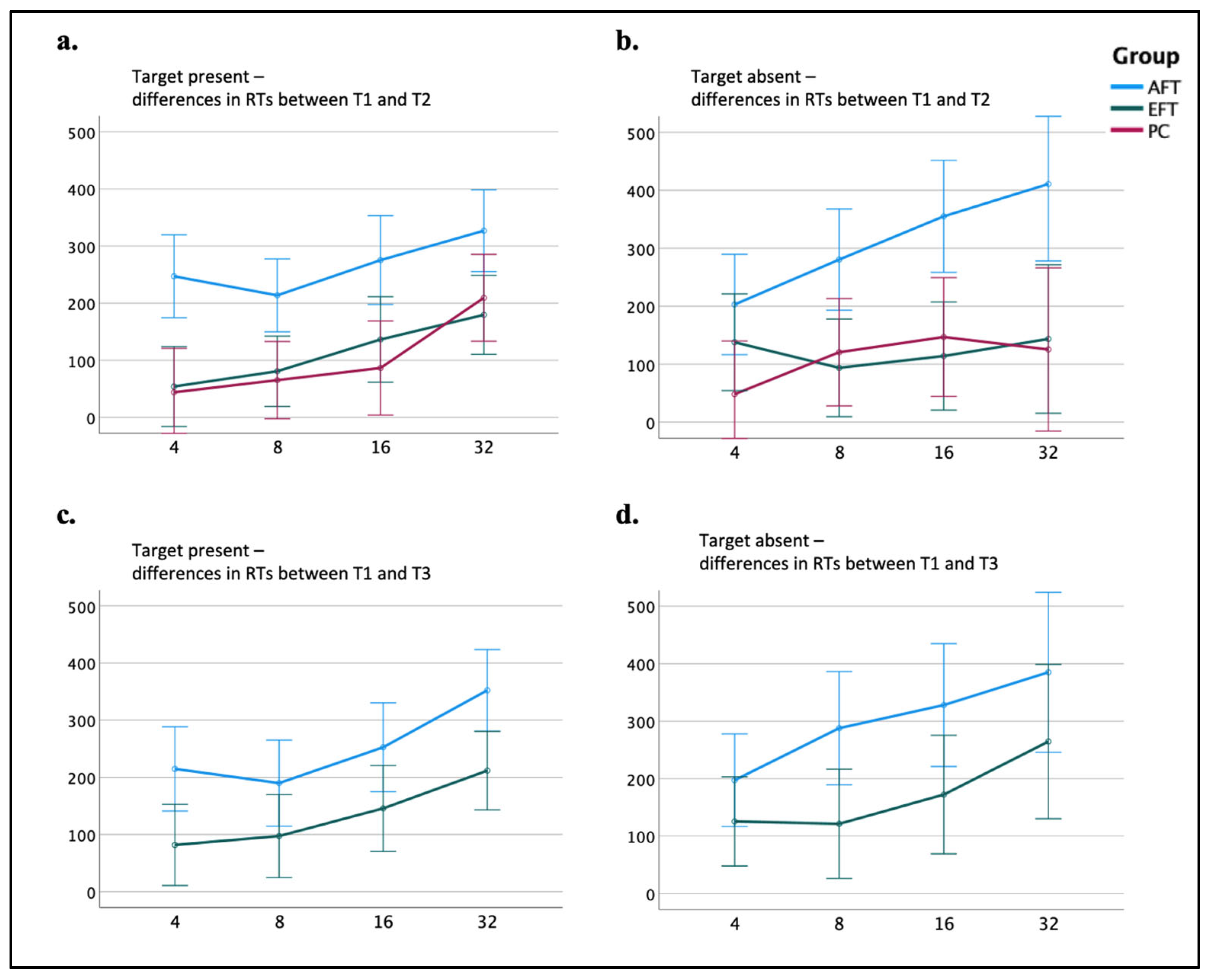
2.2.2. Conjunctive Visual Search Task (CVST)—Selective-Spatial Attention
2.2.3. Corsi Block-Tapping Task Forward—Visuospatial Working Memory Capacity
2.2.4. Corsi Block-Tapping Task Backward—Visuospatial Working Memory Capacity
2.2.5. Raven’s Colored Progressive Matrices (CPM) [84]—Nonverbal Abstract Reasoning
2.2.6. Arithmetic Evaluation—Basic Mathematical Operations
2.2.7. Child Behaviour Check List (CBCL)—Parent-Rated Behaviour
2.2.8. Behaviour Rating Inventory of Executive Functioning (BRIEF)—Parent-Rated Executive Function
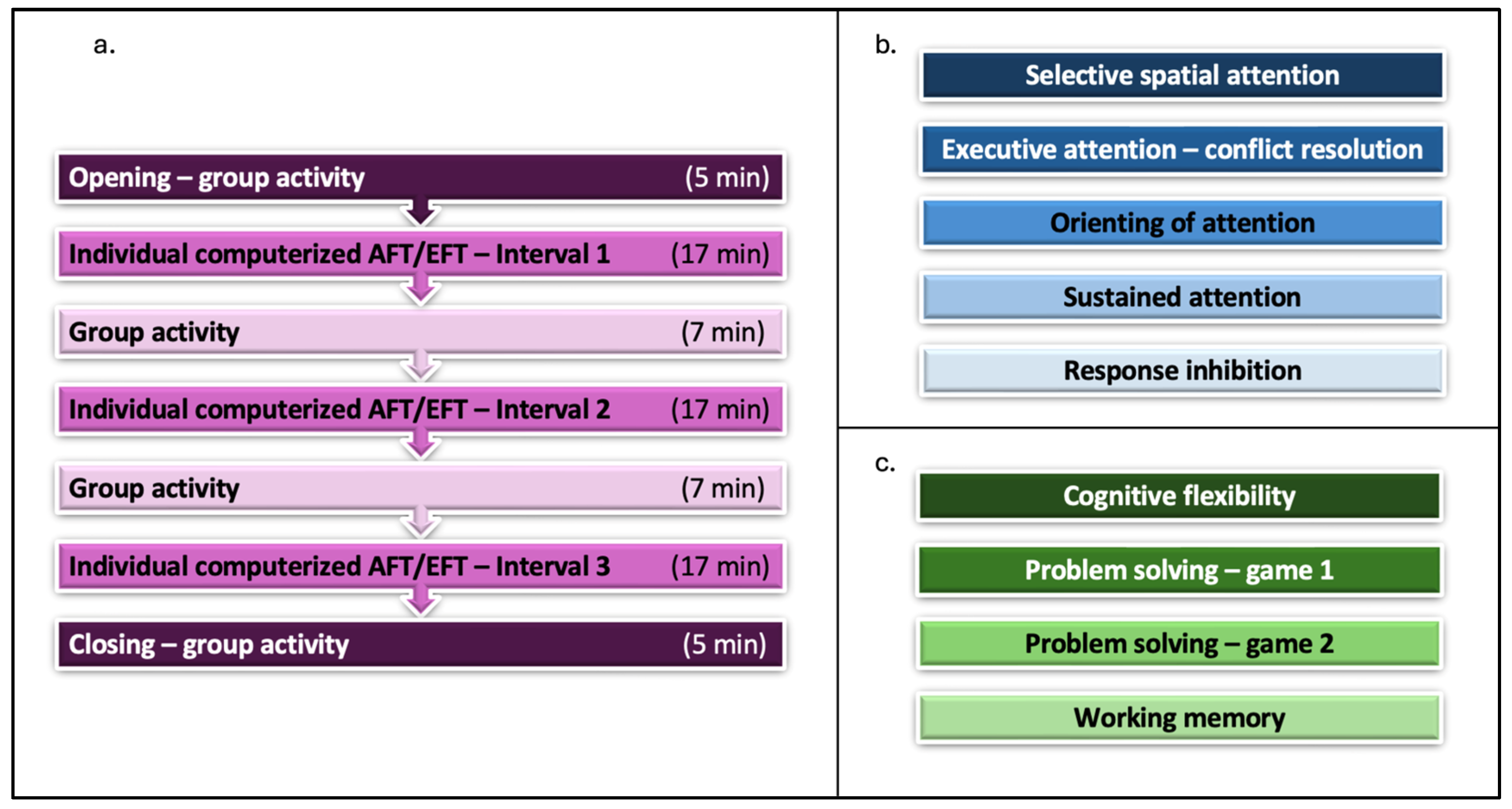
2.3. Procedure
2.4. Statistical Approach
2.4.1. Assessing the Effects of the Two Training Protocols
2.4.2. Gender, Age, and Medication Use
2.4.3. Missing Data
2.4.4. Data Trimming
3. Results
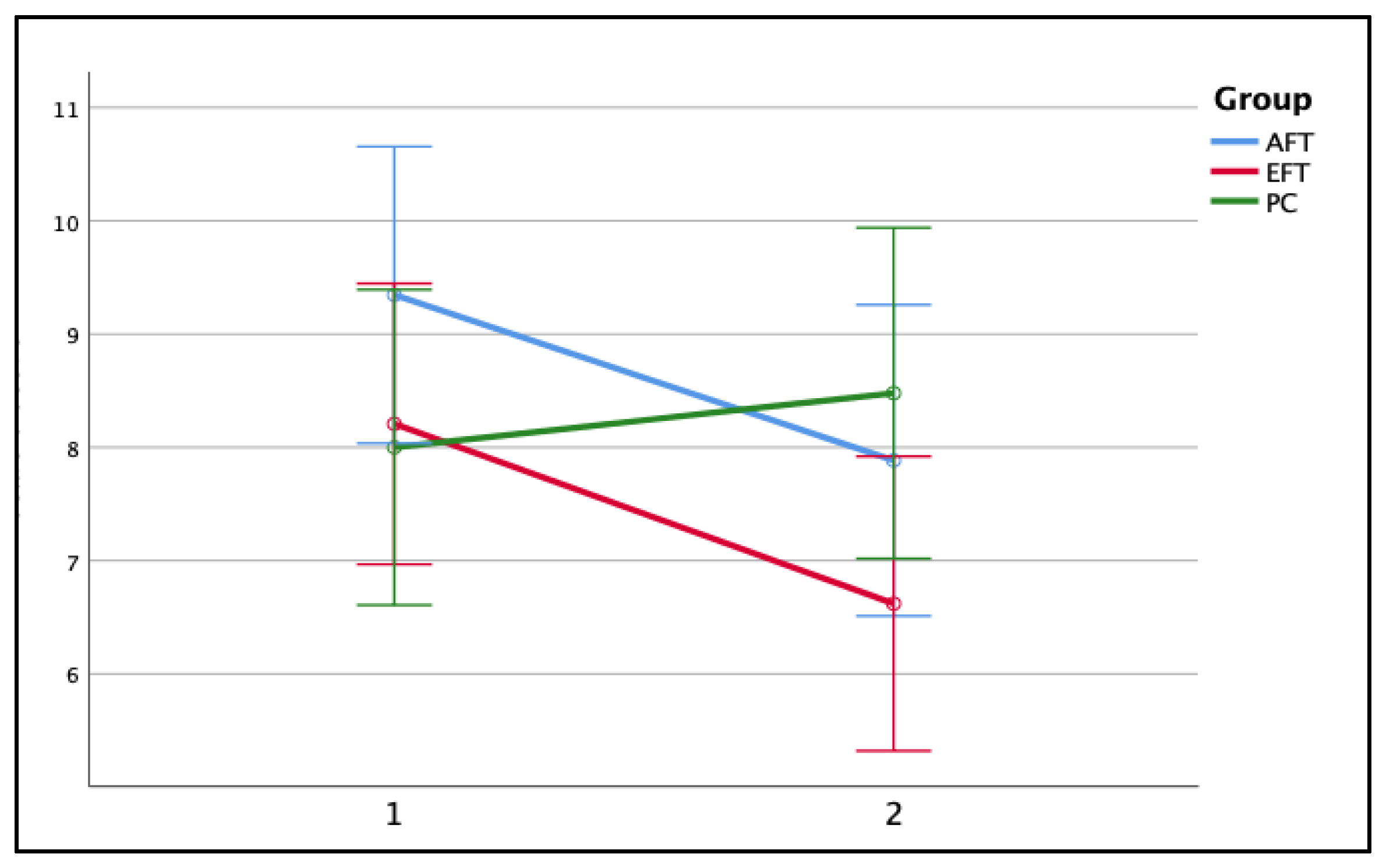
3.1. Training Effects on Objective Measures of Attention Functioning and Executive Functioning
3.2. Training Effects on Subjective Measures of Attention Functioning and Executive Functioning
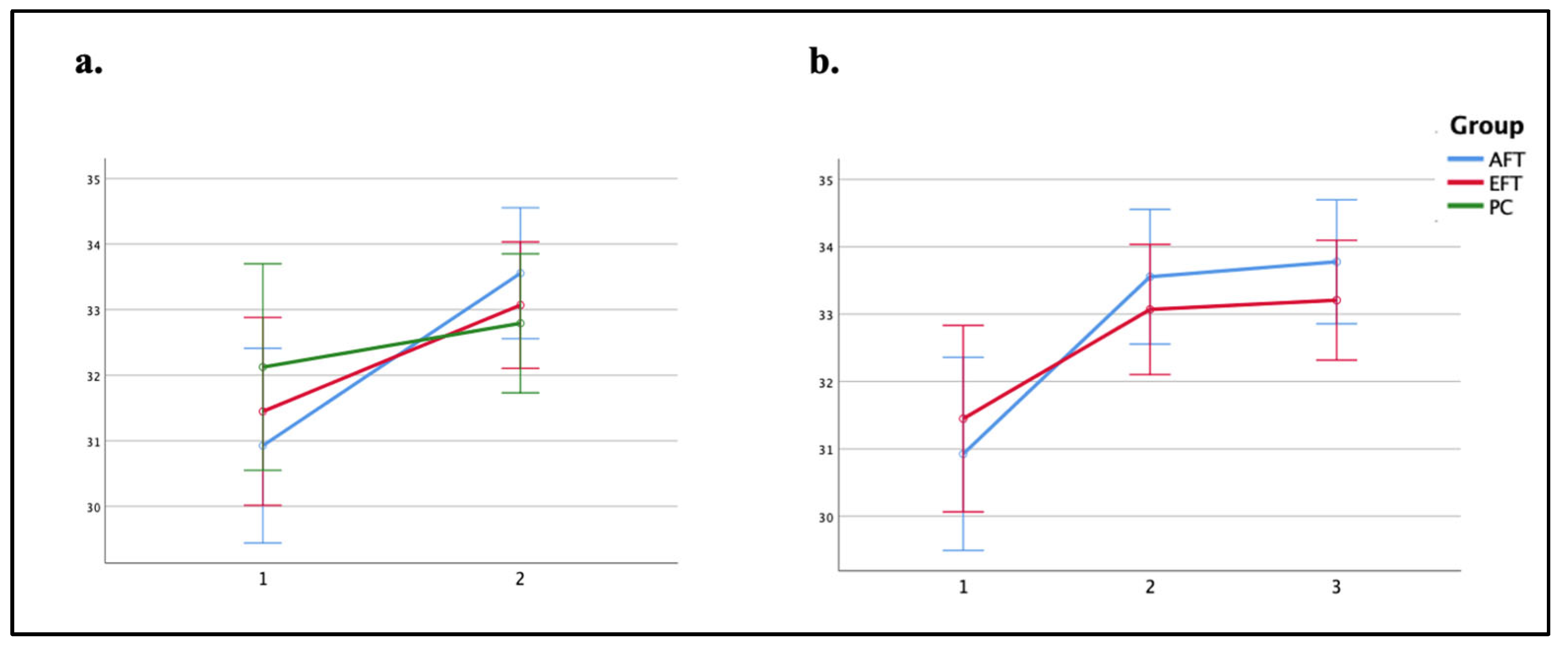
3.3. Training Effects on Arithmetic Performance
3.4. Summary of the Effects of the AFT and the EFT Protocols
4. Discussion
4.1. Limitations and Future Research
4.2. Implications
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
| Time | Target’s Presence | Set Size | Group | Average RTs (ms) | Accuracy Rates | n | ||
|---|---|---|---|---|---|---|---|---|
| M | SD | M | SD | |||||
| 1 | Target present | 4 | AFT | 956 | 188 | 0.974 | 0.035 | 27 |
| EFT | 933 | 191 | 0.969 | 0.049 | 29 | |||
| PC | 929 | 194 | 0.945 | 0.056 | 24 | |||
| 8 | AFT | 954 | 214 | 0.970 | 0.049 | 27 | ||
| EFT | 963 | 187 | 0.944 | 0.068 | 29 | |||
| PC | 958 | 185 | 0.973 | 0.033 | 24 | |||
| 16 | AFT | 1110 | 291 | 0.920 | 0.088 | 27 | ||
| EFT | 1108 | 257 | 0.922 | 0.075 | 29 | |||
| PC | 1086 | 230 | 0.935 | 0.072 | 24 | |||
| 32 | AFT | 1284 | 280 | 0.868 | 0.126 | 27 | ||
| EFT | 1261 | 266 | 0.886 | 0.093 | 29 | |||
| PC | 1286 | 274 | 0.842 | 0.102 | 24 | |||
| Target absent | 4 | AFT | 1068 | 248 | 0.985 | 0.027 | 27 | |
| EFT | 1129 | 267 | 0.961 | 0.056 | 29 | |||
| PC | 1087 | 244 | 0.971 | 0.046 | 24 | |||
| 8 | AFT | 1172 | 336 | 0.985 | 0.023 | 27 | ||
| EFT | 1149 | 269 | 0.976 | 0.047 | 29 | |||
| PC | 1141 | 249 | 0.969 | 0.060 | 24 | |||
| 16 | AFT | 1384 | 459 | 0.990 | 0.020 | 27 | ||
| EFT | 1312 | 291 | 0.982 | 0.034 | 29 | |||
| PC | 1267 | 307 | 0.959 | 0.066 | 24 | |||
| 32 | AFT | 1666 | 596 | 0.987 | 0.033 | 27 | ||
| EFT | 1646 | 425 | 0.984 | 0.028 | 29 | |||
| PC | 1548 | 422 | 0.974 | 0.035 | 24 | |||
| 2 | Target present | 4 | AFT | 709 | 188 | 0.972 | 0.052 | 27 |
| EFT | 879 | 263 | 0.959 | 0.047 | 29 | |||
| PC | 884 | 194 | 0.949 | 0.071 | 24 | |||
| 8 | AFT | 740 | 208 | 0.978 | 0.042 | 27 | ||
| EFT | 882 | 194 | 0.970 | 0.039 | 29 | |||
| PC | 893 | 191 | 0.964 | 0.045 | 24 | |||
| 16 | AFT | 834 | 214 | 0.937 | 0.055 | 27 | ||
| EFT | 972 | 205 | 0.938 | 0.061 | 29 | |||
| PC | 1000 | 198 | 0.939 | 0.051 | 24 | |||
| 32 | AFT | 957 | 247 | 0.894 | 0.089 | 27 | ||
| EFT | 1082 | 234 | 0.921 | 0.108 | 29 | |||
| PC | 1076 | 224 | 0.917 | 0.075 | 24 | |||
| Target absent | 4 | AFT | 865 | 275 | 0.964 | 0.048 | 27 | |
| EFT | 991 | 244 | 0.977 | 0.039 | 29 | |||
| PC | 1039 | 296 | 0.962 | 0.048 | 24 | |||
| 8 | AFT | 892 | 301 | 0.980 | 0.038 | 27 | ||
| EFT | 1055 | 323 | 0.988 | 0.029 | 29 | |||
| PC | 1020 | 197 | 0.968 | 0.050 | 24 | |||
| 16 | AFT | 1028 | 322 | 0.989 | 0.021 | 27 | ||
| EFT | 1198 | 265 | 0.977 | 0.032 | 29 | |||
| PC | 1120 | 242 | 0.973 | 0.059 | 24 | |||
| 32 | AFT | 1255 | 403 | 0.983 | 0.044 | 27 | ||
| EFT | 1503 | 433 | 0.977 | 0.039 | 29 | |||
| PC | 1422 | 454 | 0.967 | 0.053 | 24 | |||
| 3 | Displays with target | 4 | AFT | 741 | 208 | 0.961 | 0.042 | 27 |
| EFT | 851 | 213 | 0.967 | 0.036 | 29 | |||
| 8 | AFT | 764 | 224 | 0.976 | 0.045 | 27 | ||
| EFT | 866 | 232 | 0.973 | 0.033 | 29 | |||
| 16 | AFT | 857 | 225 | 0.950 | 0.060 | 27 | ||
| EFT | 963 | 279 | 0.926 | 0.059 | 29 | |||
| 32 | AFT | 933 | 226 | 0.928 | 0.092 | 27 | ||
| EFT | 1049 | 258 | 0.913 | 0.081 | 29 | |||
| Displays with no target | 4 | AFT | 871 | 256 | 0.961 | 0.047 | 27 | |
| EFT | 1004 | 254 | 0.980 | 0.038 | 29 | |||
| 8 | AFT | 885 | 243 | 0.983 | 0.034 | 27 | ||
| EFT | 1027 | 283 | 0.964 | 0.065 | 29 | |||
| 16 | AFT | 1056 | 360 | 0.983 | 0.039 | 27 | ||
| EFT | 1140 | 282 | 0.979 | 0.037 | 29 | |||
| 32 | AFT | 1281 | 405 | 0.985 | 0.036 | 27 | ||
| EFT | 1382 | 394 | 0.968 | 0.049 | 29 | |||
Appendix B
| Time | Group | Summary Scores of the Tasks | |||||
|---|---|---|---|---|---|---|---|
| Corsi Block-Tapping Task Forward | Corsi Block-Tapping Task Backward | ||||||
| M | SD | n | M | SD | n | ||
| 1 | AFT | 40.23 | 15.41 | 26 | 38.58 | 17.91 | 26 |
| EFT | 35.82 | 18.99 | 28 | 35.17 | 15.97 | 29 | |
| PC | 35.00 | 10.72 | 24 | 44.04 | 10.78 | 23 | |
| 2 | AFT | 44.69 | 16.60 | 26 | 38.50 | 16.08 | 26 |
| EFT | 41.43 | 20.43 | 28 | 39.14 | 14.37 | 29 | |
| PC | 40.58 | 16.89 | 24 | 38.35 | 14.56 | 23 | |
Appendix C
| Time | Group | Internalising Behaviour Score | Externalising Behaviour Score | Social Problems Score | n | |||
|---|---|---|---|---|---|---|---|---|
| M | SD | M | SD | M | SD | |||
| 1 | AFT | 11.92 | 8.35 | 9.04 | 6.80 | 4.73 | 3.70 | 26 |
| EFT | 9.72 | 7.05 | 10.00 | 7.27 | 4.14 | 3.71 | 29 | |
| PC | 10.26 | 6.75 | 12.52 | 10.04 | 5.57 | 4.13 | 23 | |
| 2 | AFT | 11.15 | 9.36 | 9.19 | 7.25 | 4.69 | 4.81 | 26 |
| EFT | 8.07 | 7.44 | 10.34 | 7.47 | 3.52 | 3.19 | 29 | |
| PC | 9.78 | 7.38 | 11.43 | 10.79 | 4.09 | 3.64 | 23 | |
| Scale | F | df | p | ηp2 |
|---|---|---|---|---|
| Internalising behaviour | 0.22 | 2.75 | 0.800 | 0.006 |
| Externalising behaviour | 0.43 | 2.75 | 0.650 | 0.011 |
| Social problems syndrome | 1.34 | 2.75 | 0.269 | 0.034 |
Appendix D
| Time | Group | Subscales’ Total Raw Scores | n | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Inhibit | Shift | Emotional Control | Initiate | Working Memory | Plan/Organise | Organisation of Materials | Monitor | |||||||||||
| M | SD | M | SD | M | SD | M | SD | M | SD | M | SD | M | SD | M | SD | |||
| 1 | AFT | 16.54 | 4.54 | 15.42 | 3.81 | 20.58 | 5.77 | 17.31 | 2.57 | 23.58 | 3.11 | 26.96 | 4.80 | 14.73 | 2.71 | 17.12 | 3.65 | 26 |
| EFT | 18.24 | 4.84 | 15.66 | 3.23 | 19.59 | 5.40 | 17.03 | 2.96 | 22.90 | 3.30 | 26.97 | 4.20 | 13.10 | 3.22 | 16.97 | 2.81 | 29 | |
| PC | 20.09 | 5.67 | 16.57 | 3.84 | 21.57 | 5.19 | 16.39 | 2.98 | 23.30 | 3.05 | 26.61 | 4.87 | 13.61 | 3.88 | 18.26 | 3.41 | 23 | |
| 2 | AFT | 15.88 | 4.29 | 14.15 | 3.80 | 17.46 | 5.19 | 16.31 | 3.02 | 22.15 | 3.34 | 26.50 | 4.92 | 14.12 | 2.72 | 15.38 | 3.49 | 26 |
| EFT | 16.76 | 4.45 | 14.03 | 2.97 | 16.52 | 4.63 | 15.66 | 3.36 | 20.86 | 3.74 | 25.76 | 4.90 | 12.48 | 3.33 | 15.79 | 3.02 | 29 | |
| PC | 18.78 | 5.59 | 14.96 | 4.12 | 18.61 | 5.57 | 15.96 | 3.56 | 21.96 | 4.38 | 25.61 | 5.31 | 12.96 | 3.17 | 16.74 | 3.91 | 23 | |
Appendix E
| Time | Group | Arithmetic’s Task Duration (ms) | Arithmetic’s Accuracy (%) | n | ||
|---|---|---|---|---|---|---|
| M | SD | M | SD | |||
| 1 | AFT | 528 | 284 | 84.62 | 18.86 | 26 |
| EFT | 569 | 254 | 81.61 | 18.93 | 28 | |
| PC | 505 | 280 | 88.23 | 15.66 | 24 | |
| 2 | AFT | 440 | 243 | 88.56 | 16.99 | 26 |
| EFT | 554 | 289 | 84.38 | 14.62 | 28 | |
| PC | 419 | 265 | 90.10 | 13.40 | 24 | |
| 3 | AFT | 477 | 275 | 86.73 | 19.54 | 26 |
| EFT | 516 | 271 | 78.57 | 21.93 | 28 | |
References
- Chacko, A.; Kofler, M.; Jarrett, M. Improving Outcomes for Youth with ADHD: A Conceptual Framework for Combined Neurocognitive and Skill-Based Treatment Approaches. Clin. Child Fam. Psychol. Rev. 2014, 17, 368–384. [Google Scholar] [CrossRef] [PubMed]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition, Text Revision; American Psychiatric Association: Washington, DC, USA, 2022. [Google Scholar]
- Pliszka, S.; AACAP Work Group on Quality Issues. Practice Parameter for the Assessment and Treatment of Children and Adolescents with Attention-Deficit/Hyperactivity Disorder. J. Am. Acad. Child Adolesc. Psychiatry 2007, 46, 894–921. [Google Scholar] [CrossRef] [PubMed]
- Raggi, V.L.; Chronis, A.M. Interventions to Address the Academic Impairment of Children and Adolescents with ADHD. J. Clin. Child Fam. Psychol. 2006, 9, 85–111. [Google Scholar] [CrossRef] [PubMed]
- The MTA Cooperative Group. A 14-Month Randomized Clinical Trial of Treatment Strategies for Attention-Deficit/Hyperactivity Disorder. Arch. Gen. Psychiatry 1999, 56, 1073–1086. [Google Scholar] [CrossRef] [PubMed]
- Van der Oord, S.; Prins, P.J.M.; Oosterlaan, J.; Emmelkamp, P.M.G. Efficacy of Methylphenidate, Psychosocial Treatments and Their Combination in School-Aged Children with ADHD: A Meta-Analysis. Clin. Psychol. Rev. 2008, 28, 783–800. [Google Scholar] [CrossRef]
- Hinshaw, S.P.; Arnold, L.E.; MTA Cooperative Group. Attention-Deficit Hyperactivity Disorder, Multimodal Treatment, and Longitudinal Outcome: Evidence, Paradox, and Challenge. Wiley Interdiscip. Rev. Cogn. Sci. 2015, 6, 39–52. [Google Scholar] [CrossRef]
- Caye, A.; Swanson, J.M.; Coghill, D.; Rohde, L.A. Treatment Strategies for ADHD: An Evidence-Based Guide to Select Optimal Treatment. Mol. Psychiatry 2019, 24, 390–408. [Google Scholar] [CrossRef]
- Hennissen, L.; Bakker, M.J.; Banaschewski, T.; Carucci, S.; Coghill, D.; Danckaerts, M.; Dittmann, R.W.; Hollis, C.; Kovshoff, H.; McCarthy, S.; et al. Cardiovascular Effects of Stimulant and Non-Stimulant Medication for Children and Adolescents with ADHD: A Systematic Review and Meta-Analysis of Trials of Methylphenidate, Amphetamines and Atomoxetine. CNS Drugs 2017, 31, 199–215. [Google Scholar] [CrossRef]
- Krain, A.L.; Kendall, P.C.; Power, T.J. The Role of Treatment Acceptability in the Initiation of Treatment for ADHD. J. Atten. Disord. 2005, 9, 425–434. [Google Scholar] [CrossRef]
- Lee, J.; Grizenko, N.; Bhat, V.; Sengupta, S.; Polotskaia, A.; Joober, R. Relation between Therapeutic Response and Side Effects Induced by Methylphenidate as Observed by Parents and Teachers of Children with ADHD. BMC Psychiatry 2011, 11, 70. [Google Scholar] [CrossRef]
- Rajwan, E.; Chacko, A.; Moeller, M. Nonpharmacological Interventions for Preschool ADHD: State of the Evidence and Implications for Practice. Prof. Psychol. Res. Pract. 2012, 43, 520–526. [Google Scholar] [CrossRef]
- Sonuga-Barke, E.J.S.; Brandeis, D.; Cortese, S.; Daley, D.; Ferrin, M.; Holtmann, M.; Stevenson, J.; Danckaerts, M.; Van Der Oord, S.; Döpfner, M.; et al. Nonpharmacological Interventions for ADHD: Systematic Review and Meta-Analyses of Randomized Controlled Trials of Dietary and Psychological Treatments. Am. J. Psychiatry 2013, 170, 275–289. [Google Scholar] [CrossRef] [PubMed]
- Kerns, K.A.; Eso, K.; Thomson, J. Investigation of a Direct Intervention for Improving Attention in Young Children With ADHD. Dev. Neuropsychol. 1999, 16, 273–295. [Google Scholar] [CrossRef]
- Kolodny, T.; Ashkenazi, Y.; Farhi, M.; Shalev, L. Computerized Progressive Attention Training (CPAT) vs. Active Control in Adults with ADHD. J. Cogn. Enhanc. 2017, 1, 526–538. [Google Scholar] [CrossRef]
- Shalev, L.; Tsal, Y.; Mevorach, C. Computerized Progressive Attentional Training (CPAT) Program: Effective Direct Intervention for Children with ADHD. Child Neuropsychol. 2007, 13, 382–388. [Google Scholar] [CrossRef]
- Spaniol, M.M.; Shalev, L.; Kossyvaki, L.; Mevorach, C. Attention Training in Autism as a Potential Approach to Improving Academic Performance: A School-Based Pilot Study. J. Autism Dev. Disord. 2018, 48, 592–610. [Google Scholar] [CrossRef]
- Tamm, L.; Epstein, J.N.; Peugh, J.L.; Nakonezny, P.A.; Hughes, C.W. Preliminary Data Suggesting the Efficacy of Attention Training for School-Aged Children with ADHD. Dev. Cogn. Neurosci. 2013, 4, 16–28. [Google Scholar] [CrossRef]
- Trinczer, I.L.; Maayan, T.; Shalev, L. “Attentive Kindergarten”: A Small Group Intervention Boosting Attention among Kindergarten Children. Educ. Sci. 2023, 13, 664. [Google Scholar] [CrossRef]
- Shalev, L.; Kataev, N.; Mevorach, C. Training of Cognitive Control in Developmental Disorders: Pitfalls and Promises. In interventions in Learning Disabilities: A Handbook on Systematic Training Programs for Individuals with Learning Disabilities; Springer International Publishing: Cham, Switzerland, 2016; pp. 243–254. [Google Scholar]
- Epstein, J.N.; Tsal, Y. Evidence for Cognitive Training as a Treatment Strategy for Children With Attention-Deficit/Hyperactivity Disorder. J. ADHD Relat. Disord. 2010, 1, 49–64. [Google Scholar]
- Posner, M.I.; Rothbart, M.K. Influencing Brain Networks: Implications for Education. Trends Cogn. Sci. 2005, 9, 99–103. [Google Scholar] [CrossRef]
- Tamm, L.; Hughes, C.; Ames, L.; Pickering, J.; Silver, C.H.; Stavinoha, P.; Castillo, C.L.; Rintelmann, J.; Moore, J.; Foxwell, A.; et al. Attention Training for School-Aged Children with ADHD: Results of an Open Trial. J. Atten. Disord. 2010, 14, 86–94. [Google Scholar] [CrossRef] [PubMed]
- Semrud-Clikeman, M.; Nielsen, K.H.; Clinton, A.; Sylvester, L.; Parle, N.; Connor, R.T. An Intervention Approach for Children with Teacher-and Parent-Identified Attentional Difficulties. J. Learn. Disabil. 1999, 32, 581–590. [Google Scholar] [CrossRef] [PubMed]
- Davis, N.O.; Bower, J.; Kollins, S.H. Proof-of-Concept Study of an at-Home, Engaging, Digital Intervention for Pediatric ADHD. PLoS ONE 2018, 13, e0189749. [Google Scholar] [CrossRef] [PubMed]
- Kollins, S.H.; DeLoss, D.J.; Cañadas, E.; Lutz, J.; Findling, R.L.; Keefe, R.S.E.; Epstein, J.N.; Cutler, A.J.; Faraone, S.V. A Novel Digital Intervention for Actively Reducing Severity of Paediatric ADHD (STARS-ADHD): A Randomised Controlled Trial. Lancet Digit. Health 2020, 2, e168–e178. [Google Scholar] [CrossRef]
- Wexler, B.E.; Vitulano, L.A.; Moore, C.; Katsovich, L.; Smith, S.D.; Rush, C.; Grantz, H.; Dong, J.; Leckman, J.F. An Integrated Program of Computer-Presented and Physical Cognitive Training Exercises for Children with Attention-Deficit/Hyperactivity Disorder. Psychol. Med. 2020, 51, 1524–1535. [Google Scholar] [CrossRef]
- Klingberg, T.; Forssberg, H.; Westerberg, H. Training of Working Memory in Children with ADHD. J. Clin. Exp. Neuropsychol. 2002, 24, 781–791. [Google Scholar] [CrossRef]
- Klingberg, T.; Fernell, E.; Olesen, P.J.; Johnson, M.; Gustafsson, P.; Dahlstrom, K.; Gillberg, C.G.; Forssberg, H.; Westerberg, H. Computerized Training of Working Memory in Children With ADHD—A Randomized, Controlled Trial. J. Am. Acad. Child Adolesc. Psychiatry 2005, 44, 177–186. [Google Scholar] [CrossRef]
- Jones, M.R.; Katz, B.; Buschkuehl, M.; Jaeggi, S.M.; Shah, P. Exploring N-Back Cognitive Training for Children with ADHD. J. Atten. Disord. 2018, 24, 704–719. [Google Scholar] [CrossRef]
- Steiner, N.J.; Sheldrick, R.C.; Gotthelf, D.; Perrin, E.C. Computer-Based Attention Training in the Schools for Children With Attention Deficit/Hyperactivity Disorder: A Preliminary Trial. Clin. Pediatr. 2011, 50, 615–622. [Google Scholar] [CrossRef]
- Chimiklis, A.L. Examining the Effects of a Multi-Component Neurocognitive Intervention for School-Aged Children with Co-Occurring ADHD and Reading Difficulties. Ph.D. Thesis, City University of New York, New York, NY, USA, 2019; pp. 1–138. [Google Scholar]
- Rabiner, D.L.; Murray, D.W.; Skinner, A.T.; Malone, P.S. A Randomized Trial of Two Promising Computer-Based Interventions for Students with Attention Difficulties. J. Abnorm. Child Psychol. 2010, 38, 131–142. [Google Scholar] [CrossRef]
- van der Donk, M.; Hiemstra-Beernink, A.C.; Tjeenk-Kalff, A.; van der Leij, A.; Lindauer, R. Cognitive Training for Children with ADHD: A Randomized Controlled Trial of Cogmed Working Memory Training and ‘Paying Attention in Class. Front. Psychol. 2015, 6, 1081. [Google Scholar] [CrossRef] [PubMed]
- Gray, S.A.; Chaban, P.; Martinussen, R.; Goldberg, R.; Gotlieb, H.; Kronitz, R.; Hockenberry, M.; Tannock, R. Effects of a Computerized Working Memory Training Program on Working Memory, Attention, and Academics in Adolescents with Severe LD and Comorbid ADHD: A Randomized Controlled Trial. J. Child Psychol. Psychiatry 2012, 53, 1277–1284. [Google Scholar] [CrossRef] [PubMed]
- Cortese, S.; Ferrin, M.; Brandeis, D.; Buitelaar, J.; Daley, D.; Dittmann, R.W.; Holtmann, M.; Santosh, P.; Stevenson, J.; Stringaris, A.; et al. Cognitive Training for Attention-Deficit/Hyperactivity Disorder: Meta-Analysis of Clinical and Neuropsychological Outcomes From Randomized Controlled Trials. J. Am. Acad. Child Adolesc. Psychiatry 2015, 54, 164–174. [Google Scholar] [CrossRef] [PubMed]
- Rapport, M.D.; Orban, S.A.; Kofler, M.J.; Friedman, L.M. Do Programs Designed to Train Working Memory, Other Executive Functions, and Attention Benefit Children with ADHD? A Meta-Analytic Review of Cognitive, Academic, and Behavioral Outcomes. Clin. Psychol. Rev. 2013, 33, 1237–1252. [Google Scholar] [CrossRef]
- Sonuga-barke, E.; Brandeis, D.; Holtmann, M.; Cortese, S. Computer-Based Cognitive Training for ADHD A Review of Current Evidence. Child Adolesc. Psychiatr. Clin. N. Am. 2014, 23, 807–824. [Google Scholar] [CrossRef]
- Coghill, D.R.; Seth, S.; Matthews, K. A Comprehensive Assessment of Memory, Delay Aversion, Timing, Inhibition, Decision Making and Variability in Attention Deficit Hyperactivity Disorder: Advancing beyond the Three-Pathway Models. Psychol. Med. 2014, 44, 1989–2001. [Google Scholar] [CrossRef]
- Nigg, J. Attention-Deficit/Hyperactivity Disorder and Adverse Health Outcomes. Clin. Psychol. Rev. 2013, 33, 215–228. [Google Scholar] [CrossRef]
- Sonuga-barke, E.; Bitsakou, P.; Thompson, M. Beyond the Dual Pathway Model: Evidence for the Dissociation of Timing, Inhibitory, Attention-Deficit/Hyperactivity Disorder. J. Am. Acad. Child Adolesc. Psychiatry 2010, 49, 345–355. [Google Scholar]
- Tsal, Y.; Shalev, L.; Mevorach, C. The Diversity of Attention Deficits in ADHD: The Prevalence of Four Cognitive Factors in ADHD versus Controls. J. Learn. Disabil. 2005, 38, 142–157. [Google Scholar] [CrossRef]
- Van Hulst, B.M.; de Zeeuw, P.; Durston, S. Distinct Neuropsychological Profiles within ADHD: A Latent Class Analysis of Cognitive Control, Reward Sensitivity and Timing. Psychol. Med. 2015, 45, 735–745. [Google Scholar] [CrossRef]
- Nigg, J.T.; Willcutt, E.G.; Doyle, A.E.; Sonuga-barke, E.J.S. Causal Heterogeneity in Attention-Deficit/Hyperactivity Disorder: Do We Need Neuropsychologically Impaired Subtypes? Biol. Psychiatry 2005, 57, 1224–1230. [Google Scholar] [CrossRef] [PubMed]
- Trinczer, I.; Shalev, L. Heterogeneous Cognitive Profiles among Children with Attention Deficit/Hyperactivity Disorder (ADHD). J. Vis. 2018, 18, 1122. [Google Scholar] [CrossRef]
- Nigg, J.T. What Causes ADHD?: Understanding What Goes Wrong and Why; Guilford Press: New York, NY, USA, 2006; ISBN 1593852673. [Google Scholar]
- Nigg, J.T.; Casey, B.J. An Integrative Theory of Attention-Deficit/Hyperactivity Disorder Based on the Cognitive and Affective Neurosciences. Dev. Psychol. 2005, 17, 785–806. [Google Scholar] [CrossRef] [PubMed]
- Pennington, B.F. From Single to Multiple Deficit Models of Developmental Disorders. Cognition 2006, 101, 385–413. [Google Scholar] [CrossRef]
- Willcutt, E.G.; Pennington, B.F.; Duncan, L.; Smith, S.D.; Keenan, J.M.; Wadsworth, S.; DeFries, J.C.; Olson, R.K. Understanding the Complex Etiologies of Developmental Disorders: Behavioral and Molecular Genetic Approaches. J. Dev. Behav. Pediatr. 2010, 31, 533–544. [Google Scholar] [CrossRef]
- Shalev, L.; Tsal, Y. The Wide Attentional Window: A Major Deficit of Children with Attention Difficulties. J. Learn. Disabil. 2003, 36, 517–527. [Google Scholar] [CrossRef]
- Shalev, L.; Kolodny, T.; Shalev, N.; Mevorach, C. Attention Functioning among Adolescents with Multiple Learning, Attentional, Behavioral, and Emotional Difficulties. J. Learn. Disabil. 2016, 49, 582–596. [Google Scholar] [CrossRef]
- Lukov, L.; Friedmann, N.; Shalev, L.; Khentov-kraus, L.; Shalev, N.; Lorber, R.; Guggenheim, R. Dissociations between Developmental Dyslexias and Attention Deficits. Front. Hum. Neurosci. 2015, 5, 1501. [Google Scholar] [CrossRef]
- Barkley, R.A. Behavioral Inhibition, Sustained Attention, and Executive Functions: Constructing a Unifying Theory of ADHD. Psychol. Bull. 1997, 121, 65–94. [Google Scholar] [CrossRef]
- Brown, T.E. Attention Deficit Disorder: The Unfocused Mind in Children and Adults; Yale University Press: New Haven, CT, USA, 2005; ISBN 9780300106411. [Google Scholar]
- Miyake, A.; Friedman, N.P.; Emerson, M.J.; Witzki, A.H.; Howerter, A.; Wager, T.D. The Unity and Diversity of Executive Functions and Their Contributions to Complex “Frontal Lobe” Tasks: A Latent Variable Analysis. Cognit. Psychol. 2000, 41, 49–100. [Google Scholar] [CrossRef]
- Friedman, N.P.; Miyake, A. Unity and Diversity of Executive Functions: Individual Differences as a Window on Cognitive Structure. CORTEX 2017, 86, 186–204. [Google Scholar] [CrossRef] [PubMed]
- Lehto, J.E.; Juujärvi, P.; Kooistra, L.; Pulkkinen, L. Dimensions of Executive Functioning: Evidence from Children. Br. J. Dev. Psychol. 2003, 21, 59–80. [Google Scholar] [CrossRef]
- Collins, A.; Koechlin, E. Reasoning, Learning, and Creativity: Frontal Lobe Function and Human Decision-Making. PLoS Biol. 2012, 10, 1001293. [Google Scholar] [CrossRef] [PubMed]
- Miller, K.J. Executive Functions. Pediatr. Ann. 2005, 34, 310–317. [Google Scholar] [CrossRef] [PubMed]
- Diamond, A.; Barnett, W.S.; Thomas, J.; Munro, S. Preschool Program Improves Cognitive Control. Science 2007, 318, 1387–1388. [Google Scholar] [CrossRef]
- Banich, M.T. Executive Function: The Search for an Integrated Account. Curr. Dir. Psychol. Sci. 2009, 18, 89–94. [Google Scholar] [CrossRef]
- Schreiber, J.E.; Possin, K.L.; Girard, J.M.; Rey-Casserly, C. Executive Function in Children with Attention Deficit/Hyperactivity Disorder: The NIH EXAMINER Battery. J. Int. Neuropsychol. Soc. 2014, 20, 41–51. [Google Scholar] [CrossRef]
- Kofler, M.J.; Rapport, M.D.; Bolden, J.; Altro, T.A. Working Memory as a Core Deficit in ADHD: Preliminary Findings and Implications. ADHD Rep. 2008, 16, 8–14. [Google Scholar] [CrossRef]
- Gansler, D.A.; Fucetola, R.; Krengel, M.; Stetson, S.; Zimering, R.; Makary, C. Are There Cognitive Subtypes in Adult Attention Deficit/Hyperactivity Disorder? J. Nerv. Ment. Dis. 1998, 186, 776–781. [Google Scholar] [CrossRef]
- Raiker, J.S.; Rapport, M.D.; Kofler, M.J.; Sarver, D.E. Objectively-Measured Impulsivity and Attention-Deficit/Hyperactivity Disorder (ADHD): Testing Competing Predictions from the Working Memory and Behavioral Inhibition Models of ADHD. J. Abnorm. Child Psychol. 2012, 40, 699–713. [Google Scholar] [CrossRef]
- Kasper, L.J.; Alderson, R.M.; Hudec, K.L. Moderators of Working Memory Deficits in Children with Attention-Deficit/Hyperactivity Disorder (ADHD): A Meta-Analytic Review. Clin. Psychol. Rev. 2012, 32, 605–617. [Google Scholar] [CrossRef] [PubMed]
- Cockcroft, K. Working Memory Functioning in Children with Attention-Deficit/Hyperactivity Disorder (ADHD): A Comparison between Subtypes and Normal Controls. J. Child Adolesc. Ment. Health 2011, 23, 107–118. [Google Scholar] [CrossRef] [PubMed]
- Boonstra, A.M.; Oosterlaan, J.; Sergeant, J.A.; Buitelaar, J.K. Executive Functioning in Adult ADHD: A Meta-Analytic Review. Psychol. Med. 2005, 35, 1097–1108. [Google Scholar] [CrossRef] [PubMed]
- Van De Voorde, S.; Roeyers, H.; Verté, S.; Wiersema, J.R. Working Memory, Response Inhibition, and within-Subject Variability in Children with Attention-Deficit/Hyperactivity Disorder or Reading Disorder. J. Clin. Exp. Neuropsychol. 2010, 32, 366–379. [Google Scholar] [CrossRef]
- O’Neill, S.; Berwid, O.; Bédard, A. The Exercise–Cognition Interaction and ADHD. In Exercise-Cognition Interaction; McMorris, T., Ed.; Academic Press: Cambridge, MA, USA, 2016; pp. 375–398. [Google Scholar]
- Baddeley, A.D.; Hitch, G.J. Development of Working Memory: Should the Pascual-Leone and the Baddeley and Hitch Models Be Merged? J. Exp. Child Psychol. 2000, 77, 128–137. [Google Scholar] [CrossRef]
- Baddeley, A. Working Memory. Curr. Biol. 2010, 20, R136–R140. [Google Scholar] [CrossRef]
- Owen, A.M. Cognitive Planning in Humans: Neuropsychological, Neuroanatomical and Neuropharmacological Perspectives. Prog. Neurobiol. 1997, 53, 431–450. [Google Scholar] [CrossRef]
- Robinson, S.; Goddard, L.; Dritschel, B.; Wisley, M.; Howlin, P. Executive Functions in Children with Autism Spectrum Disorders. Brain Cogn. 2009, 71, 362–368. [Google Scholar] [CrossRef]
- Spaniol, M.; Mevorach, C.; Shalev, L.; Teixeira, M.C.T.V.; Lowenthal, R.; de Paula, C.S. Attention Training in Children with Autism Spectrum Disorder Improves Academic Performance: A Double-Blind Pilot Application of the Computerized Progressive Attentional Training Program. Autism Res. 2021, 14, 1769–1776. [Google Scholar] [CrossRef]
- Stern, P.; Kolodny, T.; Tsafrir, S.; Cohen, G.; Shalev, L. Near and Far Transfer Effects of Computerized Progressive Attention Training (CPAT) Versus Mindfulness Based Stress Reduction (MBSR) Practice Among Adults With ADHD. J. Atten. Disord. 2023, 27, 757–776. [Google Scholar] [CrossRef]
- Yalom, I.D. The Theory and Practice of Group Psychotherapy; Basic Books: New York, NY, USA, 1970. [Google Scholar]
- Brunelli, A.A.; Murphy, G.C.; Athanasou, J.A. Effectiveness of Social Support Group Interventions for Psychosocial Outcomes: A Meta-Analytic Review. Aust. J. Rehabil. Couns. 2016, 22, 104–127. [Google Scholar] [CrossRef]
- Segal, D.; Mashal, N.; Shalev, L. Semantic Conflicts Are Resolved Differently by Adults with and without ADHD. Res. Dev. Disabil. 2015, 47, 416–429. [Google Scholar] [CrossRef] [PubMed]
- Treisman, A.M.; Gelade, G. A Feature-Integration Theory of Attention. Cognit. Psychol. 1980, 12, 97–136. [Google Scholar] [CrossRef] [PubMed]
- Corsi, M.P. Human Memory and the Medial Temporal Lobe Region of the Brain. Ph.D. Thesis, McGill University, Montreal, QC, Canada, 1972. [Google Scholar]
- Kessels, R.P.; Van Zandvoort, M.J.; Postma, A.; Kappelle, L.J.; De Haan, E.H. The Corsi Block-Tapping Task: Standardization and Normative Data. Appl. Neuropsychol. 2000, 7, 252–258. [Google Scholar] [CrossRef] [PubMed]
- Kessels, R.P.C.; Berg, E.V.D.; Ruis, C.; Brands, A.M.A. The Backward Span of the Corsi Block-Tapping Task and Its Association With the WAIS-III Digit Span. Assessment 2008, 15, 426–434. [Google Scholar] [CrossRef]
- Raven, J.C. Coloured Progressive Matrices (CPM); Beltz Test Gesellschaft: Göttingen, Germany, 2002. [Google Scholar]
- Achenbach, T.; Rescorla, L. Manual for the ASEBA School-Age Forms & Profiles: Child Behavior Checklist for Ages 6-18, Teacher’s Report Form, Youth Self-Report; University of Vermont, Research Center for Children, Youth, and Families: Burlington, VT, USA, 2001; ISBN 9780938565734. [Google Scholar]
- Gioia, G.; Isquith, P.; Guy, S.; Kenworthy, L. Behavior Rating Inventory of Executive Function: BRIEF; Psychological Assessment Resources: Odessa, FL, USA, 2000. [Google Scholar]
- Tuckman, B.W. Developmental Sequence in Small Groups. Psychol. Bull. 1965, 63, 384–399. [Google Scholar] [CrossRef]
- Tuckman, B.W.; Jensen, M.A.C. Stages of Small-Group Development Revisited. Group Organ. Manag. 1977, 2, 419–427. [Google Scholar] [CrossRef]
- Kolodny, T.; Mevorach, C.; Shalev, L. Isolating Response Inhibition in the Brain: Parietal versus Frontal Contribution. Cortex 2017, 88, 173–185. [Google Scholar] [CrossRef]
- Eriksen, B.; Eriksen, C.W. Effects of Noise Letters upon the Identification of a Target Letter in a Nonsearch Task. Percept. Psychophys. 1974, 16, 143–149. [Google Scholar] [CrossRef]
- Posner, M.I.; Snyder, C.R.R.; Davidson, B.J. Attention and the Detection of Signals. J. Exp. Psychol. 1980, 109, 160–174. [Google Scholar] [CrossRef]
- Navon, D. Forest before Trees: The Precedence of Global Features in Visual Perception. Cognit. Psychol. 1977, 9, 353–383. [Google Scholar] [CrossRef]
- Davis, B.L.; Maclagan, D. The Card Game Set. Math. Intell. 2003, 25, 33–40. [Google Scholar] [CrossRef]
- Kirchner, W.K. Age Differences in Short-Term Retention of Rapidly Changing Information. J. Exp. Psychol. 1958, 55, 352–358. [Google Scholar] [CrossRef] [PubMed]
- Kerns, K.A.; Macsween, J.; Wekken, S.V.; Gruppuso, V. Investigating the Efficacy of an Attention Training Programme in Children with Foetal Alcohol Spectrum Disorder. Dev. Neurorehabilit. 2010, 13, 413–422. [Google Scholar] [CrossRef]
- Sampanis, D.; Mevorach, C.; Shalev, L.; Mohammed, S.; Humphreys, G. Reducing Cognitive Deficits after Stroke through Computerized Progressive Attentional Training (CPAT): A Pilot Study. Phys. Med. Rehabil. Int. 2015, 2, 1058. [Google Scholar]
- Bikic, A.; Leckman, J.F.; Christensen, T.Ø.; Bilenberg, N.; Dalsgaard, S. Attention and Executive Functions Computer Training for Attention—Deficit/Hyperactivity Disorder (ADHD): Results from a Randomized, Controlled Trial. Eur. Child Adolesc. Psychiatry 2018, 27, 1563–1574. [Google Scholar] [CrossRef]
- Lange, K.W.; Tucha, L.; Hauser, J.; Lange, K.M.; Stasik, D.; Tucha, O. Attention Training in Attention Deficit Hyperactivity Disorder. Aula Abierta 2012, 40, 55–60. [Google Scholar]
- Jaeggi, S.M.; Buschkuehl, M.; Jonides, J.; Perrig, W.J. Improving Fluid Intelligence with Training on Working Memory. Proc. Natl. Acad. Sci. USA 2008, 105, 6829–6833. [Google Scholar] [CrossRef]
- Rueda, M.R.; Rothbart, M.K.; Mccandliss, B.D.; Saccomanno, L.; Posner, M.I. Training, Maturation, and Genetic Influences on the Development of Executive Attention. Proc. Natl. Acad. Sci. USA 2005, 102, 4931–14936. [Google Scholar] [CrossRef]
- Rueda, M.R.; Checa, P.; Cómbita, L.M. Enhanced Efficiency of the Executive Attention Network after Training in Preschool Children: Immediate Changes and Effects after Two Months. Dev. Cogn. Neurosci. 2012, 2, S192–S204. [Google Scholar] [CrossRef]
- Au, J.; Sheehan, E.; Tsai, N.; Duncan, G.J.; Buschkuehl, M.; Jaeggi, S.M. Improving Fluid Intelligence with Training on Working Memory: A Meta-Analysis. Psychon. Bull. Rev. 2015, 22, 366–377. [Google Scholar] [CrossRef]
- van der Oord, S.; Ponsioen, A.J.G.B.; Geurts, H.M.; Brink, E.L.T.; Prins, P.J.M. A Pilot Study of the Efficacy of a Computerized Executive Functioning Remediation Training With Game Elements for Children With ADHD in an Outpatient Setting: Outcome on Parent- and Teacher- Rated Executive Functioning and ADHD Behavior. J. Atten. Disord. 2012, 18, 699–712. [Google Scholar] [CrossRef]

| Age | Gender | Medication Status | |||||
|---|---|---|---|---|---|---|---|
| Group | n | M | SD | n | n | ||
| AFT | 27 | 10.38 | 1.12 | Boys | 18 | Use | 12 |
| Girls | 9 | Do Not Use | 15 | ||||
| EFT | 29 | 10.46 | 1.07 | Boys | 16 | Use | 13 |
| Girls | 13 | Do Not Use | 16 | ||||
| PC | 24 | 10.53 | 1.15 | Boys | 17 | Use | 19 |
| Girls | 7 | Do Not Use | 5 | ||||
| Domain | Assessment Tool | Description | Outcome Measures |
|---|---|---|---|
| Sustained attention | Continuous Performance Test (CPT) | Participants respond to target geometric shapes while ignoring others |
|
| Selective-spatial attention | Conjunctive Visual Search Task (CVST) | Search for blue square among red squares and blue circles |
|
| Visuospatial working memory | Corsi Block-Tapping Task Forward | Reproduce sequence of lit blocks in same order |
|
| Visuospatial working memory | Corsi Block-Tapping Task Backward | Reproduce sequence of lit blocks in reverse order |
|
| Nonverbal abstract reasoning | Raven’s Colored Progressive Matrices | Complete visual patterns |
|
| Behavioural symptoms | CBCL Questionnaire | Parent-rated behavioural assessment |
|
| Executive functioning | BRIEF Questionnaire | Parent-rated executive function assessment |
|
| Arithmetic | Arithmetic Evaluation | Basic arithmetic operations |
|
| AFT | EFT | |
|---|---|---|
| Near transfer | Sustained attention (+) | Nonverbal abstract reasoning (+) |
| Selective-spatial attention (+) | ||
| Far transfer | ADHD symptomatology (N/A) | ADHD symptomatology (N/A) |
| Nonverbal abstract reasoning (+) | ||
| Arithmetic performance 1 (−) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Trinczer, I.L.; Shalev, L. Computerised Attention Functions Training Versus Computerised Executive Functions Training for Children with Attention Deficit/Hyperactivity Disorder: A Randomised Controlled Trial. J. Clin. Med. 2024, 13, 7239. https://doi.org/10.3390/jcm13237239
Trinczer IL, Shalev L. Computerised Attention Functions Training Versus Computerised Executive Functions Training for Children with Attention Deficit/Hyperactivity Disorder: A Randomised Controlled Trial. Journal of Clinical Medicine. 2024; 13(23):7239. https://doi.org/10.3390/jcm13237239
Chicago/Turabian StyleTrinczer, Inbar Lucia, and Lilach Shalev. 2024. "Computerised Attention Functions Training Versus Computerised Executive Functions Training for Children with Attention Deficit/Hyperactivity Disorder: A Randomised Controlled Trial" Journal of Clinical Medicine 13, no. 23: 7239. https://doi.org/10.3390/jcm13237239
APA StyleTrinczer, I. L., & Shalev, L. (2024). Computerised Attention Functions Training Versus Computerised Executive Functions Training for Children with Attention Deficit/Hyperactivity Disorder: A Randomised Controlled Trial. Journal of Clinical Medicine, 13(23), 7239. https://doi.org/10.3390/jcm13237239






