Electrical Impedance Tomography-Based Evaluation of Anesthesia-Induced Development of Atelectasis in Obese Patients
Abstract
1. Introduction
2. Materials and Methods
2.1. Patients
2.2. Electrical Impedance Tomography (EIT)
2.3. EIT Measurements
2.4. Induction of General Anesthesia and Mechanical Ventilation
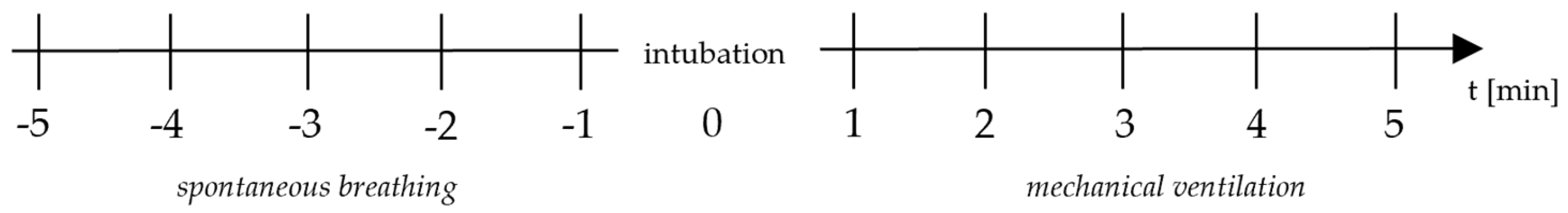
2.5. Endpoints and Study Procedure
2.6. Statistical Analysis
3. Results
Distribution of Tidal Ventilation and GI Index Five Minutes Pre- and Post-Intubation
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Obesity Federation. World Obesity Observatory. 2024. Available online: https://data.worldobesity.org (accessed on 27 July 2024).
- Westbrook, P.R.; Stubbs, S.E.; Sessler, A.D.; Rehder, K.; Hyatt, R.E. Effects of Anesthesia and Muscle Paralysis on Respiratory Mechanics in Normal Man. J. Appl. Physiol. 1973, 34, 81–86. [Google Scholar] [CrossRef]
- Hedenstierna, G.; Edmark, L. Mechanisms of Atelectasis in the Perioperative Period. Best Pract. Res. Clin. Anaesthesiol. 2010, 24, 157–169. [Google Scholar] [CrossRef] [PubMed]
- Brismar, B.; Hedenstierna, G.; Lundquist, H.; Strandberg, A.; Svensson, L.; Tokics, L. Pulmonary Densities During Anesthesia with Muscular Relaxation—A Proposal of Atelectasis. Anesthesiology 1985, 62, 422–428. [Google Scholar] [CrossRef] [PubMed]
- Dantzker, D.R.; Wagner, P.D.; West, J.B. Proceedings: Instability of Poorly Ventilated Lung Units During Oxygen Breathing. J. Physiol. 1974, 242, 72. [Google Scholar]
- Reinius, H.; Jonsson, L.; Gustafsson, S.; Sundbom, M.; Duvernoy, O.; Pelosi, P.; Hedenstierna, G.; Freden, F. Prevention of Atelectasis in Morbidly Obese Patients During General Anesthesia and Paralysis: A Computerized Tomography Study. Anesthesiology 2009, 111, 979–987. [Google Scholar] [CrossRef]
- Pelosi, P.; Croci, M.; Ravagnan, I.; Tredici, S.; Pedoto, A.; Lissoni, A.; Gattinoni, L. The Effects of Body Mass on Lung Volumes, Respiratory Mechanics, and Gas Exchange During General Anesthesia. Anesth. Analg. 1998, 87, 654–660. [Google Scholar] [CrossRef]
- Boriek, A.M.; Lopez, M.A.; Velasco, C.; Bakir, A.A.; Frolov, A.; Wynd, S.; Babb, T.G.; Hanania, N.A.; Hoffman, E.A.; Sharafkhaneh, A. Obesity Modulates Diaphragm Curvature in Subjects with and without Copd. Am. J. Physiol. Integr. Comp. Physiol. 2017, 313, R620–R629. [Google Scholar] [CrossRef]
- Jones, R.L.; Nzekwu, M.M. The Effects of Body Mass Index on Lung Volumes. Chest 2006, 130, 827–833. [Google Scholar] [CrossRef]
- Lellouche, F.; Dionne, S.; Simard, S.; Bussières, J.; Dagenais, F. High Tidal Volumes in Mechanically Ventilated Patients Increase Organ Dysfunction after Cardiac Surgery. Anesthesiology 2012, 116, 1072–1082. [Google Scholar] [CrossRef]
- Bluth, T.; Neto, A.S.; Schultz, M.J.; Pelosi, P.; de Abreu, M.G. Effect of Intraoperative High Positive End-Expiratory Pressure (Peep) with Recruitment Maneuvers vs. Low Peep on Postoperative Pulmonary Complications in Obese Patients: A Randomized Clinical Trial. JAMA 2019, 321, 2292–2305. [Google Scholar]
- Rothen, H.U.; Sporre, B.; Engberg, G.; Wegenius, G.; Hedenstierna, G. Re-Expansion of Atelectasis During General Anaesthesia: A Computed Tomography Study. Br. J. Anaesth. 1993, 71, 788–795. [Google Scholar] [CrossRef] [PubMed]
- Cammarota, G.; Simonte, R.; Longhini, F.; Spadaro, S.; Vetrugno, L.; De Robertis, E. Advanced Point-of-Care Bedside Monitoring for Acute Respiratory Failure. Anesthesiology 2023, 138, 317–334. [Google Scholar] [CrossRef] [PubMed]
- Braun, M.; Ruscher, L.; Fuchs, A.; Kämpfer, M.; Huber, M.; Luedi, M.M.; Riva, T.; Vogt, A.; Riedel, T. Atelectasis in obese patients undergoing laparoscopic bariatric surgery are not increased upon discharge from Post Anesthesia Care Unit. Front. Med. 2023, 10, 1233609. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Dargvainis, M.; Ohnesorge, H.; Schädler, D.; Alkatout, I.; Frerichs, I.; Becher, T. Recruitable alveolar collapse and overdistension during laparoscopic gynecological surgery and mechanical ventilation: A prospective clinical study. BMC Anesthesiol. 2022, 22, 251. [Google Scholar] [CrossRef]
- Girrbach, F.; Petroff, D.; Schulz, S.; Hempel, G.; Lange, M.; Klotz, C.; Scherz, S.; Giannella-Neto, A.; Beda, A.; Jardim-Neto, A.; et al. Individualised Positive End-Expiratory Pressure Guided by Electrical Impedance Tomography for Robot-Assisted Laparoscopic Radical Prostatectomy: A Prospective, Randomised Controlled Clinical Trial. Br. J. Anaesth. 2020, 125, 373–382. [Google Scholar] [CrossRef]
- Vasques, F.; Sanderson, B.; Barrett, N.A.; Camporota, L. Monitoring of Regional Lung Ventilation Using Electrical Impedance Tomography. Minerva Anestesiol. 2019, 85, 1231–1241. [Google Scholar] [CrossRef]
- Nestler, C.; Simon, P.; Petroff, D.; Hammermüller, S.; Kamrath, D.; Wolf, S.; Dietrich, A.; Camilo, L.M.; Beda, A.; Carvalho, A.R.; et al. Individualized Positive End-Expiratory Pressure in Obese Patients During General Anaesthesia: A Randomized Controlled Clinical Trial Using Electrical Impedance Tomography. Br. J. Anaesth. 2017, 119, 1194–1205. [Google Scholar] [CrossRef]
- Girrbach, F.; Petroff, D.; Mols, S.; Brechtelsbauer, K.; Wrigge, H.; Simon, P. Extubation with Reduced Inspiratory Oxygen Concentration or Postoperative Continuous Positive Pressure to Improve Oxygenation after Laparoscopic Bariatric Surgery: A Randomized Controlled Trial. Anesthesiology 2023, 139, 546–548. [Google Scholar] [CrossRef]
- Canet, J.; Gallart, L.; Gomar, C.; Paluzie, G.; Valles, J.; Castillo, J.; Sabate, S.; Mazo, V.; Briones, Z.; Sanchis, J.; et al. Prediction of Postoperative Pulmonary Complications in a Population-Based Surgical Cohort. Anesthesiology 2010, 113, 1338–1350. [Google Scholar] [CrossRef]
- Costa, E.L.; Lima, R.G.; Amato, M.B. Electrical Impedance Tomography. Curr. Opin. Crit. Care 2009, 15, 18–24. [Google Scholar] [CrossRef]
- Zhao, Z.; Möller, K.; Steinmann, D.; Frerichs, I.; Guttmann, J. Evaluation of an Electrical Impedance Tomography-Based Global Inhomogeneity Index for Pulmonary Ventilation Distribution. Intensiv. Care Med. 2009, 35, 1900–1906. [Google Scholar] [CrossRef] [PubMed]
- Eichenberger, A.-S.; Proietti, S.; Wicky, S.; Frascarolo, P.; Suter, M.; Spahn, D.R.; Magnusson, L. Morbid Obesity and Postoperative Pulmonary Atelectasis: An Underestimated Problem. Anesthesia Analg. 2002, 95, 1788–1792. [Google Scholar] [CrossRef] [PubMed]
- Mancilla-Galindo, J.; Ortiz-Gomez, J.E.; Pérez-Nieto, O.R.; De Jong, A.; Escarramán-Martínez, D.; Kammar-García, A.; Mata, L.C.R.; Díaz, A.M.; Guerrero-Gutiérrez, M.A. Preoperative Atelectasis in Patients with Obesity Undergoing Bariatric Surgery: A Cross-Sectional Study. Anesth Analg. 2024, Epub ahead of print. [CrossRef] [PubMed]
- Hedenstierna, G.; Rothen, H.U. Respiratory Function During Anesthesia: Effects on Gas Exchange. Comp. Physiol. 2012, 2, 69–96. [Google Scholar]
- Hedenstierna, G.; Tokics, L.; Scaramuzzo, G.; Rothen, H.U.; Edmark, L.; Ohrvik, J. Oxygenation Impairment During Anesthesia: Influence of Age and Body Weight. Anesthesiology 2019, 131, 46–57. [Google Scholar] [CrossRef]
- Hedenstierna, G.; Santesson, J. Breathing Mechanics, Dead Space and Gas Exchange in the Extremely Obese, Breathing Spontaneously and During Anaesthesia with Intermittent Positive Pressure Ventilation. Acta Anaesthesiol. Scand. 1976, 20, 248–254. [Google Scholar] [CrossRef]
- Hedenstierna, G.; Tokics, L.; Reinius, H.; Rothen, H.U.; Östberg, E.; Öhrvik, J. Higher Age and Obesity Limit Atelectasis Formation During Anaesthesia: An Analysis of Computed Tomography Data in 243 Subjects. Br. J. Anaesth. 2020, 124, 336–344. [Google Scholar] [CrossRef]
- Williams, E.C.; Motta-Ribeiro, G.C.; Vidal Melo, M.F. Driving Pressure and Transpulmonary Pressure: How Do We Guide Safe Mechanical Ventilation? Anesthesiology 2019, 131, 155–163. [Google Scholar] [CrossRef]
- Loring, S.H.; Topulos, G.P.; Hubmayr, R.D. Transpulmonary Pressure: The Importance of Precise Definitions and Limiting Assumptions. Am. J. Respir. Crit. Care Med. 2016, 194, 1452–1457. [Google Scholar] [CrossRef]
- De Jong, A.; Wrigge, H.; Hedenstierna, G.; Gattinoni, L.; Chiumello, D.; Frat, J.-P.; Ball, L.; Schetz, M.; Pickkers, P.; Jaber, S. How to Ventilate Obese Patients in the Icu. Intensiv. Care Med. 2020, 46, 2423–2435. [Google Scholar] [CrossRef]
- Chi, Y.; Zhao, Z.; Frerichs, I.; Long, Y.; He, H. Prevalence and Prognosis of Respiratory Pendelluft Phenomenon in Mechanically Ventilated Icu Patients with Acute Respiratory Failure: A Retrospective Cohort Study. Ann. Intensiv. Care 2022, 12, 22. [Google Scholar] [CrossRef] [PubMed]
- Zhao, Z.; Steinmann, D.; Frerichs, I.; Guttmann, J.; Möller, K. Peep Titration Guided by Ventilation Homogeneity: A Feasibility Study Using Electrical Impedance Tomography. Crit. Care 2010, 14, R8. [Google Scholar] [CrossRef] [PubMed]
- Gibbs, K.W.; Semler, M.W.; Driver, B.E.; Seitz, K.P.; Stempek, S.B.; Taylor, C.; Resnick-Ault, D.; White, H.D.; Gandotra, S.; Doerschug, K.C.; et al. Noninvasive Ventilation for Preoxygenation during Emergency Intubation. N. Engl. J. Med. 2024, 390, 2165–2177. [Google Scholar] [CrossRef] [PubMed]



| Total | Study 1 | Study 2 | Study 3 | |
|---|---|---|---|---|
| Number of cases | 102 | 38 | 39 | 25 |
| Sex, female n (%) | 67 (65.7) | 26 (68.4) | 25 (64.1) | 16 (64.0) |
| Age [years] | 45 ± 12.6 | 45 ± 13.6 | 47 ± 11.4 | 44 ± 12.7 |
| Height [cm] | 171.0 ± 12.1 | 169.4 ± 13.2 | 172.2 ± 10.9 | 170.5 ± 10.5 |
| Weight [kg] | 147.4 ± 33.5 | 147.6 ± 45.2 | 152.8 ± 21.8 | 142.8 ± 31.4 |
| BMI [kg m−2] | 49.9 ± 8.9 | 50.0 ± 11.9 | 51.8 ± 8.0 | 48.3 ± 9.1 |
| Before Intubation Spontaneous Breathing | After Intubation Mechanical Ventilation | Before vs. After Intubation | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| t (min) | −5 | −4 | −3 | −2 | −1 | +1 | +2 | +3 | +4 | +5 | p-Value * |
| % VT non-dependent | |||||||||||
| n | 68 | 70 | 78 | 84 | 93 | 94 | 83 | 62 | 56 | 50 | <0.001 |
| median | 58.5 | 57.8 | 57.7 | 58.2 | 58.4 | 72.7 | 72.7 | 69.7 | 69.4 | 71.5 | |
| 95% CI | 55.9–61.0 | 54.7–60.5 | 53.8–60.8 | 54.9–60.9 | 55.4–60.3 | 68.7–75.8 | 68.1–76.1 | 67.8–75.3 | 67.0–75.7 | 66.9–79.1 | |
| GI Index | |||||||||||
| n | 67 | 69 | 81 | 91 | 99 | 94 | 78 | 54 | 43 | 36 | <0.001 |
| median | 50.6 | 49.2 | 49.7 | 49.1 | 49.1 | 72.6 | 72.7 | 69.8 | 69.6 | 70.0 | |
| 95% CI | 49.3–51.7 | 48.6–50.4 | 48.9–50.8 | 48.5–50.0 | 48.1–50.9 | 70.4–75.1 | 66.7–76.1 | 63.8–76.0 | 64.2–77.8 | 62.6– 76.7 | |
| Before Intubation Spontaneous Breathing | After Intubation Mechanical Ventilation | Δ | p-Value * | |
|---|---|---|---|---|
| median vVT (%) | 58.26 | 71.53 | +13.27% | <0.001 |
| 95% CI for vVT (%) | 57.02–59.39 | 69.66–73.88 | ||
| median GI Index | 49.37 | 71.36 | +21.99 | <0.001 |
| 95% CI for GI Index | 49.05–49.97 | 69.16–73.73 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nothofer, S.; Steckler, A.; Lange, M.; Héžeľ, A.; Dumps, C.; Wrigge, H.; Simon, P.; Girrbach, F. Electrical Impedance Tomography-Based Evaluation of Anesthesia-Induced Development of Atelectasis in Obese Patients. J. Clin. Med. 2024, 13, 7736. https://doi.org/10.3390/jcm13247736
Nothofer S, Steckler A, Lange M, Héžeľ A, Dumps C, Wrigge H, Simon P, Girrbach F. Electrical Impedance Tomography-Based Evaluation of Anesthesia-Induced Development of Atelectasis in Obese Patients. Journal of Clinical Medicine. 2024; 13(24):7736. https://doi.org/10.3390/jcm13247736
Chicago/Turabian StyleNothofer, Stefanie, Alexander Steckler, Mirko Lange, Anja Héžeľ, Christian Dumps, Hermann Wrigge, Philipp Simon, and Felix Girrbach. 2024. "Electrical Impedance Tomography-Based Evaluation of Anesthesia-Induced Development of Atelectasis in Obese Patients" Journal of Clinical Medicine 13, no. 24: 7736. https://doi.org/10.3390/jcm13247736
APA StyleNothofer, S., Steckler, A., Lange, M., Héžeľ, A., Dumps, C., Wrigge, H., Simon, P., & Girrbach, F. (2024). Electrical Impedance Tomography-Based Evaluation of Anesthesia-Induced Development of Atelectasis in Obese Patients. Journal of Clinical Medicine, 13(24), 7736. https://doi.org/10.3390/jcm13247736








