A Feasibility Study of a Controlled Standing Fulcrum Side-Bending Test in Adolescent Idiopathic Scoliosis
Abstract
:1. Introduction
2. Materials and Methods
2.1. Design of the Study
2.2. The CSFS Test—Controlled Quantitative Standing Fulcrum Side-Bending Test
2.3. Data Processing and Statistical Analysis
3. Results
The CSFS Test
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- He, C.; Wong, M.-S. Spinal Flexibility Assessment on the Patients With Adolescent Idiopathic Scoliosis: A Literature Review. Spine 2018, 43, E250–E258. [Google Scholar] [CrossRef]
- Wong, L.P.K.; Cheung, P.W.H.; Cheung, J.P.Y. Curve Type, Flexibility, Correction, and Rotation Are Predictors of Curve Progression in Patients with Adolescent Idiopathic Scoliosis Undergoing Conservative Treatment: A Systematic Review. Bone Joint J. 2022, 104-B, 424–432. [Google Scholar] [CrossRef] [PubMed]
- Luo, C.L.; Ma, C.Z.H.; Zou, Y.Y.; Zhang, L.S.; Wong, M.S. Associations between Spinal Flexibility and Bracing Outcomes in Adolescent Idiopathic Scoliosis: A Literature Review. J. Orthop. Surg. Res. 2023, 18, 955. [Google Scholar] [CrossRef] [PubMed]
- Cheung, J.P.Y.; Cheung, P.W.H. Supine Flexibility Predicts Curve Progression for Patients with Adolescent Idiopathic Scoliosis Undergoing Underarm Bracing. Bone Joint J. 2020, 102-B, 254–260. [Google Scholar] [CrossRef] [PubMed]
- Khodaei, M.; Pachêco-Pereira, C.; Trac, S.; Chan, A.; Le, L.H.; Lou, E. Radiographic Methods to Estimate Surgical Outcomes Based on Spinal Flexibility Assessment in Patients Who Have Adolescent Idiopathic Scoliosis: A Systematic Review. Spine J. 2018, 18, 2128–2139. [Google Scholar] [CrossRef] [PubMed]
- Büchler, P.; de Oliveria, M.E.; Studer, D.; Schumann, S.; Zheng, G.; Schneider, J.; Hasler, C.C. Axial Suspension Test to Assess Pre-Operative Spinal Flexibility in Patients with Adolescent Idiopathic Scoliosis. Eur. Spine J. 2014, 23, 2619–2625. [Google Scholar] [CrossRef] [PubMed]
- Berger, S.; de Oliveira, M.; Schuman, S.; Schneider, J.; Studer, D.; Hasler, C.; Zheng, G.; Büchler, P. Patient-Specific Spinal Stiffness in AIS: A Preoperative and Noninvasive Method. Eur. Spine J. 2015, 24, 249–255. [Google Scholar] [CrossRef] [PubMed]
- Negrini, S.; Donzelli, S.; Aulisa, A.G.; Czaprowski, D.; Schreiber, S.; de Mauroy, J.C.; Diers, H.; Grivas, T.B.; Knott, P.; Kotwicki, T.; et al. 2016 SOSORT Guidelines: Orthopaedic and Rehabilitation Treatment of Idiopathic Scoliosis during Growth. Scoliosis Spinal Disord. 2018, 13, 3. [Google Scholar] [CrossRef] [PubMed]
- Wong, C.; Adriansen, J.; Jeppsen, J.; Balslev-Clausen, A. Intervariability in Radiographic Parameters and General Evaluation of a Low-Dose Fluoroscopic Technique in Patients with Idiopathic Scoliosis. Acta Radiol. Open 2021, 10, 20584601211043256. [Google Scholar] [CrossRef] [PubMed]
- KERN & SOHN GmbH KERN FH500. Universelles Digitales Kraftmessgerät Für Zug- Und Druckkraftmessungen Mit RS-232 Schnittstelle. Available online: https://docs.rs-online.com/e1e1/0900766b816836cc.pdf (accessed on 14 March 2023).
- Cheung, J.P.Y.; Yiu, K.K.L.; Vidyadhara, S.; Chan, P.P.Y.; Cheung, P.W.H.; Mak, K.C. Predictability of Supine Radiographs for Determining In-Brace Correction for Adolescent Idiopathic Scoliosis. Spine 2018, 43, 971–976. [Google Scholar] [CrossRef] [PubMed]
- Cheung, J.P.Y.; Cheung, P.W.H.; Yeng, W.C.; Chan, L.C.K. Does Curve Regression Occur During Underarm Bracing in Patients with Adolescent Idiopathic Scoliosis? Clin. Orthop. Relat. Res. 2020, 478, 334–345. [Google Scholar] [CrossRef] [PubMed]
- Lyder, C.H. Pressure Ulcer Prevention and Management. JAMA 2003, 289, 223–226. [Google Scholar] [CrossRef] [PubMed]
- Fairhurst, H.; Little, J.P.; Adam, C.J. Intra-Operative Measurement of Applied Forces during Anterior Scoliosis Correction. Clin. Biomech. 2016, 40, 68–73. [Google Scholar] [CrossRef] [PubMed]
- Koutras, C.; Pérez, J.; Kardash, K.; Otaduy, M.A. A Study of the Sensitivity of Biomechanical Models of the Spine for Scoliosis Brace Design. Comput. Methods Programs Biomed. 2021, 207, 106125. [Google Scholar] [CrossRef] [PubMed]
- Lamarre, M.-E.; Parent, S.; Labelle, H.; Aubin, C.-E.; Joncas, J.; Cabral, A.; Petit, Y. Assessment of Spinal Flexibility in Adolescent Idiopathic Scoliosis: Suspension versus Side-Bending Radiography. Spine 2009, 34, 591–597. [Google Scholar] [CrossRef] [PubMed]
- Koutras, C.; Shayestehpour, H.; Pérez, J.; Wong, C.; Rasmussen, J.; Tournier, M.; Nesme, M.; Otaduy, M.A. Biomechanical Morphing for Personalized Fitting of Scoliotic Torso Skeleton Models. Front. Bioeng. Biotechnol. 2022, 10, 945461. [Google Scholar] [CrossRef] [PubMed]
- Lafon, Y.; Lafage, V.; Steib, J.-P.; Dubousset, J.; Skalli, W. In Vivo Distribution of Spinal Intervertebral Stiffness Based on Clinical Flexibility Tests. Spine 2010, 35, 186–193. [Google Scholar] [CrossRef] [PubMed]
- Little, J.P.; Adam, C.J. Effects of Surgical Joint Destabilization on Load Sharing between Ligamentous Structures in the Thoracic Spine: A Finite Element Investigation. Clin. Biomech. 2011, 26, 895–903. [Google Scholar] [CrossRef] [PubMed]
- Little, J.P.; Adam, C.J. The Effect of Soft Tissue Properties on Spinal Flexibility in Scoliosis: Biomechanical Simulation of Fulcrum Bending. Spine 2009, 34, E76–E82. [Google Scholar] [CrossRef] [PubMed]
- Langensiepen, S.; Semler, O.; Sobottke, R.; Fricke, O.; Franklin, J.; Schönau, E.; Eysel, P. Measuring Procedures to Determine the Cobb Angle in Idiopathic Scoliosis: A Systematic Review. Eur. Spine J. 2013, 22, 2360–2371. [Google Scholar] [CrossRef] [PubMed]


| Pt Number | Initial Cobb’s Angle | Curve Type | MRI | Cobb’s Angle at Evaluation | Age at Examination (Years) | Time Diagnosis to Evaluation (Months) | End Evaluation |
|---|---|---|---|---|---|---|---|
| 2 | 11.00 | sin TL konx | - | 24.00 | 12.43 | 71.97 | 1 |
| 4 | 7.00 | T dex konc | - | 17.00 | 13.04 | 56.48 | 0 |
| 7 | 26.00 | S dex TL | Ia | 21.00 | 18.68 | 12.59 | 0 |
| 15 | 4.00 | S dex konx | arkolyse l5 | 13.00 | 15.64 | 49.22 | 0 |
| 17 | 10.00 | high T sin konx | - | 3.00 | 11.81 | 12.99 | 0 |
| 24 | 0.00 | - | 0.00 | 12.04 | −10.65 | 0 | |
| 30 | 12.00 | high T dex konx | Ia | 8.00 | 14.34 | 30.35 | 0 |
| 31 | 11.00 | L sin konx | - | 11.00 | 15.31 | 0.00 | 0 |
| 33 | 14.00 | short TL sin | - | 8.00 | 9.77 | 84.23 | 0 |
| 34 | 11.00 | L sin konx | - | 14.00 | 14.65 | 63.06 | 0 |
| 35 | 18.00 | high T dex | - | 10.00 | 11.73 | 3.81 | 0 |
| 36 | 10.00 | high T dex | - | 10.00 | 13.61 | 6.02 | 0 |
| 37 | 10.00 | L sin konx | Ia | 10.00 | 12.21 | 28.54 | 0 |
| 38 | 13.00 | L sin konx | - | 11.00 | 15.05 | 46.22 | 0 |
| 39 | 11.00 | TL dex konc | - | 10.00 | 9.52 | 23.80 | 0 |
| 40 | 18.00 | L dex konx | Ia | 26.00 | 16.19 | 4.77 | 0 |
| 41 | 18.00 | S T dex | Ia | 20.00 | 9.67 | 5.75 | 1 |
| 42 | 10.00 | C TL dex | - | 10.00 | 12.88 | 7.66 | 0 |
| 43 | 10.00 | L dex konx | 15.00 | 14.76 | 18.94 | 0 | |
| 44 | 7.00 | L sin konx | 5.00 | 10.21 | 26.27 | 0 | |
| 45 | 16.00 | C TL | 4.10 | 14.81 | 18.71 | 0 |
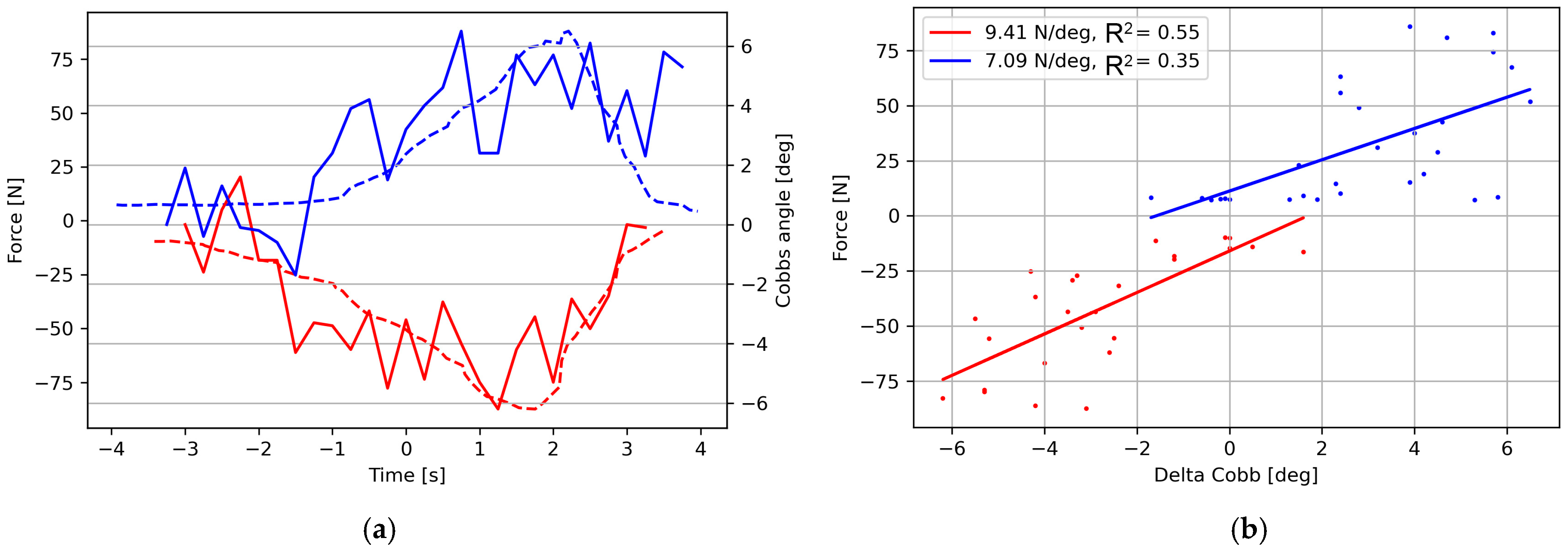
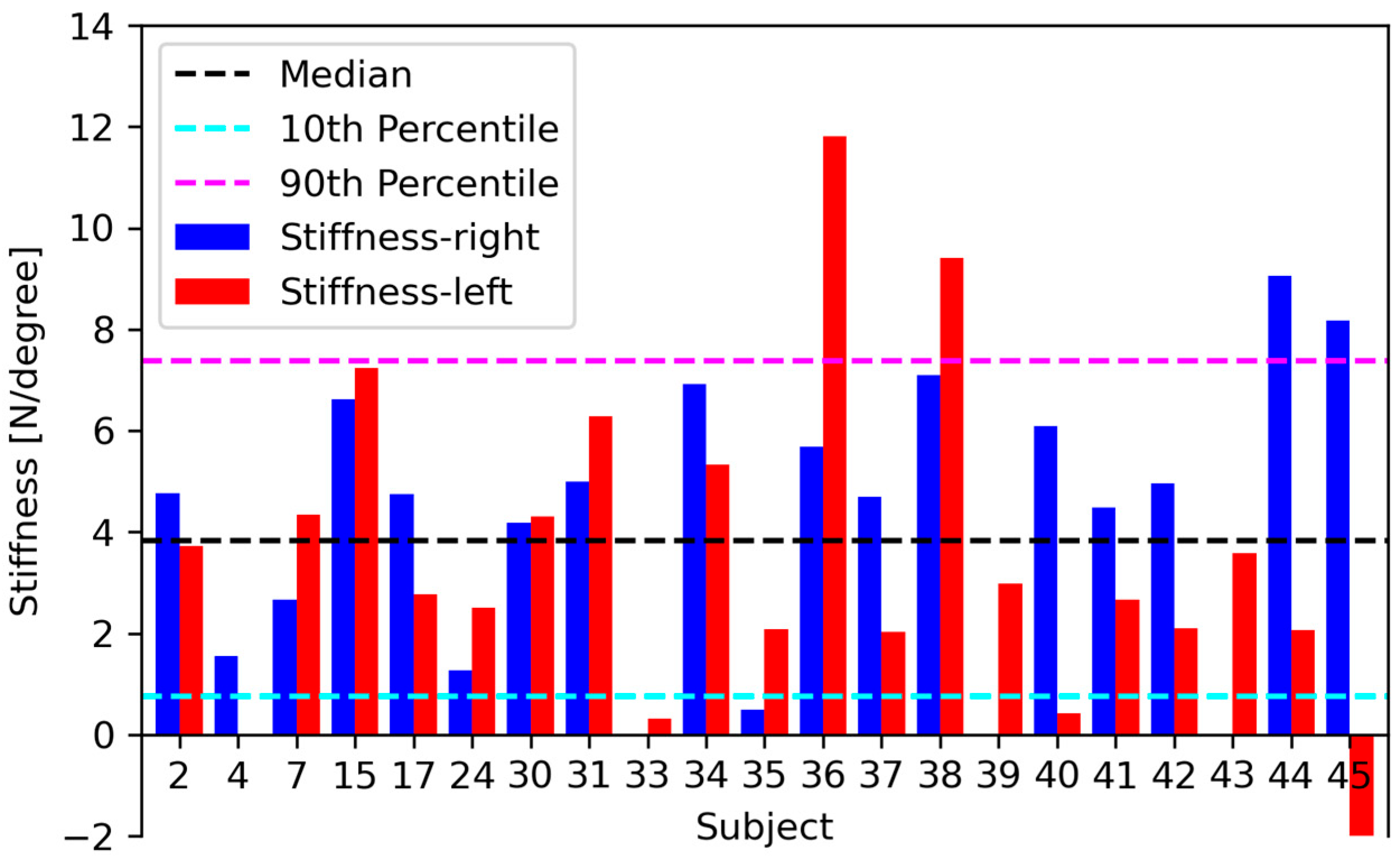
| Subject | Stiffness-Right | Stiffness-Left | R2-Right | R2-Left | Force Max |
|---|---|---|---|---|---|
| 2 | 4.77 | 3.73 | 0.91 | 0.60 | 101.89 |
| 4 | 2.66 | 4.34 | 0.60 | 0.68 | 73.58 |
| 7 | 6.62 | 7.23 | 0.67 | 0.76 | 90.01 |
| 15 | 4.74 | 2.77 | 0.90 | 0.56 | 11.28 |
| 17 | 1.28 | 2.50 | 0.18 | 0.48 | - |
| 24 | 4.18 | 4.31 | 0.37 | 0.75 | 33.93 |
| 30 | 5.00 | 6.29 | 0.56 | 0.55 | 62.08 |
| 31 | 6.91 | 5.33 | 0.76 | 0.69 | 85.72 |
| 33 | 0.49 | 2.09 | 0.10 | 0.51 | 12.89 |
| 34 | 5.69 | 11.81 | 0.55 | 0.61 | 87.50 |
| 35 | 4.69 | 2.02 | 0.52 | 0.14 | 33.52 |
| 36 | 7.09 | 9.41 | 0.59 | 0.74 | 90.75 |
| 37 | 6.08 | 0.41 | 0.57 | 0.04 | 84.43 |
| 38 | 4.49 | 2.67 | 0.71 | 0.26 | 71.58 |
| 39 | 4.95 | 2.10 | 0.86 | 0.54 | 35.25 |
| 40 | 0.02 | 3.58 | 0.00 | 0.85 | 27.03 |
| 41 | 9.06 | 2.06 | 0.82 | 0.65 | 27.79 |
| 42 | 8.17 | −2.12 | 0.42 | −0.22 | 12.40 |
| Stiffness | Stiffness-Right | Stiffness-Left | R-Right | R-Left | Force Max Left | Diff Cobbs Left | Force Max Right | Diff Cobbs Right | |
|---|---|---|---|---|---|---|---|---|---|
| Median | 4.37 | 4.86 | 3.18 | 0.58 | 0.58 | 75.60 | 18.50 | 74.20 | 14.10 |
| 25 Percentile | 2.20 | 3.80 | 2.08 | 0.41 | 0.42 | 55.20 | 12.70 | 56.60 | 8.25 |
| 75 Percentile | 6.24 | 3.80 | 2.08 | 0.78 | 0.70 | 101.10 | 21.65 | 88.00 | 23.55 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wong, C.; Koutras, C.; Shayestehpour, H.; Dahl, B.; Otaduya, M.A.; Rasmussen, J. A Feasibility Study of a Controlled Standing Fulcrum Side-Bending Test in Adolescent Idiopathic Scoliosis. J. Clin. Med. 2024, 13, 7809. https://doi.org/10.3390/jcm13247809
Wong C, Koutras C, Shayestehpour H, Dahl B, Otaduya MA, Rasmussen J. A Feasibility Study of a Controlled Standing Fulcrum Side-Bending Test in Adolescent Idiopathic Scoliosis. Journal of Clinical Medicine. 2024; 13(24):7809. https://doi.org/10.3390/jcm13247809
Chicago/Turabian StyleWong, Christian, Christos Koutras, Hamed Shayestehpour, Benny Dahl, Miguel A. Otaduya, and John Rasmussen. 2024. "A Feasibility Study of a Controlled Standing Fulcrum Side-Bending Test in Adolescent Idiopathic Scoliosis" Journal of Clinical Medicine 13, no. 24: 7809. https://doi.org/10.3390/jcm13247809
APA StyleWong, C., Koutras, C., Shayestehpour, H., Dahl, B., Otaduya, M. A., & Rasmussen, J. (2024). A Feasibility Study of a Controlled Standing Fulcrum Side-Bending Test in Adolescent Idiopathic Scoliosis. Journal of Clinical Medicine, 13(24), 7809. https://doi.org/10.3390/jcm13247809







