Digital Twins Use in Plastic Surgery: A Systematic Review
Abstract
1. Introduction
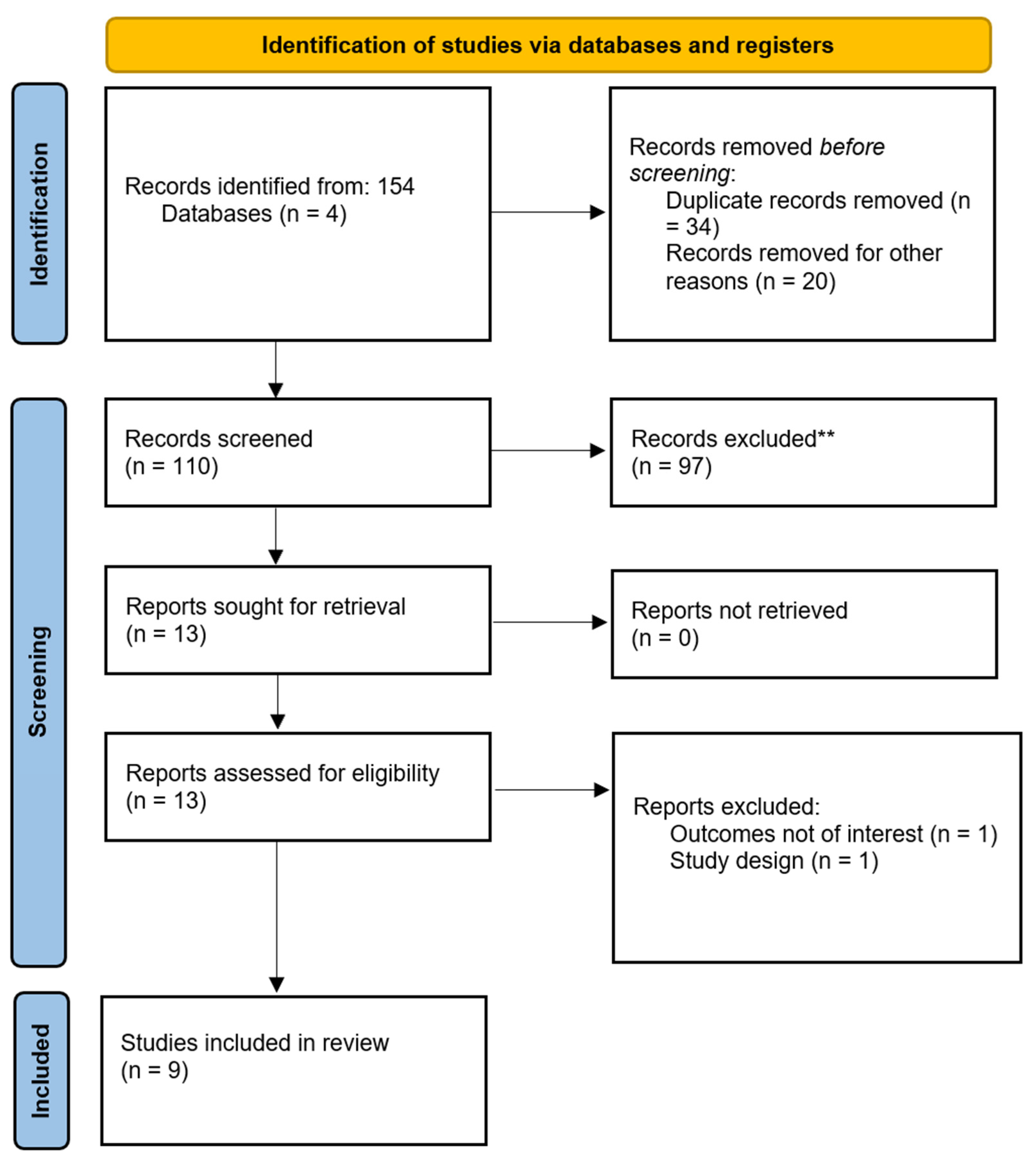
2. Materials and Methods
2.1. Search Strategy
- (“digital twin” OR “virtual twin” OR “cyber-physical system” OR “computational model”);
- AND (“plastic surgery” OR “reconstructive surgery” OR “cosmetic surgery” OR “aesthetic surgery” OR “maxillofacial surgery” OR “faciomaxillary surgery”);
- AND (“simulation” OR “virtual model” OR “personalised surgery”).
2.2. Inclusion Criteria
- Study Type: Original research articles, randomised controlled trials, systematic reviews, clinical trials, cohort studies, and case series studies that describe the application of digital twin technology in plastic surgery. Both experimental and observational studies were considered.
- Participants: Studies involving human subjects undergoing plastic, reconstructive, or cosmetic surgery where digital twin technology was used for preoperative planning, intraoperative decision-making, or postoperative follow-up.
- Outcomes: Studies on clinical outcomes, patient satisfaction, surgical accuracy, complication rates, or cost-effectiveness associated with using digital twins in plastic surgery.
- Technological Focus: Studies that explicitly mention using digital twins or comparable virtual models that simulate surgical procedures or predict outcomes in plastic surgery.
- Language: Only studies published in English were considered.
2.3. Exclusion Criteria
- Study Type: Editorials, commentaries, and conference abstracts were excluded unless they provided data from original research. Non-peer-reviewed articles were also excluded.
- Technological Scope: Studies focusing on general simulation technologies without the specific use of digital twins, such as virtual reality or generic 3D modelling without real-time feedback mechanisms, were excluded.
- Surgical Specialty: Studies focusing on other surgical fields outside plastic surgery, such as general, orthopaedic, or neurological surgery, were only allowed if the technology discussed directly applied to plastic surgery.
- Duplicate Studies: Duplicate publications of the same study were excluded, although the most complete version of the study was included if data were presented in multiple papers.
2.4. Data Extraction
- Study Characteristics: Author(s), year of publication, study design, and country of origin.
- Participants: Number of participants, demographic information (e.g., age, gender), and the specific type of plastic surgery performed (e.g., breast reconstruction, facial surgery, limb reconstruction).
- Digital Twin Technology: Description of the digital twin model used, including the type of software, hardware, data inputs (e.g., imaging, biomechanical data), and whether real-time feedback was incorporated.
- Clinical Application: The stage of the surgical process where the digital twin was utilised (e.g., preoperative planning, intraoperative decision-making, postoperative monitoring).
- Outcomes: The primary and secondary outcomes reported in each study, such as surgical precision, complication rates, patient satisfaction, length of hospital stay, and cost-effectiveness.
- Study Limitations: The authors acknowledge limitations, such as small sample sizes, short follow-up periods, or technical challenges in implementing digital twin models.
2.5. Data Synthesis, Analysis, and Risk of Bias (Quality) Assessment
3. Results
3.1. Study Characteristics
3.2. Clinical Outcomes
- Surgical Precision: Multiple studies reported improvements in surgical precision through the use of digital twins. For example, Bosc et al. observed sub-millimetre accuracy in maxillofacial procedures when incorporating AR, and Alkhayer et al. reported maxillary and mandibular positioning errors within a 2 mm range for orthognathic surgeries. As highlighted by Ayoub and Pulijala (2019) [17], the use of virtual reality in maxillofacial surgery further supports the role of digital twin applications in achieving improved precision.
- Patient Satisfaction and Outcomes: Patient satisfaction was consistently enhanced across studies that employed patient-specific surgical planning, as seen in rhinoplasty cases reported by Sobral et al. (2021) and Arias Gallo et al. (2023) [18,19]. Sobral et al. noted high patient satisfaction with improved aesthetic outcomes using accessible software tools for 3D virtual planning, while Arias Gallo et al. highlighted the utility of patient-specific surgical guides in improving alignment with preoperative goals.
- Reduced Complication Rates: The systematic review and meta-analysis by Ohkuma et al. (2014) on breast reconstruction surgery provided quantitative evidence of reduced complication rates with the integration of computed tomographic angiography in preoperative planning, leading to a 13% decrease in flap-related complications and improved donor-site outcomes [20].
3.3. Limitations
3.4. Risk of Bias
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Negri, E.; Fumagalli, L.; Macchi, M. A review of the roles of Digital Twin in CPS-based production systems. Procedia Manuf. 2017, 11, 9. [Google Scholar] [CrossRef]
- Björnsson, B.; Borrebaeck, C.; Elander, N.; Gasslander, T.; Gawel, D.R.; Gustafsson, M.; Jörnsten, R.; Lee, E.J.; Li, X.; Lilja, S.; et al. Digital twins to personalize medicine. Genome Med. 2019, 12, 4. [Google Scholar] [CrossRef]
- Douthwaite, J.A.; Lesage, B.; Gleirscher, M.; Calinescu, R.; Aitken, J.M.; Alexander, R.; Law, J. A Modular Digital Twinning Framework for Safety Assurance of Collaborative Robotics. Front. Robot. AI 2021, 8, 758099. [Google Scholar] [CrossRef] [PubMed]
- Xie, Y.; Seth, I.; Hunter-Smith, D.J.; Rozen, W.M.; Ross, R.; Lee, M. Aesthetic surgery advice and counseling from artificial intelligence: A rhinoplasty consultation with ChatGPT. Aesthetic Plast. Surg. 2023, 47, 1985–1993. [Google Scholar] [CrossRef]
- Grieves, M.W. Product lifecycle management: The new paradigm for enterprises. Int. J. Prod. 2005, 2, 71–84. [Google Scholar] [CrossRef]
- Glaessgen, E.S.D. The Digital Twin Paradigm for Future NASA and U.S. Air Force Vehicles. In Proceedings of the 53rd AIAA/ASME/ASCE/AHS/ASC Structures, Structural Dynamics and Materials Conference, Honolulu, HI, USA, 23–26 April 2012. [Google Scholar]
- Sahal, R.; Alsamhi, S.H.; Brown, K.N. Personal Digital Twin: A Close Look into the Present and a Step towards the Future of Personalised Healthcare Industry. Sensors 2022, 22, 5918. [Google Scholar] [CrossRef] [PubMed]
- Seth, I.; Xie, Y.; Rodwell, A.; Gracias, D.; Bulloch, G.; Hunter-Smith, D.J.; Rozen, W.M. Exploring the role of a large language model on carpal tunnel syndrome management: An observation study of ChatGPT. J. Hand Surg. 2023, 48, 1025–1033. [Google Scholar] [CrossRef]
- Croatti, A.; Gabellini, M.; Montagna, S.; Ricci, A. On the Integration of Agents and Digital Twins in Healthcare. J. Med. Syst. 2020, 44, 161. [Google Scholar] [CrossRef]
- Venkatesh, K.P.; Raza, M.M.; Kvedar, J.C. Health digital twins as tools for precision medicine: Considerations for computation, implementation, and regulation. NPJ Digit. Med. 2022, 5, 150. [Google Scholar] [CrossRef] [PubMed]
- Fagherazzi, G. Deep Digital Phenotyping and Digital Twins for Precision Health: Time to Dig Deeper. J. Med. Internet Res. 2020, 22, e16770. [Google Scholar] [CrossRef]
- Bosc, R.; Fitoussi, A.; Hersant, B.; Dao, T.H.; Meningaud, J.P. Intraoperative augmented reality with heads-up displays in maxillofacial surgery: A systematic review of the literature and a classification of relevant technologies. Int. J. Oral Maxillofac. Surg. 2019, 48, 132–139. [Google Scholar] [CrossRef] [PubMed]
- Elnagar, M.H.; Gajendrareddy, P.; Lee, M.K.; Allareddy, V. Artificial Intelligence and Orthodontic Practice: The Future Unveiled. In Integrated Clinical Orthodontics; Wiley: Hoboken, NJ, USA, 2023; pp. 565–575. [Google Scholar]
- Longeac, M.; Depeyre, A.; Pereira, B.; Barthelemy, I.; Dang, N.P. Virtual surgical planning and three-dimensional printing for the treatment of comminuted zygomaticomaxillary complex fracture. J. Stomatol. Oral Maxillofac. Surg. 2021, 122, 386–390. [Google Scholar] [CrossRef] [PubMed]
- Alkhayer, A.; Piffkó, J.; Lippold, C.; Segatto, E. Accuracy of virtual planning in orthognathic surgery: A systematic review. Head Face Med. 2020, 16, 1–9. [Google Scholar] [CrossRef]
- Dubron, K.; Verbist, M.; Jacobs, R.; Olszewski, R.; Shaheen, E.; Willaert, R. Augmented and virtual reality for preoperative trauma planning, focusing on orbital reconstructions: A systematic review. J. Clin. Med. 2023, 12, 5203. [Google Scholar] [CrossRef] [PubMed]
- Ayoub, A.; Pulijala, Y. The application of virtual reality and augmented reality in Oral & Maxillofacial Surgery. BMC Oral Health 2019, 19, 1–8. [Google Scholar]
- Sobral, D.S.; Duarte, D.W.; Dornelles, R.F.; Moraes, C.A. 3D virtual planning for rhinoplasty using a free add-on for open-source software. Aesthetic Surg. J. 2021, 41, NP1024–NP1032. [Google Scholar] [CrossRef]
- Gallo, J.A.; Gallego-Albertos, C.S.; Pons, M.C. Patient-specific profile guide in rhinoplasty. J. Plast. Reconstr. Aesthetic Surg. 2023, 84, 549–555. [Google Scholar] [CrossRef] [PubMed]
- Ohkuma, R.; Mohan, R.; Broyles, J.; Yamazaki, M.; Schneider, E.; Rosson, G.D. Abdominal Based Free Flap Planning in Breast Reconstruction with CT Angiography-Systematic Review and Meta-Analysis. Plast. Reconstr. Surg. 2012, 130, 63. [Google Scholar] [CrossRef]
- Seth, I.; Kenney, P.S.; Bulloch, G.; Hunter-Smith, D.J.; Thomsen, J.B.; Rozen, W.M. Artificial or augmented authorship? A conversation with a chatbot on base of thumb arthritis. Plast. Reconstr. Surg.–Glob. Open 2023, 11, e4999. [Google Scholar] [CrossRef] [PubMed]
- Sun, T.; He, X.; Li, Z. Digital twin in healthcare: Recent updates and challenges. Digit. Health 2023, 9, 20552076221149651. [Google Scholar] [CrossRef]
- Lexma. Project Breath Easy Lexma Digital Twin Lung. 2023. Available online: https://projectbreatheasy.org/ (accessed on 24 October 2024).
- Baillargeon, B.; Rebelo, N.; Fox, D.D.; Taylor, R.L.; Kuhl, E. The Living Heart Project: A robust and integrative simulator for human heart function. Eur. J. Mech. A Solids 2014, 48, 38–47. [Google Scholar] [CrossRef] [PubMed]
- Fisher, C.K.; Smith, A.M.; Walsh, J.R. Machine learning for comprehensive forecasting of Alzheimer’s Disease progression. Sci. Rep. 2019, 9, 13622. [Google Scholar] [CrossRef] [PubMed]
- Kamel Boulos, M.N.; Zhang, P. Digital Twins: From Personalised Medicine to Precision Public Health. J. Pers. Med. 2021, 11, 745. [Google Scholar] [CrossRef] [PubMed]
- Angulo, C.; Gonzalez-Abril, L.; Raya, C.; Ortega, J.A. A proposal to evolving towards digital twins in healthcare. In Proceedings of the International Work-Conference on Bioinformatics and Biomedical Engineering, Granada, Spain, 6–8 May 2020; pp. 418–427. [Google Scholar]
- Elkefi, S.; Asan, O. Digital Twins for Managing Health Care Systems: Rapid Literature Review. J. Med. Internet Res. 2022, 24, e37641. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.; Lin, Z.; Yuan, Y. A Novel Cloud-Based Framework for the Elderly Healthcare Services Using Digital Twin. IEEE Access 2019, 7, 49088–49101. [Google Scholar] [CrossRef]
- Wickramasinghe, N.; Ulapane, N.; Andargoli, A.; Ossai, C.; Shuakat, N.; Nguyen, T.; Zelcer, J. Digital twins to enable better precision and personalized dementia care. JAMIA Open 2022, 5, ooac072. [Google Scholar] [CrossRef]
- Diaz, R.G.; Fedwa, L.; El Saddik, A. DTCoach: Your Digital Twin Coach on the Edge During COVID-19 and Beyond. IEEE Instrum. Meas. Mag. 2021, 24, 22–28. [Google Scholar] [CrossRef]
- Tröbinger, M.; Costinescu, A.; Xing, H.; Elsner, J.; Hu, T.; Naceri, A.; Figueredo, L.; Jensen, E.; Burschka, D.; Haddadin, S. A dual docto-patient twin paradigm for transparent remote examination, diagnosis, and rehabilitation. In Proceedings of the IEEE/RSJ International Conference on Intelligent Robots and Systems (IROS), Prague, Czech Republic, 27 September–1 October 2021; pp. 2933–2940. [Google Scholar]
- Merkel, M.J.; Edwards, R.; Ness, J.; Eriksson, C.; Yoder, S.; Gilliam, S.; Ellero, K.; Barreto-Costa, C.; Graven, P.; Terry, J.R.; et al. Statewide Real-Time Tracking of Beds and Ventilators During Coronavirus Disease 2019 and Beyond. Crit. Care Explor. 2020, 2, e0142. [Google Scholar] [CrossRef]
- Collins, B.E. Reducing Hospital Harm: Establishing a Command Centre to Foster Situational Awareness. Health Q. 2022, 25, 75–81. [Google Scholar] [CrossRef] [PubMed]
- Sun, T.; He, X.; Song, X.; Shu, L.; Li, Z. The Digital Twin in Medicine: A Key to the Future of Healthcare? Front. Med. 2022, 9, 907066. [Google Scholar] [CrossRef] [PubMed]
| Author | Year | Study Design | Surgical Area | Technological Focus | Outcomes Reported | Limitations | Country |
|---|---|---|---|---|---|---|---|
| Bosc et al. [12] | 2019 | Systematic Review | Maxillofacial Surgery | Augmented reality (AR) in surgery | High precision (<1 mm error) | Limited to AR, small number of studies | France |
| Elnagar et al. [13] | 2020 | Descriptive Overview | Orthodontics and Orthognathic Surgery | Digital workflow for surgical planning | Improved surgical precision | Descriptive, not a clinical trial | USA |
| Longeac et al. [14] | 2016 | Original Research | Craniofacial Surgery | Digital simulation in surgical education | Improved skill acquisition | Limited by small sample size | USA |
| Alkhayer et al. [15] | 2020 | Systematic Review | Orthognathic Surgery | Virtual surgical planning | 2 mm maxillary/mandibular accuracy | No cost analysis | Germany |
| Dubron et al. [16] | 2023 | Systematic Review | Orbital Reconstructions | AR in preoperative planning | Accurate placement of implants | 2–3 mm higher error rates than traditional methods | Belgium |
| Ayoub and Pulijala [17] | 2019 | Descriptive Overview | Oral and Maxillofacial Surgery | Virtual reality (VR) in maxillofacial surgery | Improved accuracy in surgery | No patient outcome data | UK |
| Sobral et al. [18] | 2021 | Case Series | Rhinoplasty | 3D virtual planning with Blender | Enhanced surgical precision, high patient satisfaction | Small sample size, no control group | Brazil |
| Arias Gallo et al. [19] | 2023 | Methodological Study | Rhinoplasty | Patient-specific surgical guides | Improved surgical outcomes with patient-specific guides | Small sample size, no long-term data | Spain |
| Ohkuma et al. [20] | 2014 | Systematic Review and Meta-Analysis | Breast Reconstruction | Virtual surgical planning using computed tomographic angiography (CTA) | Reduced flap-related complications, reduced donor-site morbidity, shorter operative times | Predominantly observational studies, generalizability affected by variability in techniques | Japan |
| Author | Year | Study Design | Surgical Area | Quality Assessment Tool | Risk of Bias | Key Concerns |
| Bosc et al. [12] | 2019 | Systematic Review | Maxillofacial Surgery | AMSTAR 2 | Moderate to High | Limited number of studies; inconsistent data across included studies; potential publication bias. |
| Elnagar et al. [13] | 2020 | Descriptive Overview | Orthodontics and Orthognathic Surgery | JBI | High | The descriptive nature limits generalizability, lacks control or comparison groups, and creates a risk of reporting bias. |
| Longeac et al. [14] | 2016 | Original Research | Craniofacial Surgery | Newcastle–Ottawa Scale (NOS) | Moderate | Small sample size; limited follow-up; risk of selection bias due to single-centre study. |
| Alkhayer et al. [15] | 2020 | Systematic Review | Orthognathic Surgery | AMSTAR 2 | Moderate | No cost analysis; variability in outcomes and measurement methods; potential for selection bias. |
| Dubron et al. [16] | 2023 | Systematic Review | Orbital Reconstructions | AMSTAR 2 | Moderate | Variation in methods and equipment among studies; lack of patient-centred outcomes; moderate risk of bias due to inconsistent methodologies. |
| Ayoub and Pulijala [17] | 2019 | Descriptive Overview | Oral and Maxillofacial Surgery | JBI | High | No outcome data; lack of patient perspective; high potential for reporting and selection bias. |
| Sobral et al. [18] | 2021 | Case Series | Rhinoplasty | JBI | High | Small sample, no control group; high potential for selection and reporting bias due to lack of comparator or standardisation. |
| Arias Gallo et al. [19] | 2023 | Methodological Study | Rhinoplasty | Newcastle–Ottawa Scale (NOS) | Moderate | Small sample, no long-term data; risk of selection bias, limited scope and standardisation across methodology. |
| Ohkuma et al. [20] | 2014 | Systematic Review and Meta-Analysis | Breast Reconstruction | AMSTAR 2 | Low to Moderate | Heterogeneity in study designs; lack of control over surgical techniques; overall high quality but limited by observational data nature. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Seth, I.; Lim, B.; Lu, P.Y.J.; Xie, Y.; Cuomo, R.; Ng, S.K.-H.; Rozen, W.M.; Sofiadellis, F. Digital Twins Use in Plastic Surgery: A Systematic Review. J. Clin. Med. 2024, 13, 7861. https://doi.org/10.3390/jcm13247861
Seth I, Lim B, Lu PYJ, Xie Y, Cuomo R, Ng SK-H, Rozen WM, Sofiadellis F. Digital Twins Use in Plastic Surgery: A Systematic Review. Journal of Clinical Medicine. 2024; 13(24):7861. https://doi.org/10.3390/jcm13247861
Chicago/Turabian StyleSeth, Ishith, Bryan Lim, Phil Y. J. Lu, Yi Xie, Roberto Cuomo, Sally Kiu-Huen Ng, Warren M. Rozen, and Foti Sofiadellis. 2024. "Digital Twins Use in Plastic Surgery: A Systematic Review" Journal of Clinical Medicine 13, no. 24: 7861. https://doi.org/10.3390/jcm13247861
APA StyleSeth, I., Lim, B., Lu, P. Y. J., Xie, Y., Cuomo, R., Ng, S. K.-H., Rozen, W. M., & Sofiadellis, F. (2024). Digital Twins Use in Plastic Surgery: A Systematic Review. Journal of Clinical Medicine, 13(24), 7861. https://doi.org/10.3390/jcm13247861









