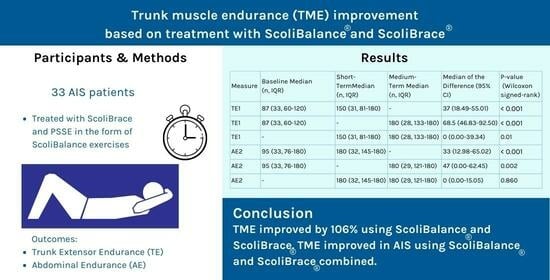
The Improvement of Trunk Muscle Endurance in Adolescents with Idiopathic Scoliosis Treated with ScoliBrace® and the ScoliBalance® Exercise Approach
Abstract
:1. Introduction
2. Materials and Methods
2.1. Sample
2.2. Inclusion and Exclusion Criteria
2.3. Data Collection and Outcome Measures
2.4. Analysis
3. Results
3.1. Initial Description of the Dataset
3.2. Comparing TE and AE between Timepoints
3.2.1. TE and AE including All Cases (Including Those Patients Who Achieved the Maximum of 180 s)
3.2.2. TE and AE (Not including Patients Who Achieved the Maximum of 180 s)
3.3. Number and Proportion of Those Who Reached 180 s
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A. ScoliBalance® Exercise Approach as a Physiotherapeutic Scoliosis-Specific Exercise (PSSE) Program for Adolescent Idiopathic Scoliosis (AIS)
Appendix A.1. The Concept
Appendix A.2. Description of the ScoliBalance® Program
- The curve classification was determined using a simple classification system, i.e., lumbar, thoracolumbar, thoracic, and double curve (primary thoracic, primary lumbar, or balanced).
- The patient was prescribed a ScoliCorrection using multiple steps to create the corrective movements (Figure A1). This commenced in a sitting posture, whereby the patient was taught the steps of the ScoliCorrection with the aim of achieving 3D autocorrection. For single curves, the patient was prescribed a ScoliCorrection based on the curve classification and involved over-correction, mirror image®, and corrective breathing for posture correction [11,13,15,53]. The aim was to harness the biomechanical principles of spinal coupling through movement (Figure A2) where possible. Where overcorrection was not possible, e.g., due to large amounts of deformity, then the patient was instructed to focus more on achieving a ScoliCorrection in a neutral posture.
- The patient was also given an orthotic (ScoliRoll®)device (Figure A3) to use once per day at home for 25 min, starting with 2 min on Day 1 and progressing to 25 min over 1–2 weeks.
- The patient was then prescribed exercises to stabilize the corrected posture through ScoliExcercises and integration into activities of daily living, e.g., sit to stand. Progression over time is from a seated to standing position, which is later challenged by exercises in the corrected position (Figure A4).
- Patient education was provided verbally to the patient at every session so that each day the patient was left able to independently complete the required exercises and integration into ADLs.
- Each patient was prescribed 20–25 min of exercise daily. This incorporated an individualized approach, whereby each patient was prescribed a series of repetitions and sets of each exercise relevant to their curve type. The exercises were prescribed in a sitting position and progressed to standing by about week 5.
- Each patient attended the clinic weekly and was asked to perform their home exercise program daily.
- Compliance was monitored verbally at each weekly session. The program was progressed based on individual capacity and performance rather than a one-size-fits-all approach.




| Session 1 | Session 2 | Session 3 | Session 4 | Session 5 | Session 6 | Sessions 7–9 | Session 10+ |
|---|---|---|---|---|---|---|---|
| Teach the appropriate ScoliCorrection step by step | Double arm raise (DA raise) | Seated bicep curl (BC) | Seated BC and shoulder press (SP) | Forward lean shoulder press | Standing Bicep curl | Standing BC Shoulder Press | Bent over row |
| Based on patient’s needs, goals, and clinical presentation | Seated ball toss | Seated T-row | Seated T to Y row | Lateral raise Band | Standing T-row | Standing T to Y row | Lunge |
| Seated calf raise or leg lift | Seated marching | Seated Marching and Ball Toss | Two ball toss | Standing ball toss | Walking and ball toss | Tandem Walk Ball Toss | |
| Forward lean (FWD lean) | FWD lean DA or SA raise | Sit to stand | FWD/BWD lean + leg lift | Sit to Stand Squat | Squat | Squat Press | |
| Single arm raise (SA raise) | Backward lean (BWD lean) | Combined FWD/BWD lean | Standing ScoliCorrection | Standing calf raise | Calf Raise + Side Raise | Aeroplane | |
| Backward lean marching | BWD lean marching and ball toss | FWD/BWD lean + leg lift + arm lift | Step Up | Runner Step Up Curl |
Appendix B. ScoliBrace®
References
- Weinstein, S.L.; Dolan, L.A.; Cheng, J.C.; Danielsson, A.; Morcuende, J.A. Adolescent idiopathic scoliosis. Lancet 2008, 371, 1527–1537. [Google Scholar] [CrossRef]
- Marya, S.; Tambe, A.D.; Millner, P.A.; Tsirikos, A.I. Adolescent idiopathic scoliosis: A review of aetiological theories of a multifactorial disease. Bone Jt. J. 2022, 104, 915–921. [Google Scholar] [CrossRef]
- Lenz, M.; Oikonomidis, S.; Harland, A.; Fürnstahl, P.; Farshad, M.; Bredow, J.; Eysel, P.; Scheyerer, M.J. Scoliosis and Prognosis—A systematic review regarding patient-specific and radiological predictive factors for curve progression. Eur. Spine J. 2021, 30, 1813–1822. [Google Scholar] [CrossRef]
- Negrini, S.; Hresko, T.M.; O’brien, J.P.; Price, N.; Boards, S.; Committee, S.N.-O. Recommendations for research studies on treatment of idiopathic scoliosis: Consensus 2014 between SOSORT and SRS non–operative management committee. Scoliosis 2015, 10, 8. [Google Scholar] [CrossRef]
- Lee, C.; Fong, D.Y.; Cheung, K.M.; Cheng, J.C.; Ng, B.K.; Lam, T.; Yip, P.S.; Luk, K.D. A new risk classification rule for curve progression in adolescent idiopathic scoliosis. Spine J. 2012, 12, 989–995. [Google Scholar] [CrossRef]
- Negrini, S.; Aulisa, A.G.; Aulisa, L.; Circo, A.B.; De Mauroy, J.C.; Durmala, J.; Grivas, T.B.; Knott, P.; Kotwicki, T.; Maruyama, T. 2011 SOSORT guidelines: Orthopaedic and rehabilitation treatment of idiopathic scoliosis during growth. Scoliosis 2012, 7, 3. [Google Scholar] [CrossRef]
- Negrini, S.; Donzelli, S.; Aulisa, A.G.; Czaprowski, D.; Schreiber, S.; de Mauroy, J.C.; Diers, H.; Grivas, T.B.; Knott, P.; Kotwicki, T. 2016 SOSORT guidelines: Orthopaedic and rehabilitation treatment of idiopathic scoliosis during growth. Scoliosis Spinal Disord. 2018, 13, 3. [Google Scholar] [CrossRef]
- Gao, C.; Zheng, Y.; Fan, C.; Yang, Y.; He, C.; Wong, M. Could the clinical effectiveness be improved under the integration of orthotic intervention and scoliosis-specific exercise in managing adolescent idiopathic scoliosis?: A randomized controlled trial study. Am. J. Phys. Med. Rehabil. 2019, 98, 642–648. [Google Scholar] [CrossRef]
- Negrini, A.; Verzini, N.; Parzini, S.; Negrini, A.; Negrini, S. Role of physical exercise in the treatment of mild idiopathic adolescent scoliosis. Eur. Medicophysica 2001, 37, 181–190. [Google Scholar]
- Zaina, F.; Negrini, S.; Atanasio, S.; Fusco, C.; Romano, M.; Negrini, A. Specific exercises performed in the period of brace weaning can avoid loss of correction in Adolescent Idiopathic Scoliosis (AIS) patients: Winner of SOSORT’s 2008 Award for Best Clinical Paper. Scoliosis 2009, 4, 8. [Google Scholar] [CrossRef]
- Berdishevsky, H.; Lebel, V.A.; Bettany-Saltikov, J.; Rigo, M.; Lebel, A.; Hennes, A.; Romano, M.; Białek, M.; M’hango, A.; Betts, T. Physiotherapy scoliosis-specific exercises–a comprehensive review of seven major schools. Scoliosis Spinal Disord. 2016, 11, 20. [Google Scholar] [CrossRef]
- Aktan, D.; Erdoganoglu, Y. Effect of short-term 3-dimensional schroth exercises in adolescent idiopathic scoliosis: An observational study. J. Manip. Physiol. Ther. 2021, 44, 612–620. [Google Scholar] [CrossRef]
- Schreiber, S.; Parent, E.C.; Moez, E.K.; Hedden, D.M.; Hill, D.; Moreau, M.J.; Lou, E.; Watkins, E.M.; Southon, S.C. The effect of Schroth exercises added to the standard of care on the quality of life and muscle endurance in adolescents with idiopathic scoliosis—An assessor and statistician blinded randomized controlled trial: “SOSORT 2015 Award Winner”. Scoliosis 2015, 10, 24. [Google Scholar] [CrossRef]
- Kuru, T.; Yeldan, İ.; Dereli, E.E.; Özdinçler, A.R.; Dikici, F.; Çolak, İ. The efficacy of three-dimensional Schroth exercises in adolescent idiopathic scoliosis: A randomised controlled clinical trial. Clin. Rehabil. 2016, 30, 181–190. [Google Scholar] [CrossRef]
- Schreiber, S.; Parent, E.C.; Khodayari Moez, E.; Hedden, D.M.; Hill, D.L.; Moreau, M.; Lou, E.; Watkins, E.M.; Southon, S.C. Schroth physiotherapeutic scoliosis-specific exercises added to the standard of care lead to better Cobb angle outcomes in adolescents with idiopathic scoliosis–an assessor and statistician blinded randomized controlled trial. PLoS ONE 2016, 11, e0168746. [Google Scholar] [CrossRef]
- Kwan, K.Y.H.; Cheng, A.C.; Koh, H.Y.; Chiu, A.Y.; Cheung, K.M.C. Effectiveness of Schroth exercises during bracing in adolescent idiopathic scoliosis: Results from a preliminary study—SOSORT Award 2017 Winner. Scoliosis Spinal Disord. 2017, 12, 32. [Google Scholar] [CrossRef]
- Marti, C.L.; Glassman, S.D.; Knott, P.T.; Carreon, L.Y.; Hresko, M.T. Scoliosis Research Society members attitudes towards physical therapy and physiotherapeutic scoliosis specific exercises for adolescent idiopathic scoliosis. Scoliosis 2015, 10, 16. [Google Scholar] [CrossRef]
- Weinstein, S.L.; Dolan, L.A.; Wright, J.G.; Dobbs, M.B. Design of the bracing in adolescent idiopathic scoliosis trial (BrAIST). Spine 2013, 38, 1832. [Google Scholar] [CrossRef]
- Falk, B.; Rigby, W.A.; Akseer, N. Adolescent idiopathic scoliosis: The possible harm of bracing and the likely benefit of exercise. Spine J. 2015, 15, 1169–1171. [Google Scholar] [CrossRef]
- Takasaki, H.; Miki, T. The impact of continuous use of lumbosacral orthoses on trunk motor performance: A systematic review with meta-analysis. Spine J. 2017, 17, 889–900. [Google Scholar] [CrossRef]
- Biering-Sørensen, F. Physical measurements as risk indicators for low-back trouble over a one-year period. Spine 1984, 9, 106–119. [Google Scholar] [CrossRef]
- Minjollet, L.; Abelin-Genevois, K.; De Chelle, G.; Sakoun, L.; Pujol, A.; Blay, G.L.; Bernard, J.-C. Are trunk muscles weaker in adolescent females with adolescent idiopathic scoliosis compared with their healthy counterparts? Isokinet. Exerc. Sci. 2021, 29, 419–427. [Google Scholar] [CrossRef]
- Cheung, J.; Halbertsma, J.P.; Veldhuizen, A.G.; Sluiter, W.J.; Maurits, N.M.; Cool, J.C.; van Horn, J.R. A preliminary study on electromyographic analysis of the paraspinal musculature in idiopathic scoliosis. Eur. Spine J. 2005, 14, 130–137. [Google Scholar] [CrossRef]
- Federau, C.; Kroismayr, D.; Dyer, L.; Farshad, M.; Pfirrmann, C. Demonstration of asymmetric muscle perfusion of the back after exercise in patients with adolescent idiopathic scoliosis using intravoxel incoherent motion (IVIM) MRI. NMR Biomed. 2020, 33, e4194. [Google Scholar] [CrossRef]
- Stetkarova, I.; Zamecnik, J.; Bocek, V.; Vasko, P.; Brabec, K.; Krbec, M. Electrophysiological and histological changes of paraspinal muscles in adolescent idiopathic scoliosis. Eur. Spine J. 2016, 25, 3146–3153. [Google Scholar] [CrossRef]
- Mannion, A.; Meier, M.; Grob, D.; Müntener, M. Paraspinal muscle fibre type alterations associated with scoliosis: An old problem revisited with new evidence. Eur. Spine J. 1998, 7, 289–293. [Google Scholar] [CrossRef]
- Zapata, K.A.; Wang-Price, S.S.; Sucato, D.J.; Dempsey-Robertson, M. Ultrasonographic measurements of paraspinal muscle thickness in adolescent idiopathic scoliosis: A comparison and reliability study. Pediatr. Phys. Ther. 2015, 27, 119–125. [Google Scholar] [CrossRef]
- Linek, P.; Wolny, T.; Saulicz, E.; Mysliwiec, A. Side differences of the lateral abdominal wall in supine rest position in mild adolescent idiopathic thoracolumbar scoliosis. Turk. J. Phys. Med. Rehabil. 2017, 63, 224. [Google Scholar] [CrossRef]
- Kim, D.-K.; Kim, C.-Y.; Lee, B.-K.; Seo, D. A comparison of ultrasonography measurement on the abdominal muscle thickness between adolescent idiopathic scoliosis and healthy subjects. J. Back Musculoskelet. Rehabil. 2018, 31, 65–74. [Google Scholar] [CrossRef]
- Doran, M.; Öneş, K.; Terzibaşioğlu, A.M.; Çinar, Ç.; Ata, İ. Ultrasonographic evaluation of abdominal muscle thickness symmetry in adolescent idiopathic scoliosis: A case-controlled study. Eur. J. Phys. Rehabil. Med. 2021, 57, 968–976. [Google Scholar] [CrossRef]
- Le Blay, G.; Pujol, A.; Verdun, S.; Bard-Pondarré, R.; Bernard, J.-C.; Chaléat-Valayer, E. Isokinetic evaluation of the trunk flexors and extensors in women with and without scoliosis: A comparative study. Isokinet. Exerc. Sci. 2021, 29, 75–81. [Google Scholar] [CrossRef]
- Odermatt, D.; Mathieu, P.A.; Beausejour, M.; Labelle, H.; Aubin, C.É. Electromyography of scoliotic patients treated with a brace. J. Orthop. Res. 2003, 21, 931–936. [Google Scholar] [CrossRef] [PubMed]
- Danielsson, A.J.; Romberg, K.; Nachemson, A.L. Spinal range of motion, muscle endurance, and back pain and function at least 20 years after fusion or brace treatment for adolescent idiopathic scoliosis: A case-control study. Spine 2006, 31, 275–283. [Google Scholar] [CrossRef] [PubMed]
- Azadinia, F.; Takamjani, E.E.; Kamyab, M.; Parnianpour, M.; Cholewicki, J.; Maroufi, N. Can lumbosacral orthoses cause trunk muscle weakness? A systematic review of literature. Spine J. 2017, 17, 589–602. [Google Scholar] [CrossRef] [PubMed]
- Fayolle-Minon, I.; Calmels, P. Effect of wearing a lumbar orthosis on trunk muscles: Study of the muscle strength after 21 days of use on healthy subjects. Jt. Bone Spine 2008, 75, 58–63. [Google Scholar] [CrossRef] [PubMed]
- Romberg, K.; Danielsson, A.; Olsén, M.F.; Kjellby-Wendt, G. Spinal mobility and muscle function in middle-aged patients treated for early onset idiopathic scoliosis: Compared with untreated and treated adolescent onset patients. Spine Deform. 2022, 10, 1085–1095. [Google Scholar] [CrossRef]
- Gubbels, C.M.; Oakely, P.A.; McAviney, J.; Harrison, D.E.; Brown, B.T. Reduction of Scheuermann’s deformity and scoliosis using ScoliBrace and a scoliosis specific rehabilitation program: A case report. J. Phys. Ther. Sci. 2019, 31, 159–165. [Google Scholar] [CrossRef] [PubMed]
- McAviney, J.; Brown, B.T. Treatment of infantile idiopathic scoliosis using a novel thoracolumbosacral orthosis: A case report. J. Med. Case Rep. 2022, 16, 20. [Google Scholar] [CrossRef]
- Harrison, D.D.; Janik, T.J.; Harrison, G.R.; Troyanovich, S.; Harrison, D.E.; Harrison, S.O. Chiropractic biophysics technique: A linear algebra approach to posture in chiropractic. J. Manip. Physiol. Ther. 1996, 19, 525–535. [Google Scholar]
- McGill, S.M.; Childs, A.; Liebenson, C. Endurance times for low back stabilization exercises: Clinical targets for testing and training from a normal database. Arch. Phys. Med. Rehabil. 1999, 80, 941–944. [Google Scholar] [CrossRef]
- Smith, A.J.; O’Sullivan, P.B.; Campbell, A.C.; Straker, L.M. The relationship between back muscle endurance and physical, lifestyle, and psychological factors in adolescents. J. Orthop. Sports Phys. Ther. 2010, 40, 517–523. [Google Scholar] [CrossRef]
- Janik, F.; Toulotte, C.; Seichepine, A.L.; Masquelier, B.; Barbier, F.; Fabre, C. Isometric strength database for muscle maximal voluntary endurance field tests: Normative data. Sports Med. Open 2021, 7, 47. [Google Scholar] [CrossRef]
- Chen, L.-W.; Bih, L.-I.; Ho, C.-C.; Huang, M.-H.; Chen, C.-T.; Wei, T.-S. Endurance times for trunk-stabilization exercises in healthy women: Comparing 3 kinds of trunk-flexor exercises. J. Sport Rehabil. 2003, 12, 199–207. [Google Scholar] [CrossRef]
- Johnson, O.E.; Mbada, C.E.; Akosile, C.O.; Agbeja, O.A. Isometric endurance of the back extensors in school-aged adolescents with and without low back pain. J. Back Musculoskelet. Rehabil. 2009, 22, 205–211. [Google Scholar] [CrossRef]
- Mbada, C.E.; Ayanniyi, O.; Adedoyin, R.A.; Johnson, O.E.; Dada, O.O. Back Muscles’endurance in Adolescents and Adults: Normative Data for A Sub-Saharan African Population. J. Musculoskelet. Res. 2011, 14, 1150004. [Google Scholar] [CrossRef]
- McGill, S.; Belore, M.; Crosby, I.; Russell, C. Clinical tools to quantify torso flexion endurance: Normative data from student and firefighter populations. Occup. Ergon. 2010, 9, 55–61. [Google Scholar] [CrossRef]
- Andersen, L.B.; Wedderkopp, N.; Leboeuf-Yde, C. Association between back pain and physical fitness in adolescents. Spine 2006, 31, 1740–1744. [Google Scholar] [CrossRef]
- Zoabli, G.; Mathieu, P.A.; Aubin, C.-É. Back muscles biometry in adolescent idiopathic scoliosis. Spine J. 2007, 7, 338–344. [Google Scholar] [CrossRef]
- Jiang, H.; Meng, Y.; Jin, X.; Zhang, C.; Zhao, J.; Wang, C.; Gao, R.; Zhou, X. Volumetric and fatty infiltration imbalance of deep paravertebral muscles in adolescent idiopathic scoliosis. Med. Sci. Monit. Int. Med. J. Exp. Clin. Res. 2017, 23, 2089. [Google Scholar] [CrossRef]
- Sato, T.; Hirano, T.; Ito, T.; Morita, O.; Kikuchi, R.; Endo, N.; Tanabe, N. Back pain in adolescents with idiopathic scoliosis: Epidemiological study for 43,630 pupils in Niigata City, Japan. Eur. Spine J. 2011, 20, 274–279. [Google Scholar] [CrossRef]
- Barba, N.; Ignasiak, D.; Villa, T.M.T.; Galbusera, F.; Bassani, T. Assessment of trunk muscle activation and intervertebral load in adolescent idiopathic scoliosis by musculoskeletal modelling approach. J. Biomech. 2021, 114, 110154. [Google Scholar] [CrossRef] [PubMed]
- Romano, M.; Minozzi, S.; Bettany-Saltikov, J.; Zaina, F.; Chockalingam, N.; Kotwicki, T.; Maier-Hennes, A.; Negrini, S. Exercises for adolescent idiopathic scoliosis. Cochrane Database Syst. Rev. 2012, 2012, CD007837. [Google Scholar] [CrossRef] [PubMed]
- Weiss, H.-R.; Klein, R. Improving excellence in scoliosis rehabilitation: A controlled study of matched pairs. Pediatr. Rehabil. 2006, 9, 190–200. [Google Scholar] [CrossRef] [PubMed]


| Total number of patients | 33 |
| Age | Mean 13.24 years Range 9–17 years Standard Deviation 1.64 |
| Sex | Female 29 (87.88%) Male 4 (12.12%) |
| Primary Curve Location | Left Thoracolumbar 7 (21.21%) Right Thoracic 26 (78.79%) |
| Largest Cobb Angle | Mean 38.97° Standard Deviation 9.49 |
| Measure of Comparison | Baseline Median (n, Inter-Quartile Range) | Short-Term Median (n, Inter-Quartile Range) | Medium-Term Median (n, Inter-Quartile Range) | Median of the Difference (95% CI) | p-Value (Wilcoxon Signed- Rank Test) |
|---|---|---|---|---|---|
| TE 1 | 87 (33, 60–120) | 150 (31, 81–180) | - | 37 (18.49–55.01) | <0.001 |
| TE 1 | 87 (33, 60–120) | - | 180 (28, 133–180) | 68.5 (46.83–92.50) | <0.001 |
| TE 1 | - | 150 (31, 81–180) | 180 (28, 133–180) | 0 (0.00–39.34) | 0.01 |
| AE 2 | 95 (33, 76–180) | 180 (32, 145–180) | - | 33 (12.98–65.02) | <0.001 |
| AE 2 | 95 (33, 76–180) | - | 180 (29, 121–180) | 47 (0.00–62.45) | 0.002 |
| AE 2 | - | 180 (32, 145–180) | 180 (29, 121–180) | 0 (0.00–15.05) | 0.860 |
| Measure of Comparison | Baseline Median (n, Inter-Quartile Range) | Short-Term Median (n, Inter-Quartile Range) | Medium-Term Median (n, Inter-Quartile Range) | Median of the Difference (95% CI) | p-Value (Wilcoxon Signed-Rank Test) |
|---|---|---|---|---|---|
| TE 1 | 70 (27, 45–103) | 94 (17, 74–133) | - | 29 (16.05–48.90) | < 0.001 |
| TE 1 | 70 (27, 45–103) | - | 119 (12, 83–136.5) | 47.5 (30.96–74.68) | 0.002 |
| TE 1 | - | 94 (17, 74–133) | 119 (12, 83–136.5) | 20.5 (−2.70–46.70) | 0.025 |
| AE 2 | 81.5 (24, 63–105.5) | 131 (12, 67.5–152) | - | 42.5 (14.49–75.72) | 0.004 |
| AE 2 | 81.5 (24, 63–105.5) | - | 110 (11, 80–128) | 45 (−36.21–58.14) | 0.139 |
| AE 2 | - | 131 (12, 67.5–152) | 110 (11, 80–128) | 24.5 (−40.80–70.50) | 0.674 |
| Measure | Timepoint | Total Number of Measurements | Number (Proportion) Who Did Not Reach 180 s | Number (Proportion) Who Reached 180 s |
|---|---|---|---|---|
| TE 1 | Baseline | 33 | 27 (81.82%) | 6 (18.18%) |
| TE 1 | Short-term | 31 | 17 (54.84%) | 14 (45.16%) |
| TE 1 | Medium-term | 28 | 12 (42.86%) | 16 (57.14%) |
| AE 2 | Baseline | 33 | 24 (72.73%) | 9 (27.27%) |
| AE 2 | Short-term | 32 | 12 (37.50%) | 20 (62.50%) |
| AE 2 | Medium-term | 29 | 11 (37.93%) | 18 (62.07%) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Marchese, R.; Du Plessis, J.; Pooke, T.; McAviney, J. The Improvement of Trunk Muscle Endurance in Adolescents with Idiopathic Scoliosis Treated with ScoliBrace® and the ScoliBalance® Exercise Approach. J. Clin. Med. 2024, 13, 653. https://doi.org/10.3390/jcm13030653
Marchese R, Du Plessis J, Pooke T, McAviney J. The Improvement of Trunk Muscle Endurance in Adolescents with Idiopathic Scoliosis Treated with ScoliBrace® and the ScoliBalance® Exercise Approach. Journal of Clinical Medicine. 2024; 13(3):653. https://doi.org/10.3390/jcm13030653
Chicago/Turabian StyleMarchese, Rosemary, Juan Du Plessis, Tamara Pooke, and Jeb McAviney. 2024. "The Improvement of Trunk Muscle Endurance in Adolescents with Idiopathic Scoliosis Treated with ScoliBrace® and the ScoliBalance® Exercise Approach" Journal of Clinical Medicine 13, no. 3: 653. https://doi.org/10.3390/jcm13030653
APA StyleMarchese, R., Du Plessis, J., Pooke, T., & McAviney, J. (2024). The Improvement of Trunk Muscle Endurance in Adolescents with Idiopathic Scoliosis Treated with ScoliBrace® and the ScoliBalance® Exercise Approach. Journal of Clinical Medicine, 13(3), 653. https://doi.org/10.3390/jcm13030653