Clinical Outcomes after Multivalve Surgery in Octogenarians: Evaluating the Need for a Paradigm Shift
Abstract
1. Introduction
2. Patients and Methods
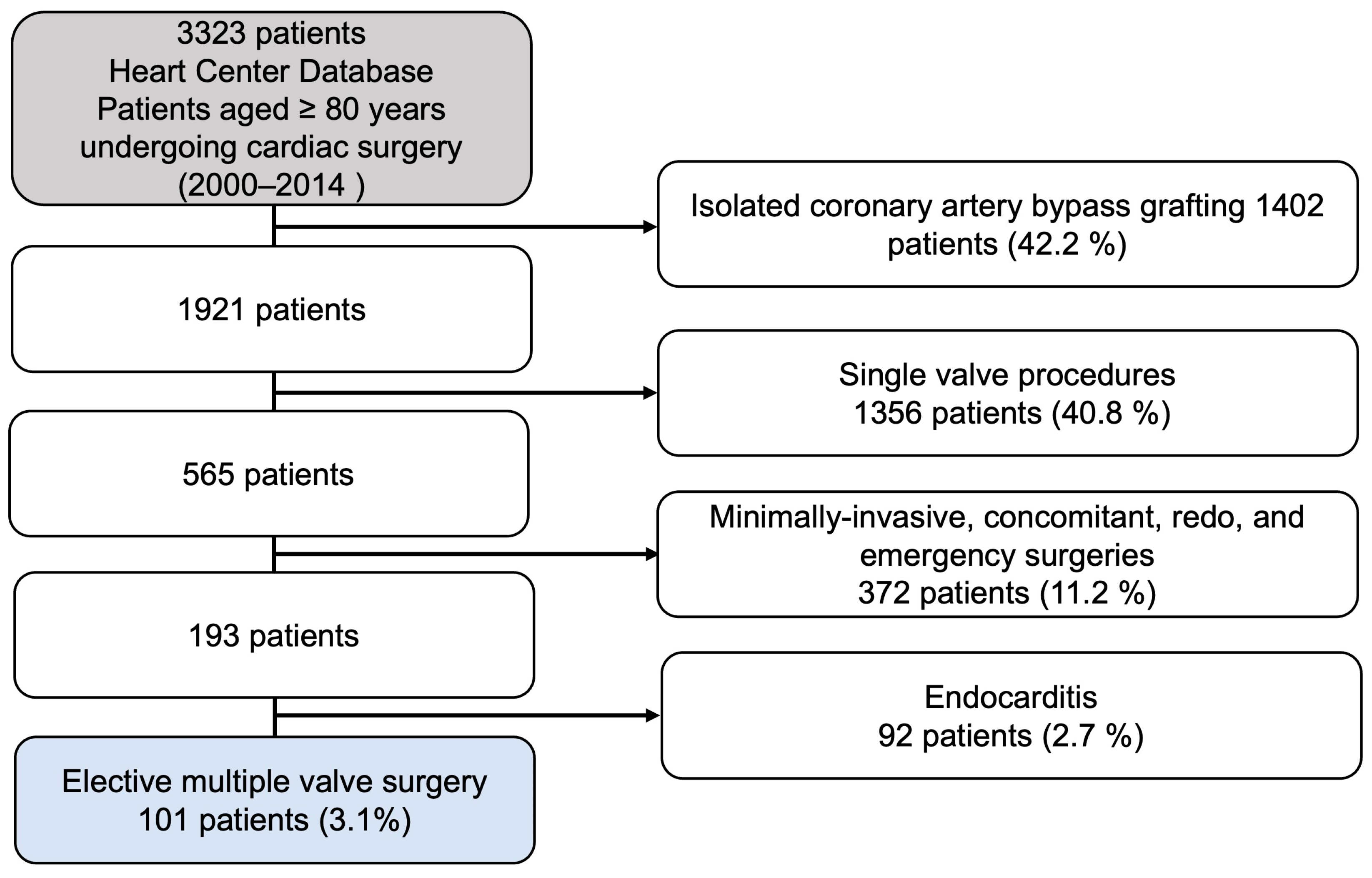
2.1. Inclusion and Exclusion Criteria
2.2. Study Design and Ethical Statement
2.3. Patients
2.4. Statistical Analysis
2.5. Surgical Techniques
3. Results
3.1. Baseline Characteristics
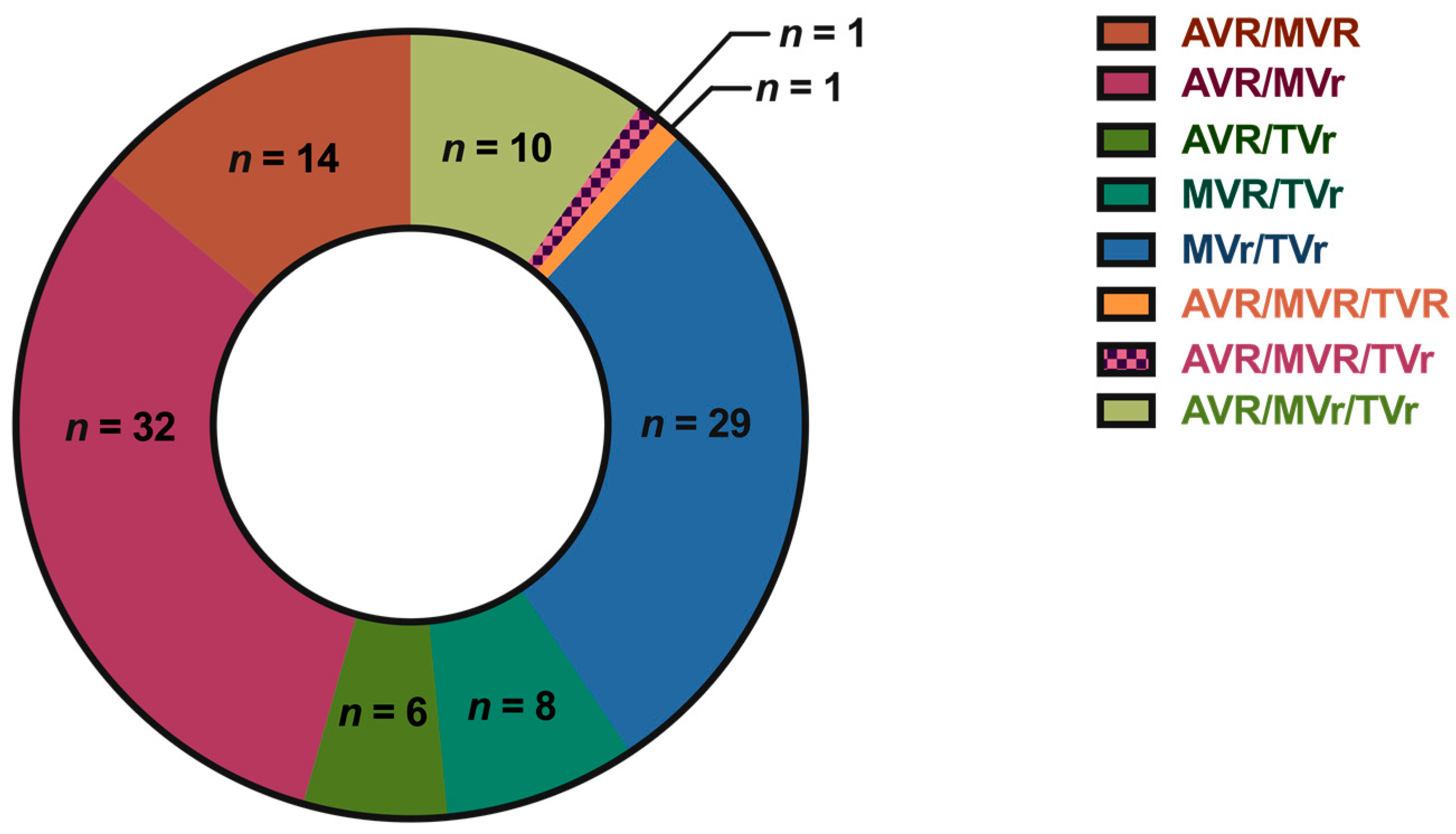
3.2. Surgical Procedures
3.3. In-Hospital Outcomes
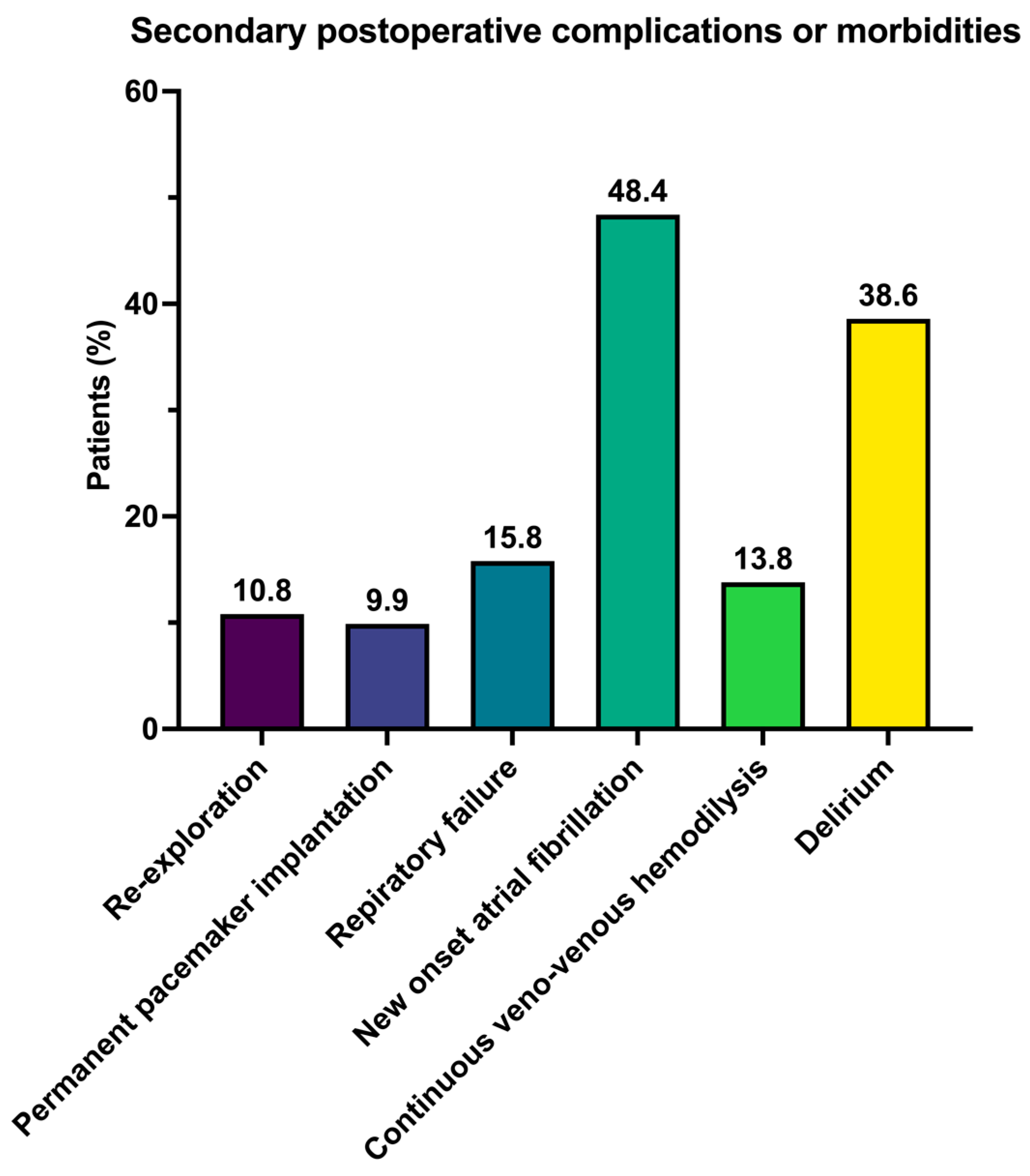
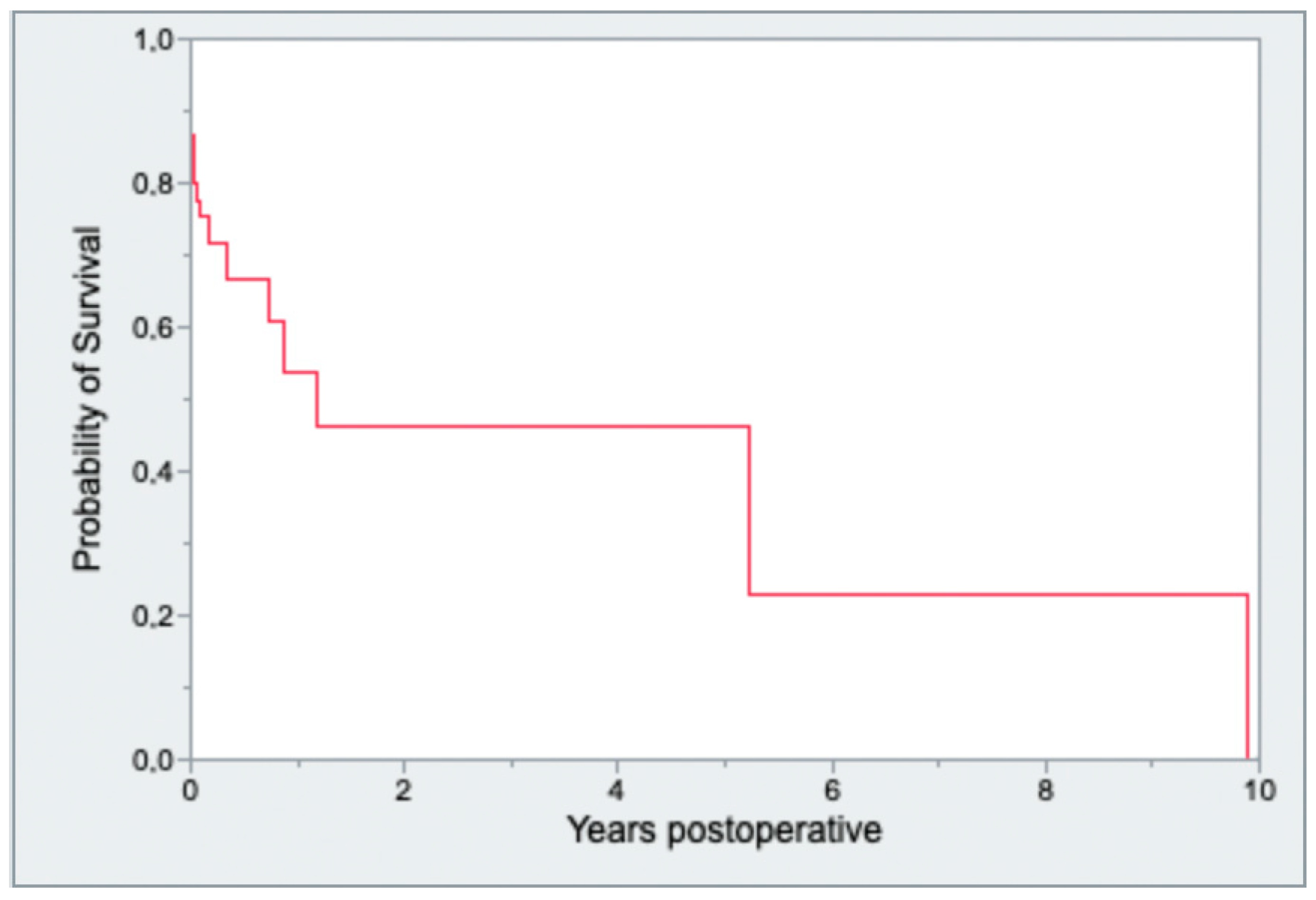
3.4. Survival Analysis
3.5. Univariate and Multivariate Analysis
3.5.1. Univariate and Multivariate Analysis for In-Hospital Mortality
3.5.2. Univariate and Multivariate Analysis for One-Year Mortality
4. Discussion
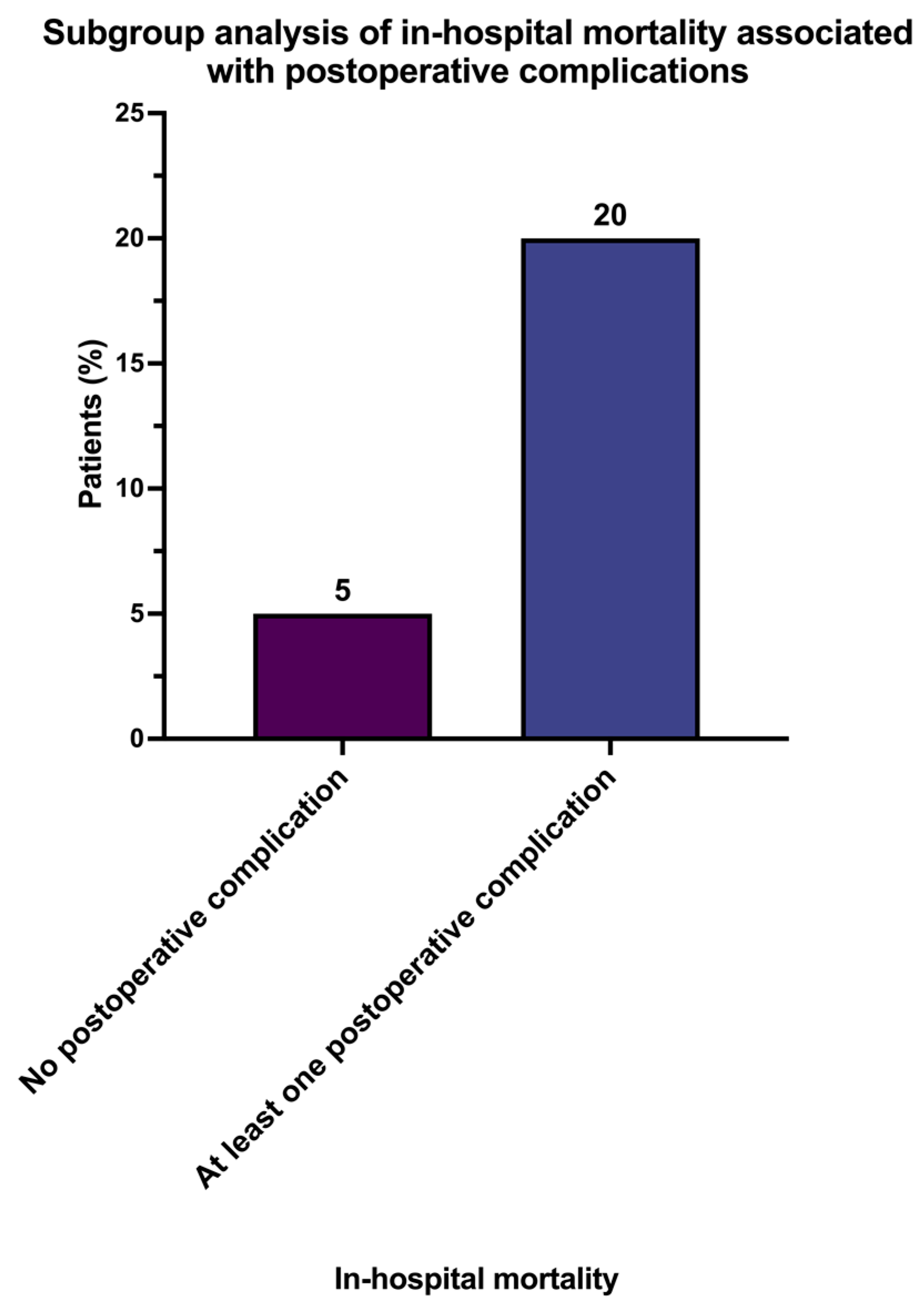
- Mortality increased fourfold once at least one postoperative complication occurred.
- Octogenarians face a high in-hospital mortality rate of 13.9%.
- Nearly half (43.8%) of the octogenarian patients who underwent multiple valve surgery died after one year.
- In our investigation, postoperative delirium emerged as a significant independent risk factor, contributing not only to an elevated risk of in-hospital mortality but also to a higher likelihood of one-year mortality. Additionally, prolonged surgical procedure time was identified as an independent risk factor associated with increased in-hospital mortality. While continuous veno-venous hemodialysis showed an independent impact on in-hospital mortality, it did not exhibit a significant effect on one-year mortality. Furthermore, both re-intubation and the transfusion of packed red blood cells were identified as independent risk factors for one-year mortality.
5. Limitations
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Eurostat. Population Structure and Ageing. Available online: https://ec.europa.eu/eurostat/statistics-explained/index.php?title=Population_structure_and_ageing#The_share_of_elderly_people_continues_to_increase (accessed on 10 November 2022).
- Beckmann, A.; Meyer, R.; Lewandowski, J.; Markewitz, A.; Blassfeld, D.; Boning, A. German Heart Surgery Report 2021: The Annual Updated Registry of the German Society for Thoracic and Cardiovascular Surgery. Thorac. Cardiovasc. Surg. 2022, 70, 362–376. [Google Scholar] [CrossRef]
- Rodgers, J.L.; Jones, J.; Bolleddu, S.I.; Vanthenapalli, S.; Rodgers, L.E.; Shah, K.; Karia, K.; Panguluri, S.K. Cardiovascular Risks Associated with Gender and Aging. J. Cardiovasc. Dev. Dis. 2019, 6, 19. [Google Scholar] [CrossRef]
- Unger, P.; Clavel, M.A.; Lindman, B.R.; Mathieu, P.; Pibarot, P. Pathophysiology and management of multivalvular disease. Nat. Rev. Cardiol. 2016, 13, 429–440. [Google Scholar] [CrossRef]
- Nkomo, V.T.; Gardin, J.M.; Skelton, T.N.; Gottdiener, J.S.; Scott, C.G.; Enriquez-Sarano, M. Burden of valvular heart diseases: A population-based study. Lancet 2006, 368, 1005–1011. [Google Scholar] [CrossRef] [PubMed]
- Lee, R.; Li, S.; Rankin, J.S.; O’Brien, S.M.; Gammie, J.S.; Peterson, E.D.; McCarthy, P.M.; Edwards, F.H.; Society of Thoracic Surgeons Adult Cardiac Surgical Database. Fifteen-year outcome trends for valve surgery in North America. Ann. Thorac. Surg. 2011, 91, 677–684. [Google Scholar] [CrossRef]
- Bossone, E.; Di Benedetto, G.; Frigiola, A.; Carbone, G.L.; Panza, A.; Cirri, S.; Ballotta, A.; Messina, S.; Rega, S.; Citro, R.; et al. Valve surgery in octogenarians: In-hospital and long-term outcomes. Can. J. Cardiol. 2007, 23, 223–227. [Google Scholar] [CrossRef] [PubMed]
- Alfieri, O.; Maisano, F. Mitral valve surgery in the elderly: New insights and unanswered questions. Eur. Heart J. 2011, 32, 535–536. [Google Scholar] [CrossRef]
- Akins, C.W.; Daggett, W.M.; Vlahakes, G.J.; Hilgenberg, A.D.; Torchiana, D.F.; Madsen, J.C.; Buckley, M.J. Cardiac operations in patients 80 years old and older. Ann. Thorac. Surg. 1997, 64, 606–614. [Google Scholar] [CrossRef] [PubMed]
- Bhamidipati, C.M.; LaPar, D.J.; Fonner, E., Jr.; Kern, J.A.; Kron, I.L.; Ailawadi, G. Outcomes and cost of cardiac surgery in octogenarians is related to type of operation: A multiinstitutional analysis. Ann. Thorac. Surg. 2011, 91, 499–505. [Google Scholar] [CrossRef] [PubMed]
- Fruitman, D.S.; MacDougall, C.E.; Ross, D.B. Cardiac surgery in octogenarians: Can elderly patients benefit? Quality of life after cardiac surgery. Ann. Thorac. Surg. 1999, 68, 2129–2135. [Google Scholar] [CrossRef] [PubMed]
- Habib, A.M.; Hussain, A.; Jarvis, M.; Cowen, M.E.; Chaudhry, M.A.; Loubani, M.; Cale, A.; Ngaage, D.L. Changing clinical profiles and in-hospital outcomes of octogenarians undergoing cardiac surgery over 18 years: A single-centre experiencedagger. Interact. Cardiovasc. Thorac. Surg. 2019, 28, 602–606. [Google Scholar] [CrossRef]
- Jones, J.M.; Loubani, M.; Grant, S.W.; Goodwin, A.T.; Trivedi, U.; Kendall, S.; Jenkins, D.P. Cardiac surgery in older patients: Hospital outcomes during a 15-year period from a complete national series. Interact. Cardiovasc. Thorac. Surg. 2022, 34, 532–539. [Google Scholar] [CrossRef] [PubMed]
- Saha, S.; Varghese, S.; Ahmad, A.A.; Jebran, A.F.; Waezi, N.; Niehaus, H.; Baraki, H.; Kutschka, I. Complex Valve Surgery in Elderly Patients: Increasingly Necessary and Surprisingly Feasible. Thorac. Cardiovasc. Surg. 2020, 68, 107–113. [Google Scholar] [CrossRef] [PubMed]
- Guiraudon, G.M.; Ofiesh, J.G.; Kaushik, R. Extended vertical transatrial septal approach to the mitral valve. Ann. Thorac. Surg. 1991, 52, 1058–1060. [Google Scholar] [CrossRef] [PubMed]
- Unger, P.; Pibarot, P.; Tribouilloy, C.; Lancellotti, P.; Maisano, F.; Iung, B.; Pierard, L.; European Society of Cardiology Council on Valvular Heart Disease. Multiple and Mixed Valvular Heart Diseases. Circ. Cardiovasc. Imaging 2018, 11, e007862. [Google Scholar] [CrossRef] [PubMed]
- Unger, P.; Tribouilloy, C. Aortic Stenosis with Other Concomitant Valvular Disease: Aortic Regurgitation, Mitral Regurgitation, Mitral Stenosis, or Tricuspid Regurgitation. Cardiol. Clin. 2020, 38, 33–46. [Google Scholar] [CrossRef]
- Yang, L.T.; Enriquez-Sarano, M.; Scott, C.G.; Padang, R.; Maalouf, J.F.; Pellikka, P.A.; Michelena, H.I. Concomitant Mitral Regurgitation in Patients with Chronic Aortic Regurgitation. J. Am. Coll. Cardiol. 2020, 76, 233–246. [Google Scholar] [CrossRef] [PubMed]
- Abah, U.; Dunne, M.; Cook, A.; Hoole, S.; Brayne, C.; Vale, L.; Large, S. Does quality of life improve in octogenarians following cardiac surgery? A systematic review. BMJ Open 2015, 5, e006904. [Google Scholar] [CrossRef] [PubMed]
- Lee, K.B.; Rosenfeld, E.S.; Napolitano, M.A.; Chen, S.W.; Amdur, R.L.; Greenberg, M.D.; Trachiotis, G.D. Influence of Age on Cardiac Surgery Outcomes in United States Veterans. Heart Surg. Forum. 2020, 23, E225–E230. [Google Scholar] [CrossRef]
- Roques, F.; Nashef, S.A.; Michel, P.; Gauducheau, E.; de Vincentiis, C.; Baudet, E.; Cortina, J.; David, M.; Faichney, A.; Gabrielle, F.; et al. Risk factors and outcome in European cardiac surgery: Analysis of the EuroSCORE multinational database of 19030 patients. Eur. J. Cardiothorac. Surg. 1999, 15, 816–822. [Google Scholar] [CrossRef]
- Nashef, S.A.; Roques, F.; Sharples, L.D.; Nilsson, J.; Smith, C.; Goldstone, A.R.; Lockowandt, U. EuroSCORE II. Eur. J. Cardiothorac. Surg. 2012, 41, 734–744. [Google Scholar] [CrossRef]
- Friedrich, I.; Simm, A.; Kotting, J.; Tholen, F.; Fischer, B.; Silber, R.E. Cardiac surgery in the elderly patient. Dtsch. Arztebl. Int. 2009, 106, 416–422. [Google Scholar] [CrossRef]
- Salis, S.; Mazzanti, V.V.; Merli, G.; Salvi, L.; Tedesco, C.C.; Veglia, F.; Sisillo, E. Cardiopulmonary bypass duration is an independent predictor of morbidity and mortality after cardiac surgery. J. Cardiothorac. Vasc. Anesth. 2008, 22, 814–822. [Google Scholar] [CrossRef]
- Atladottir, H.O.; Modrau, I.S.; Jakobsen, C.J.; Torp-Pedersen, C.T.; Gissel, M.S.; Nielsen, D.V. Impact of perioperative course during cardiac surgery on outcomes in patients 80 years and older. J. Thorac. Cardiovasc. Surg. 2021, 162, 1568–1577. [Google Scholar] [CrossRef]
- Doenst, T.; Berretta, P.; Bonaros, N.; Savini, C.; Pitsis, A.; Wilbring, M.; Gerdisch, M.; Kempfert, J.; Rinaldi, M.; Folliguet, T.; et al. Aortic cross-clamp time correlates with mortality in the mini-mitral international registry. Eur. J. Cardiothorac. Surg. 2023, 63, ezad147. [Google Scholar] [CrossRef]
- Villareal, R.P.; Hariharan, R.; Liu, B.C.; Kar, B.; Lee, V.V.; Elayda, M.; Lopez, J.A.; Rasekh, A.; Wilson, J.M.; Massumi, A. Postoperative atrial fibrillation and mortality after coronary artery bypass surgery. J. Am. Coll. Cardiol. 2004, 43, 742–748. [Google Scholar] [CrossRef]
- Filardo, G.; Hamilton, C.; Hebeler, R.F., Jr.; Hamman, B.; Grayburn, P. New-onset postoperative atrial fibrillation after isolated coronary artery bypass graft surgery and long-term survival. Circ. Cardiovasc. Qual. Outcomes 2009, 2, 164–169. [Google Scholar] [CrossRef]
- Mariscalco, G.; Engstrom, K.G. Postoperative atrial fibrillation is associated with late mortality after coronary surgery, but not after valvular surgery. Ann. Thorac. Surg. 2009, 88, 1871–1876. [Google Scholar] [CrossRef]
- Mariscalco, G.; Klersy, C.; Zanobini, M.; Banach, M.; Ferrarese, S.; Borsani, P.; Cantore, C.; Biglioli, P.; Sala, A. Atrial fibrillation after isolated coronary surgery affects late survival. Circulation 2008, 118, 1612–1618. [Google Scholar] [CrossRef] [PubMed]
- Vahanian, A.; Beyersdorf, F.; Praz, F.; Milojevic, M.; Baldus, S.; Bauersachs, J.; Capodanno, D.; Conradi, L.; De Bonis, M.; De Paulis, R.; et al. 2021 ESC/EACTS Guidelines for the management of valvular heart disease. Eur. Heart J. 2022, 43, 561–632. [Google Scholar] [CrossRef] [PubMed]

| Variables | |
|---|---|
| Baseline demographic characteristics | |
| Age (years), mean ± SD | 82.0 ± 2.0 |
| Sex (female), n (%) | 67 (66.3) |
| Body mass index (kg/m2), mean ± SD | 25.7 ± 4.1 |
| Clinical symptoms and signs | |
| NYHA class III or IV, n (%) | 78 (77.2) |
| Dyspnea | 89 (88.1) |
| Anginal complaints | 11 (10.9) |
| Medical history | |
| Coronary artery disease, n (%) | 53 (52.4) |
| Preoperative LVEF < 50%, n (%) | 40 (39.6) |
| Preoperative atrial fibrillation, n (%) | 51 (53.6) |
| Chronic obstructive pulmonary disease, n (%) | 7 (6.9) |
| Pulmonary arterial hypertension, n (%) | 54 (53.5) |
| Chronic kidney disease, n (%) | 44 (43.6) |
| Extracardiac arteriopathy, n (%) | 14 (13.9) |
| Diabetes mellitus, n (%) | 40 (39.6) |
| Valve Pathology | |
| Aortic valve pathology, n (%) | 73 (72.2) |
| Aortic valve stenosis, n (%) | 58 (79.5) |
| Aortic valve regurgitation, n (%) | 15 (20.5) |
| Mitral valve pathology, n (%) | 95 (94.1) |
| Mitral valve stenosis, n (%) | 6 (6.3) |
| Mitral valve regurgitation, n (%) | 89 (93.7) |
| Tricuspid valve pathology, n (%) | 74 (73.2) |
| Tricuspid valve stenosis, n (%) | 1 (1.3) |
| Tricuspid valve regurgitation, n (%) | 73 (98.7) |
| Surgical risk stratification | |
| Logistic EuroSCORE (%), mean ± SD | 25.3 ± 19.5 |
| EuroSCORE II (%), mean ± SD | 16.8 ± 11.3 |
| Variables | In-Hospital Mortality | One-Year Mortality | ||||||
|---|---|---|---|---|---|---|---|---|
| Univariable Analysis | Multivariable Analysis | Univariable Analysis | Multivariable Analysis | |||||
| OR (95% CI) | p | OR (95% CI) | p | OR (95% CI) | p | OR (95% CI) | p | |
| Baseline demographic characteristics | ||||||||
| Age (years) | - | 0.110 | - | 0.210 | - | 0.400 | - | 0.170 |
| Sex (female) | - | 0.270 | - | 0.140 | - | 0.100 | - | 0.460 |
| Body mass index (kg/m2) | 1.2 (1.1, 2.9) | 0.040 * | - | 0.170 | - | 0.990 | - | 0.950 |
| Medical history | ||||||||
| Coronary artery disease | - | 0.280 | - | 0.360 | - | 0.410 | - | 0.520 |
| Preoperative LVEF < 50% | - | 0.090 | - | 0.110 | - | 0.110 | - | 0.410 |
| Preoperative atrial fibrillation | - | 0.170 | - | 0.170 | - | 0.630 | - | 0.570 |
| Chronic obstructive pulmonary disease | - | 0.230 | - | 0.450 | - | 0.330 | - | 0.480 |
| Pulmonary arterial hypertension | - | 0.090 | - | 0.249 | 1.3 (1.2, 3.1) | 0.020 * | - | 0.180 |
| Chronic kidney disease | - | 0.560 | - | 0.910 | - | 0.900 | - | 0.920 |
| Extracardiac arteriopathy | - | 0.400 | - | 0.110 | - | 0.690 | - | 0.520 |
| Diabetes mellitus | - | 0.950 | - | 0.210 | - | 0.360 | - | 0.150 |
| Procedural parameters | ||||||||
| Surgical procedure time (min) | 2.1 (1.7, 3.6) | <0.010 * | 1.9 (1.2, 3.1) | 0.010 * | 2.1 (1.2, 3.8) | <0.001 * | - | 0.680 |
| Parameters of postoperative clinical course | ||||||||
| Perioperative myocardial infarction | 1.8 (1.1, 3.1) | 0.040 * | - | 0.999 | - | 0.190 | - | 0.490 |
| Perioperative stroke | 2.2 (1.5, 3.0) | <0.010 * | - | 0.991 | 1.6 (1.1, 2.4) | 0.040 * | - | 0.999 |
| Postoperative delirium | 1.4 (1.1, 2.5) | 0.040 * | 2.4 (1.3, 2.7) | <0.01 * | 1.7 (1.3, 3.5) | <0.010 * | 1.6 (1.2, 1.8) | <0.001 * |
| New-onset atrial fibrillation | - | 0.170 | - | 0.174 | 1.3 (1.1, 3.8) | <0.010 * | 1.8 (1.4, 2.3) | <0.001 * |
| Re-intubation | - | 0.340 | - | 0.549 | 1.8 (1.1, 4.7) | 0.040 * | 2.1 (1.7–2.4) | <0.001 * |
| Continuous veno-venous hemodialysis | 3.8 (2.7, 6.8) | <0.010 * | 4.5 (3.0, 6.5) | <0.010 * | 2.5 (1.5, 5.6) | 0.040 * | - | 0.950 |
| Pulmonary arterial hypertension | - | 0.090 | - | 0.249 | 1.4 (1.1, 2.9) | 0.030 * | 0.100 | |
| Re-exploration | 3.1 (2.2, 7.6) | 0.020 * | - | 0.500 | - | 0.123 | - | 0.330 |
| Transfusion of PRBC (any) | - | 0.080 | - | 0.131 | 1.9 (1.2, 3.7) | 0.040 * | 1.3 (1.1, 1.6) | <0.001 * |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Taghizadeh-Waghefi, A.; Petrov, A.; Arzt, S.; Alexiou, K.; Tugtekin, S.-M.; Matschke, K.; Kappert, U.; Wilbring, M. Clinical Outcomes after Multivalve Surgery in Octogenarians: Evaluating the Need for a Paradigm Shift. J. Clin. Med. 2024, 13, 745. https://doi.org/10.3390/jcm13030745
Taghizadeh-Waghefi A, Petrov A, Arzt S, Alexiou K, Tugtekin S-M, Matschke K, Kappert U, Wilbring M. Clinical Outcomes after Multivalve Surgery in Octogenarians: Evaluating the Need for a Paradigm Shift. Journal of Clinical Medicine. 2024; 13(3):745. https://doi.org/10.3390/jcm13030745
Chicago/Turabian StyleTaghizadeh-Waghefi, Ali, Asen Petrov, Sebastian Arzt, Konstantin Alexiou, Sems-Malte Tugtekin, Klaus Matschke, Utz Kappert, and Manuel Wilbring. 2024. "Clinical Outcomes after Multivalve Surgery in Octogenarians: Evaluating the Need for a Paradigm Shift" Journal of Clinical Medicine 13, no. 3: 745. https://doi.org/10.3390/jcm13030745
APA StyleTaghizadeh-Waghefi, A., Petrov, A., Arzt, S., Alexiou, K., Tugtekin, S.-M., Matschke, K., Kappert, U., & Wilbring, M. (2024). Clinical Outcomes after Multivalve Surgery in Octogenarians: Evaluating the Need for a Paradigm Shift. Journal of Clinical Medicine, 13(3), 745. https://doi.org/10.3390/jcm13030745







