Correlations between Sagittal Parameters and Functional Scores in 65-Year-Old Osteoporotic Females with Vertebral Body Fracture under Low-Energy Mechanism
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
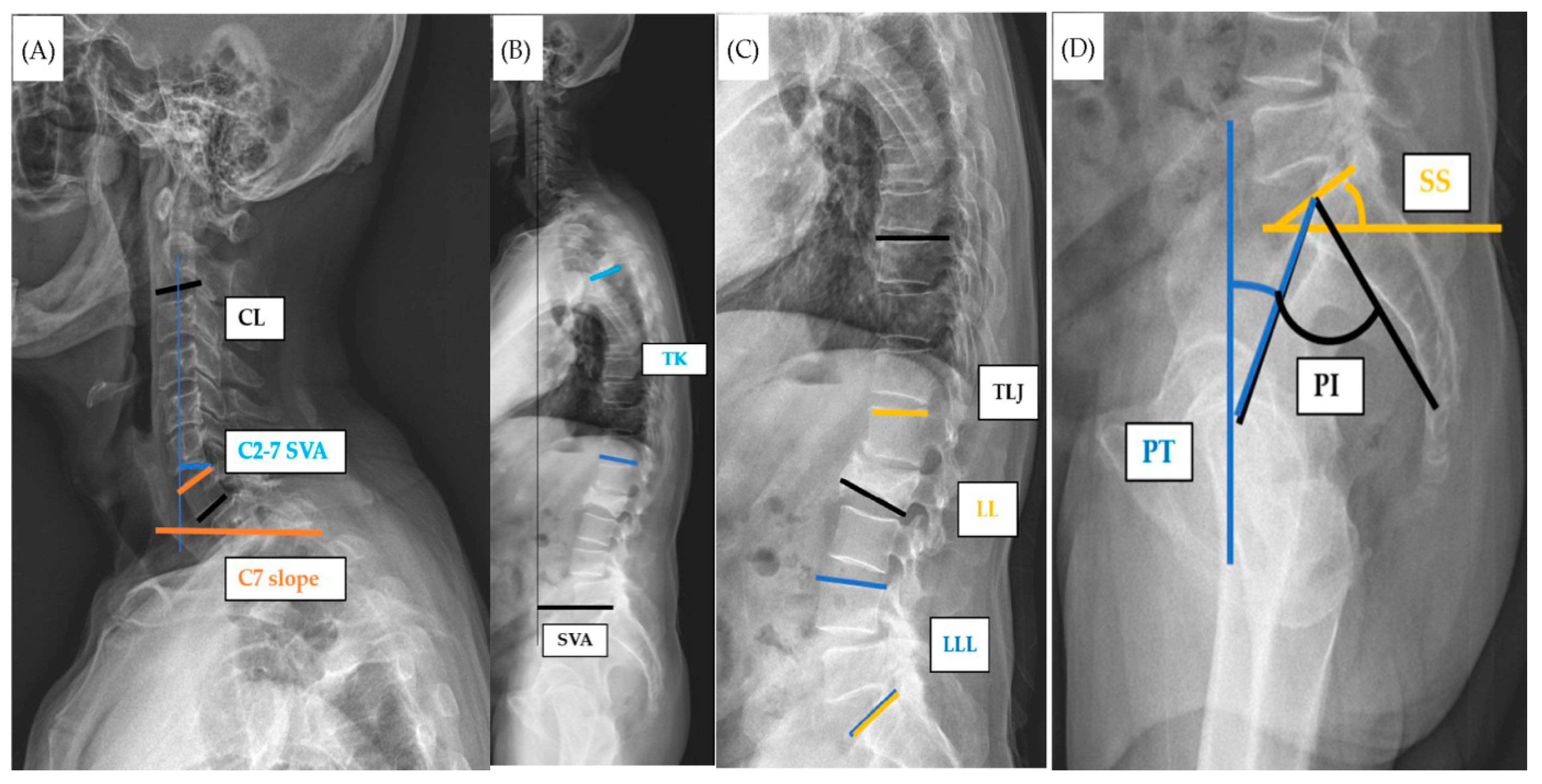
2.2. Spinal Sagittal Parameters
2.3. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Kanis, J.A.; Burlet, N.; Cooper, C.; Delmas, P.D.; Reginster, J.Y.; Borgstrom, F.; Rizzoli, R.; European Society for Clinical and Economic Aspects of Osteoporosis and Osteoarthritis (ESCEO). European guidance for the diagnosis and management of osteoporosis in postmenopausal women. Osteoporos. Int. 2008, 19, 399–428. [Google Scholar] [CrossRef]
- Maccagnano, G.; Notarnicola, A.; Pesce, V.; Mudoni, S.; Tafuri, S.; Moretti, B. The Prevalence of Fragility Fractures in a Population of a Region of Southern Italy Affected by Thyroid Disorders. BioMed Res. Int. 2016, 2016, 6017165. [Google Scholar] [CrossRef]
- Hoyt, D.; Urits, I.; Orhurhu, V.; Orhurhu, M.S.; Callan, J.; Powell, J.; Manchikanti, L.; Kaye, A.D.; Kaye, R.J.; Viswanath, O. Current Concepts in the Management of Vertebral Compression Fractures. Curr. Pain Headache Rep. 2020, 24, 16. [Google Scholar] [CrossRef]
- Ioannidis, G.; Papaioannou, A.; Hopman, W.M.; Akhtar-Danesh, N.; Anastassiades, T.; Pickard, L.; Kennedy, C.C.; Prior, J.C.; Olszynski, W.P.; Davison, K.S.; et al. Relation between fractures and mortality: Results from the Canadian Multicentre Osteoporosis Study. CMAJ 2009, 181, 265–271. [Google Scholar] [CrossRef]
- Kado, D.M.; Browner, W.S.; Palermo, L.; Nevitt, M.C.; Genant, H.K.; Cummings, S.R. Vertebral fractures and mortality in older women: A prospective study. Study of Osteoporotic Fractures Research Group. Arch. Intern. Med. 1999, 159, 1215–1220. [Google Scholar] [CrossRef]
- Ji, C.; Rong, Y.; Wang, J.; Yu, S.; Yin, G.; Fan, J.; Tang, P.; Jiang, D.; Liu, W.; Gong, F.; et al. Risk Factors for Refracture following Primary Osteoporotic Vertebral Compression Fractures. Pain Physician 2021, 24, E335–E340. [Google Scholar] [CrossRef] [PubMed]
- Lindsay, R.; Silverman, S.L.; Cooper, C.; Hanley, D.A.; Barton, I.; Broy, S.B.; Licata, A.; Benhamou, L.; Geusens, P.; Flowers, K.; et al. Risk of new vertebral fracture in the year following a fracture. JAMA 2001, 285, 320–323. [Google Scholar] [CrossRef] [PubMed]
- Fechtenbaum, J.; Etcheto, A.; Kolta, S.; Feydy, A.; Roux, C.; Briot, K. Sagittal balance of the spine in patients with osteoporotic vertebral fractures. Osteoporos. Int. 2016, 27, 559–567. [Google Scholar] [CrossRef]
- Hu, Z.; Man, G.C.W.; Kwok, A.K.L.; Law, S.W.; Chu, W.W.C.; Cheung, W.H.; Qiu, Y.; Cheng, J.C.Y. Global sagittal alignment in elderly patients with osteoporosis and its relationship with severity of vertebral fracture and quality of life. Arch. Osteoporos. 2018, 13, 95. [Google Scholar] [CrossRef] [PubMed]
- Imagama, S.; Hasegawa, Y.; Matsuyama, Y.; Sakai, Y.; Ito, Z.; Hamajima, N.; Ishiguro, N. Influence of sagittal balance and physical ability associated with exercise on quality of life in middle-aged and elderly people. Arch. Osteoporos. 2011, 6, 13–20. [Google Scholar] [CrossRef]
- Arima, K.; Abe, Y.; Nishimura, T.; Okabe, T.; Tomita, Y.; Mizukami, S.; Kanagae, M.; Aoyagi, K. Association of vertebral compression fractures with physical performance measures among community-dwelling Japanese women aged 40 years and older. BMC Musculoskelet. Disord. 2017, 18, 176. [Google Scholar] [CrossRef] [PubMed]
- Yeh, K.T.; Lee, R.P.; Chen, I.H.; Yu, T.C.; Peng, C.H.; Liu, K.L.; Wang, J.H.; Wu, W.T. Are There Age- and Sex-related Differences in Spinal Sagittal Alignment and Balance Among Taiwanese Asymptomatic Adults? Clin. Orthop. Relat. Res. 2018, 476, 1010–1017. [Google Scholar] [CrossRef] [PubMed]
- Mi Le, J.R.; Yeh, K.T.; Chen, C.W.; Jaw, F.S.; Yang, S.H.; Wu, W.T. Quantitative evaluation of correlation between lumbosacral lordosis and pelvic incidence in standing position among asymptomatic Asian adults: A prospective study. Sci. Rep. 2022, 12, 18965. [Google Scholar] [CrossRef] [PubMed]
- Park, S.W.; Shin, Y.S.; Kim, H.J.; Lee, J.H.; Shin, J.S.; Ha, I.H. The dischargeable cut-off score of Oswestry Disability Index (ODI) in the inpatient care for low back pain with disability. Eur. Spine J. 2014, 23, 2090–2096. [Google Scholar] [CrossRef]
- Boonstra, A.M.; Schiphorst Preuper, H.R.; Balk, G.A.; Stewart, R.E. Cut-off points for mild, moderate, and severe pain on the visual analogue scale for pain in patients with chronic musculoskeletal pain. Pain 2014, 155, 2545–2550. [Google Scholar] [CrossRef]
- Takahashi, K.; Wakabayashi, H.; Maeda, K.; Nagai, T.; Momosaki, R. Impact of body mass index on outcomes of inpatients with vertebral compression fractures in Japan: A retrospective cohort study. Geriatr. Gerontol. Int. 2023, 23, 788–794. [Google Scholar] [CrossRef]
- Ryan, S.D.; Fried, L.P. The impact of kyphosis on daily functioning. J. Am. Geriatr. Soc. 1997, 45, 1479–1486. [Google Scholar] [CrossRef]
- Roghani, T.; Zavieh, M.K.; Manshadi, F.D.; King, N.; Katzman, W. Age-related hyperkyphosis: Update of its potential causes and clinical impacts-narrative review. Aging Clin. Exp. Res. 2017, 29, 567–577. [Google Scholar] [CrossRef]
- Chau, L.T.C.; Hu, Z.; Ko, K.S.Y.; Man, G.C.W.; Yeung, K.H.; Law, Y.Y.; Lau, L.C.M.; Wong, R.M.Y.; Chu, W.C.W.; Cheng, J.C.Y.; et al. Global sagittal alignment of the spine, pelvis, lower limb after vertebral compression fracture and its effect on quality of life. BMC Musculoskelet. Disord. 2021, 22, 476. [Google Scholar] [CrossRef]
- Govil, G.; Tomar, L.; Dhawan, P. Knee-Spine Syndrome: Management Dilemma When Knee Osteoarthritis Coexists With Spine Degeneration. Cureus 2022, 14, e24939. [Google Scholar] [CrossRef]
- Alsoof, D.; Anderson, G.; McDonald, C.L.; Basques, B.; Kuris, E.; Daniels, A.H. Diagnosis and Management of Vertebral Compression Fracture. Am. J. Med. 2022, 135, 815–821. [Google Scholar] [CrossRef]
- Notarnicola, A.; Maccagnano, G.; Gallone, M.F.; Mastromauro, L.; Rifino, F.; Pesce, V.; Covelli, I.; Moretti, B. Extracorporeal shockwave therapy versus exercise program in patients with low back pain: Short-term results of a randomised controlled trial. J. Biol. Regul. Homeost. Agents 2018, 32, 385–389. [Google Scholar] [PubMed]
- Vilà-Canet, G.; García de Frutos, A.; Covaro, A.; Ubierna, M.T.; Caceres, E. Thoracolumbar fractures without neurological impairment: A review of diagnosis and treatment. EFORT Open Rev. 2016, 1, 332–338. [Google Scholar] [CrossRef]
- Parreira, P.C.S.; Maher, C.G.; Megale, R.Z.; March, L.; Ferreira, M.L. An overview of clinical guidelines for the management of vertebral compression fracture: A systematic review. Spine J. 2017, 17, 1932–1938. [Google Scholar] [CrossRef]
- Bailey, C.S.; Urquhart, J.C.; Dvorak, M.F.; Nadeau, M.; Boyd, M.C.; Thomas, K.C.; Kwon, B.K.; Gurr, K.R.; Bailey, S.I.; Fisher, C.G. Orthosis versus no orthosis for the treatment of thoracolumbar burst fractures without neurologic injury: A multicenter prospective randomized equivalence trial. Spine J. 2014, 14, 2557–2564. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.J.; Yi, J.M.; Cho, H.G.; Chang, B.S.; Lee, C.K.; Kim, J.H.; Yeom, J.S. Comparative study of the treatment outcomes of osteoporotic compression fractures without neurologic injury using a rigid brace, a soft brace, and no brace: A prospective randomized controlled non-inferiority trial. J. Bone Joint Surg. Am. 2014, 96, 1959–1966. [Google Scholar] [CrossRef] [PubMed]
- Gutierrez-Gonzalez, R.; Ortega, C.; Royuela, A.; Zamarron, A. Vertebral compression fractures managed with brace: Risk factors for progression. Eur. Spine J. 2023, 32, 3885–3891. [Google Scholar] [CrossRef] [PubMed]
- Boss, S.; Srivastava, V.; Anitescu, M. Vertebroplasty and Kyphoplasty. Phys. Med. Rehabil. Clin. N. Am. 2022, 33, 425–453. [Google Scholar] [CrossRef] [PubMed]
- Li, L.; Ren, J.; Liu, J.; Wang, H.; Wang, X.; Liu, Z.; Sun, T. Results of Vertebral Augmentation Treatment for Patients of Painful Osteoporotic Vertebral Compression Fractures: A Meta-Analysis of Eight Randomized Controlled Trials. PLoS ONE 2015, 10, e0138126. [Google Scholar] [CrossRef]
- Cazzato, R.L.; Bellone, T.; Scardapane, M.; De Marini, P.; Autrusseau, P.A.; Auloge, P.; Garnon, J.; Jennings, J.W.; Gangi, A. Vertebral augmentation reduces the 12-month mortality and morbidity in patients with osteoporotic vertebral compression fractures. Eur. Radiol. 2021, 31, 8246–8255. [Google Scholar] [CrossRef]
- McCarthy, J.; Davis, A. Diagnosis and Management of Vertebral Compression Fractures. Am. Fam. Physician 2016, 94, 44–50. [Google Scholar] [PubMed]
- Cho, I.; Jeon, C.; Lee, S.; Lee, D.; Hwangbo, G. Effects of lumbar stabilization exercise on functional disability and lumbar lordosis angle in patients with chronic low back pain. J. Phys. Ther. Sci. 2015, 27, 1983–1985. [Google Scholar] [CrossRef] [PubMed]
- Lafage, V.; Schwab, F.; Patel, A.; Hawkinson, N.; Farcy, J.P. Pelvic tilt and truncal inclination: Two key radiographic parameters in the setting of adults with spinal deformity. Spine 2009, 34, E599–E606. [Google Scholar] [CrossRef] [PubMed]
- Li, J.; Zhang, D.; Shen, Y. Impact of cervical sagittal parameters on axial neck pain in patients with cervical kyphosis. J. Orthop. Surg. Res. 2020, 15, 434. [Google Scholar] [CrossRef] [PubMed]
- Perez, E.A.; Woodroffe, R.W.; Park, B.; Gold, C.; Helland, L.C.; Seaman, S.C.; Hitchon, P.W. Cervical alignment in the obese population following posterior cervical fusion for cervical myelopathy. Clin. Neurol. Neurosurg. 2022, 212, 107059. [Google Scholar] [CrossRef] [PubMed]
- Li, W.S.; Cai, Y.F.; Cong, L. The Effect of Vertebral Augmentation Procedure on Painful OVCFs: A Meta-Analysis of Randomized Controlled Trials. Glob. Spine J. 2022, 12, 515–525. [Google Scholar] [CrossRef]
- Wardlaw, D.; Cummings, S.R.; Van Meirhaeghe, J.; Bastian, L.; Tillman, J.B.; Ranstam, J.; Eastell, R.; Shabe, P.; Talmadge, K.; Boonen, S. Efficacy and safety of balloon kyphoplasty compared with non-surgical care for vertebral compression fracture (FREE): A randomised controlled trial. Lancet 2009, 373, 1016–1024. [Google Scholar] [CrossRef]
- Taylor, R.S.; Fritzell, P.; Taylor, R.J. Balloon kyphoplasty in the management of vertebral compression fractures: An updated systematic review and meta-analysis. Eur. Spine J. 2007, 16, 1085–1100. [Google Scholar] [CrossRef]


| Item | Mean ± SD | Min. | Max. |
|---|---|---|---|
| Age | 72.71 ± 5.61 | 65 | 91 |
| BMI | 26.48 ± 5.14 | 13.48 | 49.79 |
| Spinal sagittal alignment | |||
| CL | 18.61 ± 14.23 | −27 | 70 |
| C7 slope | 28.52 ± 11.1 | −14.53 | 69.45 |
| C2–7 SVA | 17.21 ± 11.53 | 0 | 59.71 |
| LL | 38.99 ± 18.4 | −8 | 88 |
| LLL (L4-S1) | 30.18 ± 13.15 | −7 | 75 |
| TL junction (T10-L2) | 15.47 ± 10.68 | 1 | 60 |
| SVA | 64.75 ± 41.95 | 0 | 218.76 |
| PI | 55.13 ± 14.14 | 17.9 | 86.65 |
| SS | 32.76 ± 12.52 | 4.1 | 68.64 |
| PT | 22.37 ± 9.98 | −9.53 | 46.93 |
| PI-LL | 18.48 ± 13.79 | 0.06 | 55.07 |
| Functional outcome | |||
| ODI | 24.8 ± 9.38 | 10 | 48 |
| VAS | 5.25 ± 2.29 | 1 | 9 |
| Item | Crude | Adjusted | ||
|---|---|---|---|---|
| OR (95% CI) | p Value | OR (95% CI) | p Value | |
| Age | 0.96 (0.90, 1.02) | 0.144 | 0.92 (0.84, 1.01) | 0.086 |
| BMI | 1.04 (0.98, 1.11) | 0.237 | 1.09 (0.98, 1.21) | 0.107 |
| CL | 1.00 (0.98, 1.02) | 0.877 | ||
| C7 slope | 1.01 (0.98, 1.04) | 0.566 | ||
| C2–7 SVA | 0.99 (0.96, 1.02) | 0.543 | ||
| LL | 0.98 (0.97, 1.00) | 0.068 | 0.96 (0.92, 1.01) | 0.114 |
| LLL (L4-S1) | 1.01 (0.99, 1.04) | 0.244 | ||
| TL junction (T10-L2) | 1.27 (1.18, 1.37) | <0.001 * | 1.28 (1.18, 1.39) | <0.001 * |
| SVA | 0.99 (0.99, 1.01) | 0.830 | ||
| PI | 0.97 (0.94, 0.99) | 0.008 * | 0.98 (0.93, 1.03) | 0.400 |
| SS | 0.97 (0.94, 0.99) | 0.016 * | 1.04 (0.96, 1.12) | 0.327 |
| PT | 0.99 (0.96, 1.02) | 0.442 | ||
| PI-LL | 1.01 (0.99, 1.03) | 0.495 | ||
| Item | Crude | Adjusted | ||
|---|---|---|---|---|
| OR (95% CI) | p Value | OR (95% CI) | p Value | |
| Age | 0.95 (0.90, 1.01) | 0.125 | 0.93 (0.86, 1.01) | 0.070 |
| BMI | 1.04 (0.98, 1.11) | 0.197 | 1.06 (0.98, 1.16) | 0.146 |
| CL | 1.00 (0.98, 1.02) | 0.998 | ||
| C7 slope | 1.01 (0.98, 1.04) | 0.465 | ||
| C2–7 SVA | 0.99 (0.96, 1.02) | 0.355 | ||
| LL | 0.99 (0.98, 1.01) | 0.447 | ||
| LLL (L4-S1) | 1.02 (0.996, 1.05) | 0.094 | 0.99 (0.95, 1.03) | 0.672 |
| TL junction (T10-L2) | 1.16 (1.10, 1.22) | <0.001 * | 1.17 (1.10, 1.23) | <0.001 * |
| SVA | 1.00 (0.99, 1.00) | 0.359 | ||
| PI | 0.98 (0.96, 1.00) | 0.111 | 1.00 (0.96, 1.04) | 0.959 |
| SS | 0.98 (0.95, 1.01) | 0.125 | 0.99 (0.94, 1.05) | 0.926 |
| PT | 0.99 (0.96, 1.03) | 0.734 | ||
| PI-LL | 0.99 (0.98, 1.02) | 0.948 | ||
| Item | Age ≤ 72 y/o (n = 89) | Age > 72 y/o (n = 72) | Nonobese (n = 93) | Obese (n = 68) | ||||
|---|---|---|---|---|---|---|---|---|
| OR (95% CI) | p Value | OR (95% CI) | p Value | OR (95% CI) | p Value | OR (95% CI) | p Value | |
| Age | - | - | - | - | 0.88 (0.73, 1.05) | 0.149 | 0.95 (0.82, 1.09) | 0.453 |
| BMI | 1.15 (0.95, 1.38) | 0.144 | 1.01 (0.83, 1.23) | 0.947 | - | - | - | - |
| CL | 0.92 (0.83, 1.02) | 0.116 | 0.97 (0.87, 1.08) | 0.524 | 0.96 (0.88, 1.05) | 0.386 | 0.91 (0.81, 1.03) | 0.138 |
| C7 slope | 1.10 (0.97, 1.26) | 0.143 | 0.93 (0.80, 1.09) | 0.367 | 1.05 (0.94, 1.17) | 0.434 | 0.99 (0.82, 1.19) | 0.926 |
| C2–7 SVA | 0.91 (0.82, 1.01) | 0.089 | 1.06 (0.94, 1.20) | 0.356 | 0.93 (0.84, 1.03) | 0.169 | 0.94 (0.82, 1.09) | 0.419 |
| LL | 0.89 (0.80, 0.99) | 0.043 * | 1.11 (0.98, 1.25) | 0.098 | 0.95 (0.87, 1.04) | 0.300 | 1.01 (0.87, 1.18) | 0.874 |
| LLL (L4-S1) | 0.96 (0.87, 1.07) | 0.484 | 0.91 (0.80, 1.04) | 0.167 | 0.94 (0.84, 1.05) | 0.282 | 0.95 (0.85, 1.07) | 0.422 |
| TL junction (T10-L2) | 1.53 (1.23, 1.90) | <0.001 * | 1.35 (1.13, 1.61) | 0.001 * | 1.35 (1.16, 1.57) | <0.001 * | 1.61 (1.23, 2.10) | 0.001 * |
| SVA | 1.00 (0.97, 1.04) | 0.974 | 1.01 (0.97, 1.04) | 0.731 | 0.99 (0.95, 1.03) | 0.599 | 1.02 (0.98, 1.06) | 0.249 |
| SS | 1.11 (0.94, 1.31) | 0.223 | 0.98 (0.83, 1.15) | 0.772 | 1.06 (0.91, 1.25) | 0.453 | 0.97 (0.78, 1.20) | 0.757 |
| PT | 0.97 (0.90, 1.06) | 0.512 | 0.93 (0.84, 1.03) | 0.158 | 0.92 (0.85, 0.99) | 0.036 * | 1.05 (0.94, 1.17) | 0.373 |
| Item | Age ≤ 72 y/o (n = 89) | Age > 72 y/o (n = 72) | Nonobese (n = 93) | Obese (n = 68) | ||||
|---|---|---|---|---|---|---|---|---|
| OR (95% CI) | p Value | OR (95% CI) | p Value | OR (95% CI) | p Value | OR (95% CI) | p Value | |
| Age | - | - | - | - | 0.88 (0.74, 1.05) | 0.153 | 0.99 (0.88, 1.13) | 0.914 |
| BMI | 0.99 (0.89, 1.11) | 0.913 | 1.16 (0.96, 1.40) | 0.120 | - | - | - | - |
| CL | 0.93 (0.87, 0.99) | 0.047 * | 0.95 (0.86, 1.05) | 0.342 | 0.95 (0.86, 1.04) | 0.268 | 0.92 (0.85, 1.002) | 0.056 |
| C7 slope | 1.08 (0.99, 1.19) | 0.086 | 0.99 (0.86, 1.15) | 0.956 | 1.13 (0.98, 1.29) | 0.086 | 0.98 (0.85, 1.12) | 0.770 |
| C2–7 SVA | 0.94 (0.87, 1.01) | 0.111 | 0.98 (0.87, 1.1) | 0.692 | 0.85 (0.76, 0.96) | 0.007 * | 0.99 (0.89, 1.11) | 0.853 |
| LL | 0.95 (0.87, 1.02) | 0.169 | 1.05 (0.94, 1.17) | 0.377 | 0.94 (0.87, 1.03) | 0.182 | 0.98 (0.87, 1.11) | 0.729 |
| LLL (L4-S1) | 1.00 (0.92, 1.09) | 0.950 | 1.01 (0.92, 1.10) | 0.897 | 0.96 (0.88, 1.06) | 0.412 | 0.95 (0.86, 1.06) | 0.376 |
| TL junction (T10-L2) | 1.24 (1.11, 1.38) | <0.001 * | 1.18 (1.07, 1.30) | 0.001 * | 1.26 (1.12, 1.41) | <0.001 * | 1.40 (1.17, 1.69) | <0.001 * |
| SVA | 0.99 (0.97, 1.02) | 0.630 | 1.01 (0.98, 1.04) | 0.674 | 0.96 (0.92, 1.01) | 0.095 | 1.00 (0.98, 1.04) | 0.750 |
| SS | 1.04 (0.92, 1.18) | 0.490 | 0.95 (0.81, 1.11) | 0.524 | 1.08 (0.94, 1.24) | 0.256 | 1.04 (0.87, 1.24) | 0.638 |
| PT | 1.02 (0.96, 1.09) | 0.517 | 0.95 (0.87, 1.04) | 0.289 | 0.97 (0.9, 1.04) | 0.363 | 1.03 (0.94, 1.12) | 0.572 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chen, S.-W.; Wu, W.-T.; Lee, R.-P.; Yu, T.-C.; Chen, I.-H.; Wang, J.-H.; Yeh, K.-T. Correlations between Sagittal Parameters and Functional Scores in 65-Year-Old Osteoporotic Females with Vertebral Body Fracture under Low-Energy Mechanism. J. Clin. Med. 2024, 13, 774. https://doi.org/10.3390/jcm13030774
Chen S-W, Wu W-T, Lee R-P, Yu T-C, Chen I-H, Wang J-H, Yeh K-T. Correlations between Sagittal Parameters and Functional Scores in 65-Year-Old Osteoporotic Females with Vertebral Body Fracture under Low-Energy Mechanism. Journal of Clinical Medicine. 2024; 13(3):774. https://doi.org/10.3390/jcm13030774
Chicago/Turabian StyleChen, Szu-Wei, Wen-Tien Wu, Ru-Ping Lee, Tzai-Chiu Yu, Ing-Ho Chen, Jen-Hung Wang, and Kuang-Ting Yeh. 2024. "Correlations between Sagittal Parameters and Functional Scores in 65-Year-Old Osteoporotic Females with Vertebral Body Fracture under Low-Energy Mechanism" Journal of Clinical Medicine 13, no. 3: 774. https://doi.org/10.3390/jcm13030774
APA StyleChen, S.-W., Wu, W.-T., Lee, R.-P., Yu, T.-C., Chen, I.-H., Wang, J.-H., & Yeh, K.-T. (2024). Correlations between Sagittal Parameters and Functional Scores in 65-Year-Old Osteoporotic Females with Vertebral Body Fracture under Low-Energy Mechanism. Journal of Clinical Medicine, 13(3), 774. https://doi.org/10.3390/jcm13030774











