The Trochlear Paradox in Native Knees and Its Potential Impact on Total Knee Arthroplasty: An MRI-Based Correlation Study Investigating the Effect of Varying Posterior Femoral Condyle Angles on the Patellofemoral Joint
Abstract
:1. Introduction
2. Methods
2.1. Aim of the Study
2.2. Patient Collective
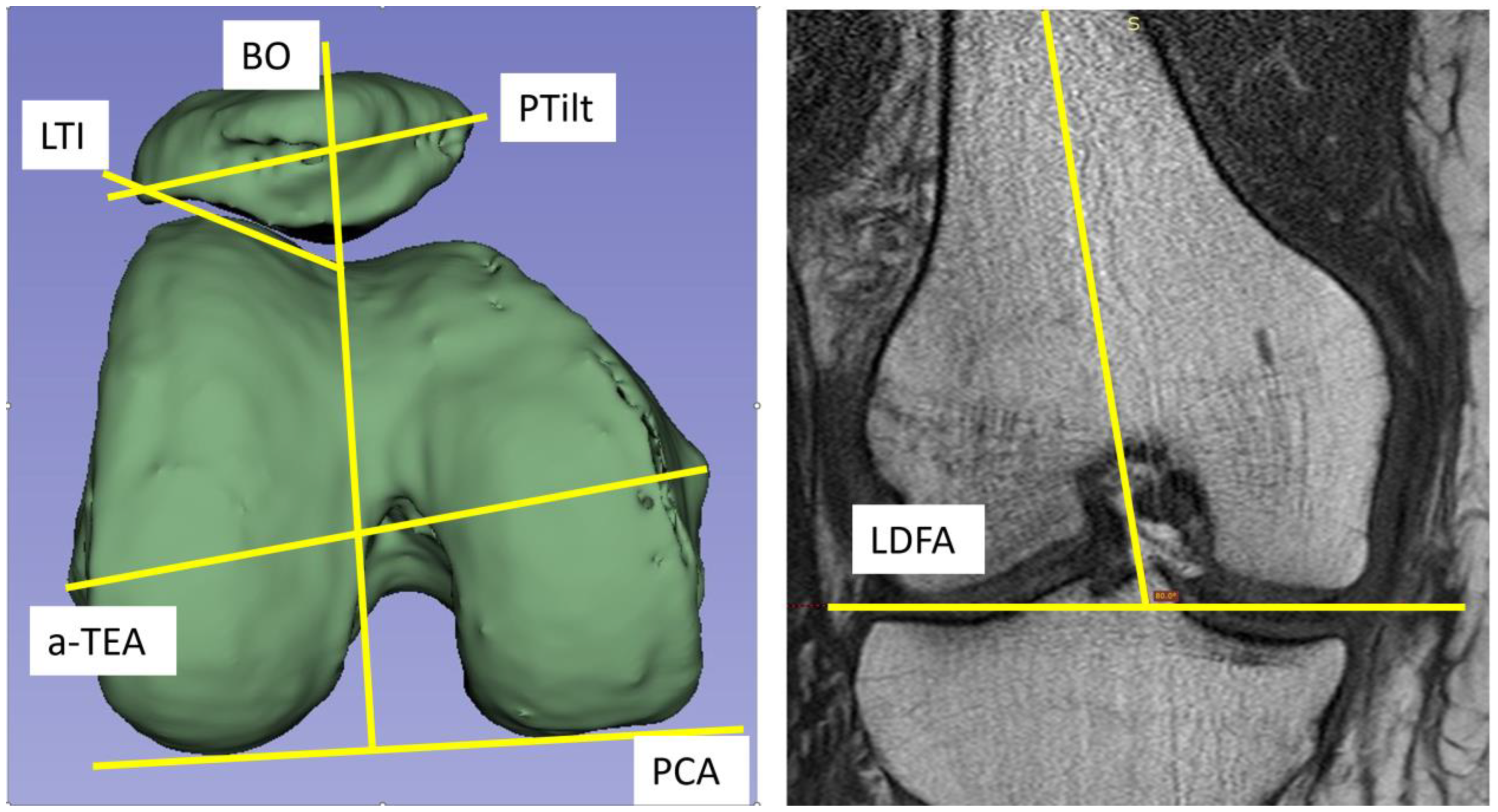
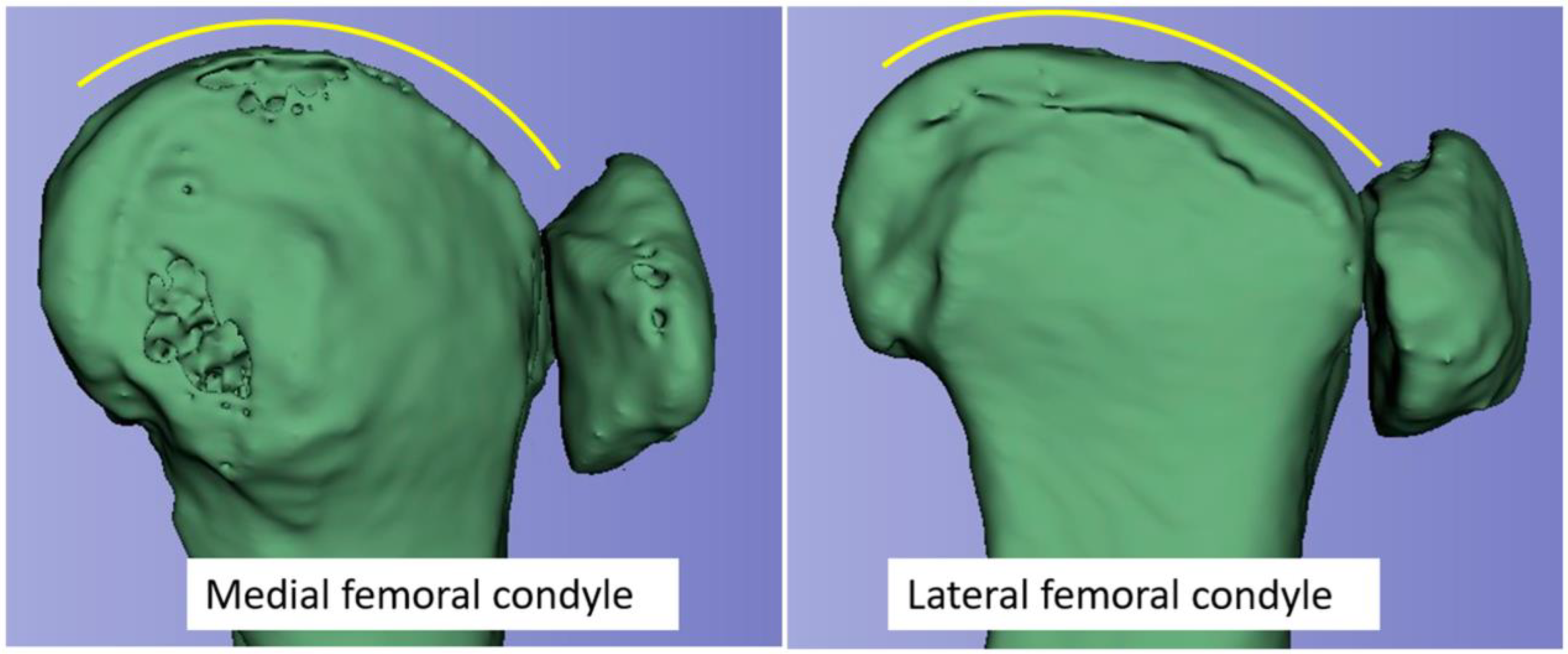
2.3. Radiological Measurements
2.4. Statistical Analysis
2.5. Language
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
List of Abbreviations
| TKA | Total knee arthroplasty |
| TKR | Total knee replacement |
| LDFA | Lateral distal condylar angle |
| PCA | Posterior condylar angle |
| PTilt | Patella tilt |
| LTI | Lateral trochlear angle |
| BO | Bisect offset |
| TEA | Transepicondylar line |
| a-TEA | Anatomical transepicondylar line |
References
- Ranawat, A.S.; Ranawat, C.S.; Elkus, M.; Rasquinha, V.J.; Rossi, R.; Babhulkar, S. Total knee arthroplasty for severe valgus deformity. JBJS 2005, 87, 271–284. [Google Scholar]
- Bourne, R.B.; Chesworth, B.M.; Davis, A.M.; Mahomed, N.N.; Charron, K.D. Patient satisfaction after total knee arthroplasty: Who is satisfied and who is not? Clin. Orthop. Relat. Res. 2010, 468, 57–63. [Google Scholar] [CrossRef] [PubMed]
- Ghomrawi, H.M.K.; Lee, L.Y.; Nwachukwu, B.U.; Jain, D.; Wright, T.; Padgett, D.; Bozic, K.J.; Lyman, S. Preoperative Expectations Associated with Postoperative Dissatisfaction after Total Knee Arthroplasty: A Cohort Study. J. Am. Acad. Orthop. Surg. 2020, 28, e145–e150. [Google Scholar] [CrossRef]
- Parvizi, J.; Nunley, R.M.; Berend, K.R.; Lombardi, A.V., Jr.; Ruh, E.L.; Clohisy, J.C.; Hamilton, W.G.; Della Valle, C.J.; Barrack, R.L. High level of residual symptoms in young patients after total knee arthroplasty. Clin. Orthop. Relat. Res. 2014, 472, 133–137. [Google Scholar] [CrossRef] [PubMed]
- Berger, R.A.; Rubash, H.E.; Seel, M.J.; Thompson, W.H.; Crossett, L.S. Determining the rotational alignment of the femoral component in total knee arthroplasty using the epicondylar axis. Clin. Orthop. Relat. Res. 1993, 286, 40–47. [Google Scholar] [CrossRef]
- Victor, J. Rotational alignment of the distal femur: A literature review. Orthop. Traumatol. Surg. Res. 2009, 95, 365–372. [Google Scholar] [CrossRef] [PubMed]
- Sappey-Marinier, E.; Pauvert, A.; Batailler, C.; Swan, J.; Cheze, L.; Servien, E.; Lustig, S. Kinematic versus mechanical alignment for primary total knee arthroplasty with minimum 2 years follow-up: A systematic review. SICOT J. 2020, 6, 18. [Google Scholar] [CrossRef] [PubMed]
- Daines, B.K.; Dennis, D.A. Gap balancing vs. measured resection technique in total knee arthroplasty. Clin. Orthop. Surg. 2014, 6, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Howell, S.M.; Roth, J.D.; Hull, M.L. Kinematic Alignment in Total Knee Arthroplasty Definition, History, Principle, Surgical Technique, and Results of an Alignment Option for TKA. Principle, Surgical Technique, and Results of an Alignment Option for TKA. Arthropaedia 2014, 1, 44–53. [Google Scholar]
- Karasavvidis, T.; Pagan Moldenhauer, C.A.; Haddad, F.S.; Hirschmann, M.T.; Pagnano, M.W.; Vigdorchik, J.M. Current Concepts in Alignment in Total Knee Arthroplasty. J. Arthroplast. 2023, 38, S29–S37. [Google Scholar] [CrossRef]
- Rosa, S.B.; Hazratwala, K.; Wilkinson, M.P.R. Mismatch between trochlear coronal alignment of arthritic knees and currently available prosthesis: A morphological analysis of 4116 knees and 45 implant designs. Knee Surg. Sports Traumatol. Arthrosc. 2022, 31, 3116–3123. [Google Scholar] [CrossRef] [PubMed]
- Elias, J.J.; Soehnlen, N.T.; Guseila, L.M.; Cosgarea, A.J. Dynamic tracking influenced by anatomy in patellar instability. Knee 2016, 23, 450–455. [Google Scholar] [CrossRef] [PubMed]
- Wibeeg, G. Roentgenographs and Anatomic Studies on the Femoropatellar Joint: With Special Reference to Chondromalacia Patellae. Acta Orthop. Scand. 1941, 12, 319–410. [Google Scholar] [CrossRef]
- Freeman, M.A.R.; Pinskerova, V. The Movement of the Knee Studied by Magnetic Resonance Imaging. Clin. Orthop. Relat. Res. 2003, 410, 35–43. [Google Scholar] [CrossRef] [PubMed]
- Liao, T.C.; Jergas, H.; Tibrewala, R.; Bahroos, E.; Link, T.M.; Majumdar, S.; Souza, R.B.; Pedoia, V. Longitudinal analysis of the contribution of 3D patella and trochlear bone shape on patellofemoral joint osteoarthritic features. J. Orthop. Res. 2021, 39, 506–515. [Google Scholar] [CrossRef] [PubMed]
- Wheatley, M.G.A.; Rainbow, M.J.; Clouthier, A.L. Patellofemoral Mechanics: A Review of Pathomechanics and Research Approaches. Curr. Rev. Musculoskelet. Med. 2020, 13, 326–337. [Google Scholar] [CrossRef] [PubMed]
- Qiu, L.; Li, J.; Sheng, B.; Yang, H.; Xiao, Z.; Lv, F.; Lv, F. Patellar shape is associated with femoral trochlear morphology in individuals with mature skeletal development. BMC Musculoskelet. Disord. 2022, 23, 56. [Google Scholar] [CrossRef]
- Maine, S.; Ngo-Nguyen, C.; Barzan, M.; Stockton, C.; Modenese, L.; Lloyd, D.; Carty, C. Bisect offset ratio and cartilaginous sulcus angle are good combined predictors of recurrent patellar dislocation in children and adolescents. J. ISAKOS 2021, 6, 265–270. [Google Scholar] [CrossRef]
- Hungerford, D.S.; Krackow, K.A. Total joint arthroplasty of the knee. Clin. Orthop. Relat. Res. 1985, 192, 23–33. [Google Scholar] [CrossRef]
- Krackow, K.A.H.D. Anatomy and kinetics of the normal knee. In Total Knee Arthroplasty: A Comprehensive Approach; Hungerford, D.S., Krackow, K.A., Kenna, R.V., Eds.; William & Wilkins: Baltimore, MD, USA, 1984; pp. 5–19. [Google Scholar]
- Ficat, R.P. Disorders of the Patello-Femoral Joint; Ficat, R.P., Hungerford, D.S., Eds.; Williams & Wilkins: Baltimore, MD, USA, 1977. [Google Scholar]
- Dejour, H.; Walch, G.; Nove-Josserand, L.; Guier, C. Factors of patellar instability: An anatomic radiographic study. Knee Surg. Sports Traumatol. Arthrosc. 1994, 2, 19–26. [Google Scholar] [CrossRef]
- Hofmann, A.A.; Tkach, T.K.; Evanich, C.J.; Camargo, M.P.; Zhang, Y. Patellar component medialization in total knee arthroplasty. J. Arthroplast. 1997, 12, 155–160. [Google Scholar] [CrossRef] [PubMed]
- Kulkarni, S.K.; Freeman, M.A.; Poal-Manresa, J.C.; Asencio, J.I.; Rodriguez, J.J. The patello-femoral joint in total knee arthroplasty: Is the design of the trochlea the critical factor? Knee Surg. Sports Traumatol. Arthrosc. 2001, 9 (Suppl. S1), S8–S12. [Google Scholar] [CrossRef] [PubMed]
- Goodfellow, J.; Hungerford, D.S.; Zindel, M. Patello-femoral joint mechanics and pathology. 1. Functional anatomy of the patello-femoral joint. J. Bone Jt. Surg. Br. 1976, 58, 287–290. [Google Scholar] [CrossRef] [PubMed]
- Smidt, G.L. Biomechanical analysis of knee flexion and extension. J. Biomech. 1973, 6, 79–92. [Google Scholar] [CrossRef] [PubMed]
- Hallen, L.G.; Lindahl, O. The “screw-home” movement in the knee-joint. Acta Orthop. Scand. 1966, 37, 97–106. [Google Scholar] [CrossRef] [PubMed]
- Menschik, A. Mechanik des Kniegelenkes. 1 Mechanics of the knee-joint. 1 (author’s transl). Z. Orthop. Ihre Grenzgeb. 1974, 112, 481–495. [Google Scholar] [PubMed]
- Roger, J.; Lustig, S.; Cerciello, S.; Bruno, C.F.; Neyret, P.; Servien, E. Short lateral posterior condyle is associated with trochlea dysplasia and patellar dislocation. Knee Surg. Sports Traumatol. Arthrosc. 2019, 27, 731–739. [Google Scholar] [CrossRef]
- Woiczinski, M.; Kistler, M.; Schroder, C.; Braun, C.; Weber, P.; Muller, P.E.; Jansson, V.; Steinbruck, A. TKA design-integrated trochlea groove rotation reduces patellofemoral pressure. Knee Surg. Sports Traumatol. Arthrosc. 2019, 27, 1680–1692. [Google Scholar] [CrossRef]
- Kebbach, M.; Mick, E.; Kirschner, S.; Luetzner, J.; Bader, R. Intraoperative analysis of patellofemoral joint morphology before and after total knee arthroplasty: A feasibility study. Orthopadie 2022, 51, 580–589. [Google Scholar] [CrossRef]
- Steinbrück, A.; Schröder, C.; Woiczinski, M.; Fottner, A.; Müller, P.E.; Jansson, V. The effect of trochlea tilting on patellofemoral contact patterns after total knee arthroplasty: An in vitro study. Arch. Orthop. Trauma Surg. 2014, 134, 867–872. [Google Scholar] [CrossRef]


| Variable | N | Average | Std-Dev. | Min | Max | LDFA | PCA | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| LDFA [°] | 94 | 82.35 | 1.81 | 78.3 | 86.6 | Pearson correlation | two-side p-value | N | Pearson correlation | two-side p-value | N |
| PCA [°] | 100 | 6.49 | 2.02 | 2.4 | 10.6 | ||||||
| LTI [°] | 99 | 19.58 | 3.87 | 10 | 28 | 0.129 | 0.219 | 93 | −0.319 | 0.001 | 99 |
| PTilt [°] | 94 | 10.31 | 4.04 | 1 | 18 | −0.100 | 0.350 | 89 | 0.428 | <0.001 | 94 |
| BO [%] | 94 | 58.20 | 6.00 | 45.6 | 73.8 | 0.013 | 0.902 | 88 | 0.330 | 0.001 | 94 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Röttinger, T.; Lisitano, L.; Abelmann-Brockmann, J.; Rau, K.; Koenemann, N.; Fenwick, A.; Mayr, E.; Röttinger, H. The Trochlear Paradox in Native Knees and Its Potential Impact on Total Knee Arthroplasty: An MRI-Based Correlation Study Investigating the Effect of Varying Posterior Femoral Condyle Angles on the Patellofemoral Joint. J. Clin. Med. 2024, 13, 790. https://doi.org/10.3390/jcm13030790
Röttinger T, Lisitano L, Abelmann-Brockmann J, Rau K, Koenemann N, Fenwick A, Mayr E, Röttinger H. The Trochlear Paradox in Native Knees and Its Potential Impact on Total Knee Arthroplasty: An MRI-Based Correlation Study Investigating the Effect of Varying Posterior Femoral Condyle Angles on the Patellofemoral Joint. Journal of Clinical Medicine. 2024; 13(3):790. https://doi.org/10.3390/jcm13030790
Chicago/Turabian StyleRöttinger, Timon, Leonard Lisitano, Johanna Abelmann-Brockmann, Kim Rau, Nora Koenemann, Annabel Fenwick, Edgar Mayr, and Heinz Röttinger. 2024. "The Trochlear Paradox in Native Knees and Its Potential Impact on Total Knee Arthroplasty: An MRI-Based Correlation Study Investigating the Effect of Varying Posterior Femoral Condyle Angles on the Patellofemoral Joint" Journal of Clinical Medicine 13, no. 3: 790. https://doi.org/10.3390/jcm13030790
APA StyleRöttinger, T., Lisitano, L., Abelmann-Brockmann, J., Rau, K., Koenemann, N., Fenwick, A., Mayr, E., & Röttinger, H. (2024). The Trochlear Paradox in Native Knees and Its Potential Impact on Total Knee Arthroplasty: An MRI-Based Correlation Study Investigating the Effect of Varying Posterior Femoral Condyle Angles on the Patellofemoral Joint. Journal of Clinical Medicine, 13(3), 790. https://doi.org/10.3390/jcm13030790





