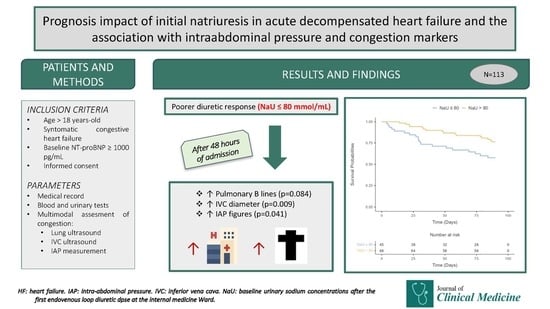
Prognostic Impact of Induced Natriuresis in Acute Decompensated Heart Failure and Its Association with Intraabdominal Pressure and Other Congestion Markers: A Multimodal Approach to Congestion Assessment
Abstract
1. Introduction
2. Materials and Methods
3. Results
3.1. Baseline Characteristics
3.2. Multimodal Assessment of Congestion and Intraabdominal Pressure
3.3. Outcomes
4. Discussion
4.1. Natriuresis and Decongestion in Acute Heart Failure
4.2. Clinical Implications
5. Conclusions
6. Limitations
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- McDonagh, T.A.; Metra, M.; Adamo, M.; Gardner, R.S.; Baumbach, A.; Böhm, M.; Burri, H.; Butler, J.; Čelutkienė, J.; Chioncel, O.; et al. 2021 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur. Heart J. 2021, 42, 3599–3726. [Google Scholar] [CrossRef]
- Boorsma, E.M.; Ter Maaten, J.M.; Damman, K.; Dinh, W.; Gustafsson, F.; Goldsmith, S.; Burkhoff, D.; Zannad, F.; Udelson, J.E.; Voors, A.A. Congestion in heart failure: A contemporary look at physiology, diagnosis and treatment. Nat. Rev. Cardiol. 2020, 17, 641–655. [Google Scholar] [CrossRef]
- Costanzo, M.R.; Jessup, M. Treatment of congestion in heart failure with diuretics and extracorporeal therapies: Effects on symptoms, renal function, and prognosis. Heart Fail. Rev. 2012, 17, 313–324. [Google Scholar] [CrossRef]
- Rubio-Gracia, J.; Demissei, B.G.; Ter Maaten, J.M.; Cleland, J.G.; O’Connor, C.M.; Metra, M.; Ponikowski, P.; Teerlink, J.R.; Cotter, G.; Davison, B.A.; et al. Prevalence, predictors and clinical outcome of residual congestion in acute decompensated heart failure. Int. J. Cardiol. 2018, 258, 185–191. [Google Scholar] [CrossRef]
- Lala, A.; McNulty, S.E.; Mentz, R.J.; Dunlay, S.M.; Vader, J.M.; AbouEzzeddine, O.F.; DeVore, A.D.; Khazanie, P.; Redfield, M.M.; Goldsmith, S.R.; et al. Relief and recurrence of congestion during and after hospitalization for acute heart failure insights from diuretic optimization strategy evaluation in acute decompensated heart failure (DOSE-AHF) and cardiorenal rescue study in acute decompensated heart failure (CARESS-HF). Circ. Heart Fail. 2015, 8, 741–748. [Google Scholar] [CrossRef]
- Ambrosy, A.P.; Pang, P.S.; Khan, S.; Konstam, M.A.; Fonarow, G.C.; Traver, B.; Maggioni, A.P.; Cook, T.; Swedberg, K.; Burnett, J.C., Jr. Clinical course and predictive value of congestion during hospitalization in patients admitted for worsening signs and symptoms of heart failure with reduced ejection fraction: Findings from the EVEREST trial. Eur. Heart J. 2013, 34, 835–843. [Google Scholar] [CrossRef]
- Januzzi, J.L.; van Kimmenade, R.; Lainchbury, J.; Bayes-Genis, A.; Ordonez-Llanos, J.; Santalo-Bel, M.; Pinto, Y.M.; Richards, M. NT-proBNP testing for diagnosis and short-term prognosis in acute destabilized heart failure: An international pooled analysis of 1256 patients: The International Collaborative of NT-proBNP Study. Eur. Heart J. 2006, 27, 330–337. [Google Scholar] [CrossRef]
- Núñez, J.; Llàcer, P.; Bertomeu-González, V.; Bosch, M.J.; Merlos, P.; García-Blas, S.; Montagud, V.; Bodí, V.; Bertomeu-Martínez, V.; Pedrosa, V.; et al. Carbohydrate Antigen-125-Guided Therapy in Acute Heart Failure: CHANCE-HF: A Randomized Study. JACC Heart Fail. 2016, 4, 833–843. [Google Scholar] [CrossRef]
- Spevack, R.; Al Shukairi, M.; Jayaraman, D.; Dankoff, J.; Rudski, L.; Lipes, J. Serial lung and IVC ultrasound in the assessment of congestive heart failure. Crit Ultrasound J. 2017, 9, 7. [Google Scholar] [CrossRef]
- Li, Y.; Ai, H.; Ma, N.; Li, P.; Ren, J. Lung ultrasound-guided treatment for heart failure: An updated meta-analysis and trial sequential analysis. Front. Cardiovasc. Med. 2022, 9, 943633. [Google Scholar] [CrossRef]
- Brinkley, D.M., Jr.; Burpee, L.J.; Chaudhry, S.P.; Smallwood, J.A.; Lindenfeld, J.; Lakdawala, N.K.; Desai, A.S.; Stevenson, L.W. Spot Urine Sodium as Triage for Effective Diuretic Infusion in an Ambulatory Heart Failure Unit. J. Card. Fail. 2018, 24, 349–354. [Google Scholar] [CrossRef]
- Luk, A.; Groarke, J.D.; Desai, A.S.; Mahmood, S.S.; Gopal, D.M.; Joyce, E.; Shah, S.P.; Lindenfeld, J.; Stevenson, L.; Lakdawala, N.K. First spot urine sodium after initial diuretic identifies patients at high risk for adverse outcome after heart failure hospitalization. Am. Heart J. 2018, 203, 95–100. [Google Scholar] [CrossRef]
- Testani, J.M.; Brisco, M.A.; Turner, J.M.; Spatz, E.S.; Bellumkonda, L.; Parikh, C.R.; Tang, W.H. Loop diuretic efficiency: A metric of diuretic responsiveness with prognostic importance in acute decompensated heart failure. Circ. Heart Fail. 2014, 7, 261–270. [Google Scholar] [CrossRef]
- Rao, V.S.; Ivey-Miranda, J.B.; Cox, Z.L.; Riello, R.; Griffin, M.; Fleming, J.; Soucier, R.; Sangkachand, P.; O’Brien, M.; LoRusso, F.; et al. Natriuretic Equation to Predict Loop Diuretic Response in Patients With Heart Failure. J. Am. Coll. Cardiol. 2021, 77, 695–708. [Google Scholar] [CrossRef]
- Damman, K.; Ter Maaten, J.M.; Coster, J.E.; Krikken, J.A.; van Deursen, V.M.; Krijnen, H.K.; Hofman, M.; Nieuwland, W.; van Veldhuisen, D.J.; Voors, A.A.; et al. Clinical importance of urinary sodium excretion in acute heart failure. Eur. J. Heart Fail. 2020, 22, 1438–1447. [Google Scholar] [CrossRef]
- Hodson, D.Z.; Griffin, M.; Mahoney, D.; Raghavendra, P.; Ahmad, T.; Turner, J.; Wilson, F.P.; Tang, W.H.W.; Rao, V.S.; Collins, S.P.; et al. Natriuretic Response Is Highly Variable and Associated With 6-Month Survival: Insights From the ROSE-AHF Trial. JACC Heart Fail. 2019, 7, 383–391. [Google Scholar] [CrossRef]
- Biegus, J.; Zymliński, R.; Testani, J.; Marciniak, D.; Zdanowicz, A.; Jankowska, E.A.; Banasiak, W.; Ponikowski, P. Renal profiling based on estimated glomerular filtration rate and spot urine sodium identifies high-risk acute heart failure patients. Eur. J. Heart Fail. 2021, 23, 729–739. [Google Scholar] [CrossRef]
- Ter Maaten, J.M.; Beldhuis, I.E.; van der Meer, P.; Krikken, J.A.; Coster, J.E.; Nieuwland, W.; van Veldhuisen, D.J.; Voors, A.A.; Damman, K. Natriuresis-guided therapy in acute heart failure: Rationale and design of the Pragmatic Urinary Sodium-based treatment algorithm in Acute Heart Failure (PUSH-AHF) trial. Eur. J. Heart Fail. 2022, 24, 385–392. [Google Scholar] [CrossRef]
- Ter Maaten, J.M.; Beldhuis, I.E.; van der Meer, P.; Krikken, J.A.; Postmus, D.; Coster, J.E.; Nieuwland, W.; van Veldhuisen, D.J.; Voors, A.A.; Damman, K. Natriuresis-guided diuretic therapy in acute heart failure: A pragmatic randomized trial. Nat. Med. 2023, 29, 2625–2632. [Google Scholar] [CrossRef]
- Stevens, P.E.; Levin, A. Kidney Disease: Improving Global Outcomes Chronic Kidney Disease Guideline Development Work Group Members. Evaluation and management of chronic kidney disease: Synopsis of the kidney disease: Improving global outcomes 2012 clinical practice guideline. Ann. Intern. Med. 2013, 158, 825–830. [Google Scholar] [CrossRef]
- Picano, E.; Scali, M.C.; Ciampi, Q.; Lichtenstein, D. Lung Ultrasound for the Cardiologist. JACC Cardiovasc. Imaging 2018, 11, 1692–1705. [Google Scholar] [CrossRef]
- Lichtenstein, D.A.; Mezière, G.A. Relevance of lung ultrasound in the diagnosis of acute respiratory failure: The BLUE protocol. Chest J. 2008, 134, 117–125. [Google Scholar] [CrossRef]
- Levy Adatto, N.; Preisler, Y.; Shetrit, A.; Shepshelovich, D.; Hershkoviz, R.; Isakov, O. Rapid 8-Zone Lung Ultrasound Protocol is Comparable to a Full 12-Zone Protocol for Outcome Prediction in Hospitalized COVID-19 Patients. J. Ultrasound Med. 2022, 41, 1677–1687. [Google Scholar] [CrossRef]
- Rudski, L.G.; Lai, W.W.; Afilalo, J.; Hua, L.; Handschumacher, M.D.; Chandrasekaran, K.; Solomon, S.D.; Louie, E.K.; Schiller, N.B. Guidelines for the echocardiographic assessment of the right heart in adults: A report from the American Society of Echocardiography endorsed by the European Association of Echocardiography, a registered branch of the European Society of Cardiology, and the Canadian Society of Echocardiography. J. Am. Soc. Echocardiogr. 2010, 23, 685–713. [Google Scholar] [CrossRef]
- Zymliński, R.; Biegus, J.; Sokolski, M.; Jankowska, E.A.; Banasiak, W.; Ponikowski, P. Validation of transurethral intra abdominal pressure measurement in acute heart failure. Pol. Arch. Intern. Med. 2018, 128, 403–405. [Google Scholar] [CrossRef]
- Verbrugge, F.H.; Martens, P.; Dauw, J.; Nijst, P.; Meekers, E.; Augusto, S.N., Jr.; Ter Maaten, J.M.; Damman, K.; Filippatos, G.; Lassus, J.; et al. Natriuretic Response to Acetazolamide in Patients With Acute Heart Failure and Volume Overload. J. Am. Coll. Cardiol. 2023, 81, 2013–2024. [Google Scholar] [CrossRef]
- Cuschieri, S. The STROBE guidelines. Saudi J. Anaesth. 2019, 13 (Suppl. 1), S31–S34. [Google Scholar] [CrossRef]
- Rivas-Lasarte, M.; Álvarez-García, J.; Fernández-Martínez, J.; Maestro, A.; López-López, L.; Solé-González, E.; Pirla, M.J.; Mesado, N.; Mirabet, S.; Fluvià, P. Lung ultrasound-guided treatment in ambulatory patients with heart failure: A randomized controlled clinical trial (LUS-HF study). Eur. J. Heart Fail. 2019, 21, 1605–1613. [Google Scholar] [CrossRef]
- Mullens, W.; Dauw, J.; Martens, P.; Verbrugge, F.H.; Nijst, P.; Meekers, E.; Tartaglia, K.; Chenot, F.; Moubayed, S.; Dierckx, R.; et al. Acetazolamide in Acute Decompensated Heart Failure with Volume Overload. N. Engl. J. Med. 2022, 387, 1185–1195. [Google Scholar] [CrossRef]
- Biegus, J.; Zymliński, R.; Sokolski, M.; Todd, J.; Cotter, G.; Metra, M.; Jankowska, E.A.; Banasiak, W.; Ponikowski, P. Serial assessment of spot urine sodium predicts effectiveness of decongestion and outcome in patients with acute heart failure. Eur. J. Heart Fail. 2019, 21, 624–633. [Google Scholar] [CrossRef]
- Verbrugge, F.H.; Dupont, M.; Steels, P.; Grieten, L.; Malbrain, M.; Tang, W.H.; Mullens, W. Abdominal contributions to cardiorenal dysfunction in congestive heart failure. J. Am. Coll. Cardiol. 2013, 62, 485–495. [Google Scholar] [CrossRef] [PubMed]
- Mullens, W.; Abrahams, Z.; Skouri, H.N.; Francis, G.S.; Taylor, D.O.; Starling, R.C.; Paganini, E.; Tang, W.H. Elevated Intra-Abdominal Pressure in Acute Decompensated Heart Failure. A Potential Contributor to Worsening Renal Function? J. Am. Coll. Cardiol. 2008, 51, 300–306. [Google Scholar] [CrossRef] [PubMed]
- Verbrugge, F.H.; Martens, P.; Ameloot, K.; Haemels, V.; Penders, J.; Dupont, M.; Tang, W.H.W.; Droogné, W.; Mullens, W. Acetazolamide to increase natriuresis in congestive heart failure at high risk for diuretic resistance. Eur. J. Heart Fail. 2019, 21, 1415–1422. [Google Scholar] [CrossRef] [PubMed]
- García-Magallón, B.; Cobo-Marcos, M.; Martiarena, A.D.; Hernández, E.M.; Martín Jiménez, M.L.; García, A.M.; De Castro Campos, D.; Martín, P.V.; Terciado, F.H.; González, R.G.; et al. Role of Early Assessment of Diuresis and Natriuresis in Detecting In-Hospital Diuretic Resistance in Acute Heart Failure. Front. Physiol. 2022, 13, 887734. [Google Scholar] [CrossRef]
- Dauw, J.; Lelonek, M.; Zegri-Reiriz, I.; Paredes-Paucar, C.P.; Zara, C.; George, V.; Cobo-Marcos, M.; Knappe, D.; Shchekochikhin, D.; Lekhakul, A.; et al. Rationale and Design of the Efficacy of a Standardized Diuretic Protocol in Acute Heart Failure Study. ESC Heart Fail. 2021, 8, 4685–4692. [Google Scholar] [CrossRef]
- Trullàs, J.C.; Morales-Rull, J.L.; Casado, J.; Carrera-Izquierdo, M.; Sánchez-Marteles, M.; Conde-Martel, A.; Dávila-Ramos, M.F.; Llácer, P.; Salamanca-Bautista, P.; Pérez-Silvestre, J.; et al. Combining loop with thiazide diuretics for decompensated heart failure: The CLOROTIC trial. Eur. Heart J. 2023, 44, 411–421. [Google Scholar] [CrossRef]



| Variable | Total | NaU ≤ 80 | NaU > 80 | p-Value |
|---|---|---|---|---|
| N (%) | 113 (100) | 45 (39.8) | 68 (60.2) | |
| Age (years) | 81.7 ± 8.3 | 82.0 ± 7.3 | 81.5 ± 9.0 | 0.727 |
| Women (%) | 61 (54.0) | 22 (19.5) | 39 (57.4) | 0.377 |
| NYHA | 0.159 | |||
| NYHA I (n [%]) | 20 (17.7) | 6 (13.3) | 14 (20.6) | |
| NYHA II (n [%]) | 65 (57.5) | 24 (53.3) | 41 (60.3) | |
| NYHA III (n [%]) | 26 (23.0) | 13 (28.9) | 13 (19.1) | |
| NYHA IV (n [%]) | 2 (1.8) | 2 (4.4) | 0 (0.0) | |
| LVEF | 0.434 | |||
| HFpEF (n [%]) | 58 (61.1) | 19 (52.8) | 39 (66.1) | |
| HFmrEF (n [%]) | 13 (13.7) | 6 (16.7) | 7 (11.9) | |
| HFrEF (n [%]) | 24 (25.3) | 11 (30.6) | 13 (22.0) | |
| Hypertension (n [%]) | 92 (81.4) | 33 (73.3) | 59 (86.8) | 0.072 |
| Diabetes (n [%]) | 41 (36.3) | 13 (28.9) | 28 (41.2) | 0.184 |
| AF (n [%]) | 75 (66.4) | 30 (66.7) | 45 (66.2) | 0.957 |
| COPD (n [%]) | 22 (19.5) | 13 (28.9) | 9 (13.2) | 0.040 |
| ICD (n [%]) | 30 (26.5) | 16 (35.6) | 14 (20.4) | 0.078 |
| Dyslipidemia (n [%]) | 62 (54.9) | 25 (55.6) | 37 (54.4) | 0.905 |
| eGFR (mL/min) | 51.6 (32.8) | 47.2 (25.9) | 58.1 (56.1) | 0.096 |
| eGFR groups (n [%]) | 0.054 | |||
| eGFRv ≥ 60 (n [%]) | 36 (36.0) | 10 (25.6) | 26 (42.6) | |
| eGFR 30–59 (n [%]) | 49 (49.0) | 25 (64.1) | 24 (39.3) | |
| eGFR < 29 (n [%]) | 15 (15.0) | 4 (4.0) | 11 (18.0) | |
| HF treatment | ||||
| ACEi/ARB (n [%]) | 67 (59.3) | 25 (55.6) | 42 (61.8) | 0.511 |
| Sacubitril/valsartan (n [%]) | 4 (3.5) | 2 (4.4) | 2 (2.9) | 0.672 |
| B-Blockers (n [%]) | 69 (61.1) | 28 (62.2) | 41 (60.3) | 0.837 |
| MRB (n [%]) | 24 (21.2) | 9 (20.0) | 15 (22.1) | 0.793 |
| SGLT2i (n [%]) | 10 (8.8) | 5 (11.1) | 5 (7.4) | 0.491 |
| Diuretics | ||||
| Furosemide (n [%]) | 86 (76.1) | 40 (88.9) | 46 (67.6) | 0.010 |
| Outpatient furosemide dose (mg) | 40 (55) | 40 (53) | 35 (40) | 0.049 |
| HCTZ (n [%]) | 22 (19.5) | 10 (22.2) | 12 (17.6) | 0.549 |
| Laboratory | ||||
| NT-proBNP (pg/mL) | 4898 (10,630) | 6227 (13,835) | 4113 (5384) | 0.056 |
| CA125 (pg/mL) | 38.1 (49.3) | 37.6 (44.9) | 38.7 (52.2) | 0.766 |
| Hemoglobin (g/L) | 11.8 ± 1.8 | 11.8 ± 1.8 | 11.7 ± 1.8 | 0.778 |
| Sodium (mmol/L) | 140 ± 4 | 138 ± 5 | 141 ± 3 | <0.001 |
| Potassium (mmol/L) | 4.1 ± 0.5 | 4.1 ± 0.5 | 4.1 ± 0.5 | 0.828 |
| Chloride (mmol/L) | 99 ± 6 | 97 ± 6 | 100 ± 4 | 0.002 |
| Variable | Baseline | Control at 48 h | ||||
|---|---|---|---|---|---|---|
| NaU ≤ 80 | NaU > 80 | p-Value | NaU ≤ 80 | NaU > 80 | p-Value | |
| B-lines by LUS (n) | 21 (14) | 21 (12) | 0.927 | 15 (17) | 12 (14) | 0.084 |
| IVC diameter (mm) | 21 (7) | 22 (7) | 0.973 | 22 (6) | 18 (5) | 0.009 |
| IVC colapsability < 50% | 38 (86.4) | 49 (75.4) | 0.161 | 32 (72.7) | 38 (59.4) | 0.153 |
| IAP (mmHg) | 15 (6) | 14 (5) | 0.473 | 13 (6) | 11 (5) | 0.041 |
| Natriuresis (mmol/L) | 75 (43) | 84 (55) | 0.042 | |||
| Total IV furosemide dose (mg) | 180 (138) | 140 (80) | 0.100 | |||
| Univariable | Multivariate | |||
|---|---|---|---|---|
| Variable | HR (CI 95%) | p-Value | HR (CI 95%) | p-Value |
| Age (years) | 1.02 (0.97–1.06) | 0.462 | ||
| Gender (male) | 1.49 (0.76–2.89) | 0.243 | ||
| LVEF (%) | 0.57 (0.20–1.59) | 0.285 | ||
| SBP (mmHg) | 0.99 (0.98–1.01) | 0.265 | ||
| DBP (mmHg) | 0.99 (0.97–1.01) | 0.382 | ||
| HR (B.p.m.) | 1.01 (0.99–1.03) | 0.265 | ||
| HTA | 0.71 (0.32–1.57) | 0.402 | ||
| Diabetes | 1.04 (0.52–2.06) | 0.916 | ||
| COPD | 1.75 (0.82–3.74) | 0.147 | ||
| AF | 1.05 (0.52–2.15) | 0.887 | ||
| CID | 1.26 (0.62–2.58) | 0.521 | ||
| Dislipidemia | 1.90 (0.93–3.89) | 0.077 | ||
| Previous use of furosemide | 2.85 (1.01–8.07) | 0.049 | ||
| Previous use of thiazides | 1.21 (0.55–2.66) | 0.642 | ||
| Previous use of MRB | 1.55 (0.75–3.24) | 0.239 | ||
| Previous use of b-blocker | 1.65 (0.79–3.44) | 0.182 | ||
| Previous use of ACEi/ARB | 1.15 (0.58–2.28) | 0.690 | ||
| Previous use of SGLT2i | 1.08 (0.38–3.05) | 0.890 | ||
| Egfr * | 0.39 (0.18–0.86) | 0.020 | ||
| Natriuresis > 80 mEq/L | 0.46 (0.24–0.90) | 0.023 | 0.50 (0.25–1.02) | 0.056 |
| B-lines at baseline * | 1.01 (0.57–1.82) | 0.963 | ||
| B-lines at 48 h * | 0.99 (0.58–1.69) | 0.981 | ||
| IVC diameter at baseline * | 1.02 (0.31–3.38) | 0.979 | ||
| IVC diameter at 48 h * | 2.91 (0.89–9.51) | 0.078 | ||
| IAP at baseline * | 0.73 (0.18–2.97) | 0.663 | ||
| IAP at 48 h * | 2.91 (0.72–11.8) | 0.135 | ||
| NT-proBNP at baseline * | 1.43 (1.07–1.90) | 0.016 | ||
| CA125 at baseline * | 1.40 (0.97–2.04) | 0.073 | 1.44 (0.98–2.10) | 0.059 |
| Haemoglobin at baseline | 0.90 (0.75–1.07) | 0.242 | ||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Crespo-Aznarez, S.; Campos-Saenz de Santamaría, A.; Sánchez-Marteles, M.; Josa-Laorden, C.; Ruiz-Laiglesia, F.; Amores-Arriaga, B.; Garcés-Horna, V.; Tejel-Puisac, R.; Julián-Ansón, M.A.; Giménez-López, I.; et al. Prognostic Impact of Induced Natriuresis in Acute Decompensated Heart Failure and Its Association with Intraabdominal Pressure and Other Congestion Markers: A Multimodal Approach to Congestion Assessment. J. Clin. Med. 2024, 13, 1053. https://doi.org/10.3390/jcm13041053
Crespo-Aznarez S, Campos-Saenz de Santamaría A, Sánchez-Marteles M, Josa-Laorden C, Ruiz-Laiglesia F, Amores-Arriaga B, Garcés-Horna V, Tejel-Puisac R, Julián-Ansón MA, Giménez-López I, et al. Prognostic Impact of Induced Natriuresis in Acute Decompensated Heart Failure and Its Association with Intraabdominal Pressure and Other Congestion Markers: A Multimodal Approach to Congestion Assessment. Journal of Clinical Medicine. 2024; 13(4):1053. https://doi.org/10.3390/jcm13041053
Chicago/Turabian StyleCrespo-Aznarez, Silvia, Amelia Campos-Saenz de Santamaría, Marta Sánchez-Marteles, Claudia Josa-Laorden, Fernando Ruiz-Laiglesia, Beatriz Amores-Arriaga, Vanesa Garcés-Horna, Ruben Tejel-Puisac, María Angel Julián-Ansón, Ignacio Giménez-López, and et al. 2024. "Prognostic Impact of Induced Natriuresis in Acute Decompensated Heart Failure and Its Association with Intraabdominal Pressure and Other Congestion Markers: A Multimodal Approach to Congestion Assessment" Journal of Clinical Medicine 13, no. 4: 1053. https://doi.org/10.3390/jcm13041053
APA StyleCrespo-Aznarez, S., Campos-Saenz de Santamaría, A., Sánchez-Marteles, M., Josa-Laorden, C., Ruiz-Laiglesia, F., Amores-Arriaga, B., Garcés-Horna, V., Tejel-Puisac, R., Julián-Ansón, M. A., Giménez-López, I., Pérez-Calvo, J. I., & Rubio-Gracia, J. (2024). Prognostic Impact of Induced Natriuresis in Acute Decompensated Heart Failure and Its Association with Intraabdominal Pressure and Other Congestion Markers: A Multimodal Approach to Congestion Assessment. Journal of Clinical Medicine, 13(4), 1053. https://doi.org/10.3390/jcm13041053