Epidemiology and Treatment of Surgical Infection after Ankle Arthroscopy: A Systematic Review
Abstract
1. Introduction
2. Materials and Methods
2.1. Search Strategy
2.2. Study Selection
2.3. Data Extraction/Analysis
3. Results
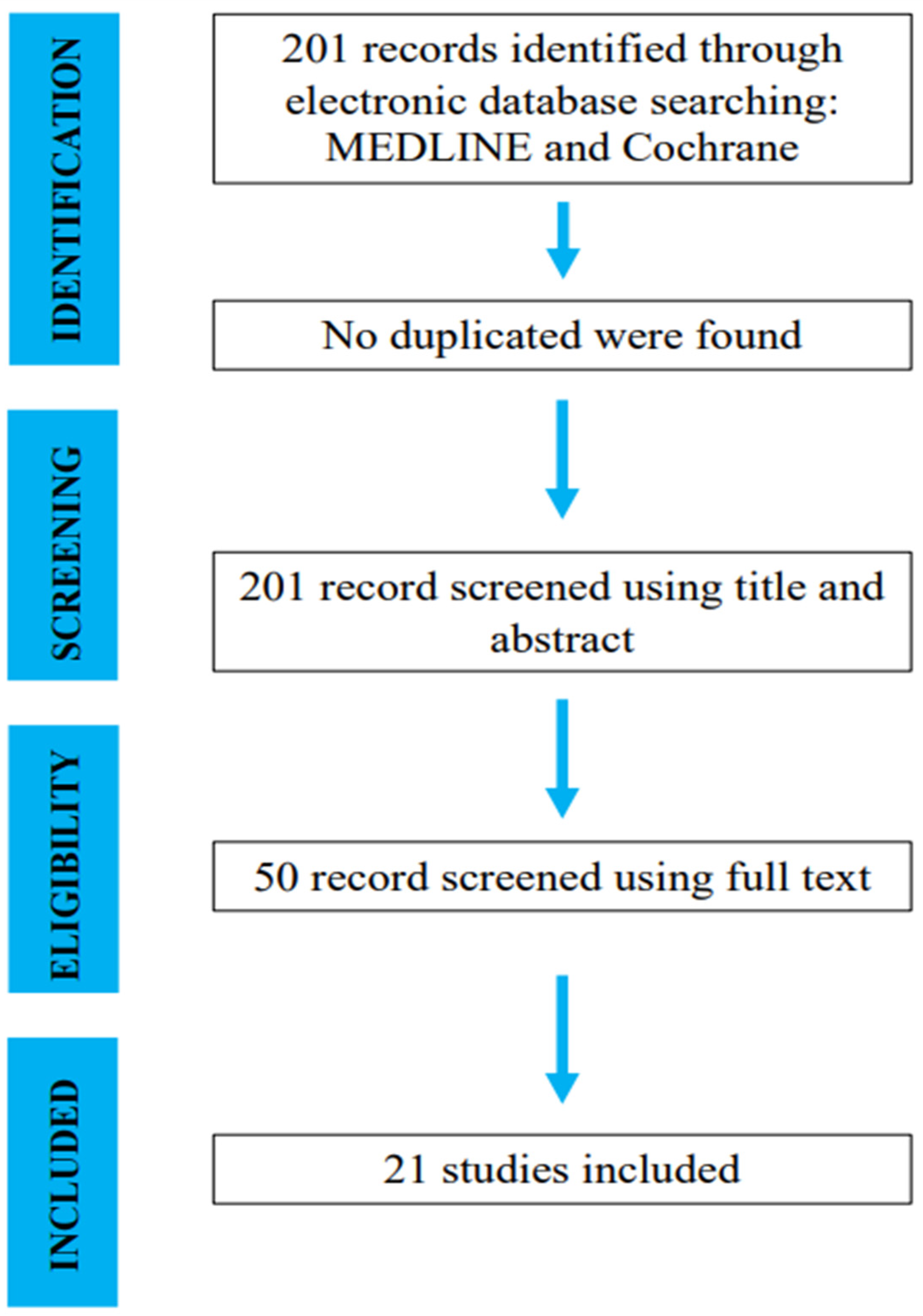
3.1. Search and Literature Selection
3.2. Study Characteristics
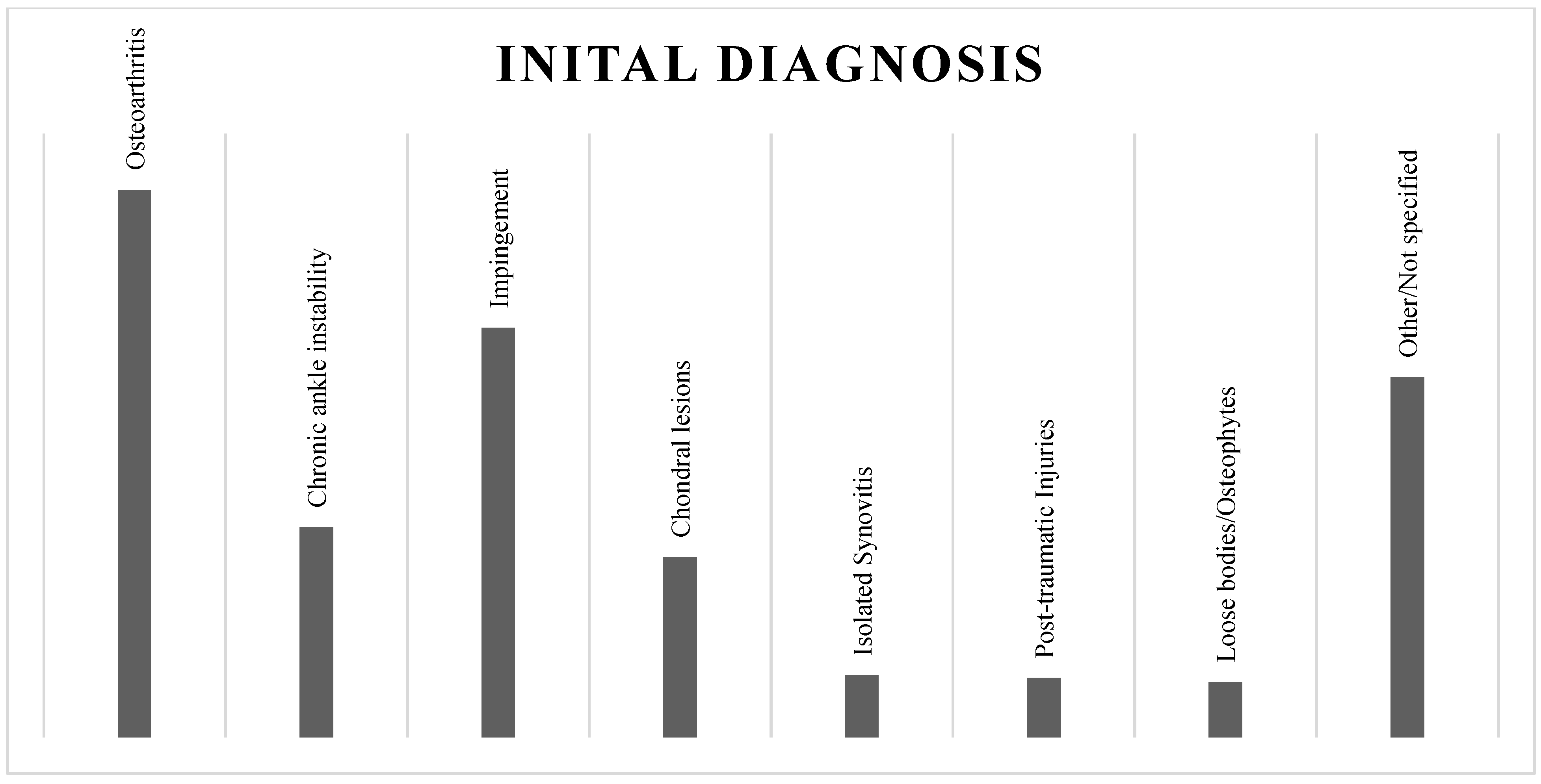
3.3. The Initial Diagnosis
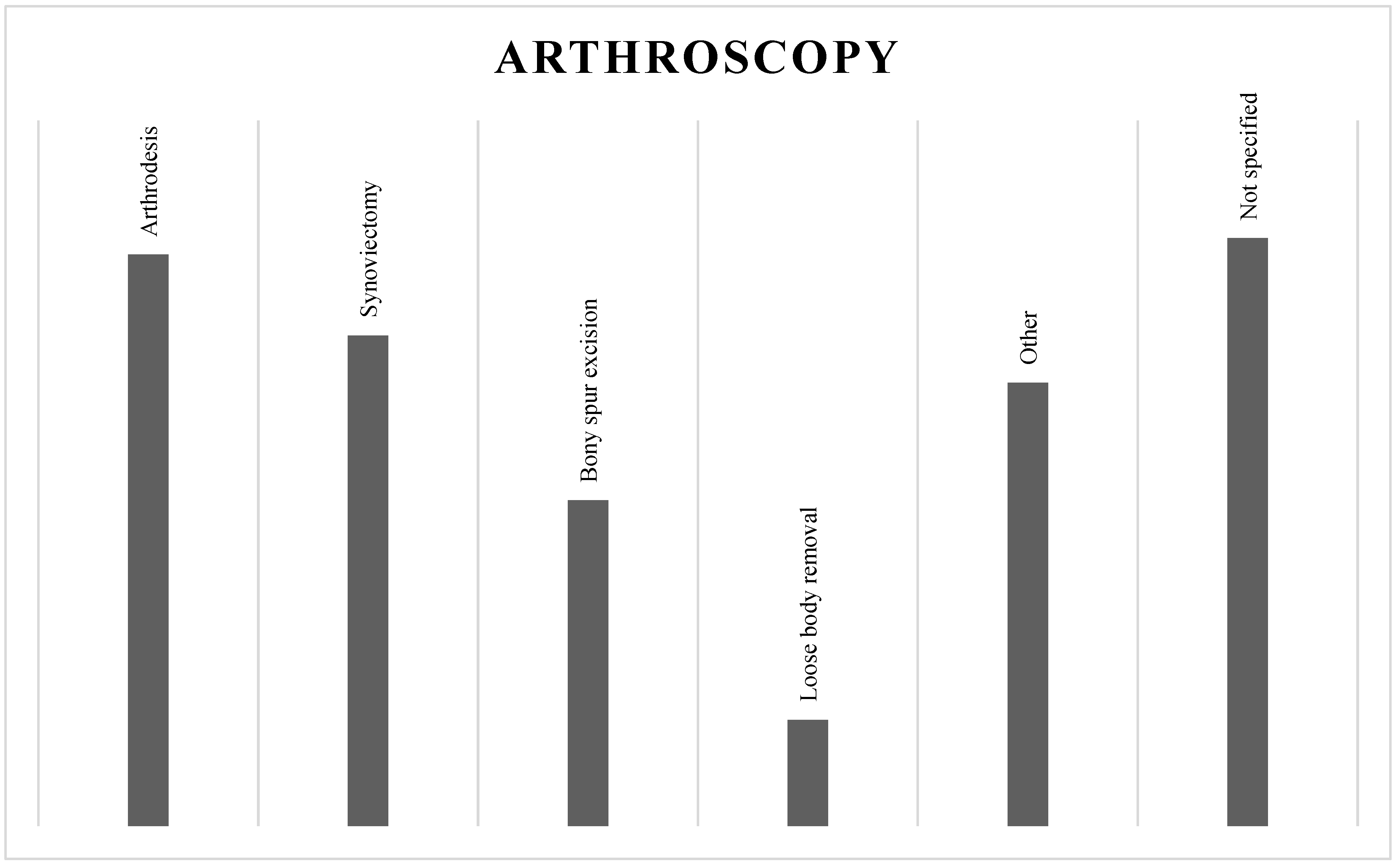
3.4. Ankle Arthroscopy
3.5. Infection Rate
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Takagi, K. The classic. Arthroscope. Kenji Takagi. J. Jap. Orthop. Assoc., 1939. Clin. Orthop. Relat. Res. 1982, 167, 6–8. [Google Scholar]
- Burman, M.S. Arthroscopy or the direct visualization of joints: An experimental cadaver study. 1931. Clin. Orthop. Relat. Res. 2001, 390, 5–9. [Google Scholar] [CrossRef]
- Martin, D.F.; Baker, C.L.; Curl, W.W.; Andrews, J.R.; Robie, D.B.; Haas, A.F. Operative ankle arthroscopy. Long-term followup. Am. J. Sports Med. 1989, 17, 16–23, discussion 23. [Google Scholar] [CrossRef]
- Chaytor, E.R.; Conti, S.F. Arthroscopy of the Foot and Ankle: Current Concepts Review. Foot Ankle Int. 1998, 19, 184–192. [Google Scholar] [CrossRef]
- Hepple, S.; Guha, A. The role of ankle arthroscopy in acute ankle injuries of the athlete. Foot Ankle Clin. 2013, 18, 185–194. [Google Scholar] [CrossRef]
- Ferkel, R.D.; Heath, D.D.; Guhl, J.F. Neurological complications of ankle arthroscopy. Arthroscopy 1996, 12, 200–208. [Google Scholar] [CrossRef]
- Niek van Dijk, C. Anterior and posterior ankle impingement. Foot Ankle Clin. 2006, 11, 663–683. [Google Scholar] [CrossRef]
- Abdelatif, N.M. Combined arthroscopic management of concurrent posterior and anterior ankle pathologies. Knee Surg. Sports Traumatol. Arthrosc. 2014, 22, 2837–2842. [Google Scholar] [CrossRef]
- Ferkel, R.D.; Small, H.N.; Gittins, J.E. Complications in foot and ankle arthroscopy. Clin. Orthop. Relat. Res. 2001, 391, 89–104. [Google Scholar] [CrossRef]
- Arshad, Z.; Aslam, A.; Al Shdefat, S.; Khan, R.; Jamil, O.; Bhatia, M. Complications following ankle arthroscopy. Bone Jt. J. 2023, 105-B, 239–246. [Google Scholar] [CrossRef]
- Young, B.H.; Flanigan, R.M.; DiGiovanni, B.F. Complications of ankle arthroscopy utilizing a contemporary noninvasive distraction technique. J. Bone Jt. Surg. Am. 2011, 93, 963–968. [Google Scholar] [CrossRef]
- Complications in arthroscopy: The knee and other joints. Committee on Complications of the Arthroscopy Association of North America. Arthroscopy 1986, 2, 253–258. [Google Scholar]
- Small, N.C. Complications in arthroscopic surgery performed by experienced arthroscopists. Arthroscopy 1988, 4, 215–221. [Google Scholar] [CrossRef]
- Barber, F.A.; Click, J.; Britt, B.T. Complications of ankle arthroscopy. Foot Ankle. 1990, 10, 263–266. [Google Scholar] [CrossRef]
- Younger, A.S.; Kalla, T.P.; McEwen, J.A.; Inkpen, K. Survey of tourniquet use in orthopaedic foot and ankle surgery. Foot Ankle Int. 2005, 26, 208–217. [Google Scholar] [CrossRef]
- Carlson, M.J.; Ferkel, R.D. Complications in ankle and foot arthroscopy. Sports Med. Arthrosc. 2013, 21, 135–139. [Google Scholar] [CrossRef]
- Sircana, G.; Passiatore, M.; Capasso, L.; Saccomanno, M.F.; Maccauro, G. Infections in arthroscopy. Eur. Rev. Med. Pharmacol. Sci. 2019, 23 (Suppl. 2), 279–287. [Google Scholar] [CrossRef]
- Werner, B.C.; Cancienne, J.M.; Burrus, M.T.; Park, J.S.; Perumal, V.; Cooper, M.T. Risk of Infection After Intra-articular Steroid Injection at the Time of Ankle Arthroscopy in a Medicare Population. Arthroscopy 2016, 32, 350–354. [Google Scholar] [CrossRef]
- Rasmussen, S.; Hjorth Jensen, C. Arthroscopic treatment of impingement of the ankle reduces pain and enhances function. Scand. J. Med. Sci. Sports. 2002, 12, 69–72. [Google Scholar] [CrossRef]
- Deng, D.F.; Hamilton, G.A.; Lee, M.; Rush, S.; Ford, L.A.; Patel, S. Complications associated with foot and ankle arthroscopy. J. Foot Ankle Surg. 2012, 51, 281–284. [Google Scholar] [CrossRef]
- Baumbach, S.F.; Massen, F.K.; Hörterer, S.; Braunstein, M.; Waizy, H.; Böcker, W.; Polzer, H. Comparison of arthroscopic to open tibiotalocalcaneal arthrodesis in high-risk patients. Foot Ankle Surg. 2019, 25, 804–811. [Google Scholar] [CrossRef]
- Blázquez Martín, T.; Iglesias Durán, E.; San Miguel Campos, M. Complications after ankle and hindfoot arthroscopy. Rev. Esp. Cir. Ortop. Traumatol. 2016, 60, 387–393. [Google Scholar] [CrossRef]
- Thein, R.; Eichenblat, M. Arthroscopic treatment of sports-related synovitis of the ankle. Am. J. Sports Med. 1992, 20, 496–498. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. Int. J. Surg. 2021, 88, 105906. [Google Scholar] [CrossRef]
- Coleman, B.D.; Khan, K.M.; Maffulli, N.; Cook, J.L.; Wark, J.D. Studies of surgical outcome after patellar tendinopathy: Clinical significance of methodological deficiencies and guidelines for future studies. Victorian Institute of Sport Tendon Study Group. Scand. J. Med. Sci. Sports 2000, 10, 2–11. [Google Scholar] [CrossRef]
- Tian, J.; Mok, T.N.; Sin, T.H.; Zha, Z.; Zheng, X.; Teng, Q.; Hou, H. Clinical outcomes of anterior tibiofibular ligament’s distal fascicle transfer versus ligament reconstruction with InternalBrace™ for chronic ankle instability patients. Arch. Orthop. Trauma Surg. 2022, 142, 2829–2837. [Google Scholar] [CrossRef]
- Ahn, J.H.; Park, D.; Park, Y.T.; Park, J.; Kim, Y.C. What should we be careful of ankle arthroscopy? J. Orthop. Surg. 2019, 27, 2309499019862502. [Google Scholar] [CrossRef]
- Quayle, J.; Shafafy, R.; Khan, M.A.; Ghosh, K.; Sakellariou, A.; Gougoulias, N. Arthroscopic versus open ankle arthrodesis. Foot Ankle Surg. 2018, 24, 137–142. [Google Scholar] [CrossRef]
- Duan, X.; Yang, L.; Yin, L. Arthroscopic arthrodesis for ankle arthritis without bone graft. J. Orthop. Surg. Res. 2016, 11, 154. [Google Scholar] [CrossRef]
- Bai, Z.; Zhang, E.; He, Y.; Yan, X.; Sun, H.; Zhang, M. Arthroscopic ankle arthrodesis in hemophilic arthropathy. Foot Ankle Int. 2013, 34, 1147–1151. [Google Scholar] [CrossRef]
- Dannawi, Z.; Nawabi, D.H.; Patel, A.; Leong, J.J.; Moore, D.J. Arthroscopic ankle arthrodesis: Are results reproducible irrespective of pre-operative deformity? Foot Ankle Surg. 2011, 17, 294–299. [Google Scholar] [CrossRef]
- Kim, E.S.; Lee, K.T.; Park, J.S.; Lee, Y.K. Arthroscopic anterior talofibular ligament repair for chronic ankle instability with a suture anchor technique. Orthopedics 2011, 34. [Google Scholar] [CrossRef]
- Galla, M.; Lobenhoffer, P. Technique and results of arthroscopic treatment of posterior ankle impingement. Foot Ankle Surg. 2011, 17, 79–84. [Google Scholar] [CrossRef]
- Gougoulias, N.E.; Agathangelidis, F.G.; Parsons, S.W. Arthroscopic ankle arthrodesis. Foot Ankle Int. 2007, 28, 695–706. [Google Scholar] [CrossRef]
- Winson, I.G.; Robinson, D.E.; Allen, P.E. Arthroscopic ankle arthrodesis. J. Bone Jt. Surg. Br. 2005, 87, 343–347. [Google Scholar] [CrossRef]
- Pierre, A.; Hulet, C.; Locker, B.; Souquet, D.; Jambou, S.; Vielpeau, C. Arthrodèse tibio-talienne sous contrôle arthroscopique: Limites et indications [Arthroscopic tibio-talar arthrodesis: Limitations and indications in 20 patients]. Rev. Chir. Orthop. Reparatrice Appar. Mot. 2003, 89, 144–151. [Google Scholar]
- Cameron, S.E.; Ullrich, P. Arthroscopic arthrodesis of the ankle joint. Arthroscopy 2000, 16, 21–26. [Google Scholar] [CrossRef]
- Rolf, C.; Saro, C.; Engström, B.; Wredmark, T.; Movin, T.; Karlsson, J. Ankle arthroscopy under local and general anaesthesia for diagnostic evaluation and treatment. Scand. J. Med. Sci. Sports. 1996, 6, 255–258. [Google Scholar] [CrossRef]
- Crosby, L.A.; Yee, T.C.; Formanek, T.S.; Fitzgibbons, T.C. Complications following arthroscopic ankle arthrodesis. Foot Ankle Int. 1996, 17, 340–342. [Google Scholar] [CrossRef] [PubMed]
- Ogilvie-Harris, D.J.; Mahomed, N.; Demazière, A. Anterior impingement of the ankle treated by arthroscopic removal of bony spurs. J. Bone Joint Surg. Br. 1993, 75, 437–440. [Google Scholar] [CrossRef] [PubMed]
- Jerosch, J.; Steinbeck, J.; Schroder, M.; Reer, R. Arthroscopically assisted arthrodesis of the ankle joint. Arch. Orthop. Trauma. Surg. 1996, 115, 182–189. [Google Scholar] [CrossRef]
- Cugat, R.; Ares, O.; Cuscó, X.; Garcia, M.; Samitier, G.; Seijas, R. Posterior tibial nerve lesions in ankle arthroscopy. Arch. Orthop. Trauma. Surg. 2008, 128, 485–487. [Google Scholar] [CrossRef]
- Cianni, L.; Caredda, M.; De Fazio, A.; Basilico, M.; Greco, T.; Cazzato, G.; Perisano, C.; Maccauro, G.; Vitiello, R. Stress-Induced Hyperglycemia is a Risk Factor for Surgical-Site Infections in Nondiabetic Patients with Open Leg Fractures. Adv. Orthop. 2023, 2023, 6695648. [Google Scholar] [CrossRef] [PubMed]
- Wise, B.T.; Connelly, D.; Rocca, M.; Mascarenhas, D.; Huang, Y.; Maceroli, M.A.; Joshi, M.; Castillo, R.C.; O’Toole, R.V. Are deep infections that present before and after 90 days from orthopaedic trauma different? An analysis of the validity of the recent change in CDC criteria for infections. Injury 2022, 53, 912–918. [Google Scholar] [CrossRef] [PubMed]
- Pauzenberger, L.; Grieb, A.; Hexel, M.; Laky, B.; Anderl, W.; Heuberer, P. Infections following arthroscopic rotator cuff repair: Incidence, risk factors, and prophylaxis. Knee Surg. Sports Traumatol. Arthrosc. 2017, 25, 595–601. [Google Scholar] [CrossRef] [PubMed]
- Voss, A.; Pfeifer, C.G.; Kerschbaum, M.; Rupp, M.; Angele, P.; Alt, V. Post-operative septic arthritis after arthroscopy: Modern diagnostic and therapeutic concepts. Knee Surg. Sports Traumatol. Arthrosc. 2021, 29, 3149–3158. [Google Scholar] [CrossRef] [PubMed]
- Bauer, T.; Boisrenoult, P.; Jenny, J.Y. Post-arthroscopy septic arthritis: Current data and practical recommendations. Orthop. Traumatol. Surg. Res. 2015, 101 (Suppl. 8), S347–S350. [Google Scholar] [CrossRef]
| Ref. | Year of Publication | Manuscript Category | N° Patients/Procedures | Age (Mean) | mCMS |
|---|---|---|---|---|---|
| Tian J et al. [26] | 2022 | Retrospective | 25/25 | 33 | 54 |
| Ahn JH et al. [27] | 2019 | Retrospective | 514/514 | 37.2 | 48 |
| Quayle J et al. [28] | 2018 | Retrospective | 50/50 | 57 | 42 |
| Duan X et al. [29] | 2016 | Prospective | 68/68 | 59 | 63 |
| Abdelatif NM et al. [8] | 2014 | Prospective | 19/19 | 29 | 62 |
| Bai Z et al. [30] | 2013 | Retrospective | 10/10 | 27.6 | 36 |
| Young BH et al. [11] | 2011 | Retrospective | 294/294 | 37 | 52 |
| Dannawi Z et al. [31] | 2011 | Retrospective | 55/55 | 63 | 55 |
| Kim ES et al. [32] | 2011 | Retrospective | 28/28 | - | 46 |
| Galla M et al. [33] | 2010 | Prospective | 30/30 | 49 | 63 |
| Gougoulias NE et al. [34] | 2007 | Retrospective | 74/78 | 54 | 48 |
| Winson IG et al. [35] | 2005 | Retrospective | 116/118 | 57 | 50 |
| Pierre A et al. [36] | 2003 | Prospective | 20/20 | 55 | 56 |
| Rasmussen S et al. [19] | 2002 | Retrospective | 105/105 | 35 | 63 |
| Cameron SE et al. [37] | 2000 | Retrospective | 15/15 | 51 | 42 |
| Rolf C et al. [38] | 1996 | Prospective | 109/112 | 31 | 65 |
| Crosby LA et al. [39] | 1996 | Prospective | 42/42 | 46 | 63 |
| Ogilvie-Harris DJ et al. [40] | 1993 | Retrospective | 17/17 | 31 | 53 |
| Thein R et al. [23] | 1992 | Prospective | 9/9 | 23 | 45 |
| Barber F A et al. [14] | 1990 | Prospective | 49/53 | 33 | 42 |
| Martin D F et al. [3] | 1989 | Retrospective | 57/58 | 32 | 58 |
| Total | 1706/1720 | 42 | 53 |
| Ref. | N° Superficial Infections/Total Infections | Medical Therapy | |||
|---|---|---|---|---|---|
| Oral ab | Local ab | Local Care | ns ab | ||
| Tian J et al. [26] | 1/1 | X | |||
| Ahn JH et al. [27] | 1/1 | X | |||
| Quayle J et al. [28] | 1/1 | X | |||
| Duan X et al. [29] | 1/1 | X | X | ||
| Abdelatif NM et al. [8] | 1/1 | X | X | ||
| Bai Z et al. [30] | 1/1 | X | |||
| Young BH et al. [11] | 2/2 | X | X | ||
| Dannawi Z et al. [31] | 3/3 | X | |||
| Kim ES et al. [32] | 1/1 | X | |||
| Gougoulias NE et al. [34] | 1/1 | X | X | ||
| Winson IG et al. [35] | 3/4 | X | |||
| Pierre A et al. [36] | 2/2 | X | |||
| Crosby LA et al. [39] | 4/5 | X | |||
| Ogilvie-Harris DJ et al. [40] | 1/1 | X | |||
| Thein R et al. [23] | 1/1 | X | |||
| Barber F A et al. [14] | 2/3 | X | X | ||
| Martin D F et al. [3] | 2/4 | X | |||
| Ref. | N° Deep Infections/Total Infections | Treatment | ||||
|---|---|---|---|---|---|---|
| IV AB | Surgical Debridement | Surgical Deb + IV AB | ns | Open Debridement/Arthroscopic Debridement | ||
| Galla M et al. [33] | 1/1 | X | Open | |||
| Winson IG et al. [35] | 1/4 | X | ||||
| Rasmussen S et al. [19] | 4/4 | X | Arthroscopic | |||
| Cameron SE et al. [37] | 2/2 | X | Open | |||
| Rolf C et al. [38] | 1/1 | X | ns | |||
| Crosby LA et al. [39] | 1/5 | X | Open | |||
| Barber F A et al. [14] | 1/3 | X | ||||
| Martin D F et al. [3] | 2/4 | X | ns | |||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
De Fazio, A.; Bocchi, M.B.; Miele, G.; Ruberto, P.; Forconi, F.; Ziranu, A.; Maccauro, G.; Vitiello, R. Epidemiology and Treatment of Surgical Infection after Ankle Arthroscopy: A Systematic Review. J. Clin. Med. 2024, 13, 983. https://doi.org/10.3390/jcm13040983
De Fazio A, Bocchi MB, Miele G, Ruberto P, Forconi F, Ziranu A, Maccauro G, Vitiello R. Epidemiology and Treatment of Surgical Infection after Ankle Arthroscopy: A Systematic Review. Journal of Clinical Medicine. 2024; 13(4):983. https://doi.org/10.3390/jcm13040983
Chicago/Turabian StyleDe Fazio, Andrea, Maria Beatrice Bocchi, Guglielmo Miele, Pasquale Ruberto, Fabrizio Forconi, Antonio Ziranu, Giulio Maccauro, and Raffaele Vitiello. 2024. "Epidemiology and Treatment of Surgical Infection after Ankle Arthroscopy: A Systematic Review" Journal of Clinical Medicine 13, no. 4: 983. https://doi.org/10.3390/jcm13040983
APA StyleDe Fazio, A., Bocchi, M. B., Miele, G., Ruberto, P., Forconi, F., Ziranu, A., Maccauro, G., & Vitiello, R. (2024). Epidemiology and Treatment of Surgical Infection after Ankle Arthroscopy: A Systematic Review. Journal of Clinical Medicine, 13(4), 983. https://doi.org/10.3390/jcm13040983






