Abstract
The aim of the present systematic review was to investigate the clinical outcomes after the perforation of the maxillary sinus by dental implants, or after maxillary sinus membrane perforation during sinus lift procedure. Twenty-nine publications were included. Failure rates of implants in cases where perforation of sinus floor had happened (11 studies) was generally low, and only one case of transient sinusitis was reported. The estimated failure rate of these implants was 2.1% (SE 1.0%, p = 0.035). There were 1817 implants (73 failures) placed in augmented sinuses in which the sinus membrane was perforated and 5043 implants (274 failures) placed in sinuses with no perforated membrane, from 18 studies. The odds of implant failure difference between the groups were not significant (OR 1.347, p = 0.197). log OR of implant failure between perforated and non-perforated membrane groups did not significantly change with the follow-up time (−0.004/month; p = 0.500). In conclusion, implant failure rate is generally low either for implants penetrating in the floor of the maxillary sinus or implants placed in augmented sinuses in which the sinus membrane was perforated. The prevalence of postoperative infection/sinusitis is low, and it may depend either on the dimensions of the perforation or on the anatomical predisposition.
1. Introduction
The area of the posterior maxilla is recognized by the presence of the maxillary sinuses, bilateral cavities that usually compromises the volume of bone available in the region [1]. The local shortage of bone is aggravated by pneumatization, the progressive expansion of the sinuses volume, a process that begins after birth and continues until the 2nd–3rd decades of life [2]. The loss of posterior maxillary teeth exacerbates the situation, due to additional pneumatization [3], and resorption of the alveolar bone, resulting in loss of bone height [4]. Moreover, the region is typically characterized by trabecular bone of low density and thin cortical bone, which may exert a negative impact on implant survival [5]. Some options for the rehabilitation of the posterior maxilla, when this region becomes edentulous due to loss of teeth, include the placement of implants anchored in the pterygoid process [6] or in the zygomatic bone [7], each approach with their advantages and risks, with potential complications more commonly observed with zygomatic implants [8,9,10]. Two other options consist of the installation of short dental implants, and grafting of the maxillary sinus floor.
Implants of short lengths can be placed when the bone is low in height. There is, however, a recommendation that the implant should be anchored to a minimum of 4 mm of bone to increase the possibility of primary stability, and consequently reduce the risk of early implant loss [11]. This is not always possible though, which prompts the health professional to consider bone grafting.
The approach of grafting the maxillary sinus is called of maxillary sinus elevation surgery, or maxillary sinus lift/augmentation. In this technique, graft material is added to the floor of the sinus to increase the height of available bone, so implants of longer lengths can be placed [12]. Complications can, however, occur, such as tearing of the (Schneiderian) sinus membrane, bleeding, infection, loss of the graft material, persistent sinusitis, among others [13].
Perforation of the sinus membrane can happen or not after perforation of the maxillary sinus floor when a dental implant is placed without sinus augmentation. No adverse effects may result when the penetration of the implant into the sinus is small, namely, less than 2 mm, and the membrane is not perforated. However, when the implant intrusion into the sinus is greater and the membrane is perforated, complications like epistaxis, thickening of the membrane, and sinusitis can occur [14].
The purpose of the present study was to investigate the implant failure rates and complications after the perforation of the maxillary sinus floor by the placement of dental implants in posterior region of the maxilla, or after maxillary sinus membrane perforation during sinus lift procedure, based on a systematic review of the literature.
2. Materials and Methods
This study followed the PRISMA 2020 Statement guidelines [15]. Register in PROSPERO was undertaken with the registration number CRD42024497046.
2.1. Focused Question
The focused question was elaborated using the participants, interventions, comparisons, outcomes (PICO) format: In patients being rehabilitated with dental implants, what is the implant failure rates and complications after either maxillary sinus perforation due to the placement of dental implants in the posterior maxilla, or maxillary sinus membrane perforation during sinus lift procedure in comparison to non-perforated cases?
2.2. Search Strategies
An electronic search without time restrictions was first undertaken in September 2022, and the last update occurred in October 2023, in the following databases: PubMed/Medline, Web of Science, and Science Direct. The following terms were used in the search strategies:
(“dental implant” OR “oral implant”) AND (“maxillary sinus” OR “maxillary sinus membrane” OR “Schneiderian membrane”) AND (perforation OR perforate OR penetration OR intrusion).
A manual search of dental implants-related journals was performed (the list of journals can be found in the Supplementary Materials). The reference lists of the identified studies and the relevant reviews on the subject were also checked for possible additional studies.
2.3. Inclusion and Exclusion Criteria
Eligibility criteria included clinical human studies providing information on patients rehabilitated with dental implants in the posterior maxilla which reported either perforation of the maxillary sinus, or perforation of the maxillary sinus membrane during the procedure of sinus lift. Only the cases rehabilitated with cylindrical screw-type modern dental implants of titanium (commercially pure Ti) or its alloys were considered.
Exclusion criteria were case reports, technical reports, animal studies, in vitro studies, and reviews papers. It was also excluded studies reporting cases rehabilitated with mini-implants, zygomatic, orthodontic, zirconia, subperiosteal, or hollow implants.
2.4. Study Selection
The titles and abstracts of all reports identified through the electronic searches were read independently by the three authors. For studies appearing to meet the inclusion criteria, or for which there were insufficient data in the title and abstract to make a clear decision, the full report was obtained. Disagreements were solved by discussion between the authors.
2.5. Quality Assessment
Quality assessment of the studies was executed according to the Quality Assessment Tool of the National Institutes of Health [16]. Studies of “good” quality were judged to have at least 7 points.
2.6. Definitions
Sinus perforation: Implant perforation of the maxillary sinus was defined as the intrusion of a dental implant into the sinus cavity during drilling or implant placement, with and without punch out Schneiderian membrane [14].
Sinus lift: Sinus lift procedures increase bone volume by augmenting the sinus cavity with autogenous bone and/or commercially available biomaterials [17].
Implant failure: An implant was considered a failure if presenting signs and symptoms that led to implant removal, i.e., a lost implant. Implant failure could be either early (the inadequacy of the host to establish or promote osseointegration in the early stages of healing) or late (the failure of either the established osseointegration or function of dental implants) [18]. Fracture of an implant was also considered as a failure [19].
Complications consisted of clinical or radiographic complications. Clinical complications: sinusitis, nasal bleeding, nasal obstruction, nasal secretion, headache, pain/tenderness in the sinus region, decreased sense of smell. Radiographic complications: thickening of Schneiderian membrane, bone reaction to the implants, sinus pathology.
2.7. Data Extraction
The following data were extracted: year of publication, study design, country, study setting, number of patients, patients’ age and sex, implant healing period, failed and placed implants with sinus perforation or with sinus membrane perforation during sinus augmentation, implant system, presence of smokers in the patients’ study group, occurrence of complications, and follow-up time. Contact with authors for providing missing data was performed.
2.8. Analyses
Implant failure was the dichotomous outcome measure evaluated. The statistical unit for ‘implant failure’ was the implant. The untransformed proportion of failure for implants that perforated the maxillary sinus floor was calculated by considering the prevalence reported in the studies.
Pairwise meta-analysis was performed for the comparison of the failure rates bewteen implants placed in augmented sinuses in which the sinus membrane was perforated and implants placed in sinuses with no perforated membrane. Heterogeneity was checked using the I2 statistic. The inverse variance method was used for the random-effects (heterogeneity p < 0.10) or fixed-effects model (heterogeneity p ≥ 0.10) [20]. The estimates of relative effect for dichotomous outcomes were expressed in odds ratio (OR).
In order to explore the possible heterogeneity of effect between studies, a meta-regression was performed in order to verify how the OR was associated with the time of follow-up.
A funnel plot (plot of effect size versus standard error) was drawn.
The data were analyzed using the statistical software OpenMeta [Analyst], version 64-bit for Windows 10 [21]. The funnel plot was generated with the software OpenMEE, version 64-bit for Windows 10 [22].
3. Results
3.1. Literature Search
The study selection process is summarized in Figure 1. The search strategy in the databases resulted in 633 papers (109 in PubMed/Medline, 195 in Web of Science, 329 in Scopus). A total of 115 articles were cited in more than one database (duplicates). The reviewers independently screened the titles and abstracts of the remaining entries, leading to the exclusion of 455 articles as the studies were not related to the subject. Of the full-text reports of the remaining 63 articles, there was a lack of information concerning either the number of failures or the total number of implants in cases with perforated sinus membrane in 8 studies. The authors of these 8 studies were contacted by e-mail up to three times asking for missing essential information for the analyses, but none of them replied. Other 26 studies did not fulfill the eligibility criteria. Hand-searching of journals and of the reference lists of selected studies did not yield additional papers. Thus, 29 studies were included in the review.
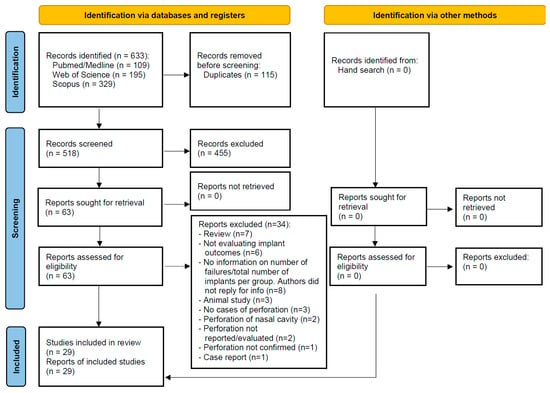
Figure 1.
Study screening process.
3.2. Description of the Studies
Out of the 29 included studies, 11 studies [23,24,25,26,27,28,29,30,31,32,33] reported on cases in which maxillary sinus perforation happened after installation of dental implants in the posterior maxilla, and 18 studies [34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51] reported on maxillary sinus membrane perforation during sinus lift procedure. Table S1 (see Supplementary Materials) presents detailed data of the 29 included studies.
3.2.1. Maxillary Sinus Perforation after Installation of Dental Implants
The articles were published between 1984 and 2022. Two of the studies were multicenter, whereas the other nine studies were unicenter, one was prospective, ten were retrospective. Seven studies were conducted in a university, two in private practices, one study in a university and private practice, with no clear information about it for one study.
In six of the studies no implant failures were observed [23,24,28,29,30,33]. One of the studies [26] was cross-sectional and investigated the possible influence of penetrating implants on the status of maxillary sinuses on CBCT exams. The failure rates of perforating implants in the remaining studies were 28.9% [25], 1.6% [31], 4% [27], and 20% [32].
The development of transient sinusitis was reported in only one case [31]. The most common radiological sign reported, although not in every patient of every study, was mucosal thickening around the penetrating implants, limited to the maxillary sinus floor, with no pain nor discomfort.
3.2.2. Maxillary Sinus Membrane Perforation during Sinus Lift Procedure
The articles were published between 2006 and 2023. One study was multicenter, whereas the other 17 studies were unicenter, 3 were prospective, 15 were retrospective. Twelve studies were conducted in a university, and six in private practices. All the studies for the exception of one [44] reported failure rates for the implants that were inserted in both the group of sinuses that presented and in the group of sinuses that did not present perforation of the sinus membrane during the sinus lifting procedure.
There were 1817 implants (73 failures) placed in augmented sinuses in which the sinus membrane was perforated and 5043 implants (274 failures) placed in sinuses with no perforated membrane. The results of the pairwise meta-analysis for this comparison are presented later on in this text.
Seven studies did not report/evaluate on the development of post-operative symptoms in the maxillary sinus [35,37,39,40,42,43,49]. For the studies that investigated symptoms, three studies reported absence of post-operative symptoms among the patients [34,50,51], while in the other eight studies [36,38,41,44,45,46,47,48] some cases of post-operative infection were observed, as well as some cases of post-operative sinusitis (see details in Table S1). Many of these patients were treated with antibiotics, with some sinuses being incised and drained.
3.3. Quality Assessment
All included studies were classified as “good” according to the quality assessment tool (see Supplementary Material). In most cases the main issues in the publications were related to not well-described statistical methods, and to the inclusion of non-consecutive patients in the studies.
3.4. Meta-Analysis
Ten studies reported the failure rate of implants when these perforated the floor of the maxillary sinus during placement. The estimated failure rate was of 2.1% (95% confidence interval 0.2%, 4.1%; standard error 1.0%, p = 0.035; heterogeneity: τ2 = 0.000, Chi2 = 21.917, I2 = 58.936, p = 0.009) (Figure 2). If the study of Brånemark et al. [25], with turned (machined) implants, is not included, the estimated failure rate goes down to 1.0% (95% confidence interval 0.0%, 1.9%; standard error 0.5%, p = 0.048; heterogeneity: τ2 = 0.000, Chi2 = 4.744, I2 = 0.000, p = 0.785).
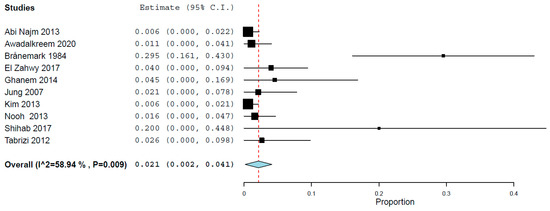
Figure 2.
Estimated failure rate of implants that perforated the maxillary sinus floor [23,24,25,27,28,29,30,31,32,33]. Red dashed line: overall effect.
Seventeen studies reported the results of implant failure for two groups, namely, patients that presented and did not present sinus membrane perforation during the sinus lift procedure. A random-effects model was used to evaluate the comparison of the implant failure between the groups, due to heterogeneity (τ2 = 0.241, Chi2 = 25.048, I2 = 36.121, p = 0.069). The pairwise meta-analysis showed implants placed in augmented sinuses in which the membrane was perforated did not have a higher risk of failure than implants placed in sinuses with no perforated membrane, with an OR 1.347 (95% confidence interval, 0.857, 2.117, p = 0.197; Figure 3). However, the effect size was not statistically significant.
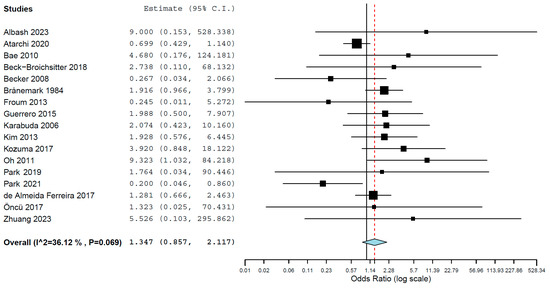
Figure 3.
Forest plot for the event ‘implant failure’, for implants placed in the posterior maxilla, between procedures that presented and did not present sinus membrane perforation during max-illary sinus lift [25,34,35,36,37,38,39,40,41,43,45,46,47,48,49,50,51]. Red dashed line: overall effect.
3.5. Meta-Regression
Of the 17 studies that had two groups (patients that presented and did not present sinus membrane perforation), 16 provided clear information about the follow-up time or mean follow-up time. For the remaining one study, no information on precise follow-up time was available.
When a meta-regression considering the follow-up period as a covariate in relation to OR was plotted for these 16 studies, it was observed that the OR decreased with and increased follow-up time, although without significance (p = 0.500) (Figure 4). The first-degree equation resulted from the linear regression of this meta-regression was
where:
y = 0.640 − 0.004x
- Intercept = 0.640 (−0.093, 1.374), standard error 0.374, p = 0.087
- Follow-up = −0.004 (−0.016, 0.008), standard error 0.006, p = 0.500
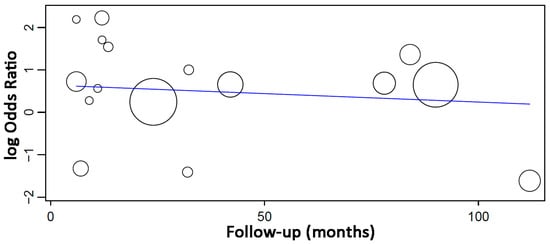
Figure 4.
Scatter plot for the meta-regression with the association between the log odds ratio (OR) of implant failure between patients that presented sinus membrane perforation and patients that did not present sinus membrane perforation, and the follow-up time (in months). Every circle represents a study and the size of the circle represents the weight of the study in the analysis. The blue line represents the fitted line plot.
3.6. Publication Bias
The funnel plot did not show a clear asymmetry (Figure 5), indicating possible absence of publication bias.
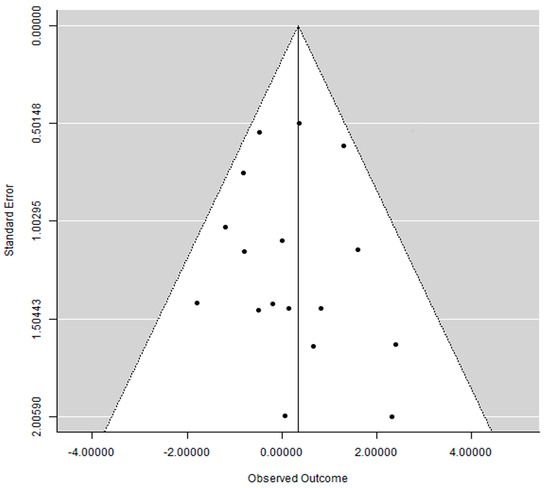
Figure 5.
Funnel plot. Each dot represents a study. The area within the white triangle represents the 95% confidence interval.
4. Discussion
The purpose of the present review was to investigate the implant failure rates and complications after the perforation of the maxillary sinus by the placement of dental implants in posterior region of the maxilla, and after maxillary sinus membrane perforation during sinus lift procedure.
The results showed that the implant failure rate is generally low for implants penetrating in the floor of the maxillary sinus. Even though mucosal thickening around the penetrating implants was not an uncommon observation, only few cases developed symptoms in the sinus. The possible reason for the low implant failure rate and the low degree of symptomatology can be due to the fact that sinus perforation, in the great majority of the cases, may not result in any adverse occurrence. It was observed that formation of bone takes place around the apical part of implants intentionally protruded into the sinus floor without perforation of the sinus membrane, even without the addition of any grafting material [52]. Complications may not occur even when the membrane is perforated. It was observed in an animal study with dogs that implant perforation is not associated with sinus complications or pathologies, regardless of the extension of the implant protrusion into the sinus—protrusions of up to 8 mm into the sinus were investigated in this study [53]. This same research group later published the results of a retrospective clinical study in humans, in which 23 implants were intentionally intruded into the maxillary sinus of 9 patients, without sinus augmentation. After being followed up from 6 to 10 months, none of the patients presented signs of sinusitis, although mucous thickening of the sinus was a common observation [29]. A recent retrospective study based on computed tomography scans observed that the perforation of the maxillary sinus floor by implants is commonly associated sinus opacification, which occurrence is suggested to be more influenced by the implant diameter than by the length of the implant that is intruded into the sinus [54]. Mucosal thickening and opacification can occur, however, even when no perforation has taken place, being associated to when implants in the posterior maxilla are located within 2 mm from the cortex of the maxillary sinus floor [26].
The estimated failure of implants when these perforated the maxillary sinus floor was low, but it would become even lower if the early study of Brånemark et al. [25] would not be included in the analysis. The much higher failure rate for perforating implants observed in aforementioned study in comparison to the other studies can be associated with the use of turned (machined) implants in this study. Turned implants present a much higher risk of failure than the surface-modified implants [55,56] used in more recent studies included in the present review. Implants with moderately roughened surfaces usually present higher survival rates due to their chemical and topographical modified surface that favors osseointegration [56].
The results of the meta-analysis suggest that implants placed in augmented sinuses in which the sinus membrane was perforated do not present a higher risk of failure in comparison to implants placed in sinuses with no perforated membrane. Most surgeons perform some kind of treatment to address the perforated membrane, and with appropriate treatment, which differ depending on the size of the perforation [57], intraoperative sinus membrane perforations do not represent a higher risk for implant failure [38]. The implant failure rate, however, may vary significantly with the perforation size, with larger perforations resulting in higher failure rates, as observed in two studies [39,42].
Cases of augmented sinuses resulting in sinusitis or infection were reported, that needed to be treated with antibiotics, and some cases were even surgically drained. The occurrence of these post-operative complications could be associated with the occurrence of membrane perforation, as it was observed that grafted sinuses that had the membrane perforated during surgery presented a much higher incidence of sinusitis or infection in comparison to the cases in which a perforation did not occur [58]. The graft may dislodge into the sinus with membrane perforation, consequently potentially disrupting the normal sinus physiology [59,60]. It must be kept in mind that is not only during surgery that the sinus membrane can tear, but overfilling of the maxillary sinus with graft material may cause necrosis of the membrane and secondary perforation [61,62]. The perforation of the membrane may lead to the disrupted function of mucociliary apparatus, besides loss of the biologic barrier, resulting in an increase of sinus bacteria invasion which may evolve to infection [63,64]. Moreover, it seems that the occurrence of postoperative chronic sinusitis could be limited to patients with a predisposition for this condition due to deviation in form and size of the inferior turbinate and the position of the nasal septum, with structural drainage problems of the paranasal sinuses [62].
One must weigh the available options in face of the possible complications. The placement of short implants, which would be an option when one would like to avoid grafting procedures, provided that there is a minimum height of bone, has a higher risk of failure in comparison to longer implants [65], while sinus lift, which has a prevalence of membrane perforation going from 22 to 50% [57], may result in displacement of the graft material into the sinus leading to postoperative sinusitis and/or infection [63,64].
Limitations of the present review include the fact that there was a considerable number of confounding factors. There was no information about how many implants were inserted and failed in several different conditions for most (if not all) of the studies. Studies reported the presence of diabetics among the patients, as well as smokers, bruxers, and patients taking bisphosphonates. All these factors could have had a considerable impact on implant failure rates [66,67,68,69]. Moreover, the implants were placed by groups of different operators, due to different studies, which may also negatively influence implant survival rates, due to the variation in the surgeons’ technique, skills, and/or judgment [70]. Furthermore, the retrospective nature of many studies results in flaws manifested by the gaps in information. In addition, several studies presented small cohort sizes and short follow-ups.
5. Conclusions
Implant failure rate is generally low for implants penetrating in the floor of the maxillary sinus. Moreover, implants placed in augmented sinuses in which the sinus membrane was perforated do not present a higher risk of failure in comparison to implants placed in sinuses with no perforated membrane. The prevalence of postoperative infection or sinusitis is low, and it may depend either on the dimensions of the perforation or on the anatomical predisposition.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/jcm13051253/s1, List of journals included in the manual (hand) searching; List of excluded articles; Table S1. Detailed data of the included studies; Table S2. Quality assessment of the included studies, according to the National Institutes of Health (NIH); PRISMA 2020 Checklist.
Author Contributions
Conceptualization, B.R.C.; methodology, Y.M.S., H.L. and B.R.C.; investigation, Y.M.S., H.L. and B.R.C.; writing—original draft, Y.M.S., H.L. and B.R.C.; formal analysis, B.R.C.; writing—review & editing, Y.M.S., H.L. and B.R.C.; visualization, B.R.C.; supervision, B.R.C. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
All the data resulted from this review is presented in the manuscript.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Yücesoy, T.; Göktaş, T.A. Evaluation of Sinus Pneumatization and Dental Implant Placement in Atrophic Maxillary Premolar and Molar Regions. Int. J. Oral. Maxillofac. Implant. 2022, 37, 407–415. [Google Scholar] [CrossRef]
- Jun, B.C.; Song, S.W.; Park, C.S.; Lee, D.H.; Cho, K.J.; Cho, J.H. The analysis of maxillary sinus aeration according to aging process; volume assessment by 3-dimensional reconstruction by high-resolutional CT scanning. Otolaryngol. Head Neck Surg. 2005, 132, 429–434. [Google Scholar] [CrossRef]
- Sharan, A.; Madjar, D. Maxillary sinus pneumatization following extractions: A radiographic study. Int. J. Oral. Maxillofac. Implant. 2008, 23, 48–56. [Google Scholar]
- Levi, I.; Halperin-Sternfeld, M.; Horwitz, J.; Zigdon-Giladi, H.; Machtei, E.E. Dimensional changes of the maxillary sinus following tooth extraction in the posterior maxilla with and without socket preservation. Clin. Implant. Dent. Relat. Res. 2017, 19, 952–958. [Google Scholar] [CrossRef]
- Chrcanovic, B.R.; Albrektsson, T.; Wennerberg, A. Bone Quality and Quantity and Dental Implant Failure: A Systematic Review and Meta-analysis. Int. J. Prosthodont. 2017, 30, 219–237. [Google Scholar] [CrossRef]
- Araujo, R.Z.; Santiago Júnior, J.F.; Cardoso, C.L.; Benites Condezo, A.F.; Moreira Júnior, R.; Curi, M.M. Clinical outcomes of pterygoid implants: Systematic review and meta-analysis. J. Craniomaxillofac Surg. 2019, 47, 651–660. [Google Scholar] [CrossRef]
- Chrcanovic, B.R.; Pedrosa, A.R.; Neto Custodio, A.L. Zygomatic implants: A critical review of the surgical techniques. Oral. Maxillofac. Surg. 2013, 17, 1–9. [Google Scholar] [CrossRef]
- Candel, E.; Peñarrocha, D.; Peñarrocha, M. Rehabilitation of the atrophic posterior maxilla with pterygoid implants: A review. J. Oral. Implantol. 2012, 38, 461–466. [Google Scholar] [CrossRef]
- Chrcanovic, B.R.; Abreu, M.H. Survival and complications of zygomatic implants: A systematic review. Oral. Maxillofac. Surg. 2013, 17, 81–93. [Google Scholar] [CrossRef]
- Chrcanovic, B.R.; Oliveira, D.R.; Custodio, A.L. Accuracy evaluation of computed tomography-derived stereolithographic surgical guides in zygomatic implant placement in human cadavers. J. Oral. Implantol. 2010, 36, 345–355. [Google Scholar] [CrossRef]
- Fenner, M.; Vairaktaris, E.; Fischer, K.; Schlegel, K.A.; Neukam, F.W.; Nkenke, E. Influence of residual alveolar bone height on osseointegration of implants in the maxilla: A pilot study. Clin. Oral. Implant. Res. 2009, 20, 555–559. [Google Scholar] [CrossRef] [PubMed]
- Kaufman, E. Maxillary sinus elevation surgery: An overview. J. Esthet. Restor. Dent. 2003, 15, 272–282; discussion 283. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.; Jang, H. A review of complications of maxillary sinus augmentation and available treatment methods. J. Korean Assoc. Oral. Maxillofac. Surg. 2019, 45, 220–224. [Google Scholar] [CrossRef]
- Ragucci, G.M.; Elnayef, B.; Suárez-López Del Amo, F.; Wang, H.L.; Hernández-Alfaro, F.; Gargallo-Albiol, J. Influence of exposing dental implants into the sinus cavity on survival and complications rate: A systematic review. Int. J. Implant. Dent. 2019, 5, 6. [Google Scholar] [CrossRef]
- Page, M.J.; Moher, D.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. PRISMA 2020 explanation and elaboration: Updated guidance and exemplars for reporting systematic reviews. BMJ 2021, 372, n160. [Google Scholar] [CrossRef]
- NIH. Quality Assessment Tool for Case Series Studies. Available online: https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools (accessed on 15 January 2020).
- Esposito, M.; Grusovin, M.G.; Rees, J.; Karasoulos, D.; Felice, P.; Alissa, R.; Worthington, H.; Coulthard, P. Effectiveness of sinus lift procedures for dental implant rehabilitation: A Cochrane systematic review. Eur. J. Oral. Implantol. 2010, 3, 7–26. [Google Scholar]
- Tonetti, M.S.; Schmid, J. Pathogenesis of implant failures. Periodontol. 2000 1994, 4, 127–138. [Google Scholar] [CrossRef]
- Chrcanovic, B.R.; Kisch, J.; Albrektsson, T.; Wennerberg, A. Factors influencing the fracture of dental implants. Clin. Implant. Dent. Relat. Res. 2018, 20, 58–67. [Google Scholar] [CrossRef]
- Egger, M.; Smith, G.D. Principles of and procedures for systematic reviews. In Systematic Reviews in Health Care: Meta-Analysis in Context; Egger, M., Smith, G.D., Altman, D.G., Eds.; BMJ Books: London, UK, 2003; pp. 23–42. [Google Scholar]
- Wallace, B.C.; Dahabreh, I.J.; Trikalinos, T.A.; Lau, J.; Trow, P.; Schmid, C.H. Closing the Gap between Methodologists and End-Users: R as a Computational Back-End. J. Stat. Softw. 2012, 49, 1–15. [Google Scholar] [CrossRef]
- Wallace, B.C.; Lajeunesse, M.J.; Dietz, G.; Dahabreh, I.J.; Trikalinos, T.A.; Schmid, C.H.; Gurevitch, J. OpenMEE: Intuitive, open-source software for meta-analysis in ecology and evolutionary biology. Methods Ecol. Evol. 2017, 8, 941–947. [Google Scholar] [CrossRef]
- Abi Najm, S.; Malis, D.; El Hage, M.; Rahban, S.; Carrel, J.P.; Bernard, J.P. Potential adverse events of endosseous dental implants penetrating the maxillary sinus: Long-term clinical evaluation. Laryngoscope 2013, 123, 2958–2961. [Google Scholar] [CrossRef]
- Awadalkreem, F.; Ahmad, A.G.; Ihde, S.; Osman, M. Effects of Corticobasal Implant Protrusion inside the Nasal and Maxillary Sinus. Ann. Maxillofac. Surg. 2020, 10, 114–121. [Google Scholar] [CrossRef]
- Brånemark27, P.I.; Adell, R.; Albrektsson, T.; Lekholm, U.; Lindström, J.; Rockler, B. An experimental and clinical study of osseointegrated implants penetrating the nasal cavity and maxillary sinus. J. Oral. Maxillofac. Surg. 1984, 42, 497–505. [Google Scholar] [CrossRef]
- Chaves, L.L.V.; Lopes Rosado, L.P.; Piccolo, S.M.; Ferreira, L.M.; Kamburoglu, K.; Junqueira, R.B.; Aquino de Castro, M.A.; Verner, F.S. Evaluation of the Maxillary Sinus of Patients with Maxillary Posterior Implants: A CBCT Cross-Sectional Study. Diagnostics 2022, 12, 3169. [Google Scholar] [CrossRef]
- El Zahwy, M.; Awad, S.; Kamel, H.M.; Mostafa, B. Clinical and Radiographic Evaluation of Dental implants Penetrating the Maxillary Sinus. J. Int. Dent. Med. Res. 2017, 10, 207–213. [Google Scholar]
- Ghanem, A.; Gad, H.M. The influence of exposing dental implants to the maxillary sinus cavity on sinus complications and implant survival rate: 6 years prospective follow-up. Egypt. Dent. J. 2014, 60, 2–9. [Google Scholar]
- Jung, J.H.; Choi, B.H.; Jeong, S.M.; Li, J.; Lee, S.H.; Lee, H.J. A retrospective study of the effects on sinus complications of exposing dental implants to the maxillary sinus cavity. Oral. Surg. Oral. Med. Oral. Pathol. Oral. Radiol. Endod. 2007, 103, 623–625. [Google Scholar] [CrossRef]
- Kim, H.Y.; Yang, J.Y.; Chung, B.Y.; Kim, J.C.; Yeo, I.S. Peri-implant bone length changes and survival rates of implants penetrating the sinus membrane at the posterior maxilla in patients with limited vertical bone height. J. Periodontal Implant. Sci. 2013, 43, 58–63. [Google Scholar] [CrossRef]
- Nooh, N. Effect of schneiderian membrane perforation on posterior maxillary implant survival. J. Int. Oral. Health 2013, 5, 28–34. [Google Scholar]
- Shihab, O.I. Intentional penetration of dental implants into the maxillary sinus: A retrospective study. Zanco J. Med. Sci. 2017, 21, 1536–1539. [Google Scholar] [CrossRef][Green Version]
- Tabrizi, R.; Amid, R.; Taha Özkan, B.; Khorshidi, H.; Langner, N.J. Effects of exposing dental implant to the maxillary sinus cavity. J. Craniofac Surg. 2012, 23, 767–769. [Google Scholar] [CrossRef]
- Albash, Z.; Khalil, A.; Sleman, N. Influence of implant protrusion length and initial bone height on intrasinus bone gain in transalveolar sinus floor elevation without bone graft: A 2-year retrospective study. Ann. Med. Surg. 2023, 85, 3291–3297. [Google Scholar] [CrossRef]
- Atarchi, A.R.; Miley, D.D.; Omran, M.T.; Abdulkareem, A.A. Early Failure Rate and Associated Risk Factors for Dental Implants Placed with and Without Maxillary Sinus Augmentation: A Retrospective Study. Int. J. Oral. Maxillofac. Implant. 2020, 35, 1187–1194. [Google Scholar] [CrossRef]
- Bae, J.H.; Kim, Y.K.; Kim, S.G.; Yun, P.Y.; Kim, J.S. Sinus bone graft using new alloplastic bone graft material (Osteon)-II: Clinical evaluation. Oral. Surg. Oral. Med. Oral. Pathol. Oral. Radiol. Endod. 2010, 109, e14–e20. [Google Scholar] [CrossRef]
- Beck-Broichsitter, B.E.; Westhoff, D.; Behrens, E.; Wiltfang, J.; Becker, S.T. Impact of surgical management in cases of intraoperative membrane perforation during a sinus lift procedure: A follow-up on bone graft stability and implant success. Int. J. Implant. Dent. 2018, 4, 6. [Google Scholar] [CrossRef]
- Becker, S.T.; Terheyden, H.; Steinriede, A.; Behrens, E.; Springer, I.; Wiltfang, J. Prospective observation of 41 perforations of the Schneiderian membrane during sinus floor elevation. Clin. Oral. Implant. Res. 2008, 19, 1285–1289. [Google Scholar] [CrossRef]
- de Almeida Ferreira, C.E.; Martinelli, C.B.; Novaes, A.B., Jr.; Pignaton, T.B.; Guignone, C.C.; Gonçalves de Almeida, A.L.; Saba-Chujfi, E. Effect of Maxillary Sinus Membrane Perforation on Implant Survival Rate: A Retrospective Study. Int. J. Oral. Maxillofac. Implant. 2017, 32, 401–407. [Google Scholar] [CrossRef]
- Froum, S.J.; Khouly, I.; Favero, G.; Cho, S.C. Effect of maxillary sinus membrane perforation on vital bone formation and implant survival: A retrospective study. J. Periodontol. 2013, 84, 1094–1099. [Google Scholar] [CrossRef]
- Guerrero, J.S. Lateral window sinus augmentation: Complications and outcomes of 101 consecutive procedures. Implant. Dent. 2015, 24, 354–361. [Google Scholar] [CrossRef]
- Hernández-Alfaro, F.; Torradeflot, M.M.; Marti, C. Prevalence and management of Schneiderian membrane perforations during sinus-lift procedures. Clin. Oral. Implant. Res. 2008, 19, 91–98. [Google Scholar] [CrossRef]
- Karabuda, C.; Arisan, V.; Özyuvaci, H. Effects of sinus membrane perforations on the success of dental implants placed in the augmented sinus. J. Periodontol. 2006, 77, 1991–1997. [Google Scholar] [CrossRef]
- Kim, G.S.; Lee, J.W.; Chong, J.H.; Han, J.J.; Jung, S.; Kook, M.S.; Park, H.J.; Ryu, S.Y.; Oh, H.K. Evaluation of clinical outcomes of implants placed into the maxillary sinus with a perforated sinus membrane: A retrospective study. Maxillofac. Plast. Reconstr. Surg. 2016, 38, 50. [Google Scholar] [CrossRef]
- Kim, Y.K.; Hwang, J.Y.; Yun, P.Y. Relationship between prognosis of dental implants and maxillary sinusitis associated with the sinus elevation procedure. Int. J. Oral. Maxillofac. Implant. 2013, 28, 178–183. [Google Scholar] [CrossRef]
- Kozuma, A.; Sasaki, M.; Seki, K.; Toyoshima, T.; Nakano, H.; Mori, Y. Preoperative chronic sinusitis as significant cause of postoperative infection and implant loss after sinus augmentation from a lateral approach. Oral. Maxillofac. Surg. 2017, 21, 193–200. [Google Scholar] [CrossRef]
- Oh, E.; Kraut, R.A. Effect of sinus membrane perforation on dental implant integration: A retrospective study on 128 patients. Implant. Dent. 2011, 20, 13–19. [Google Scholar] [CrossRef]
- Park, W.B.; Han, J.Y.; Kang, P.; Momen-Heravi, F. The clinical and radiographic outcomes of Schneiderian membrane perforation without repair in sinus elevation surgery. Clin. Implant. Dent. Relat. Res. 2019, 21, 931–937. [Google Scholar] [CrossRef]
- Park, W.B.; Herr, Y.; Chung, J.H.; Shin, S.I.; Han, J.Y.; Lim, H.C. Long-term effects of sinus membrane perforation on dental implants placed with transcrestal sinus floor elevation: A case-control study. Clin. Implant. Dent. Relat. Res. 2021, 23, 758–768. [Google Scholar] [CrossRef]
- Zhuang, X.; Lin, J.; Dong, H.; Wen, Y.; Xian, R.; Cheng, L.; Wu, J.; Li, S. The transalveolar approach with the small segmentation method for inclined maxillary sinus floor elevation: A retrospective study. Clin. Implant. Dent. Relat. Res. 2023, 26, 216–225. [Google Scholar] [CrossRef]
- Öncü, E.; Kaymaz, E. Assessment of the effectiveness of platelet rich fibrin in the treatment of Schneiderian membrane perforation. Clin. Implant. Dent. Relat. Res. 2017, 19, 1009–1014. [Google Scholar] [CrossRef]
- Thor, A.; Sennerby, L.; Hirsch, J.M.; Rasmusson, L. Bone formation at the maxillary sinus floor following simultaneous elevation of the mucosal lining and implant installation without graft material: An evaluation of 20 patients treated with 44 Astra Tech implants. J. Oral. Maxillofac. Surg. 2007, 65, 64–72. [Google Scholar] [CrossRef]
- Jung, J.H.; Choi, B.H.; Zhu, S.J.; Lee, S.H.; Huh, J.Y.; You, T.M.; Lee, H.J.; Li, J. The effects of exposing dental implants to the maxillary sinus cavity on sinus complications. Oral. Surg. Oral. Med. Oral. Pathol. Oral. Radiol. Endod. 2006, 102, 602–605. [Google Scholar] [CrossRef]
- Brandstaetter, T.; Ziv, O.; Sagy, I.; Segal, N.; Schneider, S.; Givol, N.; Levin, L.; Zadik, Y.; Kordeluk, S. Perforating dental implants and maxillary sinus pathology. Oral. Maxillofac. Surg. 2023. [Google Scholar] [CrossRef]
- Chrcanovic, B.R.; Albrektsson, T.; Wennerberg, A. Turned versus anodised dental implants: A meta-analysis. J. Oral. Rehabil. 2016, 43, 716–728. [Google Scholar] [CrossRef]
- Wennerberg, A.; Albrektsson, T.; Chrcanovic, B. Long-term clinical outcome of implants with different surface modifications. Eur. J. Oral. Implantol. 2018, 11 (Suppl. S1), S123–S136. [Google Scholar]
- Diaz-Olivares, L.A.; Cortes-Breton Brinkmann, J.; Martinez-Rodriguez, N.; Martinez-Gonzalez, J.M.; Lopez-Quiles, J.; Leco-Berrocal, I.; Meniz-Garcia, C. Management of Schneiderian membrane perforations during maxillary sinus floor augmentation with lateral approach in relation to subsequent implant survival rates: A systematic review and meta-analysis. Int. J. Implant. Dent. 2021, 7, 91. [Google Scholar] [CrossRef]
- Nolan, P.J.; Freeman, K.; Kraut, R.A. Correlation between Schneiderian membrane perforation and sinus lift graft outcome: A retrospective evaluation of 359 augmented sinus. J. Oral. Maxillofac. Surg. 2014, 72, 47–52. [Google Scholar] [CrossRef]
- Manor, Y.; Mardinger, O.; Bietlitum, I.; Nashef, A.; Nissan, J.; Chaushu, G. Late signs and symptoms of maxillary sinusitis after sinus augmentation. Oral. Surg. Oral. Med. Oral. Pathol. Oral. Radiol. Endod. 2010, 110, e1–e4. [Google Scholar] [CrossRef]
- Timmenga, N.M.; Raghoebar, G.M.; van Weissenbruch, R.; Vissink, A. Maxillary sinus floor elevation surgery. A clinical, radiographic and endoscopic evaluation. Clin. Oral. Implant. Res. 2003, 14, 322–328. [Google Scholar] [CrossRef]
- Tidwell, J.K.; Blijdorp, P.A.; Stoelinga, P.J.; Brouns, J.B.; Hinderks, F. Composite grafting of the maxillary sinus for placement of endosteal implants. A preliminary report of 48 patients. Int. J. Oral. Maxillofac. Surg. 1992, 21, 204–209. [Google Scholar] [CrossRef]
- Timmenga, N.M.; Raghoebar, G.M.; Boering, G.; van Weissenbruch, R. Maxillary sinus function after sinus lifts for the insertion of dental implants. J. Oral. Maxillofac. Surg. 1997, 55, 936–939; discussion 940. [Google Scholar] [CrossRef]
- Proussaefs, P.; Lozada, J.; Kim, J.; Rohrer, M.D. Repair of the perforated sinus membrane with a resorbable collagen membrane: A human study. Int. J. Oral. Maxillofac. Implant. 2004, 19, 413–420. [Google Scholar]
- Zijderveld, S.A.; van den Bergh, J.P.; Schulten, E.A.; ten Bruggenkate, C.M. Anatomical and surgical findings and complications in 100 consecutive maxillary sinus floor elevation procedures. J. Oral. Maxillofac. Surg. 2008, 66, 1426–1438. [Google Scholar] [CrossRef]
- Abdel-Halim, M.; Issa, D.; Chrcanovic, B.R. The Impact of Dental Implant Length on Failure Rates: A Systematic Review and Meta-Analysis. Materials 2021, 14, 3972. [Google Scholar] [CrossRef]
- Al Ansari, Y.; Shahwan, H.; Chrcanovic, B.R. Diabetes Mellitus and Dental Implants: A Systematic Review and Meta-Analysis. Materials 2022, 15, 3227. [Google Scholar] [CrossRef]
- Häggman-Henrikson, B.; Ali, D.; Aljamal, M.; Chrcanovic, B.R. Bruxism and dental implants: A systematic review and meta-analysis. J. Oral. Rehabil. 2024, 51, 202–217. [Google Scholar] [CrossRef]
- Mustapha, A.D.; Salame, Z.; Chrcanovic, B.R. Smoking and Dental Implants: A Systematic Review and Meta-Analysis. Medicina 2021, 58, 39. [Google Scholar] [CrossRef]
- Sulaiman, N.; Fadhul, F.; Chrcanovic, B.R. Bisphosphonates and Dental Implants: A Systematic Review and Meta-Analysis. Materials 2023, 16, 6078. [Google Scholar] [CrossRef]
- Chrcanovic, B.R.; Kisch, J.; Albrektsson, T.; Wennerberg, A. Impact of Different Surgeons on Dental Implant Failure. Int. J. Prosthodont. 2017, 30, 445–454. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).